Efficacy and Safety of Micropulse Transscleral Cyclophotocoagulation
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Procedure
2.3. Assessment of Outcomes
2.4. Statistical Analyses
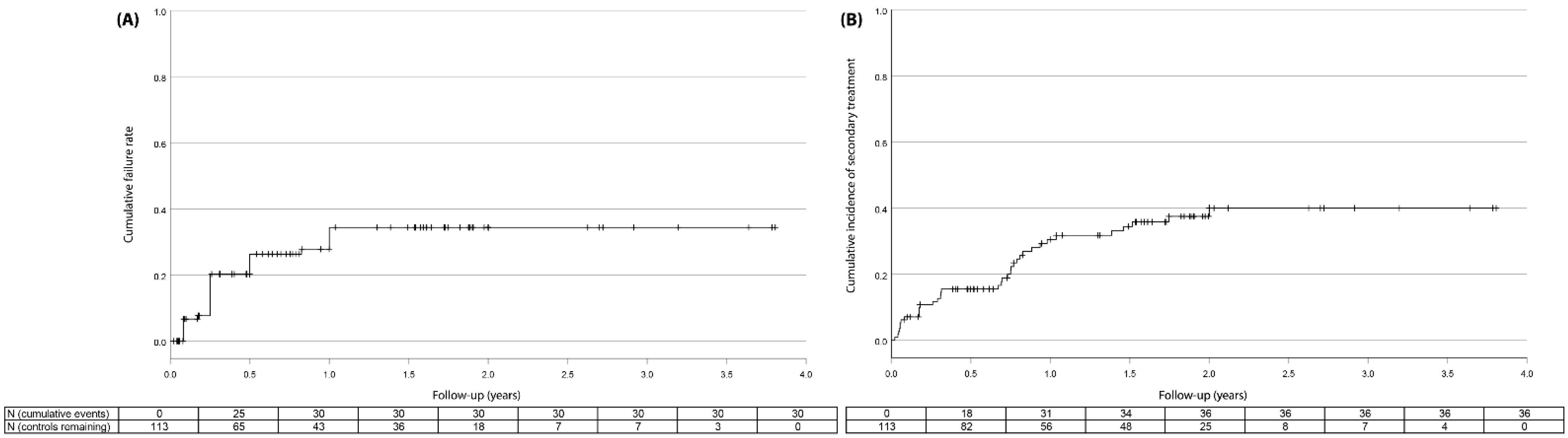
3. Results
4. Discussion
4.1. Summary of Findings
4.2. Relationship with Literature
4.3. Strength and Weaknesses
4.4. Role in Glaucoma Practice
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Hertzog, L.H.; Albrecht, K.G.; LaBree, L.; Lee, P.P. Glaucoma Care and Conformance with Preferred Practice Patterns. Examination of the private, community-based ophthalmologist: Examination of the private, community-based ophthalmologist. Ophthalmology 1996, 103, 1009–1013. [Google Scholar] [CrossRef]
- Gazzard, G.; Konstantakopoulou, E.; Garway-Heath, D.; Garg, A.; Vickerstaff, V.; Hunter, R.; Ambler, G.; Bunce, C.; Wormald, R.; Nathwani, N.; et al. Selective laser trabeculoplasty versus eye drops for first-line treatment of ocular hypertension and glaucoma (LiGHT): A multicentre randomised controlled trial. Lancet 2019, 393, 1505–1516. [Google Scholar] [CrossRef] [Green Version]
- Yadav, K.S.; Sharma, S. Implantable drainage devices in glaucoma: Quo vadis? Eur. J. Pharm. Sci. 2019, 133, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Weinreb, R.N.; Aung, T.; Medeiros, F.A. The Pathophysiology and Treatment of Glaucoma: A review. JAMA 2014, 311, 1901–1911. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chen, M.F.; Kim, C.H.; Coleman, A.L. Cyclodestructive procedures for refractory glaucoma. Cochrane Database Syst. Rev. 2016, 3, CD012223. [Google Scholar] [CrossRef]
- Vinod, K.; Gedde, S.J. Safety profile of minimally invasive glaucoma surgery. Curr. Opin. Ophthalmol. 2021, 32, 160–168. [Google Scholar] [CrossRef]
- Bloom, P.A.; Tsai, J.C.; Sharma, K.; Miller, M.H.; Rice, N.S.; Hitchings, R.A.; Khaw, P.T. “Cyclodiode”: Trans-scleral diode laser cyclophotocoagulation in the treatment of advanced refractory glaucoma. Ophthalmology 1997, 104, 1508–1520. [Google Scholar] [CrossRef]
- Ramli, N.; Htoon, H.M.; Ho, C.L.; Aung, T.; Perera, S. Risk Factors for Hypotony after Transscleral Diode Cyclophotocoagulation. J. Glaucoma 2012, 21, 169–173. [Google Scholar] [CrossRef]
- Tan, A.M.; Chockalingam, M.; Aquino, M.C.; Lim, Z.I.-L.; See, J.L.-S.; Chew, P.T. Micropulse transscleral diode laser cyclophotocoagulation in the treatment of refractory glaucoma. Clin. Exp. Ophthalmol. 2010, 38, 266–272. [Google Scholar] [CrossRef]
- Aquino, M.C.D.; Barton, K.; Tan, A.M.W.T.; Sng, C.; Li, X.; Loon, S.C.; Chew, P.T.K. Micropulse versus continuous wave transscleral diode cyclophotocoagulation in refractory glaucoma: A randomized exploratory study. Clin. Exp. Ophthalmol. 2015, 43, 40–46. [Google Scholar] [CrossRef]
- Kuchar, S.; Moster, M.R.; Reamer, C.B.; Waisbourd, M. Treatment outcomes of micropulse transscleral cyclophotocoagulation in advanced glaucoma. Lasers Med. Sci. 2015, 31, 393–396. [Google Scholar] [CrossRef] [PubMed]
- Yelenskiy, A.; Gillette, T.B.; Arosemena, A.; Stern, A.G.; Garris, W.J.; Young, C.T.; Hoyt, M.; Worley, N.; Zurakowski, D.; Ayyala, R.S. Patient Outcomes Following Micropulse Transscleral Cyclophotocoagulation: Intermediate-term Results. J. Glaucoma 2018, 27, 920–925. [Google Scholar] [CrossRef] [PubMed]
- Zaarour, K.; Abdelmassih, Y.; Arej, N.; Cherfan, G.; Tomey, K.F.; Khoueir, Z. Outcomes of Micropulse Transscleral Cyclophotocoagulation in Uncontrolled Glaucoma Patients. J. Glaucoma 2019, 28, 270–275. [Google Scholar] [CrossRef] [PubMed]
- Poelman, H.; Pals, J.; Rostamzad, P.; Bramer, W.M.; Wolfs, R.C.W.; Ramdas, W.D. Efficacy of the XEN-Implant in Glaucoma and a Meta-Analysis of the Literature. J. Clin. Med. 2021, 10, 1118. [Google Scholar] [CrossRef] [PubMed]
- Kovacic, H.; Wolfs, R.C.W.; Kılıç, E.; Ramdas, W.D. Changes in intraocular pressure after intraocular eye surgery-the influence of measuring technique. Int. J. Ophthalmol. 2019, 12, 967–973. [Google Scholar] [CrossRef]
- Heuer, D.K.; Barton, K.; Grehn, F.; Shaarawy, T.M.; Sherwood, M.B. Consensus on definitions of success. In Guidelines on Design and Reporting of Surgical Trials; Shaarawy, T.M., Sherwood, M.B., Grehn, F., Eds.; Kugler Publications: Amsterdam, The Netherlands, 2008. [Google Scholar]
- de Crom, R.M.P.C.; Slangen, C.G.M.M.; Kujovic-Aleksov, S.; Webers, C.A.B.; Berendschot, T.T.J.M.; Beckers, H.J.M. Micropulse Trans-scleral Cyclophotocoagulation in Patients With Glaucoma: 1- and 2-Year Treatment Outcomes. J. Glaucoma 2020, 29, 794–798. [Google Scholar] [CrossRef]
- Sanchez, F.G.; Peirano-Bonomi, J.C.; Grippo, T.M. Micropulse Transscleral Cyclophotocoagulation: A Hypothesis for the Ideal Parameters. Med. Hypothesis Discov. Innov. Ophthalmol. 2018, 7, 94–100. [Google Scholar]
- Nguyen, A.T.; Maslin, J.; Noecker, R.J. Early results of micropulse transscleral cyclophotocoagulation for the treatment of glaucoma. Eur. J. Ophthalmol. 2020, 30, 700–705. [Google Scholar] [CrossRef]
- Sarrafpour, S.; Saleh, D.; Ayoub, S.; Radcliffe, N.M. Micropulse Transscleral Cyclophotocoagulation: A Look at Long-Term Effectiveness and Outcomes. Ophthalmol. Glaucoma 2019, 2, 167–171. [Google Scholar] [CrossRef]
- van der Valk, R.; Webers, C.A.B.; Schouten, J.S.A.G.; Zeegers, M.P.; Hendrikse, F.; Prins, M.H. Intraocular Pressure-Lowering Effects of All Commonly Used Glaucoma Drugs: A Meta-analysis of Randomized Clinical Trials. Ophthalmology 2005, 112, 1177–1185. [Google Scholar] [CrossRef]
- Poelman, H.J.; Wolfs, R.C.; Ramdas, W.D. The Baerveldt Glaucoma Drainage Device: Efficacy, Safety, and Place in Therapy. Clin. Ophthalmol. 2020, 14, 2789–2797. [Google Scholar] [CrossRef] [PubMed]
- Yamashita, H.; Sears, M. Proof that the ciliary epithelium can regenerate. Exp. Eye Res. 1978, 27, 199–213. [Google Scholar] [CrossRef]


| Eyes (N, Patients) | 96 (84) |
| Treatments (N, secondary treatments) | 114 (18) |
| Age (years) | 65.7 ± 14.0 |
| Sex, female (N, %) | 42 (44) |
| Caucasian descent (N, %) | 90 (79) |
| Glaucoma etiology, (N, %) | |
| Primary | 51 (53) |
| Neovascular | 13 (14) |
| Uveitis | 14 (15) |
| Trauma | 2 (2) |
| Postvitrectomy | 3 (3) |
| Complicated phaco procedure | 2 (2) |
| Pseudoexfoliation syndrome (PEX) | 1 (1) |
| Pigment dispersion syndrome (PDS) | 2 (2) |
| Other | 9 (8) |
| Untreated IOP at time of diagnosis (mmHg) | 27.5 ± 12.2 |
| Baseline IOP (mmHg) | 26.6 ± 10.8 |
| Number of IOP-lowering medications | 3.4 ± 1.3 |
| Visual acuity (LogMar) | 0.4 ± 0.4 |
| Spherical equivalent (D) * | −1.7 ± 2.5 |
| Central corneal thickness (µm) | 528 ± 47 |
| Visual field mean deviation (MD; dB) | −19.38 ± 11.23 |
| Visual field pattern standard deviation (PSD; dB) | 8.00 ± 3.21 |
| Positive family history (N, %) | 24 (25) |
| Prior glaucoma surgery (N, %) ** | 26 (27) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
de Vries, V.A.; Pals, J.; Poelman, H.J.; Rostamzad, P.; Wolfs, R.C.W.; Ramdas, W.D. Efficacy and Safety of Micropulse Transscleral Cyclophotocoagulation. J. Clin. Med. 2022, 11, 3447. https://doi.org/10.3390/jcm11123447
de Vries VA, Pals J, Poelman HJ, Rostamzad P, Wolfs RCW, Ramdas WD. Efficacy and Safety of Micropulse Transscleral Cyclophotocoagulation. Journal of Clinical Medicine. 2022; 11(12):3447. https://doi.org/10.3390/jcm11123447
Chicago/Turabian Stylede Vries, Victor. A., Jan Pals, Huub J. Poelman, Parinaz Rostamzad, Roger C. W. Wolfs, and Wishal D. Ramdas. 2022. "Efficacy and Safety of Micropulse Transscleral Cyclophotocoagulation" Journal of Clinical Medicine 11, no. 12: 3447. https://doi.org/10.3390/jcm11123447
APA Stylede Vries, V. A., Pals, J., Poelman, H. J., Rostamzad, P., Wolfs, R. C. W., & Ramdas, W. D. (2022). Efficacy and Safety of Micropulse Transscleral Cyclophotocoagulation. Journal of Clinical Medicine, 11(12), 3447. https://doi.org/10.3390/jcm11123447






