Interventional Radiology in the Management of Metastases and Bone Tumors
Abstract
:1. Introduction
2. Interventional Radiology—Techniques
- 1.
- Embolization
- To lower pain and natural bleeding of tumors that cannot gain benefit from surgical or percutaneous therapy.
- To reduce tumor vascularization before percutaneous ablation and reduce the heat/cold-sink effect.
- 2.
- Thermal ablation
2.1. Radiofrequency Ablation
2.2. Microwave Ablation (MWA)
- Benign OO: MWA can reliably treat OO, with no recognized complications or recurrence; less evidence then RFA.
- Malignant (skeletal metastases, multiple myeloma, soft tissue metastases, and plasmocytomas).
2.3. Cooling Techniques: Cryoablation
- Benign: Extra-abdominal desmoid tumors, OO, OB, Aneurismal Bone Cists, primary bone tumors, neuroma and arteriovenous malformations (AVMs) and chondroblastoma.
- Malignant: Skeletal metastases (even osteoblastic and sclerotic; myeloma, soft tissue metastases, plasmocytomas, and in-transit melanoma metastases.
- Neurovascular: Palliative; neuroendocrine metastases, hemangioendotheliomas, and benign neural tumors such as Morton’s neuroma.
2.4. Non-Percutaneous Thermal Ablation Procedures: High-Intensity Focused Ultrasound Ablation (HIFU)
- Benign: OO and OB can be successfully treated with MRgFUS with complete pain relief and no morbidity; extra-abdominal desmoid tumors.
- Malignant: metastases and/or multiple myeloma, plasmocytoma, and other focal myeloproliferative disorders
2.5. Stabilizers
2.5.1. Cementoplasty
- Patients with severe pain and neurological damage caused by spinal lesions, and resistance to conventional treatments.
- Patients with spinal instability caused by spinal lesions within the vertebral body.
- Patients with contraindications to open surgery.
2.5.2. Percutaneous Osteosynthesis
2.6. General Requirements Needing Careful Analysis before IR Procedures
- -
- The primary cancer is unknown;
- -
- More than two primary tumors are suspected;
- -
- Specimen analysis is crucial to adjust systemic therapy.
2.7. Follow-Up after IR Procedures
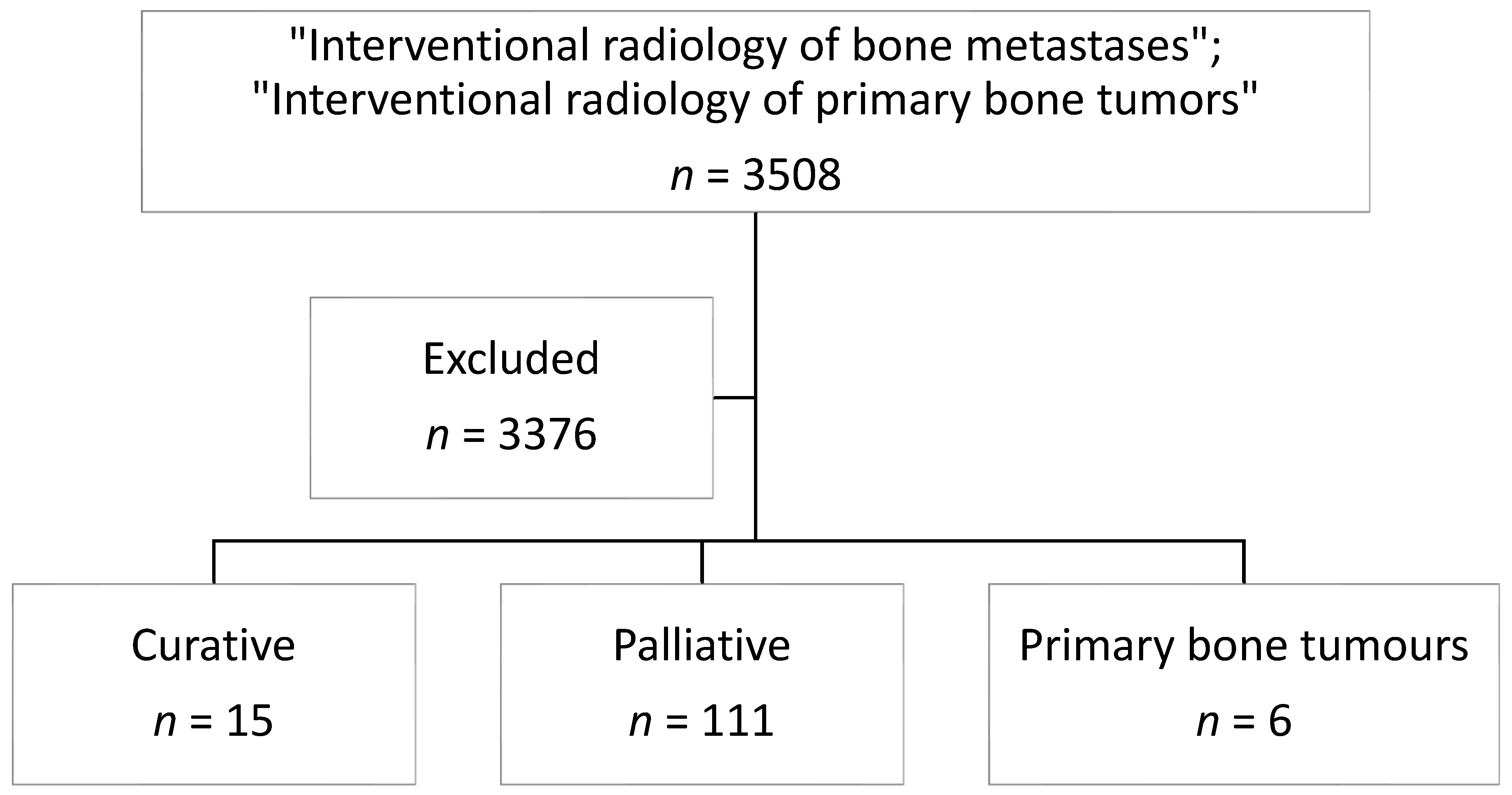
3. Literature Search Strategy and Results—Interventional Strategies in Bone Metastases
3.1. Curative Treatment
3.2. Palliative Treatments
3.3. Palliative Treatment of Both Bone Fracture and Impending Fracture
3.4. Role of Radiation Therapy and Surgery
4. Indications in Primary Bone Tumors
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Cazzato, R.L.; Arrigoni, F.; Boatta, E.; Bruno, F.; Chiang, J.B.; Garnon, J.; Zugaro, L.; Giordano, A.V.; Carducci, S.; Varrassi, M.; et al. Percutaneous management of bone metastases: State of the art, interventional strategies and joint position statement of the Italian College of MSK Radiology (ICoMSKR) and the Italian College of Interventional Radiology (ICIR). Radiol. Med. 2019, 124, 34–49. [Google Scholar] [CrossRef]
- Shimohira, M.; Nagai, K.; Hashizume, T.; Nakagawa, M.; Ozawa, Y.; Sakurai, K.; Matsushita, Y.; Yamada, S.; Otsuka, T.; Shibamoto, Y. Preoperative transarterial embolization using gelatin sponge for hypervascular bone and soft tissue tumors in the pelvis or extremities. Acta Radiol. 2016, 57, 457–462. [Google Scholar] [CrossRef]
- Kickuth, R.; Waldherr, C.; Hoppe, H.; Bonel, H.M.; Ludwig, K.; Beck, M.; Triller, J. Interventional Management of Hypervascular Osseous Metastasis: Role of Embolotherapy Before Orthopedic Tumor Resection and Bone Stabilization. AJR Am. J. Roentgenol. 2008, 191, W240–W247. [Google Scholar] [CrossRef]
- Kato, S.; Hozumi, T.; Takaki, Y.; Yamakawa, K.; Goto, T.; Kondo, T. Optimal Schedule of Preoperative Embolization for Spinal Metastasis Surgery. Spine 2013, 38, 1964–1969. [Google Scholar] [CrossRef]
- Rossi, G.; Mavrogenis, A.F.; Rimondi, E.; Braccaioli, L.; Calabrò, T.; Ruggieri, P. Selective Embolization with N-butyl Cyanoacrylate for Metastatic Bone Disease. J. Vasc. Interv. Radiol. 2011, 22, 462–470. [Google Scholar] [CrossRef]
- Chen-Xu, S.; Martel-Villagrán, J.; Bueno-Horcajadas, Á. Percutaneous management of bone metastases: State of the art. Radiología 2021, 63, 345–357. [Google Scholar] [CrossRef]
- Dalili, D.; Isaac, A.; Bazzocchi, A.; Åström, G.; Bergh, J.; Lalam, R.; Weber, M.-A.; Fritz, J.; Mansour, R. Interventional Techniques for Bone and Musculoskeletal Soft Tissue Tumors: Current Practices and Future Directions—Part I. Ablation. Semin. Musculoskelet. Radiol. 2020, 24, 692–709. [Google Scholar] [CrossRef]
- Barile, A.; Arrigoni, F.; Bruno, F.; Palumbo, P.; Floridi, C.; Cazzato, R.L.; Reginelli, A.; Zappia, M.; Brunese, L.; Zugaro, L.; et al. Present role and future perspectives of interventional radiology in the treatment of painful bone lesions. Future Oncol. 2018, 14, 2945–2955. [Google Scholar] [CrossRef]
- Callstrom, M.R.; Charboneau, J.W. Image-Guided Palliation of Painful Metastases Using Percutaneous Ablation. Tech. Vasc. Interv. Radiol. 2007, 10, 120–131. [Google Scholar] [CrossRef]
- Rosenthal, D.; Callstrom, M.R. Critical Review and State of the Art in Interventional Oncology: Benign and Metastatic Disease Involving Bone. Radiology 2012, 262, 765–780. [Google Scholar] [CrossRef]
- Arrigoni, F.; De Cataldo, C.; Bruno, F.; Palumbo, P.; Zugaro, L.; Di Staso, M.; Gravina, G.L.; Barile, A.; Masciocchi, C. Ablation, consolidation and radiotherapy for the management of metastatic lesions of the spine: Impact on the quality of life in a mid-term clinical and diagnostic follow-up in a pilot study. Med. Oncol. 2020, 37, 53. [Google Scholar] [CrossRef]
- Di Staso, M.; Zugaro, L.; Gravina, G.L.; Bonfili, P.; Marampon, F.; Di Nicola, L.; Conchiglia, A.; Ventura, L.; Franzese, P.; Gallucci, M.; et al. A feasibility study of percutaneous radiofrequency ablation followed by radiotherapy in the management of painful osteolytic bone metastases. Eur. Radiol. 2011, 21, 2004–2010. [Google Scholar] [CrossRef]
- Wallace, A.; Tomasian, A.; Vaswani, D.; Vyhmeister, R.; Chang, R.; Jennings, J. Radiographic Local Control of Spinal Metastases with Percutaneous Radiofrequency Ablation and Vertebral Augmentation. Am. J. Neuroradiol. 2016, 37, 759–765. [Google Scholar] [CrossRef] [Green Version]
- Levy, J.; Hopkins, T.; Morris, J.; Tran, N.D.; David, E.; Massari, F.; Farid, H.; Vogel, A.; O’Connell, W.G.; Sunenshine, P.; et al. Radiofrequency Ablation for the Palliative Treatment of Bone Metastases: Outcomes from the Multicenter OsteoCool Tumor Ablation Post-Market Study (OPuS One Study) in 100 Patients. J. Vasc. Interv. Radiol. 2020, 31, 1745–1752. [Google Scholar] [CrossRef]
- Gardner, C.S.; Ensor, J.E.; Ahrar, K.; Huang, S.Y.; Sabir, S.H.; Tannir, N.M.; Lewis, V.O.; Tam, A.L. Cryoablation of Bone Metastases from Renal Cell Carcinoma for Local Tumor Control. J. Bone Jt. Surg. Am. 2017, 99, 1916–1926. [Google Scholar] [CrossRef]
- Wang, F.; Gu, J.; Xu, C.; Li, G.; Lv, P. The combination of radiofrequency ablation and vertebroplasty shows advantages over single vertebroplasty in treating vertebral neoplastic lesions. Skelet. Radiol. 2022, 51, 565–571. [Google Scholar] [CrossRef]
- Pusceddu, C.; Dessì, G.; Melis, L.; Fancellu, A.; Ruggiu, G.; Sailis, P.; Congia, S.; Derudas, D.; Cau, R.; Senis, I.; et al. Combined Microwave Ablation and Osteosynthesis for Long Bone Metastases. Medicina 2021, 57, 825. [Google Scholar] [CrossRef]
- Jiao, D.; Yao, Y.; Li, Z.; Ren, J.; Han, X. Simultaneous C-arm Computed Tomography-Guided Microwave Ablation and Cementoplasty in Patients with Painful Osteolytic Bone Metastases: A Single-center Experience. Acad. Radiol. 2022, 29, 42–50. [Google Scholar] [CrossRef]
- Caracciolo, J.T.; Letson, G.D. Radiologic Approach to Bone and Soft Tissue Sarcomas. Surg. Clin. N. Am. 2016, 96, 963–976. [Google Scholar] [CrossRef]
- Dea, N.; Gokaslan, Z.; Choi, D.; Fisher, C. Spine Oncology–Primary Spine Tumors. Neurosurgery 2017, 80, S124–S130. [Google Scholar] [CrossRef] [Green Version]
- Chen, W.; Zhu, H.; Zhang, L.; Li, K.; Su, H.; Jin, C.; Zhou, K.; Bai, J.; Wu, F.; Wang, Z. Primary Bone Malignancy: Effective Treatment with High-Intensity Focused Ultrasound Ablation. Radiology 2010, 255, 967–978. [Google Scholar] [CrossRef]
- Barton, P.P.; Waneck, R.E.; Karnel, F.J.; Ritschl, P.; Kramer, J.; Lechner, G.L. Embolization of Bone Metastases. J. Vasc. Interv. Radiol. 1996, 7, 81–88. [Google Scholar] [CrossRef]
- Rybak, L.D. Fire and Ice: Thermal Ablation of Musculoskeletal Tumors. Radiol. Clin. N. Am. 2009, 47, 455–469. [Google Scholar] [CrossRef]
- Tomasian, A.; Wallace, A.; Jennings, J. Benign Spine Lesions: Advances in Techniques for Minimally Invasive Percutaneous Treatment. AJNR Am. J. Neuroradiol. 2017, 38, 852–861. [Google Scholar] [CrossRef] [Green Version]
- Dupuy, D.E.; Liu, D.; Rn, D.H.; Hanna, L.; Blume, J.D.; Ahrar, K.; Lopez, R.R.; Safran, H.; A DiPetrillo, T. Percutaneous radiofrequency ablation of painful osseous metastases: A multicenter American College of Radiology Imaging Network trial. Cancer 2010, 116, 989–997. [Google Scholar] [CrossRef] [Green Version]
- Zhao, W.; Wang, H.; Hu, J.-H.; Peng, Z.-H.; Chen, J.-Z.; Huang, J.-Q.; Jiang, Y.-N.; Luo, G.; Yi, G.-F.; Shen, J.; et al. Palliative pain relief and safety of percutaneous radiofrequency ablation combined with cement injection for bone metastasis. Jpn. J. Clin. Oncol. 2018, 48, 753–759. [Google Scholar] [CrossRef]
- Madaelil, T.P.; Wallace, A.N.; Jennings, J.W. Radiofrequency ablation alone or in combination with cementoplasty for local control and pain palliation of sacral metastases: Preliminary results in 11 patients. Skelet. Radiol. 2016, 45, 1213–1219. [Google Scholar] [CrossRef]
- Cazzato, R.L.; Auloge, P.; De Marini, P.; Rousseau, C.; Chiang, J.B.; Koch, G.; Caudrelier, J.; Rao, P.; Garnon, J.; Gangi, A. Percutaneous image-guided ablation of bone metastases: Local tumor control in oligometastatic patients. Int. J. Hyperth. 2018, 35, 493–499. [Google Scholar] [CrossRef] [Green Version]
- Callstrom, M.R.; Charboneau, J.W.; Goetz, M.P.; Rubin, J.; Atwell, T.D.; Farrell, M.A.; Welch, T.J.; Maus, T.P. Image-guided ablation of painful metastatic bone tumors: A new and effective approach to a difficult problem. Skelet. Radiol. 2006, 35, 1–15. [Google Scholar] [CrossRef]
- Barral, M.; Auperin, A.; Hakime, A.; Cartier, V.; Tacher, V.; Otmezguine, Y.; Tselikas, L.; de Baere, T.; Deschamps, F. Percutaneous Thermal Ablation of Breast Cancer Metastases in Oligometastatic Patients. Cardiovasc. Interv. Radiol. 2016, 39, 885–893. [Google Scholar] [CrossRef]
- Simon, C.J.; Dupuy, D.E. Percutaneous Minimally Invasive Therapies in the Treatment of Bone Tumors: Thermal Ablation. Semin. Musculoskelet. Radiol. 2006, 10, 137–144. [Google Scholar] [CrossRef] [PubMed]
- Erickson, J.K.; Rosenthal, D.I.; Zaleske, D.J.; Gebhardt, M.C.; Cates, J.M. Primary Treatment of Chondroblastoma with Percutaneous Radio-frequency Heat Ablation: Report of Three Cases. Radiology 2001, 221, 463–468. [Google Scholar] [CrossRef] [PubMed]
- Munk, P.L.; Malfair, D.; Rashid, F.; Torreggiani, W.C. Radiofrequency Ablation of Solitary Eosinophilic Granuloma of Bone. Am. J. Roentgenol. 2008, 191, W320. [Google Scholar] [CrossRef] [PubMed]
- Kujak, J.L.; Liu, P.T.; Johnson, G.; Callstrom, M.R. Early experience with percutaneous cryoablation of extra-abdominal desmoid tumors. Skelet. Radiol. 2010, 39, 175–182. [Google Scholar] [CrossRef] [PubMed]
- Janjan, N.A.; Payne, R.; Gillis, T.; Podoloff, D.; Libshitz, H.; Lenzi, R.; Theriault, R.; Martin, C.; Yasko, A. Presenting Symptoms in Patients Referred to a Multidisciplinary Clinic for Bone Metastases. J. Pain Symptom Manag. 1998, 16, 171–178. [Google Scholar] [CrossRef]
- Breckheimer, A.; Bruners, P.; Mahnken, A. Interventional management of a rare complication in radiofrequency ablation of an osteosclerotic bone metastasis. Rofo 2010, 182, 433. [Google Scholar] [CrossRef]
- Goetz, M.P.; Callstrom, M.R.; Charboneau, J.W.; Farrell, M.A.; Maus, T.P.; Welch, T.J.; Wong, G.Y.; Sloan, J.A.; Novotny, P.J.; Petersen, I.A.; et al. Percutaneous Image-Guided Radiofrequency Ablation of Painful Metastases Involving Bone: A Multicenter Study. J. Clin. Oncol. 2004, 22, 300–306. [Google Scholar] [CrossRef]
- Mohan, H.; Nicholson, P.; Winter, D.C.; O’Shea, D.; O’Toole, D.; Geoghegan, J.; Maguire, D.; Hoti, E.; Traynor, O.; Cantwell, C.P. Radiofrequency Ablation for Neuroendocrine Liver Metastases: A Systematic Review. J. Vasc. Interv. Radiol. 2015, 26, 935–942.e1. [Google Scholar] [CrossRef]
- Connors, J.C.; Boike, A.M.; Rao, N.; Kingsley, J.D. Radiofrequency Ablation for the Treatment of Painful Neuroma. J. Foot Ankle Surg. 2020, 59, 457–461. [Google Scholar] [CrossRef]
- Brace, C.L.; Laeseke, P.F.; Sampson, L.A.; Frey, T.M.; van der Weide, D.W.; Lee, F.T. Microwave Ablation with Multiple Simultaneously Powered Small-gauge Triaxial Antennas: Results from an in Vivo Swine Liver Model. Radiology 2007, 244, 151–156. [Google Scholar] [CrossRef]
- Wright, A.S.; Sampson, L.A.; Warner, T.F.; Mahvi, D.M.; Lee, J.F.T. Radiofrequency versus Microwave Ablation in a Hepatic Porcine Model. Radiology 2005, 236, 132–139. [Google Scholar] [CrossRef] [PubMed]
- Ringe, K.I.; Lutat, C.; Rieder, C.; Schenk, A.; Wacker, F.; Raatschen, H.-J. Experimental Evaluation of the Heat Sink Effect in Hepatic Microwave Ablation. PLoS ONE 2015, 10, e0134301. [Google Scholar] [CrossRef] [PubMed]
- Ringe, K.I.; Panzica, M.; von Falck, C. Thermoablation of Bone Tumors. Rofo 2016, 188, 539–550. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hinshaw, J.L.; Lubner, M.G.; Ziemlewicz, T.J.; Lee, F.T., Jr.; Brace, C.L. Percutaneous Tumor Ablation Tools: Microwave, Radiofrequency, or Cryoablation—What Should You Use and Why? Radiographics 2014, 34, 1344–1362. [Google Scholar] [CrossRef] [PubMed]
- Carrafiello, G.; Laganà, D.; Mangini, M.; Fontana, F.; Dionigi, G.; Boni, L.; Rovera, F.; Cuffari, S.; Fugazzola, C. Microwave tumors ablation: Principles, clinical applications and review of preliminary experiences. Int. J. Surg. 2008, 6 (Suppl. S1), S65–S69. [Google Scholar] [CrossRef] [Green Version]
- Thacker, P.G.; Callstrom, M.R.; Curry, T.B.; Mandrekar, J.N.; Atwell, T.D.; Goetz, M.P.; Rubin, J. Palliation of Painful Metastatic Disease Involving Bone with Imaging-Guided Treatment: Comparison of Patients’ Immediate Response to Radiofrequency Ablation and Cryoablation. AJR Am. J. Roentgenol. 2011, 197, 510–515. [Google Scholar] [CrossRef]
- Susa, M.; Kikuta, K.; Nakayama, R.; Nishimoto, K.; Horiuchi, K.; Oguro, S.; Inoue, M.; Yashiro, H.; Nakatsuka, S.; Nakamura, M.; et al. CT guided cryoablation for locally recurrent or metastatic bone and soft tissue tumor: Initial experience. BMC Cancer 2016, 16, 798. [Google Scholar] [CrossRef] [Green Version]
- Bang, H.J.; Littrup, P.J.; Currier, B.P.; Goodrich, D.J.; Aoun, H.D.; Klein, L.C.; Kuo, J.C.; Heilbrun, L.K.; Gadgeel, S.; Goodman, A.C. Percutaneous Cryoablation of Metastatic Lesions from Non–Small-Cell Lung Carcinoma: Initial Survival, Local Control, and Cost Observations. J. Vasc. Interv. Radiol. 2012, 23, 761–769. [Google Scholar] [CrossRef] [Green Version]
- Cazzato, R.L.; Garnon, J.; Ramamurthy, N.; Koch, G.; Tsoumakidou, G.; Caudrelier, J.; Arrigoni, F.; Zugaro, L.; Barile, A.; Masciocchi, C.; et al. Percutaneous image-guided cryoablation: Current applications and results in the oncologic field. Med. Oncol. 2016, 33, 140. [Google Scholar] [CrossRef]
- Gangi, A.; Buy, X. Percutaneous Bone Tumor Management. Semin. Interv. Radiol. 2010, 27, 124–136. [Google Scholar] [CrossRef] [Green Version]
- Bazzocchi, A.; Napoli, A.; Sacconi, B.; Battista, G.; Guglielmi, G.; Catalano, C.; Albisinni, U. MRI-guided focused ultrasound surgery in musculoskeletal diseases: The hot topics. Br. J. Radiol. 2016, 89, 20150358. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Napoli, A.; Anzidei, M.; Marincola, B.C.; Brachetti, G.; Noce, V.; Boni, F.; Bertaccini, L.; Passariello, R.; Catalano, C. MR Imaging–guided Focused Ultrasound for Treatment of Bone Metastasis. Radiographics 2013, 33, 1555–1568. [Google Scholar] [CrossRef]
- Masciocchi, C.; Conchiglia, A.; Gregori, L.M.; Arrigoni, F.; Zugaro, L.; Barile, A. Critical role of HIFU in musculoskeletal interventions. Radiol. Med. 2014, 119, 470–475. [Google Scholar] [CrossRef] [PubMed]
- Liberman, B.; Gianfelice, D.; Inbar, Y.; Beck, A.; Rabin, T.; Shabshin, N.; Chander, G.; Hengst, S.; Pfeffer, R.; Chechick, A.; et al. Pain Palliation in Patients with Bone Metastases Using MR-Guided Focused Ultrasound Surgery: A Multicenter Study. Ann. Surg. Oncol. 2009, 16, 140–146. [Google Scholar] [CrossRef] [PubMed]
- Catane, R.; Beck, A.; Inbar, Y.; Rabin, T.; Shabshin, N.; Hengst, S.; Pfeffer, R.; Hanannel, A.; Dogadkin, O.; Liberman, B.; et al. MR-guided focused ultrasound surgery (MRgFUS) for the palliation of pain in patients with bone metastases—Preliminary clinical experience. Ann. Oncol. Off. J. Eur. Soc. Med. Oncol. 2007, 18, 163–167. [Google Scholar] [CrossRef] [PubMed]
- Masciocchi, C.; Arrigoni, F.; La Marra, A.; Mariani, S.; Zugaro, L.; Barile, A. Treatment of focal benign lesions of the bone: MRgFUS and RFA. Br. J. Radiol. 2016, 89, 20150356. [Google Scholar] [CrossRef] [Green Version]
- Arrigoni, F.; Barile, A.; Zugaro, L.; Splendiani, A.; di Cesare, E.; Caranci, F.; Ierardi, A.M.; Floridi, C.; Angileri, A.S.; Reginelli, A.; et al. Intra-articular benign bone lesions treated with Magnetic Resonance-guided Focused Ultrasound (MRgFUS): Imaging follow-up and clinical results. Med. Oncol. 2017, 34, 55. [Google Scholar] [CrossRef]
- Mercadante, S.; Fulfaro, F. Management of painful bone metastases. Curr. Opin. Oncol. 2007, 19, 308–314. [Google Scholar] [CrossRef]
- Health Quality Ontario. Vertebral Augmentation Involving Vertebroplasty or Kyphoplasty for Cancer-Related Vertebral Compression Fractures: A Systematic Review. Ont. Health Technol. Assess Ser. 2016, 16, 1–34. Available online: https://pubmed.ncbi.nlm.nih.gov/27298655/ (accessed on 20 March 2022).
- Masala, S.; Chiocchi, M.; Taglieri, A.; Bindi, A.; Nezzo, M.; De Vivo, D.; Simonetti, G. Combined use of percutaneous cryoablation and vertebroplasty with 3D rotational angiograph in treatment of single vertebral metastasis: Comparison with vertebroplasty. Neuroradiology 2013, 55, 193–200. [Google Scholar] [CrossRef]
- van der Linden, E.; Kroft, L.J.; Dijkstra, P.S. Treatment of Vertebral Tumor with Posterior Wall Defect Using Image-guided Radiofrequency Ablation Combined with Vertebroplasty: Preliminary Results in 12 Patients. J. Vasc. Interv. Radiol. 2007, 18, 741–747. [Google Scholar] [CrossRef] [PubMed]
- Tsoumakidou, G.; Too, C.W.; Koch, G.; Caudrelier, J.; Cazzato, R.L.; Garnon, J.; Gangi, A. CIRSE Guidelines on Percutaneous Vertebral Augmentation. Cardiovasc. Interv. Radiol. 2017, 40, 331–342. [Google Scholar] [CrossRef] [PubMed]
- Saliou, G.; Kocheida, E.M.; Lehmann, P.; Depriester, C.; Paradot, G.; Le Gars, D.; Balut, A.; Deramond, H. Percutaneous Vertebroplasty for Pain Management in Malignant Fractures of the Spine with Epidural Involvement. Radiology 2010, 254, 882–890. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cazzato, R.L.; Buy, X.; Eker, O.; Fabre, T.; Palussiere, J. Percutaneous long bone cementoplasty of the limbs: Experience with fifty-one non-surgical patients. Eur. Radiol. 2014, 24, 3059–3068. [Google Scholar] [CrossRef] [PubMed]
- Le Clair, A.; Gangi, A.; Lacaze, F.; Javier, R.-M.; Bonidan, O.; Kempf, J.-F.; Bonnomet, F.; Limbach, F.-X.; Kuntz, J.-L.; Dietmann, J.-L.; et al. Rapid chondrolysis after an intra-articular leak of bone cement in treatment of a benign acetabular subchondral cyst: An unusual complication of percutaneous injection of acrylic cement. Skelet. Radiol. 2000, 29, 275–278. [Google Scholar] [CrossRef]
- Kassamali, R.H.; Ganeshan, A.; Hoey, E.T.D.; Crowe, P.M.; Douis, H.; Henderson, J. Pain management in spinal metastases: The role of percutaneous vertebral augmentation. Ann. Oncol. Off. J. Eur. Soc. Med. Oncol. 2011, 22, 782–786. [Google Scholar] [CrossRef]
- Halpin, R.J.; Bendok, B.R.; Sato, K.T.; Liu, J.C.; Patel, J.D.; Rosen, S.T. Combination treatment of vertebral metastases using image-guided percutaneous radiofrequency ablation and vertebroplasty: A case report. Surg. Neurol. 2005, 63, 469–474. [Google Scholar] [CrossRef]
- Schaefer, O.; Lohrmann, C.; Markmiller, M.; Uhrmeister, P.; Langer, M. Combined Treatment of a Spinal Metastasis with Radiofrequency Heat Ablation and Vertebroplasty. Am. J. Roentgenol. 2003, 180, 1075–1077. [Google Scholar] [CrossRef]
- Barragán-Campos, H.M.; Vallée, J.-N.; Lo, D.; Cormier, E.; Jean, B.; Rose, M.; Astagneau, P.; Chiras, J. Percutaneous Vertebroplasty for Spinal Metastases: Complications. Radiology 2006, 238, 354–362. [Google Scholar] [CrossRef]
- Cazzato, R.L.; Koch, G.; Buy, X.; Ramamurthy, N.; Tsoumakidou, G.; Caudrelier, J.; Catena, V.; Garnon, J.; Palussiere, J.; Gangi, A. Percutaneous Image-Guided Screw Fixation of Bone Lesions in Cancer Patients: Double-Centre Analysis of Outcomes including Local Evolution of the Treated Focus. Cardiovasc. Interv. Radiol. 2016, 39, 1455–1463. [Google Scholar] [CrossRef]
- Mirels, H. The Classic: Metastatic Disease in Long Bones A Proposed Scoring System for Diagnosing Impending Pathologic Fractures. Clin. Orthop. Relat. Res. 2003, 415, S4–S13. [Google Scholar] [CrossRef] [PubMed]
- Cazzato, R.L.; Garnon, J.; Tsoumakidou, G.; Koch, G.; Palussière, J.; Gangi, A.; Buy, X. Percutaneous image-guided screws meditated osteosynthesis of impeding and pathological/insufficiency fractures of the femoral neck in non-surgical cancer patients. Eur. J. Radiol. 2017, 90, 1–5. [Google Scholar] [CrossRef] [PubMed]
- Garnon, J.; Koch, G.; Ramamurthy, N.; Caudrelier, J.; Rao, P.; Tsoumakidou, G.; Cazzato, R.L.; Gangi, A. Percutaneous CT and Fluoroscopy-Guided Screw Fixation of Pathological Fractures in the Shoulder Girdle: Technical Report of 3 Cases. Cardiovasc. Interv. Radiol. 2016, 39, 1332–1338. [Google Scholar] [CrossRef] [PubMed]
- Deschamps, F.; de Baere, T.; Hakime, A.; Pearson, E.; Farouil, G.; Teriitehau, C.; Tselikas, L. Percutaneous osteosynthesis in the pelvis in cancer patients. Eur. Radiol. 2016, 26, 1631–1639. [Google Scholar] [CrossRef] [PubMed]
- Gangi, A.; Tsoumakidou, G.; Buy, X.; Quoix, E. Quality Improvement Guidelines for Bone Tumour Management. Cardiovasc. Interv. Radiol. 2010, 33, 706–713. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pusceddu, C.; Sotgia, B.; Fele, R.M.; Melis, L. Treatment of Bone Metastases with Microwave Thermal Ablation. J. Vasc. Interv. Radiol. 2013, 24, 229–233. [Google Scholar] [CrossRef]
- Cazzato, R.L.; De Marini, P.; Leonard-Lorant, I.; Dalili, D.; Koch, G.; Autrusseau, P.A.; Mayer, T.; Weiss, J.; Auloge, P.; Garnon, J.; et al. Percutaneous thermal ablation of sacral metastases: Assessment of pain relief and local tumor control. Diagn. Interv. Imaging 2021, 102, 355–361. [Google Scholar] [CrossRef]
- Ma, Y.; Wallace, A.N.; Waqar, S.N.; Morgensztern, D.; Madaelil, T.P.; Tomasian, A.; Jennings, J.W. Percutaneous Image-Guided Ablation in the Treatment of Osseous Metastases from Non-small Cell Lung Cancer. Cardiovasc. Interv. Radiol. 2018, 41, 726–733. [Google Scholar] [CrossRef]
- Vaswani, D.; Wallace, A.N.; Eiswirth, P.S.; Madaelil, T.P.; Chang, R.O.; Tomasian, A.; Jennings, J.W. Radiographic Local Tumor Control and Pain Palliation of Sarcoma Metastases within the Musculoskeletal System with Percutaneous Thermal Ablation. Cardiovasc. Interv. Radiol. 2018, 41, 1223–1232. [Google Scholar] [CrossRef]
- Erie, A.J.; Morris, J.M.; Welch, B.T.; Kurup, A.N.; Weisbrod, A.J.; Atwell, T.D.; Schmit, G.D.; Kwon, E.D.; Callstrom, M.R. Retrospective Review of Percutaneous Image-Guided Ablation of Oligometastatic Prostate Cancer: A Single-Institution Experience. J. Vasc. Interv. Radiol. 2017, 28, 987–992. [Google Scholar] [CrossRef]
- Aubry, S.; Dubut, J.; Nueffer, J.-P.; Chaigneau, L.; Vidal, C.; Kastler, B. Prospective 1-year follow-up pilot study of CT-guided microwave ablation in the treatment of bone and soft-tissue malignant tumours. Eur. Radiol. 2016, 27, 1477–1485. [Google Scholar] [CrossRef]
- Tomasian, A.; Wallace, A.; Northrup, B.; Hillen, T.; Jennings, J. Spine Cryoablation: Pain Palliation and Local Tumor Control for Vertebral Metastases. AJNR Am. J. Neuroradiol. 2015, 37, 189–195. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Deschamps, F.; Farouil, G.; Ternes, N.; Gaudin, A.; Hakime, A.; Tselikas, L.; Teriitehau, C.; Baudin, E.; Auperin, A.; De Baere, T. Thermal ablation techniques: A curative treatment of bone metastases in selected patients? Eur. Radiol. 2014, 24, 1971–1980. [Google Scholar] [CrossRef]
- McMenomy, B.P.; Kurup, A.N.; Johnson, G.; Carter, R.E.; McWilliams, R.R.; Markovic, S.N.; Atwell, T.D.; Schmit, G.D.; Morris, J.M.; Woodrum, D.A.; et al. Percutaneous Cryoablation of Musculoskeletal Oligometastatic Disease for Complete Remission. J. Vasc. Interv. Radiol. 2013, 24, 207–213. [Google Scholar] [CrossRef] [PubMed]
- Littrup, P.J.; Bang, H.J.; Currier, B.P.; Goodrich, D.J.; Aoun, H.D.; Heilbrun, L.K.; Adam, B.A. Soft-Tissue Cryoablation in Diffuse Locations: Feasibility and Intermediate Term Outcomes. J. Vasc. Interv. Radiol. 2013, 24, 1817–1825. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bang, H.J.; Littrup, P.J.; Goodrich, D.J.; Currier, B.P.; Aoun, H.D.; Heilbrun, L.K.; Vaishampayan, U.; Adam, B.; Goodman, A.C. Percutaneous Cryoablation of Metastatic Renal Cell Carcinoma for Local Tumor Control: Feasibility, Outcomes, and Estimated Cost-effectiveness for Palliation. J. Vasc. Interv. Radiol. 2012, 23, 770–777. [Google Scholar] [CrossRef] [Green Version]
- Arrigoni, F.; Bianchi, G.; Formiconi, F.; Palumbo, P.; Zugaro, L.; Gravina, G.L.; Barile, A.; Masciocchi, C. CT-guided cryoablation for management of bone metastases: A single center experience and review of the literature. Radiol. Med. 2022, 127, 199–205. [Google Scholar] [CrossRef]
- Jennings, J.W.; Prologo, J.D.; Garnon, J.; Gangi, A.; Buy, X.; Palussière, J.; Kurup, A.N.; Callstrom, M.; Genshaft, S.; Abtin, F.; et al. Cryoablation for Palliation of Painful Bone Metastases: The Motion Multicenter Study. Radiol. Imaging Cancer 2021, 3, 16–18. [Google Scholar] [CrossRef]
- Madani, K.; Najafi, A.; Boticella, A.; Roux, C.; Tselikas, L.; Delpla, A.; Al Ahmar, M.; de Baere, T.; Deschamps, F. Combined local treatments for vertebral metastases with limited epidural extension. Support. Care Cancer 2022, 30, 337–345. [Google Scholar] [CrossRef]
- Kastler, A.; Barbé, D.-A.; Alemann, G.; Hadjidekov, G.; Cornelis, F.H.; Kastler, B. Bipolar Radiofrequency Ablation of Painful Spinal Bone Metastases Performed under Local Anesthesia: Feasibility Regarding Patient’s Experience and Pain Outcome. Medicina 2021, 57, 966. [Google Scholar] [CrossRef]
- Pusceddu, C.; De Francesco, D.; Melis, L.; Ballicu, N.; Fancellu, A. The Role of a Navigational Radiofrequency Ablation Device and Concurrent Vertebral Augmentation for Treatment of Difficult-to-Reach Spinal Metastases. Curr. Oncol. 2021, 28, 4004–4015. [Google Scholar] [CrossRef] [PubMed]
- Yang, Y.; Li, Y.; Wu, Y.; Qiu, S.; Liu, C.; Wang, Q.; Hong, Y.; Lyu, J.; Zhang, Y.; Du, D. Retrospective analysis of CT-guided percutaneous cryoablation for treatment of painful osteolytic bone metastasis. Cryobiology 2020, 92, 203–207. [Google Scholar] [CrossRef] [PubMed]
- Yang, X.-G.; Wu, G.; Sun, Y.-Y.; Pang, H.-R.; Huang, X.-Q.; Xu, G.-H. Vesselplasty using the Mesh-Hold™ bone-filling container for the treatment of pathological vertebral fractures due to osteolytic metastases: A retrospective study. Eur. J. Radiol. 2020, 126, 108962. [Google Scholar] [CrossRef] [PubMed]
- De Marini, P.; Cazzato, R.L.; Auloge, P.; Koch, G.; Dalili, D.; Garnon, J.; Gangi, A. Percutaneous image-guided thermal ablation of bone metastases: A retrospective propensity study comparing the safety profile of radio-frequency ablation and cryo-ablation. Int. J. Hyperth. 2020, 37, 1386–1394. [Google Scholar] [CrossRef]
- Deib, G.; Deldar, B.; Hui, F.; Barr, J.S.; Khan, M.A. Percutaneous Microwave Ablation and Cementoplasty: Clinical Utility in the Treatment of Painful Extraspinal Osseous Metastatic Disease and Myeloma. AJR Am. J. Roentgenol. 2019, 212, 1377–1384. [Google Scholar] [CrossRef]
- Tanigawa, N.; Arai, Y.; Yamakado, K.; Aramaki, T.; Inaba, Y.; Kanazawa, S.; Matsui, O.; Miyazaki, M.; Kodama, Y.; Anai, H.; et al. Phase I/II Study of Radiofrequency Ablation for Painful Bone Metastases: Japan Interventional Radiology in Oncology Study Group. Cardiovasc. Interv. Radiol. 2018, 41, 1043–1048. [Google Scholar] [CrossRef]
- Prologo, J.D.; Passalacqua, M.; Patel, I.; Bohnert, N.; Corn, D. Image-guided cryoablation for the treatment of painful musculoskeletal metastatic disease: A single-center experience. Skelet. Radiol. 2014, 43, 1551–1559. [Google Scholar] [CrossRef]
- Rossi, G.; Mavrogenis, A.F.; Casadei, R.; Bianchi, G.; Romagnoli, C.; Rimondi, E.; Ruggieri, P. Embolisation of bone metastases from renal cancer. Radiol. Med. 2013, 118, 291–302. [Google Scholar] [CrossRef]
- Campanacci, L.; Bianchi, G.; Cevolani, L.; Errani, C.; Ciani, G.; Facchini, G.; Spinnato, P.; Tognù, A.; Massari, L.; Cornelis, F.H.; et al. Operating procedures for electrochemotherapy in bone metastases: Results from a multicenter prospective study on 102 patients. Eur. J. Surg. Oncol. (EJSO) 2021, 47, 2609–2617. [Google Scholar] [CrossRef]
- Koirala, N.; McLennan, G. Percutaneous reinforced osteoplasty for long bone metastases: A feasibility study. Skelet. Radiol. 2019, 49, 375–382. [Google Scholar] [CrossRef]
- Giles, S.L.; Brown, M.R.; Rivens, I.; Deppe, M.; Huisman, M.; Kim, Y.-S.; Farquhar-Smith, P.; Williams, J.E.; ter Haar, G.R.; Desouza, N.M. Comparison of Imaging Changes and Pain Responses in Patients with Intra- or Extraosseous Bone Metastases Treated Palliatively with Magnetic Resonance-Guided High-Intensity–Focused Ultrasound. J. Vasc. Interv. Radiol. 2019, 30, 1351–1360.e1. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sundararajan, S.H.; Calamita, S.; Girgis, P.; Ngo, G.; Ranganathan, S.; Giglio, M.; Gendel, V.; Goyal, S.; Nosher, J.; Roychowdhury, S. Sequential Interventional Management of Osseous Neoplasms via Embolization, Cryoablation, and Osteoplasty. J. Oncol. 2019, 2019, 5247837. [Google Scholar] [CrossRef] [PubMed]
- Tian, Q.-H.; Liu, H.-F.; Wang, T.; Cheng, Y.-S.; Wu, C.-G. Percutaneous Sacroplasty for Painful Sacral Metastases Involving Multiple Sacral Vertebral Bodies: Initial Experience with an Interpedicular Approach. Korean J. Radiol. 2019, 20, 939–946. [Google Scholar] [CrossRef] [PubMed]
- Liu, H.-F.; Wu, C.-G.; Tian, Q.-H.; Wang, T.; Yi, F. Application of Percutaneous Osteoplasty in Treating Pelvic Bone Metastases: Efficacy and Safety. Cardiovasc. Interv. Radiol. 2019, 42, 1738–1744. [Google Scholar] [CrossRef]
- Cazzato, R.L.; Garnon, J.; Caudrelier, J.; Rao, P.P.; Koch, G.; Gangi, A. Low-power bipolar radiofrequency ablation and vertebral augmentation for the palliative treatment of spinal malignancies. Int. J. Hyperth. 2018, 34, 1282–1288. [Google Scholar] [CrossRef] [Green Version]
- Chen, Z.-Q.; Wang, C.-R.; Ma, X.-J.; Sun, W.; Shen, J.-K.; Sun, M.-X.; Fu, Z.-Z.; Hua, Y.-Q.; Cai, Z.-D. Evaluation of Quality of Life Using EORTC QLQ-BM22 in Patients with Bone Metastases after Treatment with Magnetic Resonance Guided Focused Ultrasound. Orthop. Surg. 2018, 10, 264–271. [Google Scholar] [CrossRef]
- Khan, M.; Deib, G.; Deldar, B.; Patel, A.; Barr, J. Efficacy and Safety of Percutaneous Microwave Ablation and Cementoplasty in the Treatment of Painful Spinal Metastases and Myeloma. AJNR Am. J. Neuroradiol. 2018, 39, 1376–1383. [Google Scholar] [CrossRef]
- Couraud, G.; Gaston, A.-P.; Thuillier, T.; Eymard, F.; Hourdille, A.; Chevalier, X.-J.; Boussion, H.; Guignard, S. Evaluation of short-term efficacy of extraspinal cementoplasty for bone metastasis: A monocenter study of 31 patients. J. Bone Oncol. 2018, 13, 136–142. [Google Scholar] [CrossRef]
- Fares, A.; Shaaban, M.H.; Reyad, R.M.; Ragab, A.S.; Sami, M.A. Combined percutaneous radiofrequency ablation and cementoplasty for the treatment of extraspinal painful bone metastases: A prospective study. J. Egypt. Natl. Cancer Inst. 2018, 30, 117–122. [Google Scholar] [CrossRef]
- Bertrand, A.-S.; Iannessi, A.; Natale, R.; Beaumont, H.; Patriti, S.; Xiong-Ying, J.; Baudin, G.; Thyss, A. Focused ultrasound for the treatment of bone metastases: Effectiveness and feasibility. J. Ther. Ultrasound 2018, 6, 8. [Google Scholar] [CrossRef]
- Coupal, T.M.; Pennycooke, K.; I Mallinson, P.; A Ouellette, H.; Clarkson, P.W.; Hawley, P.; Munk, P.L. The Hopeless Case? Palliative Cryoablation and Cementoplasty Procedures for Palliation of Large Pelvic Bone Metastases. Pain Physician 2017, 20, E1053–E1061. [Google Scholar] [CrossRef] [PubMed]
- Pusceddu, C.; Fancellu, A.; Ballicu, N.; Fele, R.M.; Sotgia, B.; Melis, L. CT-guided percutaneous screw fixation plus cementoplasty in the treatment of painful bone metastases with fractures or a high risk of pathological fracture. Skelet. Radiol. 2017, 46, 539–545. [Google Scholar] [CrossRef] [PubMed]
- Reyad, R.; Ghobrial, H.; Hakim, S.; Hashem, R.; Elsaman, A.; Shaaban, M. Thick cement usage in percutaneous vertebroplasty for malignant vertebral fractures at high risk for cement leakage. Diagn. Interv. Imaging 2017, 98, 721–728. [Google Scholar] [CrossRef] [PubMed]
- Motta, A.; Caltabiano, G.; Palmucci, S.; Failla, G.; Basile, A. Feasibility of percutaneous cryoablation of vertebral metastases under local anaesthesia in ASAIII patients. Eur. J. Radiol. 2017, 95, 13–17. [Google Scholar] [CrossRef]
- McArthur, T.A.; Narducci, C.A.; Lander, P.H.; Lopez-Ben, R. Percutane Image-Guided Cryoablation of Painful Osseous Metastases: A Retrospective Single-Center Review. Curr. Probl. Diagn. Radiol. 2017, 46, 282–287. [Google Scholar] [CrossRef]
- Bagla, S.; Sayed, D.; Smirniotopoulos, J.; Brower, J.; Rutledge, J.N.; Dick, B.; Carlisle, J.; Lekht, I.; Georgy, B. Multicenter Prospective Clinical Series Evaluating Radiofrequency Ablation in the Treatment of Painful Spine Metastases. Cardiovasc. Interv. Radiol. 2016, 39, 1289–1297. [Google Scholar] [CrossRef]
- Facchini, G.; Di Tullio, P.; Battaglia, M.; Bartalena, T.; Tetta, C.; Errani, C.; Mavrogenis, A.F.; Rossi, G. Palliative embolization for metastases of the spine. Eur. J. Orthop. Surg. Traumatol. 2015, 26, 247–252. [Google Scholar] [CrossRef]
- Pusceddu, C.; Sotgia, B.; Fele, R.M.; Ballicu, N.; Melis, L. Combined Microwave Ablation and Cementoplasty in Patients with Painful Bone Metastases at High Risk of Fracture. Cardiovasc. Interv. Radiol. 2015, 39, 74–80. [Google Scholar] [CrossRef]
- Anzidei, M.; Napoli, A.; Sacconi, B.; Boni, F.; Noce, V.; Di Martino, M.; Saba, L.; Catalano, C. Magnetic resonance-guided focused ultrasound for the treatment of painful bone metastases: Role of apparent diffusion coefficient (ADC) and dynamic contrast enhanced (DCE) MRI in the assessment of clinical outcome. Radiol. Med. 2016, 121, 905–915. [Google Scholar] [CrossRef]
- Wang, F.A.; He, S.C.; Xiao, E.H.; Wang, S.X.; Sun, L.; Lv, P.H.; Huang, W.N. Sequential Transarterial Embolization Followed by Percu-taneous Vertebroplasty Is Safe and Effective in Pain Management in Vertebral Metastases. Pain Physician 2016, 19, E559–E567. [Google Scholar]
- Chen, F.; Xia, Y.-H.; Cao, W.-Z.; Shan, W.; Gao, Y.; Feng, C.; Wang, D. Percutaneous kyphoplasty for the treatment of spinal metastases. Oncol. Lett. 2016, 11, 1799–1806. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bianchi, G.; Campanacci, L.; Ronchetti, M.; Donati, D.M. Electrochemotherapy in the Treatment of Bone Metastases: A Phase II Trial. World J. Surg. 2016, 40, 3088–3094. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jiao, D.; Wu, G.; Ren, J.; Han, X. Radiofrequency ablation versus 125I-seed brachytherapy for painful metastases involving the bone. Oncotarget 2016, 7, 87523–87531. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Joo, B.; Park, M.-S.; Lee, S.H.; Choi, H.J.; Lim, S.T.; Rha, S.Y.; Rachmilevitch, I.; Lee, Y.H.; Suh, J.-S. Pain Palliation in Patients with Bone Metastases Using Magnetic Resonance-Guided Focused Ultrasound with Conformal Bone System: A Preliminary Report. Yonsei Med. J. 2015, 56, 503–509. [Google Scholar] [CrossRef] [Green Version]
- Wallace, A.N.; Greenwood, T.J.; Jennings, J.W. Radiofrequency ablation and vertebral augmentation for palliation of painful spinal metastases. J. Neuro-Oncol. 2015, 124, 111–118. [Google Scholar] [CrossRef]
- Wei, Z.; Zhang, K.; Ye, X.; Yang, X.; Zheng, A.; Huang, G.; Wang, J. Computed tomography-guided percutaneous microwave ablation combined with osteoplasty for palliative treatment of painful extraspinal bone metastases from lung cancer. Skelet. Radiol. 2015, 44, 1485–1490. [Google Scholar] [CrossRef]
- Di Staso, M.; Gravina, G.L.; Zugaro, L.; Bonfili, P.; Gregori, L.; Franzese, P.; Marampon, F.; Vittorini, F.; Moro, R.; Tombolini, V.; et al. Treatment of Solitary Painful Osseous Metastases with Radiotherapy, Cryoablation or Combined Therapy: Propensity Matching Analysis in 175 Patients. PLoS ONE 2015, 10, e0129021. [Google Scholar] [CrossRef] [Green Version]
- Cazzato, R.; Bonichon, F.; Buy, X.; Godbert, Y.; de Figuereido, B.; Pointillart, V.; Palussière, J. Over ten years of single-institution experience in percutaneous image-guided treatment of bone metastases from differentiated thyroid cancer. Eur. J. Surg. Oncol. (EJSO) 2015, 41, 1247–1255. [Google Scholar] [CrossRef]
- Tian, Q.-H.; Wu, C.-G.; Gu, Y.-F.; He, C.-J.; Li, M.-H.; Cheng, Y.-D. Combination Radiofrequency Ablation and Percutaneous Osteoplasty for Palliative Treatment of Painful Extraspinal Bone Metastasis: A Single-Center Experience. J. Vasc. Interv. Radiol. 2014, 25, 1094–1100. [Google Scholar] [CrossRef]
- Kastler, A.; Alnassan, H.; Aubry, S.; Kastler, B. Microwave Thermal Ablation of Spinal Metastatic Bone Tumors. J. Vasc. Interv. Radiol. 2014, 25, 1470–1475. [Google Scholar] [CrossRef]
- Hurwitz, M.D.; Ghanouni, P.; Kanaev, S.V.; Iozeffi, D.; Gianfelice, D.; Fennessy, F.M.; Kuten, A.; Meyer, J.E.; LeBlang, S.D.; Roberts, A.; et al. Magnetic Resonance–Guided Focused Ultrasound for Patients with Painful Bone Metastases: Phase III Trial Results. JNCI J. Natl. Cancer Inst. 2014, 106, dju082. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Alemann, G.; Kastler, A.; Barbé, D.-A.; Aubry, S.; Kastler, B. Treatment of Painful Extraspinal Bone Metastases with Percutaneous Bipolar Radiofrequency Under Local Anesthesia: Feasibility and Efficacy in Twenty-Eight Cases. J. Palliat. Med. 2014, 17, 947–952. [Google Scholar] [CrossRef] [PubMed]
- Botsa, E.; Mylona, S.; Koutsogiannis, I.; Koundouraki, A.; Thanos, L. CT image guided thermal ablation techniques for palliation of painful bone metastases. Ann. Palliat. Med. 2014, 3, 47–53. [Google Scholar] [CrossRef] [PubMed]
- Li, Z.; Ni, C.; Chen, L.; Sun, Z.; Yang, C.; Zhao, X.; Wang, Y. Kyphoplasty versus vertebroplasty for the treatment of malignant ver-tebral compression fractures caused by metastases: A retrospective study. Chin. Med. J. 2014, 127, 1493–1496. [Google Scholar]
- Li, F.; Wang, W.; Li, L.; Chang, Y.; Su, D.; Guo, G.; He, X.; Li, M. An Effective Therapy to Painful Bone Metastases: Cryoablation Combined with Zoledronic Acid. Pathol. Oncol. Res. 2014, 20, 885–891. [Google Scholar] [CrossRef]
- Sun, G.; Jin, P.; Liu, X.-W.; Li, M.; Li, L. Cementoplasty for managing painful bone metastases outside the spine. Eur. Radiol. 2014, 24, 731–737. [Google Scholar] [CrossRef]
- Callstrom, M.R.; Dupuy, D.; Solomon, S.B.; Beres, R.A.; Littrup, P.J.; Davis, K.W.; Paz-Fumagalli, R.; Hoffman, C.; Atwell, T.D.; Charboneau, J.W.; et al. Percutaneous image-guided cryoablation of painful metastases involving bone. Cancer 2012, 119, 1033–1041. [Google Scholar] [CrossRef] [Green Version]
- Napoli, A.; Anzidei, M.; Marincola, B.C.; Brachetti, G.; Ciolina, F.; Cartocci, G.; Marsecano, C.; Zaccagna, F.; Marchetti, L.; Cortesi, E.; et al. Primary Pain Palliation and Local Tumor Control in Bone Metastases Treated with Magnetic Resonance-Guided Focused Ultrasound. Investig. Radiol. 2013, 48, 351–358. [Google Scholar] [CrossRef]
- Anselmetti, G.C.; Manca, A.; Tutton, S.; Chiara, G.; Kelekis, A.; Facchini, F.R.; Russo, F.; Regge, D.; Montemurro, F. Percutaneous verte-bral augmentation assisted by PEEK implant in painful osteolytic vertebral metastasis involving the vertebral wall: Experience on 40 patients. Pain Physician 2013, 16, E397–E404. [Google Scholar] [CrossRef]
- Trumm, C.G.; Jakobs, T.F.; Stahl, R.; Sandner, T.A.; Paprottka, P.M.; Reiser, M.F.; Zech, C.J.; Hoffmann, R.-T. CT fluoroscopy-guided vertebral augmentation with a radiofrequency-induced, high-viscosity bone cement (StabiliT®): Technical results and polymethylmethacrylate leakages in 25 patients. Skelet. Radiol. 2012, 42, 113–120. [Google Scholar] [CrossRef]
- Kastler, A.; Alnassan, H.; Pereira, P.L.; Alemann, G.; Barbé, D.-A.; Aubry, S.; Tiberghien, F.; Kastler, B. Analgesic Effects of Microwave Ablation of Bone and Soft Tissue Tumors under Local Anesthesia. Pain Med. 2013, 14, 1873–1881. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Iannessi, A.; Amoretti, N.; Marcy, P.-Y.; Sedat, J. Percutaneous cementoplasty for the treatment of extraspinal painful bone lesion, a prospective study. Diagn. Interv. Imaging 2012, 93, 859–870. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rossi, G.; Mavrogenis, A.F.; Rimondi, E.; Ciccarese, F.; Tranfaglia, C.; Angelelli, B.; Fiorentini, G.; Bartalena, T.; Errani, C.; Ruggieri, P.; et al. Selective arterial embolisation for bone tumours: Experience of 454 cases. Radiol. Med. 2011, 116, 793–808. [Google Scholar] [CrossRef] [PubMed]
- Masala, S.A.; Guglielmi, G.; Petrella, M.C.; Mastrangeli, R.; Meschini, A.; Anselmetti, G.C.; A Bartolucci, D.; Mammucari, M.; Manenti, G.; Simonetti, G. Percutaneous ablative treatment of metastatic bone tumours: Visual analogue scale scores in a short-term series. Singap. Med. J. 2011, 52, 182–189. [Google Scholar]
- Masala, S.; Schillaci, O.; Bartolucci, A.D.; Calabria, F.; Mammucari, M.; Simonetti, G. Metabolic and clinical assessment of efficacy of cryoablation therapy on skeletal masses by 18F-FDG positron emission tomography/computed tomography (PET/CT) and visual analogue scale (VAS): Initial experience. Skelet. Radiol. 2010, 40, 159–165. [Google Scholar] [CrossRef]
- Masala, S.A.; Volpi, T.; Fucci, F.P.M.; Cantonetti, M.; Postorino, M.; Simonetti, G. Percutaneus osteoplasty in the treatment of extraspinal painful multiple myeloma lesions. Support. Care Cancer 2010, 19, 957–962. [Google Scholar] [CrossRef]
- Kashima, M.; Yamakado, K.; Takaki, H.; Kaminou, T.; Tanigawa, N.; Nakatsuka, A.; Takeda, K. Radiofrequency Ablation for the Treatment of Bone Metastases from Hepatocellular Carcinoma. AJR Am. J. Roentgenol. 2010, 194, 536–541. [Google Scholar] [CrossRef]
- Carrafiello, G.; Laganà, D.; Pellegrino, C.; Fontana, F.; Mangini, M.; Nicotera, P.; Petullà, M.; Bracchi, E.; Genovese, E.; Cuffari, S.; et al. Percutaneous imaging-guided ablation therapies in the treatment of symptomatic bone metastases: Preliminary experience. Radiol. Med. 2009, 114, 608–625. [Google Scholar] [CrossRef]
- Delpla, A.; Tselikas, L.; De Baere, T.; Laurent, S.; Mezaib, K.; Barat, M.; Nguimbous, O.; Prudhomme, C.; Al-Hamar, M.; Moulin, B.; et al. Preventive Vertebroplasty for Long-Term Consolidation of Vertebral Metastases. Cardiovasc. Interv. Radiol. 2019, 42, 1726–1737. [Google Scholar] [CrossRef]
- Thanos, L.; Mylona, S.; Galani, P.; Tzavoulis, D.; Kalioras, V.; Tanteles, S.; Pomoni, M. Radiofrequency ablation of osseous metastases for the palliation of pain. Skelet. Radiol. 2008, 37, 189–194. [Google Scholar] [CrossRef] [Green Version]
- Gianfelice, D.; Gupta, C.; Kucharczyk, W.; Bret, P.; Havill, D.; Clemons, M. Palliative Treatment of Painful Bone Metastases with MR Imaging–guided Focused Ultrasound. Radiology 2008, 249, 355–363. [Google Scholar] [CrossRef] [PubMed]
- Basile, A.; Giuliano, G.; Scuderi, V.; Motta, S.; Crisafi, R.; Coppolino, F.; Mundo, E.; Banna, G.L.; Di Raimondo, F.; Patti, M.T.; et al. Cementoplasty in the management of painful extraspinal bone metastases: Our experience. Radiol. Med. 2008, 113, 1018–1028. [Google Scholar] [CrossRef] [PubMed]
- Anselmetti, G.C.; Manca, A.; Ortega, C.; Grignani, G.; DeBernardi, F.; Regge, D. Treatment of Extraspinal Painful Bone Metastases with Percutaneous Cementoplasty: A Prospective Study of 50 Patients. Cardiovasc. Interv. Radiol. 2008, 31, 1165–1173. [Google Scholar] [CrossRef]
- Trumm, C.G.; Jakobs, T.F.; Zech, C.J.; Helmberger, T.K.; Reiser, M.F.; Hoffmann, R.-T. CT Fluoroscopy–guided Percutaneous Vertebroplasty for the Treatment of Osteolytic Breast Cancer Metastases: Results in 62 Sessions with 86 Vertebrae Treated. J. Vasc. Interv. Radiol. 2008, 19, 1596–1606. [Google Scholar] [CrossRef]
- Tuncali, K.; Morrison, P.R.; Winalski, C.S.; Carrino, J.A.; Shankar, S.; Ready, J.E.; Vansonnenberg, E.; Silverman, S.G. MRI-Guided Percutaneous Cryotherapy for Soft-Tissue and Bone Metastases: Initial Experience. AJR Am. J. Roentgenol. 2007, 189, 232–239. [Google Scholar] [CrossRef] [PubMed]
- Forauer, A.R.; Kent, E.; Cwikiel, W.; Esper, P.; Redman, B. Selective palliative transcatheter embolization of bony metastases from renal cell carcinoma. Acta Oncol. 2007, 46, 1012–1018. [Google Scholar] [CrossRef] [PubMed]
- Callstrom, M.R.; Atwell, T.D.; Charboneau, J.W.; Farrell, M.A.; Goetz, M.P.; Rubin, J.; Sloan, J.A.; Novotny, P.J.; Welch, T.J.; Maus, T.P.; et al. Painful Metastases Involving Bone: Percutaneous Image-guided Cryoablation—Prospective Trial Interim Analysis. Radiology 2006, 241, 572–580. [Google Scholar] [CrossRef]
- Weber, C.H.; Krötz, M.; Hoffmann, R.-T.; Euler, E.; Heining, S.; Pfeifer, K.-J.; Reiser, M.; Linsenmaier, U. CT-gesteuerte Vertebro- und Kyphoplastie: Vergleichende Untersuchung zu technischem Erfolg und Komplikationen bei 101 Eingriffen [CT-guided vertebroplasty and kyphoplasty: Comparing technical success rate and complications in 101 cases]. Rofo 2006, 178, 610–617. [Google Scholar] [CrossRef]
- Callstrom, M.R.; Charboneau, J.W. Percutaneous ablation: Safe, effective treatment of bone tumors. Oncology 2005, 19 (Suppl. S4), 22–26. [Google Scholar]
- Cai, H.-Y.; Liu, X.-D.; Cao, H.-P.; Wang, X.-Q.; Zhang, Z.-Y.; Dong, X.-C. Treatment effect of percutaneous vertebroplasty combined with interventional chemotherapy on vertebral metastases. Ai Zheng 2005, 24, 488–493. [Google Scholar]
- Masala, S.; Schillaci, O.; Massari, F.; Danieli, R.; Ursone, A.; Fiori, R.; Simonetti, G. MRI and bone scan imaging in the preoperative evaluation of painful vertebral fractures treated with ver-tebroplasty and kyphoplasty. In Vivo 2005, 19, 1055–1060. [Google Scholar] [PubMed]
- Guzman, R.; Dubach-Schwizer, S.; Heini, P.; Lovblad, K.-O.; Kalbermatten, D.F.; Schroth, G.; Remonda, L. Preoperative transarterial embolization of vertebral metastases. Eur. Spine J. 2004, 14, 263–268. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Masala, S.; Lunardi, P.; Fiori, R.; Liccardo, G.; Massari, F.; Ursone, A.; Simonetti, G. Vertebroplasty and Kyphoplasty in the Treatment of Malignant Vertebral Fractures. J. Chemother. 2004, 16, 30–33. [Google Scholar] [CrossRef] [PubMed]
- Poggi, G.; Gatti, C.; Melazzini, M.G.; Bernardo, G.; Strada, M.; Teragni, C.; Delmonte, A.; Tagliaferri, C.; Bonezzi, C.; Barbieri, M.; et al. Percutaneous ultrasound-guided radiofrequency thermal ablation of malignant osteolyses. Anticancer Res. 2004, 23, 4977–4983. [Google Scholar]
- Eustatia-Rutten, C.F.A.; Romijn, J.A.; Guijt, M.J.; Vielvoye, G.J.; Berg, R.V.D.; Corssmit, E.P.M.; Pereira, A.M.; Smit, J.W.A. Outcome of Palliative Embolization of Bone Metastases in Differentiated Thyroid Carcinoma. J. Clin. Endocrinol. Metab. 2003, 88, 3184–3189. [Google Scholar] [CrossRef]
- Fourney, D.R.; Schomer, D.F.; Nader, R.; Chlan-Fourney, J.; Suki, D.; Ahrar, K.; Rhines, L.D.; Gokaslan, Z.L. Percutaneous vertebroplasty and kyphoplasty for painful vertebral body fractures in cancer patients. J. Neurosurg. Spine 2003, 98, 21–30. [Google Scholar] [CrossRef]
- Winking, M.; Stahl, J.P.; Oertel, M.; Schnettler, R.; Böker, D.K. PMMA vertebroplasty in patients with malignant vertebral destruc-tion of the thoracic and lumbar spine. Ger. Med. Sci. 2003, 1, Doc08. [Google Scholar]
- Alvarez, L.; Calvo, E.; Rossi, R.E. Vertebroplasty in the treatment of vertebral tumors: Postprocedural outcome and quality of life. Eur. Spine J. 2003, 12, 356–360. [Google Scholar] [CrossRef] [Green Version]
- Hierholzer, J.; Anselmetti, G.; Fuchs, H.; Depriester, C.; Koch, K.; Pappert, D. Percutaneous Osteoplasty as a Treatment for Painful Malignant Bone Lesions of the Pelvis and Femur. J. Vasc. Interv. Radiol. 2003, 14, 773–777. [Google Scholar] [CrossRef]
- Grönemeyer, D.H.; Schirp, S.; Gevargez, A. Image-Guided Radiofrequency Ablation of Spinal Tumors: Preliminary experience with an expandable array electrode. Cancer J. 2002, 8, 33–39. [Google Scholar] [CrossRef] [Green Version]
- Chatziioannou, A.N.; Johnson, M.E.; Pneumaticos, S.G.; Lawrence, D.D.; Carrasco, C.H. Preoperative embolization of bone metastases from renal cell carcinoma. Eur. Radiol. 2000, 10, 593–596. [Google Scholar] [CrossRef] [PubMed]
- Barr, J.D.; Barr, M.S.; Lemley, T.J.; McCann, R.M. Percutaneous Vertebroplasty for Pain Relief and Spinal Stabilization. Spine 2000, 25, 923–928. [Google Scholar] [CrossRef] [PubMed]
- Martin, J.; Jean, B.; Sugiu, K.; Ruíz, D.S.M.; Piotin, M.; Murphy, K.; Rüfenacht, B.; Muster, M.; Rüfenacht, D. Vertebroplasty: Clinical experience and follow-up results. Bone 1999, 25 (Suppl. S2), 11S–15S. [Google Scholar] [CrossRef]
- Sun, S.; Lang, E.V. Bone Metastases from Renal Cell Carcinoma: Preoperative Embolization. J. Vasc. Interv. Radiol. 1998, 9, 263–269. [Google Scholar] [CrossRef]
- Weill, A.; Chiras, J.; Simon, J.M.; Rose, M.; Sola-Martinez, T.; Enkaoua, E. Spinal metastases: Indications for and results of percutaneous injection of acrylic surgical cement. Radiology 1996, 199, 241–247. [Google Scholar] [CrossRef]
- Cotten, A.; Dewatre, F.; Cortet, B.; Assaker, R.; Leblond, D.; Duquesnoy, B.; Chastanet, P.; Clarisse, J. Percutaneous vertebroplasty for osteolytic metastases and myeloma: Effects of the percentage of lesion filling and the leakage of methyl methacrylate at clinical follow-up. Radiology 1996, 200, 525–530. [Google Scholar] [CrossRef]
- Breslau, J.; Eskridge, J.M. Preoperative Embolization of Spinal Tumors. J. Vasc. Interv. Radiol. 1995, 6, 871–875. [Google Scholar] [CrossRef]
- Corcos, G.; Dbjay, J.; Mastier, C.; Leon, S.; Auperin, A.; De Baere, T.; Deschamps, F. Cement Leakage in Percutaneous Vertebroplasty for Spinal Metastases: A retrospective evaluation of incidence and risk factors. Spine 2014, 39, E332–E338. [Google Scholar] [CrossRef]
- Nakatsuka, A.; Yamakado, K.; Uraki, J.; Takaki, H.; Yamanaka, T.; Fujimori, M.; Hasegawa, T.; Sakuma, H. Safety and Clinical Outcomes of Percutaneous Radiofrequency Ablation for Intermediate and Large Bone Tumors Using a Multiple-Electrode Switching System: A Phase II Clinical Study. J. Vasc. Interv. Radiol. 2016, 27, 388–394. [Google Scholar] [CrossRef]
- Yu, W.; Tang, L.; Lin, F.; Yao, Y.; Shen, Z.; Zhou, X. High-intensity focused ultrasound: Noninvasive treatment for local unresectable recurrence of osteosarcoma. Surg. Oncol. 2015, 24, 9–15. [Google Scholar] [CrossRef]
- Anselmetti, G.C.; Manca, A.; Montemurro, F.; Hirsch, J.; Chiara, G.; Grignani, G.; Schianca, F.C.; Capaldi, A.; Scalabrini, D.R.; Sardo, E.; et al. Percutaneous Vertebroplasty in Multiple Myeloma: Prospective Long-Term Follow-Up in 106 Consecutive Patients. Cardiovasc. Interv. Radiol. 2012, 35, 139–145. [Google Scholar] [CrossRef] [PubMed]
- Li, C.; Zhang, W.; Fan, W.; Huang, J.; Zhang, F.; Wu, P. Noninvasive treatment of malignant bone tumors using high-intensity focused ultrasound. Cancer 2010, 116, 3934–3942. [Google Scholar] [CrossRef] [PubMed]
- Kim, N.J.; Kim, T.W.; Park, K.H.; Chi, M.P.; O Kim, J. The Proper Volume and Distribution of Cement Augmentation on Percutaneous Vertebroplasty. J. Korean Neurosurg. Soc. 2010, 48, 125–128. [Google Scholar] [CrossRef] [PubMed]
- Chevalier, Y.; Pahr, D.; Charlebois, M.; Heini, P.; Schneider, E.; Zysset, P. Cement Distribution, Volume, and Compliance in Vertebroplasty: Some answers from an anatomy-based nonlinear finite element study. Spine 2008, 33, 1722–1730. [Google Scholar] [CrossRef] [PubMed]
- Laredo, J.-D.; Hamze, B. Complications of percutaneous vertebroplasty and their prevention. Semin. Ultrasound CT MRI 2005, 26, 65–80. [Google Scholar] [CrossRef]
- Shimony, J.S.; Gilula, L.A.; Zeller, A.J.; Brown, D.B. Percutaneous Vertebroplasty for Malignant Compression Fractures with Epidural Involvement. Radiology 2004, 232, 846–853. [Google Scholar] [CrossRef] [PubMed]
- Johnstone, C.; Lutz, S.T. External beam radiotherapy and bone metastases. Ann. Palliat. Med. 2014, 3, 175–185. [Google Scholar] [CrossRef]
- Steenland, E.; Leer, J.; van Houwelingen, H.C.; Post, W.J.; Hout, W.B.V.D.; Kievit, J.; de Haes, H.; Martijn, H.; Oei, B.; Vonk, E.; et al. The effect of a single fraction compared to multiple fractions on painful bone metastases: A global analysis of the Dutch Bone Metastasis Study. Radiother. Oncol. 1999, 52, 101–109. [Google Scholar] [CrossRef]
- De Felice, F.; Piccioli, A.; Musio, D.; Tombolini, V. The role of radiation therapy in bone metastases management. Oncotarget 2017, 8, 25691–25699. [Google Scholar] [CrossRef] [Green Version]
- Huisman, M.; Bosch, M.A.V.D.; Wijlemans, J.W.; van Vulpen, M.; van der Linden, Y.; Verkooijen, H.M. Effectiveness of Reirradiation for Painful Bone Metastases: A Systematic Review and Meta-Analysis. Int. J. Radiat. Oncol. Biol. Phys. 2012, 84, 8–14. [Google Scholar] [CrossRef]
- Harvey, N.; Ahlmann, E.R.; Allison, D.C.; Wang, L.; Menendez, L.R. Endoprostheses Last Longer Than Intramedullary Devices in Proximal Femur Metastases. Clin. Orthop. Relat. Res. 2012, 470, 684–691. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Potter, B.K.; Chow, V.E.; Adams, S.C.; Letson, G.D.; Temple, H.T. Endoprosthetic proximal femur replacement: Metastatic versus primary tumors. Surg. Oncol. 2009, 18, 343–349. [Google Scholar] [CrossRef] [PubMed]
- Capanna, R.; De Biase, P.; Sensi, L. Minimally invasive techniques for treatment of metastatic cancer. Orthopade 2009, 38, 343–347. [Google Scholar] [CrossRef] [PubMed]
- Carrafiello, G.; Laganà, D.; Pellegrino, C.; Mangini, M.; Fontana, F.; Piacentino, F.; Recaldini, C.; Rovera, F.; Dionigi, G.; Boni, L.; et al. Ablation of painful metastatic bone tumors: A systematic review. Int. J. Surg. 2008, 6 (Suppl. S1), S47–S52. [Google Scholar] [CrossRef] [Green Version]
- Kurup, A.N.; Callstrom, M.R. Ablation of Musculoskeletal Metastases: Pain Palliation, Fracture Risk Reduction, and Oligometastatic Disease. Tech. Vasc. Interv. Radiol. 2013, 16, 253–261. [Google Scholar] [CrossRef]
- Kurup, A.N.; Morris, J.M.; Callstrom, M.R. Ablation of Musculoskeletal Metastases. AJR Am. J. Roentgenol. 2017, 209, 713–721. [Google Scholar] [CrossRef]
| Interventional Radiology Techniques | ||||
|---|---|---|---|---|
| Techniques | Type | Aim of the Technique | Indications | Curative Treatment |
| Chemical ablation | Ethanol, Doxycycline, Polidocanol (detergent sclerosant, STS (detergent sclerosant) | Chemical-based ablation |
| |
| Embolization | Nano-particles | Minimizing blood loss |
| |
| RFA | Energy-based ablations (thermoablation) | Ablation techniques (inducing tumoral necrosis) needle driven |
| √ |
| MWA | Energy-based ablations (thermoablation) | Ablation techniques (inducing tumoral necrosis) needle driven |
| √ |
| CA | Energy-based ablations (thermoablation) | Ablation techniques (inducing tumoral necrosis) needle driven |
| √ |
| MRgFUS | Energy-based ablations (thermoablation) | Ablation techniques (inducing tumoral necrosis) needleless technique |
| √ |
| Cementoplasty | Cementoplasty (PMMA) including free-hand injection, vertebroplasty, kyphoplasty | Mechanical stabilization techniques |
| |
| Osteosynthesis | Intramedullary nails and screws | Mechanical stabilization techniques |
| |
| Author | Journal | Year | Ablation Modality | Title | No. of Patients/(no. of Tumors) | % Local Control | Survival Rate Overall Survival (%/Years; Median Month | Follow-Up (Months) | % Complications |
|---|---|---|---|---|---|---|---|---|---|
| Cazzato R. et al. [77] | Diagn Interv Imaging | 2021 | RFA, CA | Percutaneous thermal ablation of sacral metastases: Assessment of pain relief and local tumor control | 23 | 7 (30%) | NR | 21 | 22 |
| Cazzato R. et al. [28] | International Journal of Hyperthermia | 2018 | RFA + CA | Percutaneous image-guided ablation of bone metastases: local tumor control in oligometastatic patients | 46 | 71.7% 1 year | 95.4% 2 years | 34 | 10 |
| Ma Y. et al. [78] | Cardiovasc Intervent Radiol | 2018 | CA, RFA, MWA | Percutaneous Image-Guided Ablation in the Treatment of Osseous Metastases from Non-small Cell Lung Cancer | 45 (76) | 68% 1 year | NR | NR | 2.6 |
| Vaswani D. et al. [79] | Cardiovasc Intervent Radiol | 2018 | RFA, CA | Radiographic Local Tumor Control and Pain Palliation of Sarcoma Metastases within the Musculoskeletal System with Percutaneous Thermal Ablation | 13 (13) | 100% 1 year | NR | 12 | 5 |
| Gardner C. et al. [15] | J Bone Joint Surg Am | 2017 | CA | Cryoablation of Bone Metastases from Renal Cell Carcinoma for Local Tumor Control | 40 (50) | 41/50 (82%) | 31 (77/1 year 26/5 years) | 35 | 4 (8) |
| Erie A. et al. [80] | J Vasc Interv Radiol | 2017 | RFA, CA | Retrospective Review of Percutaneous Image-Guided Ablation of Oligometastatic Prostate Cancer: A Single-Institution Experience | 16 (18) | 15 (83%) | 100/2 years | 27 | 0 |
| Aubry S. et al. [81] | Eur Radiol | 2017 | MWA | Prospective 1-year follow-up pilot study of CT-guided microwave ablation in the treatment of bone and soft-tissue malignant tumours | 13 (16) | 4 (36.3%) | NR | 12 | 0 |
| Wallace A. et al. [13] | AJNR Am J Neuroradiol | 2016 | CA | Radiographic Local Control of Spinal Metastases with Percutaneous Radiofrequency Ablation and Vertebral Augmentation | 56 (92) | 79% 1 year | NR | NR | 4.3 |
| Tomasian A. et al. [82] | AJNR Am J Neuroradiol | 2016 | CA | Spine Cryoablation: Pain Palliation and Local Tumor Control for Vertebral Metastases | 14 (31) | 30 (96.7%) | NR | 10 | 0 |
| Wallace A. et al. [13] | AJNR Am J Neuroradiol | 2016 | RFA | Radiographic Local Control of Spinal Metastases with Percutaneous Radiofrequency Ablation and Vertebral Augmentation | NR (55) | 70% 1 year | NR | 7.9 | 0 |
| Barral M. et al. [30] | Cardiovasc Intervent Radiol | 2016 | RFA, CRIO, MWA | Percutaneous Thermal Ablation of Breast Cancer Metastases in Oligometastatic Patients | 79/114;18/NR | 83/1 year; 76/2 years | 98.3/1 year, 95.5/2 years | 18.4 | 12 (10.5) |
| Deschamps F. et al. [83] | Eur Radiol | 2014 | RFA, CA | Thermal ablation techniques: a curative treatment of bone metastases in selected patients? | 89 (122) | 67% 1 year | 91/1 year | 22.8 | 11 (9) |
| McMenomy B. et al [84]. | J Vasc Interv Radiol | 2013 | CA | Percutaneous cryoablation of musculoskeletal oligometastatic disease for complete remission | 40 (52) | 45 (87%) | 91/1 year, 84/2 years | 21 | 2 (5) |
| Littrup P. et al. [85]. | J Vasc Interv Radiol | 2013 | CA | Soft-tissue cryoablation in diffuse locations: feasibility and intermediate term outcomes | 126/251 | 225 (90%) | NR | 11 | 5 (2.3) |
| Bang H. et al. [48]. | J Vasc Interv Radiol | 2012 | CA | Percutaneous cryoablation of metastatic lesions from non-small-cell lung carcinoma: initial survival, local control, and cost observations | 8 (18) | 17 (94%) | NR | 11 | 2 (11) |
| Bang H. et al. [86]. | J Vasc Interv Radiol | 2012 | CA | Percutaneous cryoablation of metastatic renal cell carcinoma for local tumor control: feasibility, outcomes, and estimated cost-effectiveness for palliation | 27 (48) | 47 (97%) | NR | 16 | 1 (2) |
| Author | Journal | Year | Ablation Modality | Title | No. of Patients (No. of Tumors) | No. (%) of Patients with Reduced Pain | Mean Pain Score Change | Survival Rate Overall Survival (%/Years; Median Month) | Follow-Up (Months) | % Major Complications |
|---|---|---|---|---|---|---|---|---|---|---|
| Arrigoni F. et al. [87] | Radiol Med | 2022 | CA | CT-guided cryoablation for management of bone metastases: a single center experience and review of the literature | 28 | 100% | 6.9–3.5 (3.4/10) | 100% 3 months | 3 | 0 |
| Wang F. et al. [16] | Skeletal Radiol | 2022 | RFA + PVP | The combination of radiofrequency ablation and vertebroplasty shows advantages over single vertebroplasty in treating vertebral neoplastic lesions | 35 | NR | 8.46–1.7 (6.76/10) | NR | 6 | 0 |
| Jennings J. et al. [88] | Radiol Imaging Cancer | 2021 | CA | Cryoablation for Palliation of Painful Bone Metastases: The MOTION Multicenter Study | 66 | 74% | 7.3–3.7 (3.6/10) | NR | 6 | 4.6 |
| Madani K. et al. [89] | Support Care Cancer | 2021 | RFA + PVP | Combined local treatments for vertebral metastases with limited epidural extension | 18 (24) | 66.7% | 7.3–2 (5.3/10) | 73% 2 years | 16.7 | 0 |
| Kastler A. et al. [90] | Medicina (Kaunas) | 2021 | RFA + PVP | Bipolar Radiofrequency Ablation of Painful Spinal Bone Metastases Performed under Local Anesthesia: Feasibility Regarding Patient’s Experience and Pain Outcome | 25 | 83% | 8.4–1.8 (6.6/10) | 100% 1 year | 12 | 0 |
| Pusceddu C. et al. [91] | Curr Oncol | 2021 | PVP + RFA | The Role of a Navigational Radiofrequency Ablation Device and Concurrent Vertebral Augmentation for Treatment of Difficult-to-Reach Spinal Metastases | 35 (41) | NR | 5.7–0.9 (4.8/10) | 72% 1 year | 19 | 0 |
| Levy J. et al. [14] | J Vasc Interv Radiol | 2020 | RFA | Radiofrequency Ablation for the Palliative Treatment of Bone Metastases: Outcomes from the Multicenter OsteoCool Tumor Ablation Post-Market Study (OPuS One Study) in 100 Patients | 100 (134) | 100% | 8.2–3.5 (4.7/10) | 70% 6 months | 6 | 4 |
| Jiao D. et al. [18] | Acad Radiol | 2020 | MWA + PC | Simultaneous C-arm Computed Tomography-Guided Microwave Ablation and Cementoplasty in Patients with Painful Osteolytic Bone Metastases: A Single-center Experience | 30 (42) | 100% | 7.4–1.3 (6.1/10) | 66.7 1 year | 12 | 0 |
| Yang Y. et al. [92] | Cryobiology | 2020 | CA | Retrospective analysis of CT-guided percutaneous cryoablation for treatment of painful osteolytic bone metastasis | 26 (36) | 94.4% | 7.1–1.8 (5.3/10) | 100% 6 months | 6 | 11,5 |
| Yang X. et al. [93] | Eur J Radiol | 2020 | PVP | Vesselplasty using the Mesh-Hold™ bone-filling container for the treatment of pathological vertebral fractures due to osteolytic metastases: A retrospective study | 63 (105) | 97.4% | 8.2–2.1 (6.1/10) | 66.7% 1 year | 4–30 months | 16.2 cement leakage rate;1.9 paravertebral vein embolism |
| De Marini P.et al. [94] | Int J Hyperthermia | 2020 | RFA + CA | Percutaneous image-guided thermal ablation of bone metastases: a retrospective propensity study comparing the safety profile of radio-frequency ablation and cryo-ablation | 274 | NR | NR | 99,64% 1 year | 18.5 | 2.5 |
| Deib G. et al. [95] | AJR Am J Roentgenol | 2019 | MWA + PVP | Percutaneous Microwave Ablation and Cementoplasty: Clinical Utility in the Treatment of Painful Extraspinal Osseous Metastatic Disease and Myeloma | 65 (77) | NR | 6.32–2 (4,32/10) | 90.7% 1 year | 6 | 0 |
| Tanigawa N. et al. [96] | Cardiovasc Intervent Radiol | 2018 | RFA | Phase I/II Study of Radiofrequency Ablation for Painful Bone Metastases: Japan Interventional Radiology in Oncology Study Group 0208 | 33 (33) | 69.7% | 6–1.2 (4.8/10) | 97% 1 year | 12 | 12 |
| Prologo J. et al. [97] | Skeletal Radiol | 2014 | RFA | Image-guided cryoablation for the treatment of painful musculoskeletal metastatic disease: a single-center experience | 50 (54) | 94% | 8–3 (5/10) | 100% 3 months | 3 | 8 |
| Pusceddu C. et al. [76] | J Vasc Interv Radiol | 2013 | MWA | Treatment of bone metastases with microwave thermal ablation | 18 (21) | 100% | 5.6–0.45 (5.15/10) | 100% 3 months | 3 | 0 |
| Rossi G. et al. [98] | Radiol Med | 2013 | TAE using N-2-butyl cyanoacrylate (NBCA) | Embolisation of bone metastases from renal cancer | 107 (163) | 96% | NR | 10 months | 48 | Post embolisation syndrome 9.2%; Transient paraesthesias 25%; 1 intraprocedural tear of the left L3 artery and iliopsoas haemorrhage |
| Author | Journal | Year | Ablation Modality | Title | No. of Patients(no. of Tumors) |
|---|---|---|---|---|---|
| Cazzato R. et al. [77] | Diagn Interv Imaging | 2021 | RFA/CA | Percutaneous thermal ablation of sacral metastases: Assessment of pain relief and local tumor control follow-up | 23 |
| Pusceddu C. et al. [17] | Medicina (Kaunas) | 2021 | MWA + PC | Combined Microwave Ablation and Osteosynthesis for Long Bone Metastases | 11 |
| Campanacci L. et al. [99] | Eur J Surg Oncol | 2021 | ECT | Operating procedures for electrochemotherapy in bone metastases: Results from a multicenter prospective study on 102 patients | 102 |
| Koirala N. et al. [100] | Skeletal Radiol | 2020 | PC | Percutaneous reinforced osteoplasty for long bone metastases: a feasibility study | 15 |
| Giles S. et al. [101] | J Vasc Interv Radiol | 2019 | HIFU | Comparison of Imaging Changes and Pain Responses in Patients with Intra- or Extraosseous Bone Metastases Treated Palliatively with Magnetic Resonance-Guided High-Intensity-Focused Ultrasound | 21 |
| Sundararajan S. et al. [102] | J Oncol | 2019 | TAE+CRIO | Sequential Interventional Management of Osseous Neoplasms via Embolization, Cryoablation, and Osteoplasty cooling system | 15 |
| Tian Q. et al. [103] | Korean J Radiol | 2019 | PSP | Percutaneous Sacroplasty for Painful Sacral Metastases Involving Multiple Sacral Vertebral Bodies: Initial Experience with an Interpedicular Approach | 10 |
| Liu H. et al. [104] | Cardiovasc Intervent Radiol | 2019 | POP | Application of Percutaneous Osteoplasty in Treating Pelvic Bone Metastases: Efficacy and Safety | 126 |
| Cazzato R. et al. [105] | Int J Hyperthermia | 2018 | RFA | Low-power bipolar radiofrequency ablation and vertebral augmentation for the palliative treatment of spinal malignancies | 11 (11) |
| Chen Z. et al. [106] | Orthop Surg | 2018 | HIFU | Evaluation of Quality of Life Using EORTC QLQ-BM22 in Patients with Bone Metastases after Treatment with Magnetic Resonance Guided Focused Ultrasound | 26 |
| Khan M. et al. [107] | AJNR | 2018 | MWA | Efficacy and safety of percutaneous microwave ablation and cementoplasty in the treatment of painful spinal metastases and myeloma | 69 (102) |
| Couraud G. et al. [108] | J bone oncol | 2018 | PC | Evaluation of short-term efficacy of extraspinal cementoplasty for bone metastasis: a monocenter study of 31 patients. | 31 |
| Fares A. et al. [109] | J Egypt Natl Canc Inst | 2018 | PC | Combined percutaneous radiofrequency ablation and cementoplasty for the treatment of extraspinal painful bone metastases: a prospective study. J Egypt Natl Canc | 30 |
| Bertrand A. et al. [110] | J Ther Ultrasound | 2018 | HIFU | Focused ultrasound for the treatment of bone metastases: effectiveness and feasibility | 17 |
| Ma Y. et al. [78] | Cardiovasc Intervent Radiol | 2018 | RFA/CA/MWA | Percutaneous Image-Guided Ablation in the Treatment of Osseous Metastases from Non-small Cell Lung Cancer | 45 |
| Vaswani D. et al. [79] | Cardiovasc Intervent Radiol | 2018 | CA + PC | Radiographic Local Tumor Control and Pain Palliation of Sarcoma Metastases within the Musculoskeletal System with Percutaneous Thermal Ablation | 41 |
| Coupal T. et al. [111] | Pain Physician | 2017 | TAE | The Hopeless Case? Palliative Cryoablation and Cementoplasty Procedures for Palliation of Large Pelvic Bone Metastases | 48 |
| Pusceddu C. et al. [112] | Skeletal Radiol | 2017 | PC | CT-guided percutaneous screw fixation plus cementoplasty in the treatment of painful bone metastases with fractures or a high risk of pathological fracture | 27 |
| Reyad R. et al. [113] | Diagn Interv Imaging | 2017 | PVP | Thick cement usage in percutaneous vertebroplasty for malignant vertebral fractures at high risk for cement leakage | 77 |
| Motta A. et al. [114] | Eur J Radiol | 2017 | CA | Feasibility of percutaneous cryoablation of vertebral metastases under local anaesthesia in ASAIII patients | 11 |
| McArthur T. et al. [115] | Curr Probl Diagn Radiol | 2017 | CA | Percutane Image-Guided Cryoablation of Painful Osseous Metastases: A Retrospective Single-Center Review | 16 |
| Baagla S. et al. [116] | Cardiovasc Intervent Radiol | 2016 | RFA | Multicenter Prospective Clinical Series Evaluating Radiofrequency Ablation in the Treatment of Painful Spine Metastases | 50 (69) |
| Tomasian A. et al. [82] | AJNR Am J Neuroradiol | 2016 | CA | Spine Cryoablation: Pain Palliation and Local Tumor Control for Vertebral Metastases | 14 (31) |
| Facchini G. et al. [117] | Eur J Orthop Surg Traumatol | 2016 | TAE | Palliative embolization for metastases of the spine | 164 |
| Pusceddu C. et al. [118] | Cardiovasc Intervent Radiol | 2016 | MWA + PC | Combined Microwave Ablation and Cementoplasty in Patients with Painful Bone Metastases at High Risk of Fracture follow-up | 35 (37) |
| Anzidei M. et al. [119] | Radiol Med | 2016 | HIFU | Magnetic resonance-guided focused ultrasound for the treatment of painful bone metastases: role of apparent diffusion coefficient (ADC) and dynamic contrast enhanced (DCE) MRI | 23 |
| Wang F. et al. [120] | Pain Physician | 2016 | TAE | Sequential Transarterial Embolization Followed by Percutaneous Vertebroplasty Is Safe and Effective in Pain Management in Vertebral Metastases | 25 |
| Chen F. et al. [121] | Oncol Lett | 2016 | RFA | Percutaneous kyphoplasty for the treatment of spinal metastases | 282 |
| Susa M. et al. [47] | BMC Cancer | 2016 | CA | CT guided cryoablation for locally recurrent or metastatic bone and soft tissue tumor: initial experience | 9 |
| Bianchi G. et al. [122] | World J Surg | 2016 | ECT | Electrochemotherapy in the Treatment of Bone Metastases: A Phase II Trial | 29 |
| Jiao D. et al. [123] | Oncotarget | 2016 | RFA | Radiofrequency ablation versus 125I-seed brachytherapy for painful metastases involving the bone | 79 |
| Joo B. et al. [124] | Yonsei Med J | 2015 | HIFU | Pain palliation in patients with bone metastases using magnetic resonance-guided focused ultrasound with conformal bone system: a preliminary report | 5 |
| Wallace A. et al. [125] | J Neurooncol | 2015 | RFA | Radiofrequency ablation and vertebral augmentation for palliation of painful spinal metastases | 72 (110) |
| Wei Z. et al. [126] | Skeletal Radiol | 2015 | MWA | Computed tomography-guided percutaneous microwave ablation combined with osteoplasty for palliative treatment of painful extraspinal bone metastases from lung cancer | 26 (33) |
| Di Staso M. et al. [127] | PLoS One | 2015 | CA + RTA | Treatment of solitary painful osseous metastases with radiotherapy, cryoablation or combined therapy: Propensity matching analysis in 175 patients | 175 |
| Cazzato R. et al. [128] | Eur J Surg Oncol | 2015 | RFA/PC/CA | Over ten years of single-institution experience in percutaneous image-guided treatment of bone metastases from differentiated thyroid cancer | 25 (49) |
| Tian Q. et al. [129] | J Vasc Interv Radiol | 2014 | RFA + pop | Combination radiofrequency ablation and percutaneous osteoplasty for palliative treatment of painful extraspinal bone metastasis: a single-center experience | 38 |
| Kastler A. et al. [130] | J Vasc Interv Radiol | 2014 | MWA | Microwave thermal ablation of spinal metastatic bone tumors | 17 (20) |
| Hurwitz M. et al. [131] | J Natl Cancer Inst | 2014 | HIFU | Magnetic resonance-guided focused ultrasound for patients with painful bone metastases: phase III trial results | 112/NR versus 35/NR |
| Alemann G. et al. [132] | J Palliat Med | 2014 | RFA | Treatment of painful extraspinal bone metastases with percutaneous bipolar radiofrequency under local anesthesia: feasibility and efficacy in twenty-eight cases | 28 |
| Botsa E. et al. [133] | Ann Palliat Med | 2014 | RFA/MWA | CT image guided thermal ablation techniques for palliation of painful bone metastases | 45 |
| Li Z. et al. [134] | Chin Med J (Engl) | 2014 | PVP | Kyphoplasty versus vertebroplasty for the treatment of malignant vertebral compression fractures caused by metastases: a retrospective study | 80 |
| Deschamps F. et al. [83] | Eur Radiol | 2014 | RFA + CA | Thermal ablation techniques: a curative treatment of bone metastases in selected patients? | 89 |
| Li F. et al. [135] | Pathol Oncol Res. | 2014 | CA | An Effective Therapy to Painful Bone Metastases: Cryoablation Combined with Zoledronic Acid | 56 |
| Sun G. et al. [136] | Eur Radiol | 2014 | PC | Cementoplasty for man- aging painful bone metastases outside the spine | 51 |
| Callstrom M. et al. [137] | Cancer | 2013 | CA | Percutaneous image-guided cryoablation of painful metastases involving bone: multicenter trial | 61 (69) |
| Napoli A. et al. [138] | invest Radiol | 2013 | HIFU | Primary pain palliation and local tumor control in bone metastases treated with magnetic resonance-guided focused ultrasound | 18 (18) |
| Anselmetti G. et al. [139] | Pain Physician | 2013 | PVP | Percutaneous vertebral augmentation assisted by PEEK implant in painful osteolytic vertebral metastasis involving the vertebral wall: experience on 40 patients | 40 |
| Trumm C. et al. [140] | Skeletal Radiol | 2013 | PVP | CT fluoroscopy-guided vertebral augmentation with a radiofrequency-induced, high-viscosity bone cement (StabiliT(®)): technical results and polymethylmethacrylate leakages in 25 patients | 25 |
| Kastler A. et al. [141] | Pain Med | 2013 | MWA | Analgesic effects of microwave ablation of bone and soft tissue tumors under local anesthesia | 15 (25) |
| Masala S. et al. [60] | Neuroradiology. | 2012 | CA | Combined use of percutaneous cryoablation and vertebroplasty with 3D rotational angiograph in treatment of single vertebral metastasis: Comparison with vertebroplasty. | 23 |
| Iannessi A. et al. [142] | Diagn Interv Imaging | 2012 | PC | Percutaneous cementoplasty for the treatment of extraspinal painful bone lesion: a prospective study. | 20 |
| Rossi G. et al. [143] | Radiol Med | 2011 | TAE | Selective arterial embolisation for bone tumours: experience of 454 cases | 365 (454) |
| Masala S. et al. [144] | Singapore Med J | 2011 | RFA + VP/CA + VP | Percutaneous ablative treatment of metastatic bone tumours: visual analogue scale scores in a short-term series | 30 |
| Thacker P. et al. [46] | AJR Am J Roentgenol. | 2011 | CA | Palliation of painful metastatic disease involving bone with imaging-guided treatment: Comparison of patients’ immediate response to radiofrequency ablation and cryoablation | 36 |
| Masala S. et al. [145] | Skeletal Radiol. | 2011 | CA | Metabolic and clinical assessment of efficacy of cryoablation therapy on skeletal masses by 18F-FDG positron emission tomography/computed tomography (PET/CT) and visual analogue scale (VAS): Initial experience | 20 |
| Masala S. et al. [146] | Support Care Cancer | 2011 | PC | Percutaneus osteoplasty in the treatment of extraspinal painful multiple myeloma lesions | 39 |
| Rossi G. et al. [5] | J Vasc Interv Radiol | 2011 | TAE | Selective embolization with N-butyl cyanoacrylate for metastatic bone disease | 243 (309) |
| Dupuy D. et al. [25] | Cancer | 2010 | RFA | Percutaneous radiofrequency ablation of painful osseous metastases: a multicenter American College of Radiology Imaging Network trial follow-up | 55 (55) |
| Kashima M. et al. [147] | AJR Am J Roentgenol | 2010 | RFA | Radiofrequency ablation for the treatment of bone metastases from hepatocellular carcinoma | 40 |
| Liberman B.et al. [54] | Ann Surg Oncol | 2009 | HIFU | Pain palliation in patients with bone metastases using MR-guided focused ultrasound surgery: a multicenter study | 31 (32) |
| Carrafiello G. et al. [148] | Radiol Med | 2009 | RFA | Percutaneous imaging-guided ablation therapies in the treatment of symptomatic bone metastases: preliminary experience | 10 |
| Delpla A. et al. [149] | Cardiovasc Intervent Radiol | 2009 | PVP | Preventive Vertebroplasty for Long-Term Consolidation of Vertebral Metastases | 100 |
| Thanos L. et al. [150] | Skeletal Radiol | 2008 | RFA | Radiofrequency ablation of osseous metastases for the palliation of pain | 30 |
| Gianfelice D. et al. [151] | Radiology | 2008 | HIFU | Palliative treatment of painful bone metastases with MR imaging--guided focused ultrasound | 11-dic |
| Basile A. et al. [152] | Radiol Med | 2008 | RFA + PC | Cementoplasty in the management of painful extraspinal bone metastases: our experience | 13 |
| Anselmetti G. et al. [153] | Cardiovasc Intervent Radiol | 2008 | PC | Treatment of extraspinal painful bone metastases with percutaneous cementoplasty: a prospective study of 50 patients MDCT features, and treatment with RFA | 50 |
| Trumm C. et al. [154] | J Vasc Interv Radiol | 2008 | PVP | CT fluoroscopy-guided percutaneous vertebroplasty for the treatment of osteolytic breast cancer metastases: results in 62 sessions with 86 vertebrae treated | 53 |
| Tuncali K. et al. [155] | AJR Am J Roentgenol | 2007 | CA + HIFU | MRI-guided percutaneous cryotherapy for soft-tissue and bone metastases: initial experience | 22 |
| Catane R. et al. [55] | Ann Oncol | 2007 | HIFU | MR-guided focused ultrasound surgery (MRgFUS) for the palliation of pain in patients with bone metastases--preliminary clinical experience | 113 |
| Forauer A. et al. [156] | Acta Oncol | 2007 | TAE | Selective palliative transcatheter embolization of bony metastases from renal cell carcinoma | 21 |
| Callstrom M. et al. [157] | Radiology | 2006 | CA | Painful metastases involving bone: percutaneous image-guided cryoablation--prospective trial interim analysis | 14 |
| Barragán-Campos H. et al. [69] | Radiology | 2006 | PVP | Percutaneous vertebroplasty for spinal metastases: complications | 117 |
| Weber C. et al. [158] | Rofo | 2006 | PVP | [CT-guided vertebroplasty and kyphoplasty: comparing technical success rate and complications in 101 cases] | 69 (101) |
| Callstrom M. et al. [159] | Oncology | 2005 | RFA | Percutaneous ablation: safe, effective treatment of bone tumors | 14 |
| Cai H. et al. [160] | Ai Zheng | 2005 | RFA + VP/CA + VP | [Treatment effect of percutaneous vertebroplasty combined with interventional chemotherapy on vertebral metastases] | 75 |
| Masala S. et al. [161] | In Vivo | 2005 | PVP | MRI and bone scan imaging in the preoperative evaluation of painful vertebral fractures treated with vertebroplasty and kyphoplasty | 30 |
| Guzman R. et al. [162] | Eur Spine J | 2005 | TAE | Preoperative transarterial embolization of vertebral metastases | 24 |
| Goetz M. et al. [37] | J Clin Oncol | 2004 | RFA | Percutaneous image-guided radiofrequency ablation of painful metastases involving bone: a multicenter study | 43 (43) |
| Masala S. et al. [163] | J Chemother | 2004 | PVP | Vertebroplasty and kyphoplasty in the treatment of malignant vertebral fractures | 33 |
| Poggi G. et al. [164] | Anticancer Res | 2003 | RFA | Percutaneous ultrasound-guided radiofrequency thermal ablation of malignant osteolyses | 5 |
| Eustatia-Rutten C. et al. [165] | J Clin Endocrinol Metab | 2003 | TAE | Outcome of palliative embolization of bone metastases in diferentiated thyroid carcinoma | 16 |
| Fourney D. et al. [166] | J Neurosurg | 2003 | PVP | Percutaneous vertebroplasty and kyphoplasty for painful vertebral body fractures in cancer patients | 56 |
| Winking M. et al. [167] | Ger Med Sci | 2003 | PVP | PMMA vertebroplasty in patients with malignant vertebral destruction of the thoracic and lumbar spine | 22 |
| Alvarez L. et al. [168] | Eur Spine J | 2003 | PVP | Vertebroplasty in the treatment of vertebral tumors: postprocedural outcome and quality of life | 21 |
| Hierholzer J. et al. [169] | J Vasc Interv Radiol | 2003 | PC | Percutaneous osteoplasty as a treatment for painful malignant bone lesions of the pelvis and femur | 5 |
| Grönemeyer D. et al. [170] | Cancer J | 2002 | RFA | Image-guided radiofrequency ablation of spinal tumors: preliminary experience with an expandable array electrode | 10 |
| Chatziioannou A. et al. [171] | Eur Radiol | 2000 | TAE | Preoperative embolization of bone metastases from renal cell carcinoma | 26 |
| Barr J. et al. [172] | Spine (Phila Pa 1976) | 2000 | PVP | Percutaneous vertebroplasty for pain relief and spinal stabilization | 47 |
| Martin J. et al. [173] | Bone | 1999 | PVP | Vertebroplasty: clinical experience and follow-up results | 40 |
| Sun S. et al. [174] | J Vasc Interv Radiol | 1998 | TAE | Bone metastases from renal cell carcinoma: preoperative embolization | 16 |
| Weill A. et al. [175] | Radiology | 1996 | PVP | Spinal metastases: indications for and results of percutaneous injection of acrylic surgical cement | 37 |
| Cotten A. et al. [176] | Radiology | 1996 | PVP | Percutaneous vertebroplasty for osteolytic metastases and myeloma: effects of the percentage of lesion filling and the leakage of methyl methacrylate at clinical follow-up | 37 |
| Breslau J. et al. [177] | J Vasc Interv Radiol | 1995 | TAE | Preoperative embolization of spinal tumors | 14 |
| Corcos G. et al. [178] | Spine (Phila Pa 1976) | 1995 | PVP | Cement leakage in percutaneous vertebroplasty for spinal metastases: a retrospective evaluation of incidence and risk factors | 56 |
| Author | Journal | Year | Ablation Modality | Title | No. of Patients/(No. of Tumors) | % Local Control Tumor Response (Complete or Partial Response) | Mean Pain Score Change | No. (%) of Patients with Reduced Pain | Survival Rate Overall Survival (%/Years; Median Month | Follow-Up (Months) | % Major Complications |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Nakatsuka A. et al. [179] | J Vasc Interv Radiol | 2016 | RFA | Safety and Clinical Outcomes of Percutaneous Radiofrequency Ablation for Intermediate and Large Bone Tumors Using a Multiple-Electrode Switching System: A Phase II Clinical Study | 20 | 88.9% | 3.6–1.5 (2.1/10) | 84.6% | 60.9% 1 year; 14.1 months | 12 | 0 |
| Yu W. et al. [180] | Surg Oncol | 2015 | HIFU | High-intensity focused ultrasound: noninvasive treatment for local unresectable recurrence of osteosarcoma | 27 | 85.2% | 2.04–0.32 (1.7/3) | NR | 21 months | 21 | 0 |
| Anselmetti G. et al. [181] | Cardiovasc Intervent Radiol | 2012 | PVP | Percutaneous vertebroplasty in multiple myeloma: prospective long-term follow-up in 106 consecutive patients | 106 | NR | 9–1 (8/10) | 90% | NR | 28.2 ± 12.1 months | 1.6% |
| Li C. et al. [182] | Cancer | 2010 | HIFU | Noninvasive treatment of malignant bone tumors using high-intensity focused ultrasound | 13 | 46.2%complete response; 38.4% partial response | 1.85–0.08 (1.77/3) | 100% | 38.5% 5 year; 43.0 months | 60 | 0 |
| Chen W. et al. [21] | Radiology | 2010 | HIFU | Primary bone malignancy: effective treatment with high-intensity focused ultrasound ablation follow-up | 80 | 86% | NR | NR | 50.5% 5 year | 60 | 50% |
| Li C. et al. [75] | Cancer Biol Ther | 2009 | HIFU | Osteosarcoma: Limb salvaging treatment by ultrasonographically guided high-intensity focused ultrasound | 7 | 42.9% complete response;42.9% partial response | NR | 100% | 71.4% 5 year; 68 months | 81 | 0 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sgalambro, F.; Zugaro, L.; Bruno, F.; Palumbo, P.; Salducca, N.; Zoccali, C.; Barile, A.; Masciocchi, C.; Arrigoni, F. Interventional Radiology in the Management of Metastases and Bone Tumors. J. Clin. Med. 2022, 11, 3265. https://doi.org/10.3390/jcm11123265
Sgalambro F, Zugaro L, Bruno F, Palumbo P, Salducca N, Zoccali C, Barile A, Masciocchi C, Arrigoni F. Interventional Radiology in the Management of Metastases and Bone Tumors. Journal of Clinical Medicine. 2022; 11(12):3265. https://doi.org/10.3390/jcm11123265
Chicago/Turabian StyleSgalambro, Ferruccio, Luigi Zugaro, Federico Bruno, Pierpaolo Palumbo, Nicola Salducca, Carmine Zoccali, Antonio Barile, Carlo Masciocchi, and Francesco Arrigoni. 2022. "Interventional Radiology in the Management of Metastases and Bone Tumors" Journal of Clinical Medicine 11, no. 12: 3265. https://doi.org/10.3390/jcm11123265






