The Pediatric Trochlear Migraine: Diagnostic and Therapeutic Implications
Abstract
:1. Introduction
2. Case Series
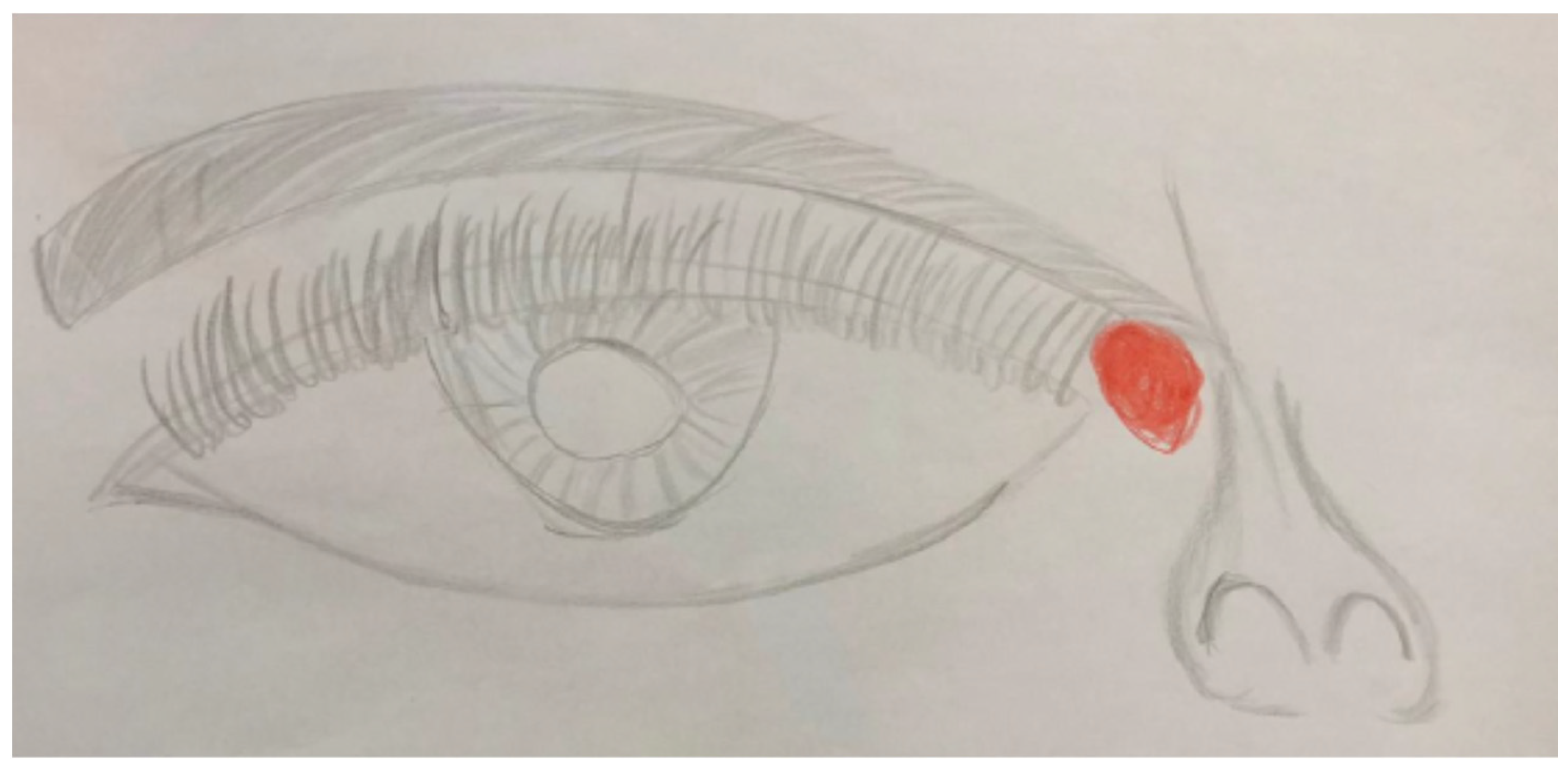
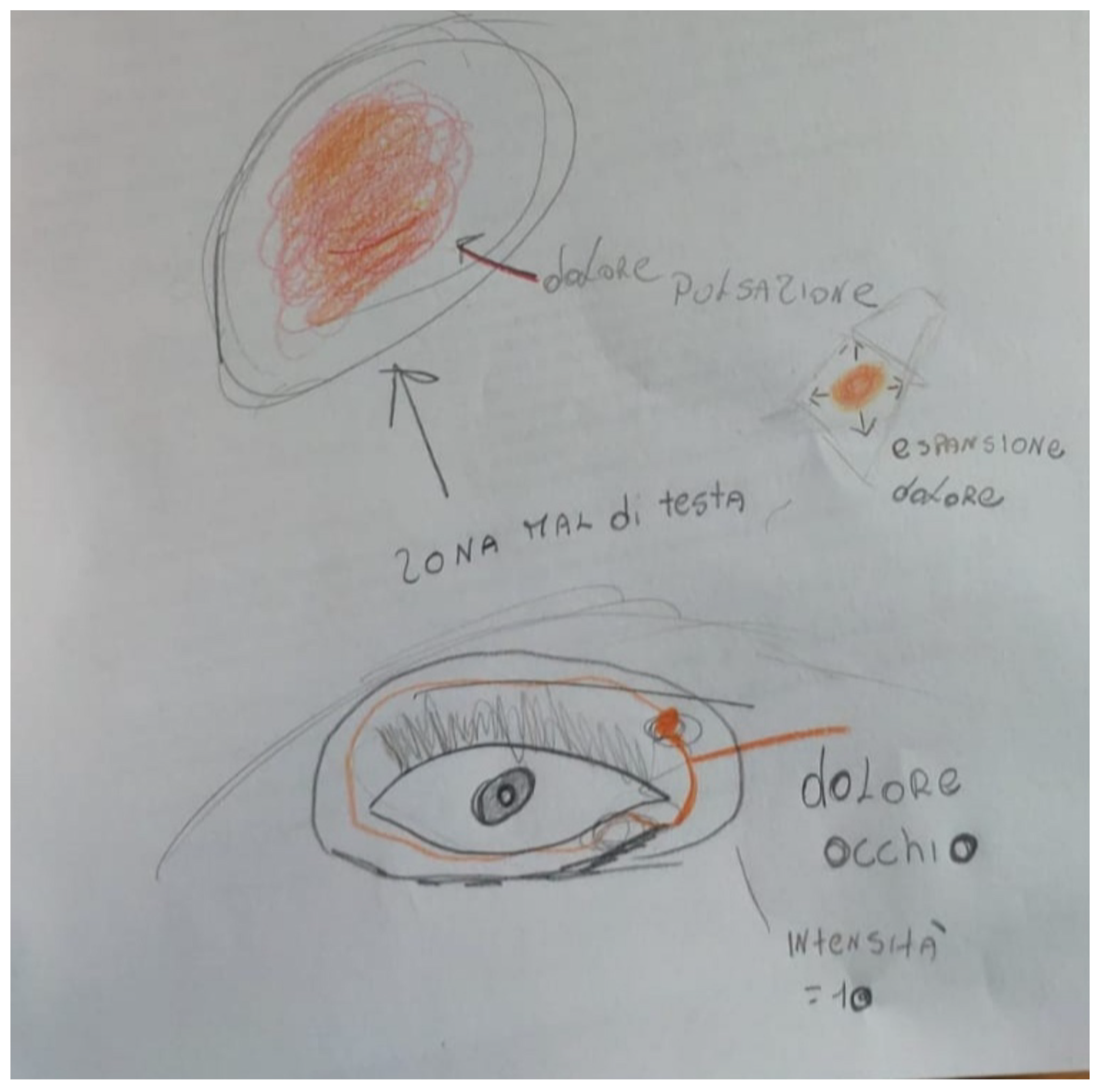
2.1. Case 1
2.2. Case 2
2.3. Case 3
2.4. Case 4
3. Clinical Features of PTM
4. Physiopathological and Anatomical Considerations
5. Differential Diagnosis
6. Nosographic Considerations
Migraine Familiarity; Pain Relief with Rest and Sleep
7. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
References
- Lance, J.W.; Goadsby, P.J. Mechanisms and Management of Headache, 6th ed.; Butterworth-Heinemann: Oxford, UK, 1998; p. 5. [Google Scholar]
- Yanguela, J.; Pareja, J.A.; Lopez, N.; Sanchez Del Rio, M. Trochleitis and migraine headache. Neurology 2002, 58, 802–805. [Google Scholar] [CrossRef] [PubMed]
- Yangüela, J.; Sanchez-del-Rio, M.; Bueno, A.; Espinosa, A.; Gili, P.; Lopez-Ferrando, N.; Barriga, F.; Nieto, J.C.; Pareja, J.A. Primary trochlear headache: A new cephalgia generated and modulated on the trochlear region. Neurology 2004, 62, 1134–1140. [Google Scholar] [CrossRef] [PubMed]
- Pareja, J.A.; Sanchez del Rio, M. Primary trochlear headache and other trochlear painful disorders. Curr. Pain Headache Rep. 2006, 10, 316–320. [Google Scholar] [CrossRef] [PubMed]
- Headache Classification Committee of the International Headache Society (IHS). The International Classification of Headache Disorders, 3rd edition. Cephalalgia 2018, 38, 1–211. [Google Scholar] [CrossRef] [PubMed]
- Evans, R.W.; Pareja, J.A. Trochleodynia and Migraine. Headache 2010, 50, 481–484. [Google Scholar] [CrossRef]
- Zaragoza-Casares, P.; Gómez-Fernández, T.; De Liaño, M.A.Z.G.; Zaragoza-Garcia, P. Bilateral idiopathic trochleitis as a cause of frontal cephalgia. Headache 2009, 49, 476–477. [Google Scholar] [CrossRef]
- Smith, J.H.; Garrityb, J.A.; Boes, C.J. Clinical features and long-term prognosis of trochlear headaches. Eur. J. Neurol. 2014, 21, 577–585. [Google Scholar] [CrossRef]
- Raieli, V.; Cardella, F.; Roppolo, R.; Messina, L.M.; Vanadia, F.; Brighina, F. Does Trochlear migraine exist? A “pure” pediatric case report and nosographic considerations. Curr. Neurobiol. 2019, 10, 1–4. [Google Scholar]
- Sánchez Ruiz, P.; Martín Villaescusa, C.; Duat Rodríguez, A.; Cantarín Extremera, V.; Ruiz-Falcó Rojas, M.L. Primary trochlear headache. A periorbital pain with a specific diagnosis and treatment. Arch. Soc. Esp. Oftalmol. 2020, 95, 150–152. [Google Scholar] [CrossRef]
- Ojha, P.; Aglave, V.; Basak, S.; Jayendra Yadav, J. Failure to identify underlying autoimmunity and primary headache disorder might be the reasons for refractoriness of trochlear headaches. Cephalalgia Rep. 2020, 3, 2515816320951770. [Google Scholar] [CrossRef]
- Ashina, M. Migraine. N. Engl. J. Med. 2020, 383, 1866–1876. [Google Scholar] [CrossRef] [PubMed]
- Do, T.P.; Heldarskard, G.F.; Kolding, L.T.; Hvedstrup, J.; Schtz, H.W. Myofascial trigger points in migraine and tension type headache. J. Headache Pain. 2018, 19, 18. [Google Scholar] [CrossRef] [PubMed]
- Fernandez-de-Las-penas, C.; Cuadrado, M.L.; Gerwin, R.D.; Pareja, J.A. Myofascial disorders in the trochlear region in unilateral migraine: A possible initiating or perpetuating factor. Clin. J. Pain. 2006, 22, 548–553. [Google Scholar] [CrossRef] [PubMed]
- Chanlalit, W.; Teeyapant, C.; Soodchuen, S. Trochlear pain: Clinical characteristics and treatment outcomes. J. Neurol. 2017, 265, 376–380. [Google Scholar] [CrossRef] [PubMed]
- Voirol, J.R.; Vilensky, J.A. The normal and variant clinical anatomy of the sensory supply of the orbit. Clin. Anat. 2014, 27, 169–175. [Google Scholar] [CrossRef]
- Jones, H.R. Netter’s Neurology; Icon Learning Systems LLC.: Teterboro, NJ, USA, 2005; pp. 77–111. [Google Scholar]
- Liu, G.T. The Trigeminal Nerve and its Central Connections; Lippincott Williams and Wilkin: Philadelphia, PA, USA, 2005; pp. 1233–1263. [Google Scholar]
- Lazino, G.; Andreoli, F.; Tognetti, P.; Limoni, F.; Calbucci, R.; Bortolami, M.; Lucchi, M.L.; Callegari, E.; Testa, C. Orbital pain and unruptured carotid-posterior communicating artery aneurysms: The role of sensory fibers of the third cranial nerve. Acta Neurochir. 1993, 120, 7–11. [Google Scholar] [CrossRef]
- Lee, J.Y.; Kim, K.D.; Hwang, E.H.; Park, H.S.; Park, C.S. Inflammatory orbital pseudotumor with infratemporal fossa extension mimicking temporomadibular joint dysfunction. Dentomaxillofac. Radiol. 2002, 31, 147–150. [Google Scholar] [CrossRef]
- Friedman, D.I. Headache and the eye. Curr. Pain Headache Rep. 2008, 12, 296–304. [Google Scholar] [CrossRef]
- Tran, M.; McClelland, C.M.; Lee, M.S. Diagnosis and management of trochleodynia, trochleitis and Trochlear headache. Front. Neurol. 2019, 10, 361. [Google Scholar] [CrossRef] [Green Version]
- Berchtold, V.; Stofferin, H.; Moriggl, B.; Brenner, B.; Pauzenberger, R.; Konschake, M. The supraorbital region revisited—An anatomic exploration of the neuro-vascular bundle with regard to frontal migraine headache. J. Plast. Reconstr. Aesthet. Surg. 2017, 70, 1171–1180. [Google Scholar] [CrossRef]
- Aurora, S. Botulinum toxin type A for the treatment of migraine. Expert Opin. Pharmacother. 2006, 7, 1085–1095. [Google Scholar] [CrossRef] [PubMed]
- Hoffmann, J.; May, A. Diagnosis, pathophysiology and management of cluster headache. Lancet Neurol. 2018, 17, 75–83. [Google Scholar] [CrossRef]
- Schwartz, D.P.; Robbins, M.S.; Grosberg, B.M. Nummular Headache Update. Curr. Pain Headache Rep. 2013, 17, 340. [Google Scholar] [CrossRef]
- Pareja, J.A.; Caminero, A.B. Supraorbital Neuralgia. Curr. Pain Headache Rep. 2006, 10, 302–305. [Google Scholar] [CrossRef]
- Villar-Quiles, R.N.; García-Moreno, H.; Mayo, D.; Gutiérrez-Viedma, Á.; Ramos, M.I.; Casas-Limón, J.; Cuadrado, M.L. Infratrochlear neuralgia: A prospective series of seven patients treated with infratrochlear nerve blocks. Cephalalgia 2018, 38, 585–591. [Google Scholar] [CrossRef]
- Manley, D.R.; Alvi, R.A. Brown’s syndrome. Curr. Op. Ophthalmol. 2011, 22, 432–440. [Google Scholar] [CrossRef]
- Martins, W.A.; Marrone, L.C.P.; Saute, R.; Becker, J.; Vargas, J.A.A.; da Costa Vargas, J.F.; Marrone, A.C.H. Ocular myositis: Insights into recurrence and semeiological presentation. Int. J. Neurosci. 2015, 125, 711–715. [Google Scholar] [CrossRef]
- Thacker, N.M.; Velez, F.G.; Demer, J.L.; Rosenbaum, A.L. Superior oblique muscle involvement in thyroid ophthalmopathy. J. AAPOS 2005, 9, 174–178. [Google Scholar] [CrossRef]
- Mullen, E.; Green, M.; Hersh, E.; Iloreta, A.M.; Bederson, J.; Shrivastava, R. Tolosa Hunt syndrome: Appraising the ICHD-3 beta diagnostic criteria. Cephalalgia 2018, 38, 1696–1700. [Google Scholar] [CrossRef]
- Pareja, J.A.; Cuadrado, M.L.; Porta-Etessam, J.; Fernández-de-las-Peñas, C.; Gili, P.; Caminero, A.B.; Cebrián, J.L. Idiopathic ophthalmodynia and idiopathic rhinalgia: Two topographic facial pain syndromes. Headache 2010, 50, 1286–1295. [Google Scholar] [CrossRef]
- Alvarez, M.; Montojo, T.; de la Casa, B.; Vela, L.; Pareja, J.A. Unilateral nasal pain with migraine features. Cephalalgia. 2013, 33, 1055–1058. [Google Scholar] [CrossRef] [PubMed]
- Pego-Regosa, R.; Vazquez-Lopez, M.E.; Iglesias-Gomez, S.; Martin-Vazquez, F.M. Association between chronic paroxsmal hemicrania and primary trochlear headache: Pathophysiology and treatment. Cephalalgia 2010, 30, 373–374. [Google Scholar]
- Cuadrado, M.I.; Porta-Etessam, J.; Pareja, J.A.; Matias-Guiu, J. Hemicrania continua responsive to trochlear injection of corticosteroids. Cephalalgia. 2010, 30, 373–374. [Google Scholar] [CrossRef] [PubMed]
- Barad, M.; Ailani, J.; Hakim, S.M.; Kissoon, N.R.; Schuster, N.M. Percutaneous Interventional Strategies for Migraine Prevention: A Systematic Review and Practice Guideline. Pain Med. 2022, 23, 164–188. [Google Scholar] [CrossRef]
- Cuadrado, M.L.; Guerrero, A.L.; Pareja, J.A. Epicrania fugax. Curr. Pain Headache Rep. 2016, 20, 21. [Google Scholar] [CrossRef]
- Raieli, V.; Compagno, A.; Damelio, M. Red ear syndrome. Curr. Pain Headache Rep. 2016, 20, 19. [Google Scholar] [CrossRef]
- The Orofacial Pain Classification Committee: International classification of orofacial pain, 1st edition (ICOP). Cephalalgia 2020, 40, 129–221. [CrossRef] [Green Version]
| Clinical Features | 1 (Raieli Unpublished Case | 2 (Raieli Unpublished Case | 3 (Raieli Unpublished Case | 4 (Raieli Unpublished Case | 1 (Yanguela et al., Neurology 2002) | 2 (Yanguela et al., Neurology 2002) | 3 (Yanguela et al., Neurology 2002) | Sanchez-ruiz et al. 2020 |
|---|---|---|---|---|---|---|---|---|
| Sex | M | M | F | M | F | F | F | F |
| Age at diagnosis trochlear pain | 12 | 11 | 16 | 11 | ? | ? | ? | 13 |
| Age at onset of migraine, y | 6 | 10 | 11 | 10 | 8 | 15 | 17 | ? |
| Migraine subtype | Ep MwA | Ep MwA | Ep MwA | Ep MwA | Ch | Ep | Ch | MwA |
| Location of migraine pain | Troch. | Troch/fronto-temp | Troch/front | Troch | R H | L H | L > R H | ? |
| Age at onset trochlear pain | 6 | Not specified | 1 years | 10 | 39 | 49 | 56 | 13 |
| Side trochlear pain | Alternanting Dx > sx | Alternanting | Alternantindx | Unilateral dx | U | U | U | U sx |
| Quality troclear pain | Puls./pre | Puls. | Puls. | Puls. | Puls. | Squez. | Sand | ? |
| Temporal pattern of active pain period | Recurrent episodes | Recurrent episodes | Recurrent Episodes | Recurrent episodes | Cont. | Cont. | Cont. | Cont |
| Intensity of trochlear pain (not included excerbations) | 7–9 | 7–8 | 7–8 | 8 | 4 | 4–5 | 3–4 | 7 |
| Photo/phonophobia associated to trochlear pain | + | + | + | − | − | − | − | + |
| Nausea associated to trochlear pain | + | + | + | + | − | − | − | + |
| Vomiting associated to trochlear pain | + | − | + | − | − | − | − | + |
| Diplopia | − | − | − | − | + | − | − | − |
| Trigger trochlear for migraine attacks | Not applicable | Not applicable | Not applicable | Not applicable | + | − | − | − |
| Response to local steroid injection | Not applicable | Not applicable | Not applicable | Not applicable | + | + | + | + |
| Response to triptans | No report | No report | + | + | No report | No report | No report | No report |
| Preventive treatment | + | + | No | + | No report | No report | No report | No report |
| Familiarity for Migraine | + | + | + | + | No report | No report | No report | No report |
| Primary Trochlear Headache | Pure Trochlear Migraine | Supra/Infratrochlear Neuralgias | |
|---|---|---|---|
| Age at onset | Adult> | pediatric | variable |
| Pain location | trochlear | trochlear | Supra/medial infratrochlear |
| Side location | unilateral | Unilateral- alternating side, bilateral | unilateral |
| Other cephalalgic side | sometimes Frontal-temporal | Frontal-temporal | frontal |
| Temporal pattern | Chronic | episodic | Continue > episodic |
| Quality of pain | variable | pulsanting | Sharp paroxysmal /dull |
| Duration of painduring symptomatic period | daily | hours | daily |
| Intensity Pain | Moderate/severe | Moderate/severe | severe |
| Allodynia | − | + | + |
| Local symptoms | − | + | − |
| Vomit | − | + | − |
| Nausea | +− | + | − |
| Phonophobia | − | + | − |
| Photophobia | +− | + | − |
| Painful ocular movements | + | −+ | − |
| Selective tenderness on the trochlear area | + | −+ | + |
| Other triggers | ? | Foods menstrual cycle etc. | trauma |
| Response to local injection of corticosteroids within 48 h | + | ? | Anestethic blockade |
| Radiological findings | no | no | possible |
| Secondary causes | no | no | Trauma/compression |
| Triptans response | − | + | − |
| Preventive oral treatment | − | + | +− |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Raieli, V.; Reina, F.; D’Agnano, D.; Nocera, G.M.; Capizzi, M.; Marchese, F.; Sciruicchio, V. The Pediatric Trochlear Migraine: Diagnostic and Therapeutic Implications. J. Clin. Med. 2022, 11, 2826. https://doi.org/10.3390/jcm11102826
Raieli V, Reina F, D’Agnano D, Nocera GM, Capizzi M, Marchese F, Sciruicchio V. The Pediatric Trochlear Migraine: Diagnostic and Therapeutic Implications. Journal of Clinical Medicine. 2022; 11(10):2826. https://doi.org/10.3390/jcm11102826
Chicago/Turabian StyleRaieli, Vincenzo, Federica Reina, Daniela D’Agnano, Giovanna Martina Nocera, Mariarita Capizzi, Francesca Marchese, and Vittorio Sciruicchio. 2022. "The Pediatric Trochlear Migraine: Diagnostic and Therapeutic Implications" Journal of Clinical Medicine 11, no. 10: 2826. https://doi.org/10.3390/jcm11102826
APA StyleRaieli, V., Reina, F., D’Agnano, D., Nocera, G. M., Capizzi, M., Marchese, F., & Sciruicchio, V. (2022). The Pediatric Trochlear Migraine: Diagnostic and Therapeutic Implications. Journal of Clinical Medicine, 11(10), 2826. https://doi.org/10.3390/jcm11102826






