Effectiveness of ERAS (Enhanced Recovery after Surgery) Protocol via Peripheral Nerve Block for Total Knee Arthroplasty
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
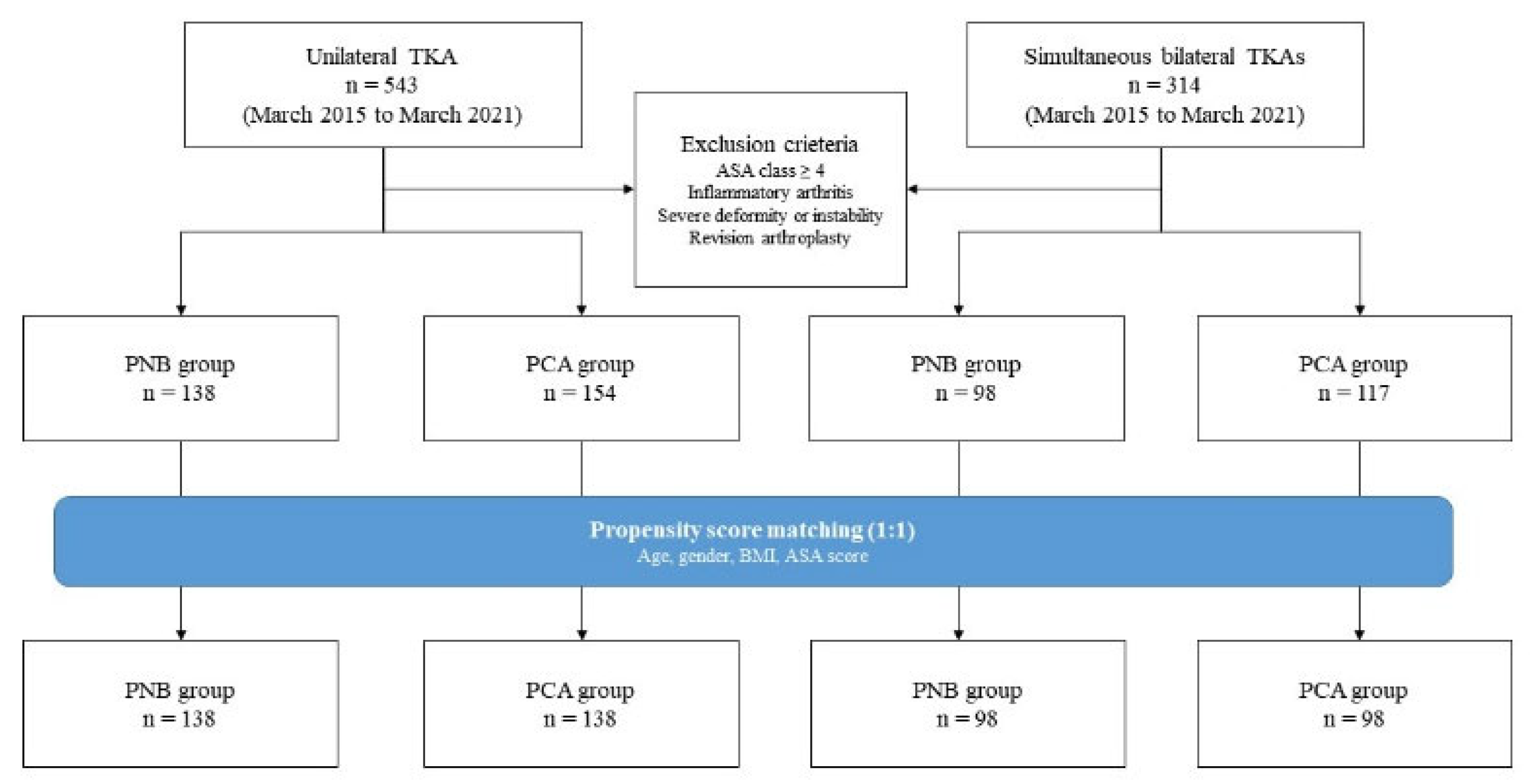
2.2. Participants
2.3. Surgery
2.4. Definition of Groups
2.5. Outcome Measures
2.6. Propensity Score Matching
2.7. Statistical Analysis
3. Results
3.1. Primary Outcome
3.2. Secondary Outcomes
3.3. Subgroup Analysis
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Chard, J.; Lohmander, S.; Smith, C.; Scott, D. Osteoarthritis. Clin. Evid. 2002, 8, 1212–1237. [Google Scholar]
- Cudejko, T.; van der Esch, M.; van der Leeden, M.; Holla, J.; Roorda, L.D.; Lems, W.; Dekker, J. Proprioception mediates the association between systemic inflammation and muscle weakness in patients with knee osteoarthritis: Results from the amsterdam osteoarthritis cohort. J. Rehabil. Med. 2018, 50, 67–72. [Google Scholar] [CrossRef] [PubMed]
- Vincent, K.R.; Vincent, H.K. Resistance exercise for knee osteoarthritis. Pm R 2012, 4, S45–S52. [Google Scholar] [CrossRef] [PubMed]
- Cudejko, T.; van der Esch, M.; Schrijvers, J.; Richards, R.; van den Noort, J.C.; Wrigley, T.; van der Leeden, M.; Roorda, L.D.; Lems, W.; Harlaar, J.; et al. The immediate effect of a soft knee brace on dynamic knee instability in persons with knee osteoarthritis. Rheumatology 2018, 57, 1735–1742. [Google Scholar] [CrossRef] [PubMed]
- Cherian, J.J.; Kapadia, B.H.; Bhave, A.; McElroy, M.J.; Cherian, C.; Harwin, S.F.; Mont, M.A. Use of transcutaneous electrical nerve stimulation device in early osteoarthritis of the knee. J. Knee Surg. 2015, 28, 321–327. [Google Scholar] [CrossRef]
- Steinmeyer, J.; Bock, F.; Stöve, J.; Jerosch, J.; Flechtenmacher, J. Pharmacological treatment of knee osteoarthritis: Special considerations of the new german guideline. Orthop. Rev. 2018, 10, 7782. [Google Scholar] [CrossRef]
- Capdevila, X.; Barthelet, Y.; Biboulet, P.; Ryckwaert, Y.; Rubenovitch, J.; d’Athis, F. Effects of perioperative analgesic technique on the surgical outcome and duration of rehabilitation after major knee surgery. Anesthesiology 1999, 91, 8–15. [Google Scholar] [CrossRef]
- Parvizi, J.; Miller, A.G.; Gandhi, K. Multimodal pain management after total joint arthroplasty. J. Bone Jt. Surg. Am. 2011, 93, 1075–1084. [Google Scholar] [CrossRef]
- Vendittoli, P.A.; Makinen, P.; Drolet, P.; Lavigne, M.; Fallaha, M.; Guertin, M.C.; Varin, F. A multimodal analgesia protocol for total knee arthroplasty. A randomized, controlled study. J. Bone Jt. Surg. Am. 2006, 88, 282–289. [Google Scholar] [CrossRef]
- Abdul-Hadi, O.; Parvizi, J.; Austin, M.S.; Viscusi, E.; Einhorn, T. Nonsteroidal anti-inflammatory drugs in orthopaedics. J. Bone Jt. Surg. Am. 2009, 91, 2020–2027. [Google Scholar]
- Husted, H.; Lunn, T.H.; Troelsen, A.; Gaarn-Larsen, L.; Kristensen, B.B.; Kehlet, H. Why still in hospital after fast-track hip and knee arthroplasty? Acta Orthop. 2011, 82, 679–684. [Google Scholar] [CrossRef] [PubMed]
- Kehlet, H. Multimodal approach to control postoperative pathophysiology and rehabilitation. Br. J. Anaesth. 1997, 78, 606–617. [Google Scholar] [CrossRef] [PubMed]
- Toftdahl, K.; Nikolajsen, L.; Haraldsted, V.; Madsen, F.; Tønnesen, E.K.; Søballe, K. Comparison of peri- and intraarticular analgesia with femoral nerve block after total knee arthroplasty: A randomized clinical trial. Acta Orthop. 2007, 78, 172–179. [Google Scholar] [CrossRef] [PubMed]
- Singelyn, F.J.; Deyaert, M.; Joris, D.; Pendeville, E.; Gouverneur, J.M. Effects of intravenous patient-controlled analgesia with morphine, continuous epidural analgesia, and continuous three-in-one block on postoperative pain and knee rehabilitation after unilateral total knee arthroplasty. Anesth. Analg. 1998, 87, 88–92. [Google Scholar] [CrossRef]
- Raj, P.P.; Knarr, D.C.; Vigdorth, E.; Denson, D.D.; Pither, C.E.; Hartrick, C.T.; Hopson, C.N.; Edström, H.H. Comparison of continuous epidural infusion of a local anesthetic and administration of systemic narcotics in the management of pain after total knee replacement surgery. Anesth. Analg. 1987, 66, 401–406. [Google Scholar] [CrossRef]
- Jaeger, P.; Nielsen, Z.J.; Henningsen, M.H.; Hilsted, K.L.; Mathiesen, O.; Dahl, J.B. Adductor canal block versus femoral nerve block and quadriceps strength: A randomized, double-blind, placebo-controlled, crossover study in healthy volunteers. Anesthesiology 2013, 118, 409–415. [Google Scholar] [CrossRef]
- Lund, J.; Jenstrup, M.T.; Jaeger, P.; Sørensen, A.M.; Dahl, J.B. Continuous adductor-canal-blockade for adjuvant post-operative analgesia after major knee surgery: Preliminary results. Acta Anaesthesiol. 2011, 55, 14–19. [Google Scholar] [CrossRef]
- Chu, C.C.; Weng, S.F.; Chen, K.T.; Chien, C.C.; Shieh, J.P.; Chen, J.Y.; Wang, J.J. Propensity score-matched comparison of postoperative adverse outcomes between geriatric patients given a general or a neuraxial anesthetic for hip surgery: A population-based study. Anesthesiology 2015, 123, 136–147. [Google Scholar] [CrossRef]
- Rubin, D.B. The design versus the analysis of observational studies for causal effects: Parallels with the design of randomized trials. Stat. Med. 2007, 26, 20–36. [Google Scholar] [CrossRef]
- Fischer, H.B.; Simanski, C.J.; Sharp, C.; Bonnet, F.; Camu, F.; Neugebauer, E.A.; Rawal, N.; Joshi, G.P.; Schug, S.A.; Kehlet, H. A procedure-specific systematic review and consensus recommendations for postoperative analgesia following total knee arthroplasty. Anaesthesia 2008, 63, 1105–1123. [Google Scholar] [CrossRef]
- Singelyn, F.J.; Gouverneur, J.M. Extended “three-in-one” block after total knee arthroplasty: Continuous versus patient-controlled techniques. Anesth. Analg. 2000, 91, 176–180. [Google Scholar]
- Paul, J.E.; Arya, A.; Hurlburt, L.; Cheng, J.; Thabane, L.; Tidy, A.; Murthy, Y. Femoral nerve block improves analgesia outcomes after total knee arthroplasty: A meta-analysis of randomized controlled trials. Anesthesiology 2010, 113, 1144–1162. [Google Scholar] [CrossRef]
- Lee, R.M.; Lim Tey, J.B.; Chua, N.H. Postoperative pain control for total knee arthroplasty: Continuous femoral nerve block versus intravenous patient controlled analgesia. Anesth. Pain Med. 2012, 1, 239–242. [Google Scholar] [CrossRef]
- Gandhi, H.J.; Trivedi, L.H.; Tripathi, D.C.; Dash, D.M.; Khare, A.M.; Gupta, M.U. A randomized, controlled trial of comparison of a continuous femoral nerve block (cfnb) and continuous epidural infusion (cei) using 0.2% ropivacaine for postoperative analgesia and knee rehabilitation after total knee arthroplasty (tka). J. Anaesthesiol. Clin. Pharm. 2019, 35, 386–389. [Google Scholar] [CrossRef] [PubMed]
- Fowler, S.J.; Symons, J.; Sabato, S.; Myles, P.S. Epidural analgesia compared with peripheral nerve blockade after major knee surgery: A systematic review and meta-analysis of randomized trials. Br. J. Anaesth. 2008, 100, 154–164. [Google Scholar] [CrossRef]
- Barrington, M.J.; Olive, D.; Low, K.; Scott, D.A.; Brittain, J.; Choong, P. Continuous femoral nerve blockade or epidural analgesia after total knee replacement: A prospective randomized controlled trial. Anesth. Analg. 2005, 101, 1824–1829. [Google Scholar] [CrossRef] [PubMed]
- Yu, R.; Wang, H.; Zhuo, Y.; Liu, D.; Wu, C.; Zhang, Y. Continuous adductor canal block provides better performance after total knee arthroplasty compared with the single-shot adductor canal block: An updated meta-analysis of randomized controlled trials. Medicine 2020, 99, e22762. [Google Scholar] [CrossRef] [PubMed]
- Carli, F.; Clemente, A.; Asenjo, J.F.; Kim, D.J.; Mistraletti, G.; Gomarasca, M.; Morabito, A.; Tanzer, M. Analgesia and functional outcome after total knee arthroplasty: Periarticular infiltration vs continuous femoral nerve block. Br. J. Anaesth. 2010, 105, 185–195. [Google Scholar] [CrossRef] [PubMed]
- Affas, F.; Nygards, E.B.; Stiller, C.O.; Wretenberg, P.; Olofsson, C. Pain control after total knee arthroplasty: A randomized trial comparing local infiltration anesthesia and continuous femoral block. Acta Orthop. 2011, 82, 441–447. [Google Scholar] [CrossRef] [PubMed]
- Kayupov, E.; Okroj, K.; Young, A.C.; Moric, M.; Luchetti, T.J.; Zisman, G.; Buvanendran, A.; Gerlinger, T.L.; Della Valle, C.J. Continuous adductor canal blocks provide superior ambulation and pain control compared to epidural analgesia for primary knee arthroplasty: A randomized, controlled trial. J. Arthroplast. 2018, 33, 1040–1044.e1. [Google Scholar] [CrossRef]
- Ng, F.Y.; Chiu, K.Y.; Yan, C.H.; Ng, K.F. Continuous femoral nerve block versus patient-controlled analgesia following total knee arthroplasty. J. Orthop. Surg. 2012, 20, 23–26. [Google Scholar] [CrossRef] [PubMed]
- Liow, R.Y.; Walker, K.; Wajid, M.A.; Bedi, G.; Lennox, C.M. The reliability of the american knee society score. Acta Orthop. Scand. 2000, 71, 603–608. [Google Scholar] [CrossRef]
- Bellamy, N.; Buchanan, W.W.; Goldsmith, C.H.; Campbell, J.; Stitt, L.W. Validation study of womac: A health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee. J. Rheumatol. 1988, 15, 1833–1840. [Google Scholar]
- Chan, E.Y.; Fransen, M.; Parker, D.A.; Assam, P.N.; Chua, N. Femoral nerve blocks for acute postoperative pain after knee replacement surgery. Cochrane Database Syst. Rev. 2014, 2014, Cd009941. [Google Scholar] [CrossRef]
- Beaupre, L.A.; Johnston, D.B.; Dieleman, S.; Tsui, B. Impact of a preemptive multimodal analgesia plus femoral nerve blockade protocol on rehabilitation, hospital length of stay, and postoperative analgesia after primary total knee arthroplasty: A controlled clinical pilot study. Sci. World J. 2012, 2012, 273821. [Google Scholar] [CrossRef]
- Gao, F.; Ma, J.; Sun, W.; Guo, W.; Li, Z.; Wang, W. Adductor canal block versus femoral nerve block for analgesia after total knee arthroplasty: A systematic review and meta-analysis. Clin. J. Pain 2017, 33, 356–368. [Google Scholar] [CrossRef]
- Kim, D.H.; Lin, Y.; Goytizolo, E.A.; Kahn, R.L.; Maalouf, D.B.; Manohar, A.; Patt, M.L.; Goon, A.K.; Lee, Y.Y.; Ma, Y.; et al. Adductor canal block versus femoral nerve block for total knee arthroplasty: A prospective, randomized, controlled trial. Anesthesiology 2014, 120, 540–550. [Google Scholar] [CrossRef]
- Shah, N.A.; Jain, N.P. Is continuous adductor canal block better than continuous femoral nerve block after total knee arthroplasty? Effect on ambulation ability, early functional recovery and pain control: A randomized controlled trial. J. Arthroplast. 2014, 29, 2224–2229. [Google Scholar] [CrossRef]
- Jæger, P.; Zaric, D.; Fomsgaard, J.S.; Hilsted, K.L.; Bjerregaard, J.; Gyrn, J.; Mathiesen, O.; Larsen, T.K.; Dahl, J.B. Adductor canal block versus femoral nerve block for analgesia after total knee arthroplasty: A randomized, double-blind study. Reg. Anesth. Pain Med. 2013, 38, 526–532. [Google Scholar] [CrossRef] [PubMed]
- Mudumbai, S.C.; Kim, T.E.; Howard, S.K.; Workman, J.J.; Giori, N.; Woolson, S.; Ganaway, T.; King, R.; Mariano, E.R. Continuous adductor canal blocks are superior to continuous femoral nerve blocks in promoting early ambulation after tka. Clin. Orthop. Relat. Res. 2014, 472, 1377–1383. [Google Scholar] [CrossRef] [PubMed]
- Patrick, M.R.; Parvataneni, H.K.; Bohannon, D.S.; Boezaart, A.P. Early experience with bilateral continuous femoral nerve block and single-injection spinal anesthesia for bilateral total knee arthroplasty: A case series. Pain Med. 2018, 19, 1839–1847. [Google Scholar] [CrossRef] [PubMed]
- Sztain, J.F.; Gabriel, R.A.; Sievert, K.E.; Khatibi, B. Bilateral adductor canal block catheters in patients undergoing simultaneous bilateral knee arthroplasty: A series of 17 patients. J. Clin. Anesth. 2018, 44, 98–99. [Google Scholar] [CrossRef] [PubMed]
- Kane, L.T.; Fang, T.; Galetta, M.S.; Goyal, D.K.C.; Nicholson, K.J.; Kepler, C.K.; Vaccaro, A.R.; Schroeder, G.D. Propensity score matching: A statistical method. Clin. Spine Surg. 2020, 33, 120–122. [Google Scholar] [CrossRef] [PubMed]




| UTKA | BTKAs | ||||||
|---|---|---|---|---|---|---|---|
| PNB Group (n = 138) | PCA Group (n = 138) | p-Value | PNB Group (n = 98) | PCA Group (n = 98) | p-Value | ||
| Age | 71.3 ± 6.6 | 70.3 ± 6.9 | 0.244 | 71.2 ± 6.0 | 70.6 ± 5.5 | 0.487 | |
| Gender, No. (%) | 0.084 | 0.578 | |||||
| Male | 30 (21.7) | 19 (13.8) | 16 (16.3) | 19 (19.4) | |||
| Female | 108 (78.3) | 119 (86.2) | 82 (83.7) | 79 (80.6) | |||
| BMI | 26.4 ± 3.2 | 26.3 ± 3.4 | 0.821 | 27.0 ± 3.9 | 26.7 ± 3.7 | 0.566 | |
| ASA | 0.918 | 0.642 | |||||
| 1 | 6 | 7 | 9 | 5 | |||
| 2 | 66 | 63 | 47 | 51 | |||
| 3 | 66 | 68 | 42 | 42 | |||
| PNB method | |||||||
| CFNB | 49 | NA | CFNB + SSFNB | 42 | NA | ||
| CACB | 89 | NA | CFNB + SSACB | 8 | NA | ||
| CACB + SSFNB | 21 | NA | |||||
| CACB + SSACB | 22 | NA | |||||
| CACB + CACB | 5 | NA | |||||
| PCA | |||||||
| IV | NA | 82 | NA | 54 | |||
| Epidural | NA | 56 | NA | 44 | |||
| PNB + IV | 138 | NA | 98 | NA | |||
| Anesthesia | 0.326 | 0.456 | |||||
| General | 50 | 58 | 53 | 44 | |||
| Spinal | 88 | 80 | 45 | 54 | |||
| UTKA | BTKAs | ||||||
|---|---|---|---|---|---|---|---|
| PNB Group (n = 138) | PCA Group (n = 138) | p-Value | PNB Group (n = 98) | PCA Group (n = 98) | p-Value | ||
| Hospital LOS | 5.3 ± 1.3 | 5.2 ± 0.8 | 0.173 | 5.3 ± 1.4 | 5.4 ± 1.5 | 0.630 | |
| AKS knee score | |||||||
| Preoperatively | 52.5 ± 15.6 | 52.9 ± 19.0 | 0.857 | 50.9 ± 11.3 | 50.6 ± 17.2 | 0.876 | |
| Postoperatively 3 M | 87.3 ± 17.7 | 84.0 ± 17.1 | 0.171 | 87.7 ± 16.7 | 89.6 ± 11.9 | 0.217 | |
| AKS function score | |||||||
| Preoperatively | 60.6 ± 16.7 | 55.3 ± 17.2 | 0.009 * | 60.1 ± 14.6 | 50.9 ± 20.1 | <0.001 * | |
| Postoperatively 3 M | 75.5 ± 18.2 | 73.4 ± 19.9 | 0.405 | 76.1 ± 15.7 | 75.5 ± 19.4 | 0.756 | |
| WOMAC | |||||||
| Preoperatively | 53.3 ± 18.7 | 52.7 ± 21.1 | 0.797 | 55.7 ± 19.5 | 54.4 ± 25.5 | 0.550 | |
| Postoperatively 3 M | 25.5 ± 25.2 | 26.7 ± 15.2 | 0.645 | 25.6 ± 22.6 | 25.8 ± 18.3 | 0.897 | |
| CFNB (n = 49) | CACB (n = 89) | p-Value | |
|---|---|---|---|
| 0–6 h Rest | 1 (0,4) | 2 (0,5) | 0.252 |
| 0–6 h Activity | 4.5 (2,7) | 5 (3,7) | 0.208 |
| 6–24 h Rest | 2.5 (0,5) | 3 (1,5) | 0.152 |
| 6–24 h Activity | 6 (4,7) | 6 (5,7) | 0.373 |
| 24–48 h Rest | 2 (0,4) | 2 (0,3) | 0.613 |
| 24–48 h Activity | 5 (3,6) | 6 (4,7) | 0.138 |
| CFNB + SSFNB (n = 42) | CFNB + SSACB (n = 8) | CACB + SSFNB (n = 21) | CACB + SSACB (n = 22) | CACB + CACB (n = 5) | p-Value | |
|---|---|---|---|---|---|---|
| 0–6 h Rest | 3 (0,4) | 3.5 (1,5) | 2 (0,5) | 2.5 (0,5) | 6 (2,8) | 0.533 |
| 0–6 h Activity | 6 (3,7) | 5 (4,7.5) | 7 (3,8) | 4.5 (3,8) | 8 (6,9) | 0.302 |
| 6–24 h Rest | 2 (0,5) | 3 (0,6.5) | 5 (3,6) | 3 (2,6) | 6 (3,8) | 0.008 * |
| 6–24 h Activity | 6 (5,7) | 6 (4,8) | 7 (6,8) | 6.5 (5,8) | 8 (7,9) | 0.058 |
| 24–48 h Rest | 2 (0,3) | 1 (0,3.5) | 4 (2,5) | 2 (0,3) | 3 (3,3) | 0.010 * |
| 24–48 h Activity | 6 (5,7) | 4.5 (3,6.5) | 6 (5,7) | 5 (3,7) | 6 (5,6) | 0.617 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, H.H.; Kwon, H.M.; Lee, W.-S.; Yang, I.H.; Choi, Y.S.; Park, K.K. Effectiveness of ERAS (Enhanced Recovery after Surgery) Protocol via Peripheral Nerve Block for Total Knee Arthroplasty. J. Clin. Med. 2022, 11, 3354. https://doi.org/10.3390/jcm11123354
Lee HH, Kwon HM, Lee W-S, Yang IH, Choi YS, Park KK. Effectiveness of ERAS (Enhanced Recovery after Surgery) Protocol via Peripheral Nerve Block for Total Knee Arthroplasty. Journal of Clinical Medicine. 2022; 11(12):3354. https://doi.org/10.3390/jcm11123354
Chicago/Turabian StyleLee, Hyun Hee, Hyuck Min Kwon, Woo-Suk Lee, Ick Hwan Yang, Yong Seon Choi, and Kwan Kyu Park. 2022. "Effectiveness of ERAS (Enhanced Recovery after Surgery) Protocol via Peripheral Nerve Block for Total Knee Arthroplasty" Journal of Clinical Medicine 11, no. 12: 3354. https://doi.org/10.3390/jcm11123354
APA StyleLee, H. H., Kwon, H. M., Lee, W.-S., Yang, I. H., Choi, Y. S., & Park, K. K. (2022). Effectiveness of ERAS (Enhanced Recovery after Surgery) Protocol via Peripheral Nerve Block for Total Knee Arthroplasty. Journal of Clinical Medicine, 11(12), 3354. https://doi.org/10.3390/jcm11123354






