Central Giant Cell Granuloma in the Mandibular Condyle in a Teenager. A Case Report with Literature Review
Abstract
:1. Introduction
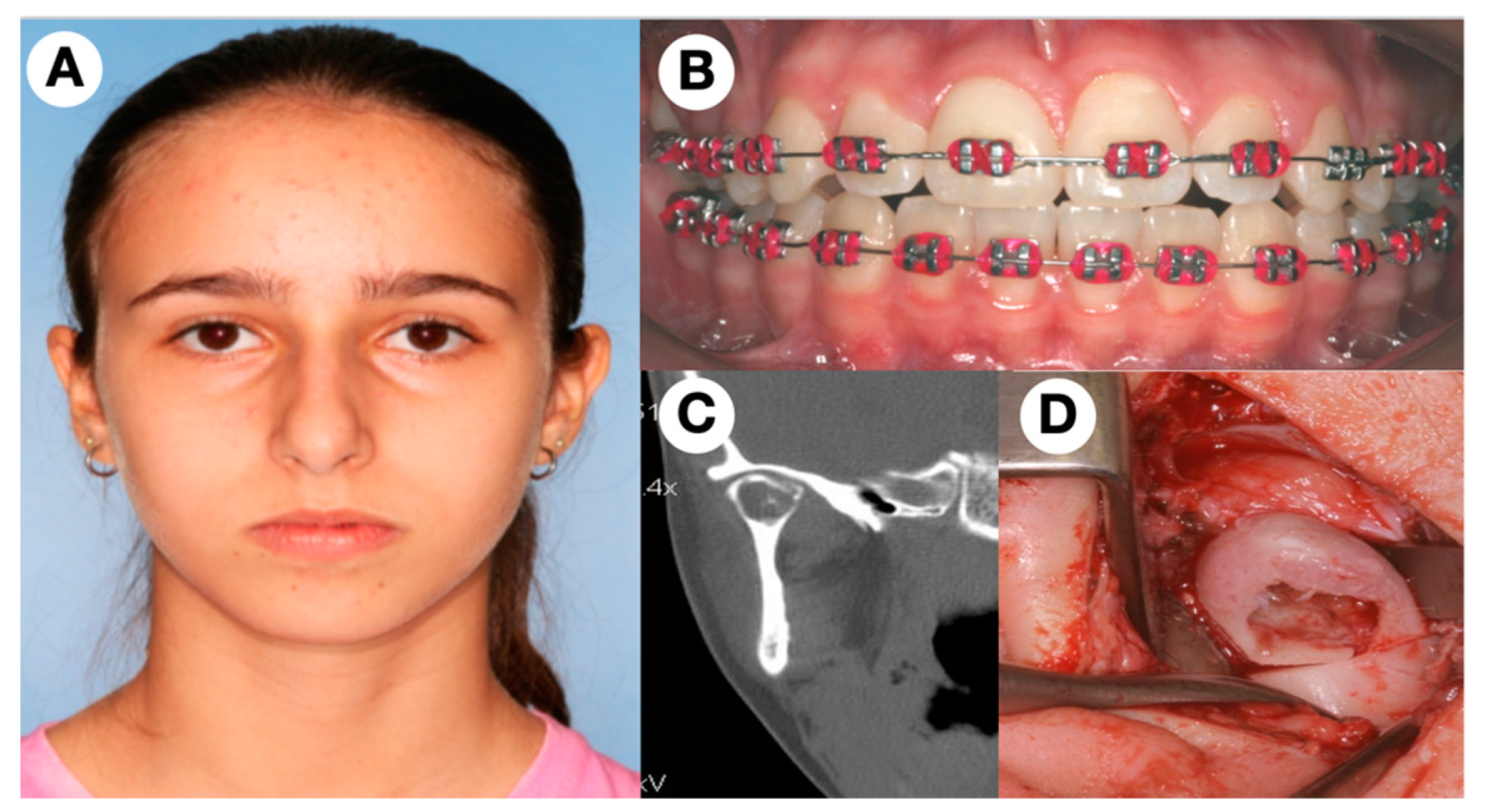
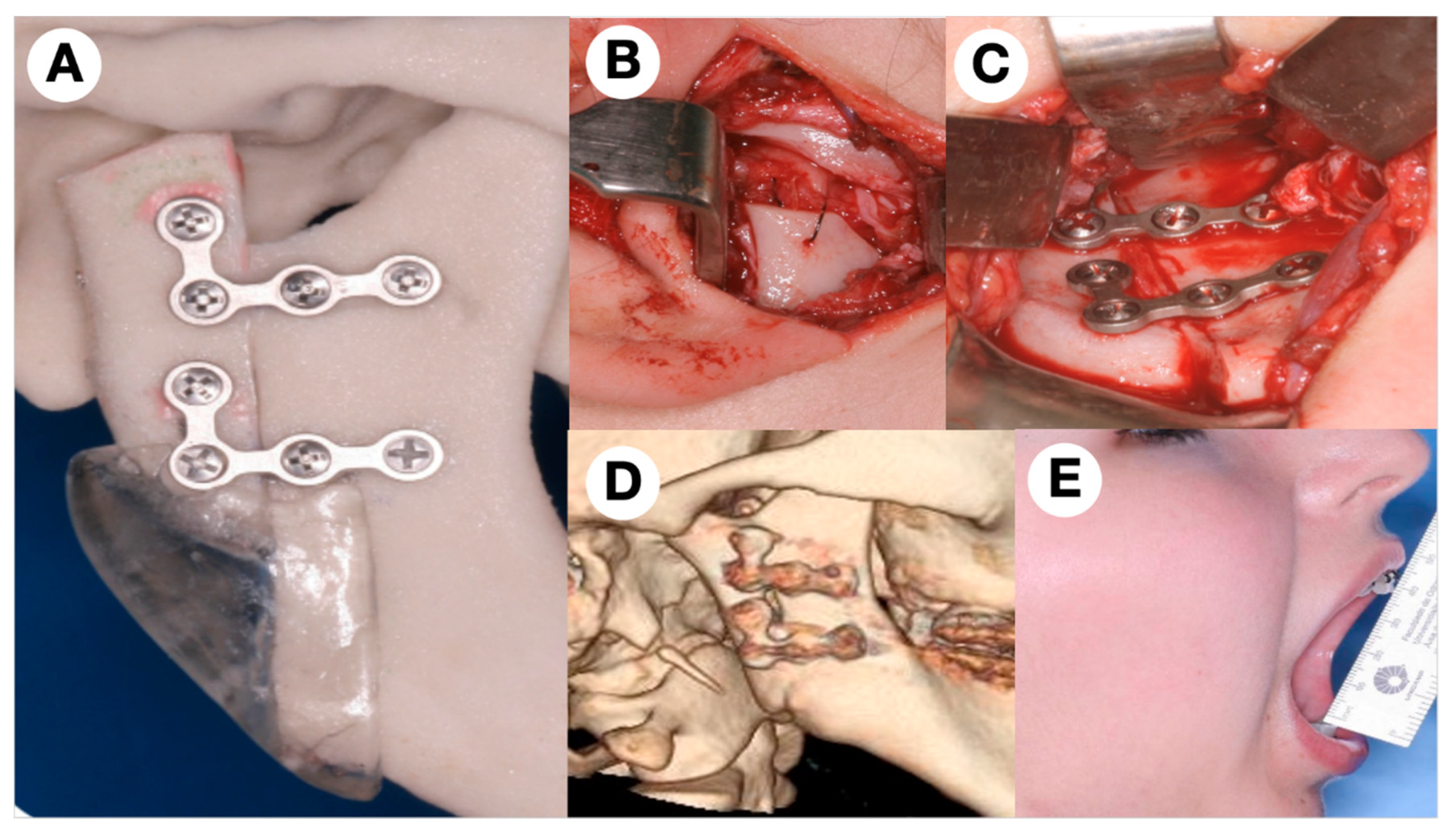
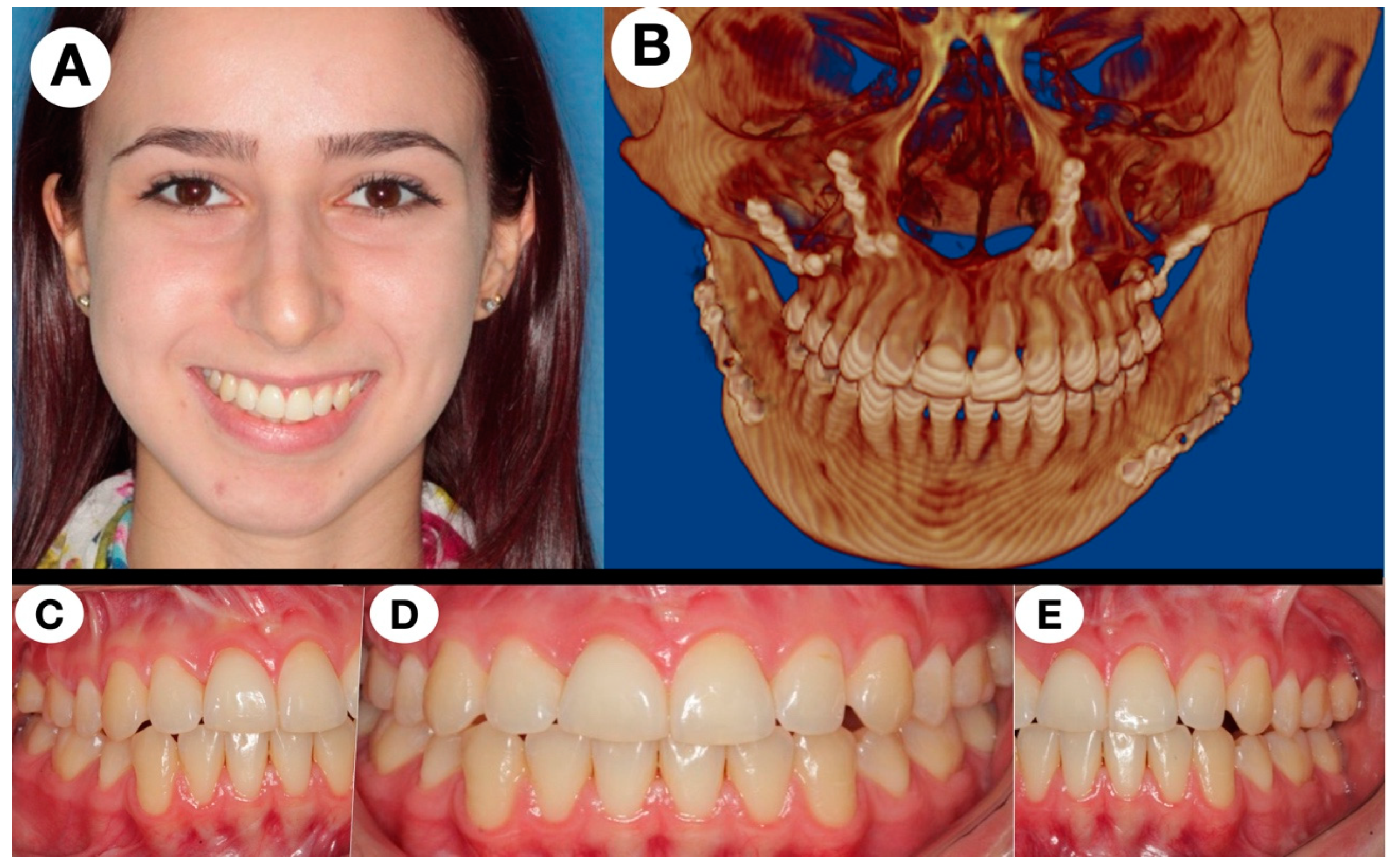
2. The Subject
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ozcan, C.; Apaydın, F.D.; Gorur, K.; Apa, D.D. Peripheral giant cell granuloma of the mandibular condyle presenting as a preauricular mass. Eur. Arch. Otorhinolaryngol. 2005, 262, 178–181. [Google Scholar] [CrossRef] [PubMed]
- Jadu, F.M.; Pharoah, M.J.; Lee, L.; Baker, G.I.; Allidina, A. Central giant cell granuloma of the mandibular condyle: A case report and review of the literature. Dentomaxillofac. Radiol. 2011, 40, 60–64. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Khanna, J.N.; Ramaswami, R.; Shah, M. Giant cell reparative granuloma of mandibular condyle—A case report. J. Oral Maxillofac. Surg. Med. Pathol. 2018, 30, 515–518. [Google Scholar] [CrossRef]
- Bocchialini, G.; Salvagni, L.; Guerini, A.; Castellani, A. Central giant cell granuloma of the mandibular condyle: A rare case and a literature review. Heliyon 2020, 6, e03085. [Google Scholar] [CrossRef] [Green Version]
- Abu-El-Naaj, I.; Ardekian, L.; Liberman, R.; Peled, M. Central giant cell granuloma of the mandibular condyle: A rare presentation. J. Oral. Maxillofac. Surg. 2002, 60, 939–941. [Google Scholar] [CrossRef]
- Munzenmayer, J.; Tapia, P.; Zeballos, J.; Martínez, A.; Compan, Á.; Urra, A.; Spencer, M.L. Central giant cell granuloma of the mandibular condyle. Case-report. Rev. Clin. Periodoncia Implantol. Rehabil. Oral. 2013, 6, 83–86. [Google Scholar]
- Chang, C.S.; Hsiao, Y.C.; Huang, F.; Chen, P.K.T.; Chen, J.P.; Noordhoff, M.S. Giant cell reparative granuloma of the mandibular condyle: A long-term case report and review of the literature. Plast. Surg. Case Stud. 2016, 2, 44–46. [Google Scholar] [CrossRef]
- Pai, D.; Kamath, A.T.; Kudva, A.; Solomon, M.M.C.; Kumar, S.; Sasikumar, P. Concomitant central giant cell granuloma and Aneurismal Bone Cyst in a Young Child. Case reports in dentistry. Case Rep. Dent. 2017, 2017, 6545848. [Google Scholar] [CrossRef]
- Chuong, R.; Kaban, L.B.; Kozakewich, H.; Perez-Atayde, A. Central Giant Cell Lesions of the Jaws: A Clinicopathologic Study. J. Oral. Maxillofac. Surg. 1986, 44, 708–713. [Google Scholar] [CrossRef]
- Tasanen, A.; von Konow, L.; Nordling, S. Central giant cell lesion in the mandibular condyle: Report of a case. Oral. Surg. Oral. Med. Oral. Pathol. 1978, 45, 532. [Google Scholar] [CrossRef]
- Shensa, D.R.; Nasseri, S. Centeral giant cell reparative granuloma of the mandibular condyle. J. Oral. Surg. 1978, 36, 642. [Google Scholar]
- Sun, Z.J.; Cai, Y.; Zwahlen, R.A.; Zheng, Y.F.; Wang, S.P.; Zhao, Y.Z. Central giant cell granuloma of the jaws: Clinical and radiological evaluation of 22 cases. Skeletal Radiol. 2009, 38, 903–909. [Google Scholar] [CrossRef] [PubMed]
- Gigliotti, J.; Alghamdi, O.; El-Hakim, M.; Makhoul, N. Central giant cell granuloma of the mandibular condyle: A case report, literature review, and discussion of treatment. Oral. Maxillofac. Surg. Cases 2015, 1, 42–46. [Google Scholar] [CrossRef] [Green Version]
- Camarini, C.; Tolentino, E. Non-surgical treatment as an alternative for the management of central giant cell granuloma: A systematic review. Clin. Oral. Investig. 2022, 26, 2111–2132. [Google Scholar] [CrossRef] [PubMed]
- Lin, J.; Mecham, J.C.; Ryan Hall, S.; Oh, C.; Lettieri, S. Padiatric mandibular central giant cell granuloma: Neoadjuvant immunotherapy to minimize surgical resection. J. Craniofac. Surg. 2021, 32, e267–e269. [Google Scholar] [CrossRef]
- Nilesh, K.; Dadhich, A.; Patil, R. Management of recurrent central giant cell granuloma of mandible using intralesional corticosteroid with long-term follow-up. BMJ Case Rep. 2020, 14, e237200. [Google Scholar] [CrossRef]
- Lipplaa, A.; Dijkstra, S.; Gelderblom, H. Challenge of denosumab in giant cell tumor of bone, and other giant cell-rich tumors of bone. Curr. Opin. Oncol. 2019, 31, 329–335. [Google Scholar] [CrossRef]
- Dolanmaz, D.; Esen, A.; Mihmanll, A.; Isik, K. Management of central giant cell granuloma of the jaws with intralesional steroid injection and review of the literature. Oral. Maxillofac. Surg. 2016, 20, 203–209. [Google Scholar] [CrossRef]
- Rasband-Lindquist, A.N.; Lindquist, J.D.; Larsen, C.; Thiessen, A.; Girod, D. Nonsurgical options to treat giant-cell tumors of the head and neck: A case report and brief review of the literature. Ear Nose Throat J. 2016, 95, E29–E34. [Google Scholar]
- Costello, B.J.; Rivera, R.; Shand, J.; Mooney, M. Growth and development considerations for craniomaxillofacial surgery. Oral Maxillofac. Surg. Clin. N. Am. 2012, 24, 377–396. [Google Scholar] [CrossRef]
- Resnick, C. Temporomandibular joint reconstruction in growing child. Oral Maxillofac. Surg. Clin. N. Am. 2018, 30, 109–121. [Google Scholar] [CrossRef] [PubMed]
- Parmar, B.S.; Garg, B.; Mehta, R.D.; Midha, A.; Thakkar, D. Ramus condyle unit reconstruction using vertical ramus osteotomy in the temporomandibular joint ankylosis. J. Maxillofac. Oral Surg. 2015, 14, 630–636. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Al-Moraissi, E.A.; El-Sharkawy, T.M.; Mounair, R.M.; El-Ghareeb, T.I. A systematic review and meta-analysis of the clinical outcomes for various surgical modalities in the management of temporomandibular joint ankylosis. Int. J. Oral Maxillofac. Surg. 2015, 44, 470–482. [Google Scholar] [CrossRef] [PubMed]
- De Meurechy, N.; Mommaerts, M.Y. Alloplastic temporomandibular joint replacement systems: A systematic review of their history. Int. J. Oral. Maxillofac. Surg. 2018, 47, 743–754. [Google Scholar] [CrossRef] [PubMed]
- Mercuri, L.G. Patient-fitted (“custom”) alloplastic temporomandibular joint replacement technique. Atlas Oral Maxillofac. Surg. Clin. N. Am. 2011, 19, 233–242. [Google Scholar] [CrossRef]
- Bach, E.; Sigaux, N.; Fauvernier, M.; Cousin, A.-S. Reason for failure of total temporomandibular joint replacement: A systematic review and meta-analysis. Int. J. Oral Maxillofac. Surg. 2022, in press. [Google Scholar] [CrossRef]
- Sidebottom, A. Alloplastic or autogenous reconstruction of the TMJ. J. Oral Biol. Craniofac. Res. 2013, 3, 135–139. [Google Scholar] [CrossRef] [Green Version]

| Author/Year | Age/Sex | Clinical Findings | Imaging | Treatment | Follow-Up |
|---|---|---|---|---|---|
| Tasanen et al. (1978) [10] | 59/M | Right painless slow-growing pre-auricular swelling. Mouth-opening limitation | Well-defined multilocular radiolucency—25 mm (right condyle) | Resection + reconstruction with CCG | 21 months NRD |
| Shensa/Nasseri, (1978) [11] | 15/M | Expansive mass. Asymptomatic | Well-defined radiolucency | Enucleation | NI |
| Abu-El-Naaj et al. (2002) [5] | 15/F | Left preauricular swelling (2 months). Asymptomatic. Normal mandibular motion | Well-defined unilocular radiolucency (3 × 2 cm), left condyle | Enucleation | 6 months NRD |
| Özcan et al. (2005) [1] | 44/F | Right preauricular swelling (2-year evolution). Pain | CT—hypodense 2 × 2 cm. MRI rim-like hypodense T1. Peripheral calcification | Curettage | 1 year NRD |
| Sun et al. (2009) [12] | NI (1 out of 22 cases) | Pain and tenderness | Well-defined radiolucency. Extending to the coronoid process | Curettage | NI |
| Jadu et al. (2011) [2] | 31/M | Painful slow-growing left pre-auricular swelling (2 years). Limited mouth opening | CT—Well defined, expansile (3.5 cm), with a granular bone pattern | Enucleation then resection after recurrence | 4 years NRD |
| Munzenmayer et al. (2013) [6] | 19/F | Asymptomatic. No occlusal or mandibular movement disorders | Well-defined multilocular radiolucency (4 × 2.2 × 1.5 cm), with granular bone pattern (left condyle) | Resection + reconstruction with NVFF | 2 years NRD |
| Gigliotti et al. (2015) [13] | 29/M | Firm and nodular left pre-auricular swelling (6 months). No occlusal changes. Discomfort during the mandibular function. | Left multilocular radiolucency with thin cortices 5.5 × 3.8 × 3.4 cm | Resection + reconstruction with CCG | 1 year NRD |
| Chang et al. (2016) [7] | 37/F | Hardened left pre-auricular mass 4 × 3 cm. Asymptomatic | Well-defined radiolucent and radiopaque areas involving two cortical in left condyle + ramus | Resection + reconstruction with CCG | 10 years NRD |
| Pai et al. (2017) [8] | 2/M | Progressive and firm increase in the right preauricular region. Painless. (4 months) | Expansive multinucleated radiolucent lesion (4.2 × 3.5 × 4 cm) with cortical perforation. | Resection + reconstruction with CCG | 18 months NRD |
| Khanna et al. (2018) [3] | 22/M | Right preauricular swelling (4 months). Pain and TMJ movements restricted | Large lesion extending to the coronoid with areas of cortical perforation at multiple places. | Resection + 2.4 mm reconstruction plate with condylar head | 1 year NRD |
| Bocchialini et al. (2020) [4] | 60/F | Right preauricular pain (1 year). Mouth-opening limitation. | A large radiolucent lesion with distortion of the right condyle | Enucleation | 1 year NRD |
| Present case | 11/F | No swellings, joint pain during mandibular motion (1 year) | Well-defined radiolucent lesion on the right mandible head | Resection + sliding vertical ramus osteotomy + later orthognathic surgery | 13 years NRD |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cantanhede, A.L.C.; Olate, S.; de Assis, A.F.; de Moraes, M. Central Giant Cell Granuloma in the Mandibular Condyle in a Teenager. A Case Report with Literature Review. J. Clin. Med. 2022, 11, 4239. https://doi.org/10.3390/jcm11144239
Cantanhede ALC, Olate S, de Assis AF, de Moraes M. Central Giant Cell Granuloma in the Mandibular Condyle in a Teenager. A Case Report with Literature Review. Journal of Clinical Medicine. 2022; 11(14):4239. https://doi.org/10.3390/jcm11144239
Chicago/Turabian StyleCantanhede, André Luís Costa, Sergio Olate, Adriano Freitas de Assis, and Márcio de Moraes. 2022. "Central Giant Cell Granuloma in the Mandibular Condyle in a Teenager. A Case Report with Literature Review" Journal of Clinical Medicine 11, no. 14: 4239. https://doi.org/10.3390/jcm11144239
APA StyleCantanhede, A. L. C., Olate, S., de Assis, A. F., & de Moraes, M. (2022). Central Giant Cell Granuloma in the Mandibular Condyle in a Teenager. A Case Report with Literature Review. Journal of Clinical Medicine, 11(14), 4239. https://doi.org/10.3390/jcm11144239







