Intrusion of Maxillary Posterior Teeth by Skeletal Anchorage: A Systematic Review and Case Report with Thin Alveolar Biotype
Abstract
:1. Introduction
2. Materials and Methods
2.1. Information Sources
2.2. Search Strategy
3. Results
3.1. Data Collection
3.2. Description of the Studies
| Author, Publication Year | Country | IA | Sample Size, Age Range, Gender | Anchorage Type | IMM | IR | IF | TT | Outcomes | Side Effects | Conclusions |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Akan B et al., 2020 [27] | Turkey | AOB | 19 patients, (5 boys, 14 girls) 16.5 years | ZP, bilateral, acrylic appliance | LC | 2.32 ± 2.13 mm | 400 g, NiTi close coil springs | 9.4 ± 0.7 months | U6 to PP occlusal plane OB anterior facial height | NA | “posterior dentoalveolar intrusion by zygomatic anchorage was an effective method for anterior open bite treatment” |
| Akl HE et al., 2020 [28] | Egypt | AOB | Intervention group: 10 subjects Control group: 10 subjects 18 to 25 years | 4 MS: 2 infrazygomatic and 2 palatal | CBCT | Intervention group: 2.26 ± 1.87 mm Control group: 2.42 ± 2.06 mm | intervention group: 400 g NiTi closed coil springs control group: 200 g | 6 months | U6 T or PM center to FH OB | Soft tissue overgrowth loose of two miniscrews | “no statistically significant difference in the amount of posterior teeth intrusion between 200 g and 400 g of applied intrusive force” “amount of intrusion increased gradually as the tooth was located more posteriorly, closer to the line of traction” |
| Al-Falahi B et al., 2018 [29] | Egypt | AOB | 15 patients (13 females and 2 males), 14.5 to 22 years (mean age 18.1 ± 2.03 years) | MS, buccal | CBCT | 2.79 ± 0.46 mm | 300 g, elastomeric chain | 5.1 ± 1.3 months | U6 to PP | EARR | “all evaluated teeth had statistically significant EARR; but, because of its small magnitude, it should be considered as clinically irrelevant” |
| Ari-Demirkaya A et al., 2005 [30] | Turkey | AOB | Study group: 16 (13 females, 3 males) 19.25 years (range 14–26 years) subjects control group: 16 subjects 19.43 years (range 14–25 years) | ZP | PR | NA | NA, closed Ni-Ti coil springs | NA | U6 tooth length | EARR | “apical root resorption of maxillary first molars after intrusion was done using zygomatic miniplates as skeletal anchorage was not clinically significantly different from apical root resorption associated with fixed orthodontic treatment without intrusion mechanics” |
| Ding WH et al., 2015 [31] | China | AOB | 36 patients: 18 hyperdivergent 18 hypodivergent females (aged 20–42 years (28.93 ± 7.55 | MS, buccal | CBCT | Hyperdivergent: 4.57 mm ± 0.98 Hypodivergent: 3.64 mm ± 1.25 | 100 g, elastomeric chains | Hyperdivergent: 3.13 months ± 0.90 Hypodivergent: 4.71 months ± 1.50 | Difference of U6 distal buccal cusp-FH plane (DB-FH) + mesial buccal cusp-FH plane (MB-FH)/2 | Miniscrew implants loose difference and change of bone during intrusion | “absolute molar intrusion could be achieved by miniscrew implant... more easily in hyperdivergent” |
| Heravi F et al., 2011 [32] | Iran | AOB | 10 females (mean age 43.6 years, range 25 to 57 years) | MS, buccal, and palatal | Parallel periapical radiographs | 2.1 ± 0.9 mm | 100 g, occlusal arm with a force gauge hook | 7.7 months (range: 4.3 to 11.5 months) | A reference axis of 2 landmarks in adjacent teeth a perpendicular line from this axis to each root apex | Dull pain on the day after surgery tongue irritation root resorption (mean 0.2 mm) intrusion relapse | “there was a significant correlation between treatment duration and mesiobuccal root resorption. No significant correlation was found between patient age and the amount of root resorption and intrusion” |
| Kim K et al., 2018 [33] | Korea | AOB | 21 patients (3 men, 18 women); mean age 23.9 years (range 18.5– 36.4) | MS, buccal, and palatal | LC | 2.2 ± 0.8 mm | NA | 9.7 ± 3.2 months (range, 6.2–15.2 months) | U6 to PP | NA | “mandible exhibited counterclockwise rotation after maxillary molar intrusion; the center of mandibular autorotation was located behind and below condylion with individual variations” “the amount of molar intrusion demonstrated relationships with vertical and sagittal cephalometric parameters” |
| Li W et al., 2013 [34] | China Australia | OVE U6 | 12 patients (4 male; 8 female) 18 to 32 years, mean age: 24.3 ± 1.26 years | MS, buccal, and palatal | CBCT | 3.3 ± 1.6 mm | 150 g, elastic chain | 6 ± 1.59 months; range: 4 to 9 months | Crown’s central fossa to reference plane | Root resorption | “volume measurements using CBCT could effectively evaluate the root resorption caused by mini-screw intrusion” |
| Marzouk ES et al., 2015 [35] | Egypt | AOB | 13 patients (9 females; 4 males) mean age 18 years, 8 months ± 2 years, 2 months | ZP | LC | 3.1 ± 0.74 mm (range: 2–4 mm) | 450 g, NiTi closed coil spring | 9 ± 2.5 months | U6 to PP | NA | “intrusion of the posterior teeth with skeletal anchorage induced counterclockwise rotation of the mandible” |
| de Oliveira TFM et al., 2015 [36] | Brazil | AOB | 9 patients (6 females, 3 males; mean age 18.7 ± 5.1 years) | ZP | LC oblique radiographs at 45° | 2.03 ± 0.87 mm | 450–500 g, elastomeric chains | 6 months | Anteroposterior position of the molar cusp and root apex The vertical position of the molar cusp and root apex | Possible root resorption | “skeletal anchorage provided intrusion of molars without changing the palatal plane angle” |
| Paccini JV et al., 2016 [37] | Brazil | OVE U6 | 19 patients (4 males, 15 females) Group 1: mean age 34.25 years ± 8.22 (range: 22.66–46.99) Group 2: mean age 39.47 years ± 8.12 (range: 21.07–47.44) | MS group 1: 2 MS: 1 buccal,1 palatal group 1: 3 MS: 2 buccal,1 palatal | LC | Group 1: 1.79 ± 1.28 mm Group 2: 2.12 ± 1.25 mm | 150 g, elastomeric chain | Group 1: 0.81 years ± 0.5 (range 0.41–1.64 years) Group 2: 1.17 years ± 0.48 (range 0.75–2.14 years) | U6 to PP U6 to SN OB | NA | “protocols of maxillary molar intrusion with two or three mini-implants presented the same efficiency of skeletal anchorage” |
| Pinzan-Vercelino CRM et al., 2015 [38] | Brazil | PP | 9 patients (7 females, 2 males) mean age 37.17 years (range: 28.5–46.41 | MS, buccal, and palatal | LC | Mean 2.4 mm (range: 1.2–4.5 mm) | NA | 9.03 ± 4.04 months (range: 3.16–16.23 months) | U6 to PP | NA | “orthodontic intrusion using direct anchorage of mini-implants was an effective method for the intrusion of maxillary molars” |
| Scheffler NR et al., 2014 [39] | USA | AOB | 30 patients (11 male and 19 female) | 16 patients MS, buccal 14 patients ZP | LC | 2.3 mm | NA, NiTi coil springs occlusal splint | Anterior face height mandibular plane angle OB | relapse no failures of miniplate anchorage 1 loose MS 1 MS fell out | “intrusion of the maxillary posterior teeth can give satisfactory correction of moderately severe anterior open bites, but 0.5 to 1.5 mm of reeruption of these teeth is likely to occur” | |
| Seres L, Kocsis A, 2009 [40] | Hungary | AOB | 7 patients (4 women and 3 men), mean age 21 years (range, 15–29 years) | ZP | LC, PR, periapical radiographs | NA | 100 to 120 g, NiTi closed coil springs | 6 months | Mandibular plane closed Point B rotated anteriorly and upward | Mild discomfort after surgery No signs or symptoms of a temporomandibular dysfunction were observed, No miniplate movement was detected no significant root resorption | ” skeletal anterior open bites due to posterior maxillary dentoalveolar hyperplasia can be closed without orthognathic surgery” |
| Sherwood K.H. et al., 2002 [41] | USA | AOB | 4 patients (2 men and 2 women) | ZP | LC, PR | Mean: 1.99 mm Range: 1.45–3.32 | Coated elastic thread | 5.5 months | 2 measurement lines on PR anterior facial height mandibular plane occlusal plane | No discernable movement of any miniplate | “true intrusion of molars can be accomplished in adults” “Anterior open bites can be closed by intruding posterior teeth, resulting in reduced anterior vertical face height, decreased mandibular plane angle, and counterclockwise rotation of the mandible” |
| Turkahraman H., Sarioglu M, 2016 [42] | Turkey | AOB | 40 patients: 20 treatment group (14 female, 6 male) mean age: 16.68 ± 2.80 years 20 control group (11 female, 9 male) mean age: 16.63 ± 2.83 years | ZP | LC | Treatment group: 3.59 ± 1.34 mm control group: 0.51 ± 0.44 mm | 200 g Ni-Ti coil springs | Treatment group: 1.00 ± 0.31 years control group: 0.95 ± 0.14 years | U6 to PP | Mesial movement of the molars by 1.52 mm was found in the treatment group | “mild to moderate skeletal anterior open bites could easily be treated with TADs without orthognathic surgery. With the rigid anchorage of mini plates, true molar intrusion was achieved” |
| Xun CL et al., 2013 [43] | China | OVE U6 | 30 patients 35.5 ± 9.0 years (range 19 to 50) | MS | LC. PR | 3.4 mm (range 1.5 to 6.5 mm) | 100–150 g, elastic chain | 6.2 ± 2.1 months | U6 to PP | Crown of the molars mesially tilted by averages of 3.1 degrees root resorption 0.2–0.4 mm on average | “intrusion treatment of over erupted molars with miniscrew anchorages could be used as an efficient and reliable method to recover lost restoration space for prosthesis” |
| Yao CC, et al., 2005 [3] | Taiwan | OVE U6 | 22 patients mean age 27.6 years (range: 15 to 42 years) | MS | Dental casts | mean: 3.1 ± 1.7 mm (range 0.34 to 8.67 mm) | 150–200 g, elastic chain | 7.6 months (range 5–12 months) | Three-dimensional (3D) digitizer, superimposing two sets of data to assess the relocation of cusp tips | Buccal–lingual tipping of the intruded U6 Clinical crown shortening of the intruded teeth | “a combination of mini-implants and fixed appliances is a a predictable and effective procedure to achieve maxillary molar intrusion” |
3.3. Study Characteristics
3.4. Risk of Bias in Studies
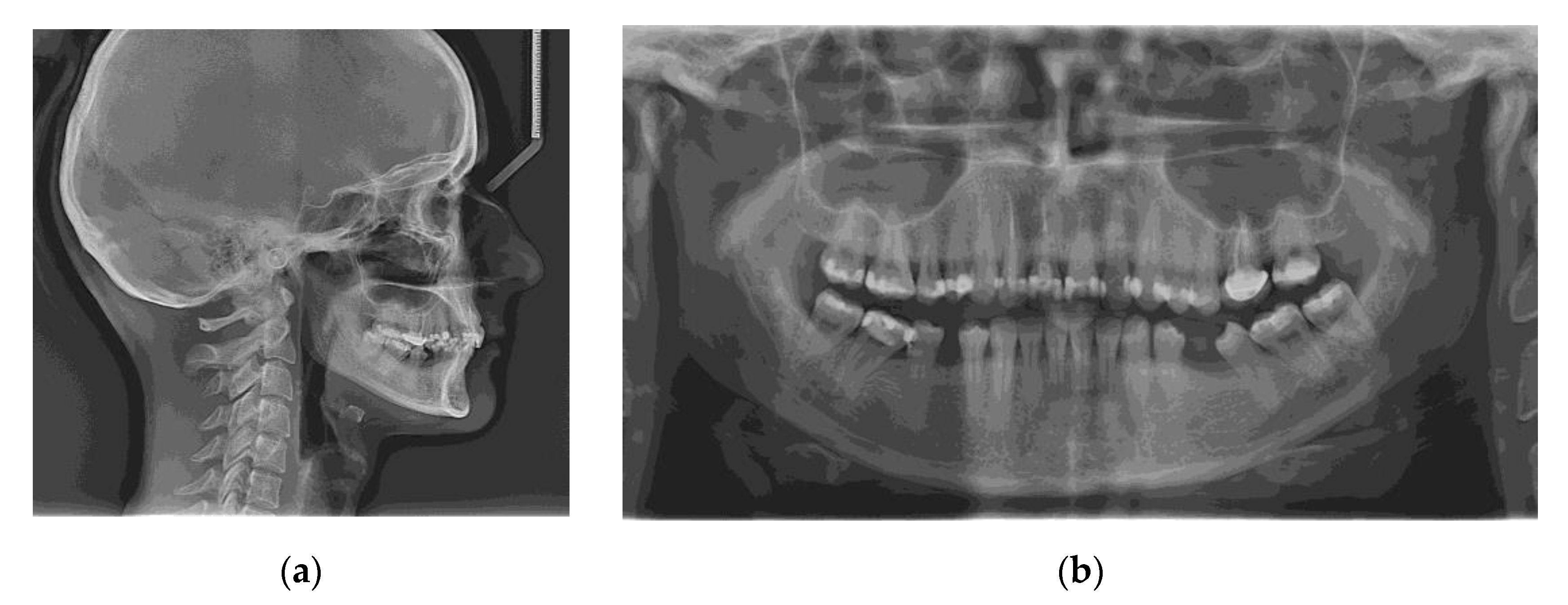
3.5. Case Report
- 12 mm (Ø 1.6 mm) Jeil Dual Top JA Screw–Palatal, between tooth 1.3 and 1.4
- 12 mm (Ø 1.6 mm) Jeil Dual Top JA Screw–Buccal, between tooth 1.4 and 1.5
- 12 mm (Ø 1.6 mm) Jeil Dual Top JA Screw–Buccal, between tooth 1.6 and 1.7
- 12 mm (Ø 1.6 mm) Jeil Dual Top JA Screw–Palatal, distal of tooth 1.7
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Gurton, A.U.; Akin, E.; Karacay, S. Initial Intrusion of the Molars in the Treatment of Anterior Open Bite Malocclusions in Growing Patients. Angle Orthod. 2004, 74, 454–464. [Google Scholar] [PubMed]
- Ng, J.; Major, P.W.; Flores-Mir, C. True Molar Intrusion Attained during Orthodontic Treatment: A Systematic Review. Am. J. Orthod. Dentofac. Orthop. 2006, 130, 709–714. [Google Scholar] [CrossRef] [PubMed]
- Yao, C.-C.J.; Lee, J.-J.; Chen, H.-Y.; Chang, Z.-C.J.; Chang, H.-F.; Chen, Y.-J. Maxillary Molar Intrusion with Fixed Appliances and Mini-Implant Anchorage Studied in Three Dimensions. Angle Orthod. 2005, 75, 754–760. [Google Scholar] [CrossRef]
- Chun, Y.S.; Row, J.; Yang, S.J.; Cha, H.S.; Han, J.S. Management of Extruded Maxillary Molars to Accommodate a Mandibular Restoration: A Clinical Report. J. Prosthet. Dent. 2000, 83, 604–606. [Google Scholar] [CrossRef]
- Yao, C.-C.J.; Wu, C.-B.; Wu, H.-Y.; Kok, S.-H.; Chang, H.-F.F.; Chen, Y.-J. Intrusion of the Overerupted Upper Left First and Second Molars by Mini-Implants with Partial-Fixed Orthodontic Appliances: A Case Report. Angle Orthod. 2004, 74, 550–557. [Google Scholar]
- Park, H.-S.; Jang, B.-K.; Kyung, H.-M. Maxillary Molar Intrusion with Micro-Implant Anchorage (MIA). Aust. Orthod. J. 2005, 21, 129–135. [Google Scholar]
- Uysal, C.; Baloş Tuncer, B.; Tuncer, C. Maxillary Posterior Intrusion with Corticotomy-Assisted Approaches with Zygomatic Anchorage-a Finite Element Stress Analysis. Prog. Orthod. 2019, 20, 8. [Google Scholar] [CrossRef]
- Sandler, P.J.; Madahar, A.K.; Murray, A. Anterior Open Bite: Aetiology and Management. Dent. Update 2011, 38, 522–524, 527–528, 531–532. [Google Scholar] [CrossRef]
- Aifa, A.; Sorel, O.; Gebeile-Chauty, S. Openbite in hyperdivergent adult: Le Fort I impaction versus maxillary molar intrusion using bone anchorage. A literature review. Orthod. Fr. 2021, 92, 215–238. [Google Scholar] [CrossRef]
- Lorean, A.; Mazor, Z.; Mijiritsky, E.; Barbu, H.; Levin, L. Segmental Dento-Alveolar Intrusive Osteotomy in Posterior Maxilla with Lack of Inter-Arch Distance for Prosthetic Rehabilitation. A Technique Combined with Sinus Floor Elevation. N. Y. State Dent. J. 2015, 81, 37–41. [Google Scholar]
- Kravitz, N.D.; Kusnoto, B.; Tsay, T.P.; Hohlt, W.F. The Use of Temporary Anchorage Devices for Molar Intrusion. J. Am. Dent. Assoc. 2007, 138, 56–64. [Google Scholar] [CrossRef] [PubMed]
- Kuroda, S.; Sakai, Y.; Tamamura, N.; Deguchi, T.; Takano-Yamamoto, T. Treatment of Severe Anterior Open Bite with Skeletal Anchorage in Adults: Comparison with Orthognathic Surgery Outcomes. Am. J. Orthod. Dentofac. Orthop. 2007, 132, 599–605. [Google Scholar] [CrossRef] [PubMed]
- Miyawaki, S.; Koyama, I.; Inoue, M.; Mishima, K.; Sugahara, T.; Takano-Yamamoto, T. Factors Associated with the Stability of Titanium Screws Placed in the Posterior Region for Orthodontic Anchorage. Am. J. Orthod. Dentofac. Orthop. 2003, 124, 373–378. [Google Scholar] [CrossRef]
- Poggio, P.M.; Incorvati, C.; Velo, S.; Carano, A. “Safe Zones”: A Guide for Miniscrew Positioning in the Maxillary and Mandibular Arch. Angle Orthod. 2006, 76, 191–197. [Google Scholar] [CrossRef] [PubMed]
- Mizrahi, E.; Mizrahi, B. Mini-Screw Implants (Temporary Anchorage Devices): Orthodontic and Pre-Prosthetic Applications. J. Orthod. 2007, 34, 80–94. [Google Scholar] [CrossRef]
- Tuncer, C.; Ataç, M.S.; Tuncer, B.B.; Kaan, E. Osteotomy Assisted Maxillary Posterior Impaction with Miniplate Anchorage. Angle Orthod. 2008, 78, 737–744. [Google Scholar] [CrossRef] [Green Version]
- Chung, K.R.; Oh, M.Y.; Ko, S.J. Corticotomy-Assisted Orthodontics. J. Clin. Orthod. 2001, 35, 331–339. [Google Scholar]
- Ahn, N.-L.; Park, H.-S. Differences in Distances between Maxillary Posterior Root Apices and the Sinus Floor According to Skeletal Pattern. Am. J. Orthod. Dentofac. Orthop. 2017, 152, 811–819. [Google Scholar] [CrossRef]
- Hodges, R.J.; Atchison, K.A.; White, S.C. Impact of Cone-Beam Computed Tomography on Orthodontic Diagnosis and Treatment Planning. Am. J. Orthod. Dentofac. Orthop. 2013, 143, 665–674. [Google Scholar] [CrossRef]
- McGowan, J.; Sampson, M.; Salzwedel, D.M.; Cogo, E.; Foerster, V.; Lefebvre, C. PRESS Peer Review of Electronic Search Strategies: 2015 Guideline Statement. J. Clin. Epidemiol. 2016, 75, 40–46. [Google Scholar] [CrossRef] [Green Version]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 Statement: An Updated Guideline for Reporting Systematic Reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef] [PubMed]
- da Costa Santos, C.M.; de Mattos Pimenta, C.A.; Nobre, M.R.C. The PICO Strategy for the Research Question Construction and Evidence Search. Rev. Lat.-Am. Enferm. 2007, 15, 508–511. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ouzzani, M.; Hammady, H.; Fedorowicz, Z.; Elmagarmid, A. Rayyan—A Web and Mobile App for Systematic Reviews. Syst. Rev. 2016, 5, 210. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Microsoft Excel; 365; Microsoft: Redmond, WA, USA, 2019.
- Zotero. Corporation for Digital Scholarship. Available online: https://www.zotero.org/ (accessed on 18 April 2022).
- Cumpston, M.; Li, T.; Page, M.J.; Chandler, J.; Welch, V.A.; Higgins, J.P.; Thomas, J. Updated Guidance for Trusted Systematic Reviews: A New Edition of the Cochrane Handbook for Systematic Reviews of Interventions. Cochrane Database Syst. Rev. 2019, 10, 14651858. [Google Scholar] [CrossRef] [Green Version]
- Akan, B.; Ünal, B.K.; Şahan, A.O.; Kızıltekin, R. Evaluation of Anterior Open Bite Correction in Patients Treated with Maxillary Posterior Segment Intrusion Using Zygomatic Anchorage. Am. J. Orthod. Dentofac. Orthop. 2020, 158, 547–554. [Google Scholar] [CrossRef] [PubMed]
- Akl, H.E.; Abouelezz, A.M.; El Sharaby, F.A.; El-Beialy, A.R.; El-Ghafour, M.A. Force Magnitude as a Variable in Maxillary Buccal Segment Intrusion in Adult Patients with Skeletal Open Bite. Angle Orthod. 2020, 90, 507–515. [Google Scholar] [CrossRef] [Green Version]
- Al-Falahi, B.; Hafez, A.M.; Fouda, M. Three-Dimensional Assessment of External Apical Root Resorption after Maxillary Posterior Teeth Intrusion with Miniscrews in Anterior Open Bite Patients. Dent. Press J. Orthod. 2018, 23, 56–63. [Google Scholar] [CrossRef]
- Ari-Demirkaya, A.; Al Masry, M.; Erverdi, N. Apical Root Resorption of Maxillary First Molars after Intrusion with Zygomatic Skeletal Anchorage. Angle Orthod. 2005, 75, 761–767. [Google Scholar]
- Ding, W.H.; Li, W.; Chen, F.; Zhang, J.F.; Lv, Y.; Chen, X.Y.; Lin, W.W.; Fu, Z.; Shi, J.J. Comparison of Molar Intrusion Efficiency and Bone Density by CT in Patients with Different Vertical Facial Morphology. J. Oral Rehabil. 2015, 42, 355–362. [Google Scholar] [CrossRef]
- Heravi, F.; Bayani, S.; Madani, A.S.; Radvar, M.; Anbiaee, N. Intrusion of Supra-Erupted Molars Using Miniscrews: Clinical Success and Root Resorption. Am. J. Orthod. Dentofac. Orthop. 2011, 139, S170–S175. [Google Scholar] [CrossRef]
- Kim, K.; Choy, K.; Park, Y.C.; Han, S.Y.; Jung, H.; Choi, Y.J. Prediction of Mandibular Movement and Its Center of Rotation for Nonsurgical Correction of Anterior Open Bite via Maxillary Molar Intrusion. Angle Orthod. 2018, 88, 538–544. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Li, W.; Chen, F.; Zhang, F.; Ding, W.; Ye, Q.; Shi, J.; Fu, B. Volumetric Measurement of Root Resorption Following Molar Mini-Screw Implant Intrusion Using Cone Beam Computed Tomography. PLoS ONE 2013, 8, e60962. [Google Scholar] [CrossRef] [PubMed]
- Marzouk, E.S.; Abdallah, E.M.; El-Kenany, W.A. Molar Intrusion in Open-Bite Adults Using Zygomatic Miniplates. Int. J. Orthod. Milwaukee 2015, 26, 47–54. [Google Scholar] [PubMed]
- Oliveira, T.F.; Nakao, C.Y.; Gonçalves, J.R.; Santos-Pinto, A. Maxillary Molar Intrusion with Zygomatic Anchorage in Open Bite Treatment: Lateral and Oblique Cephalometric Evaluation. Oral Maxillofac. Surg. 2015, 19, 71–77. [Google Scholar] [CrossRef]
- Paccini, J.V.; Cotrim-Ferreira, F.A.; Ferreira, F.V.; Freitas, K.M.; Cançado, R.H.; Valarelli, F.P. Efficiency of Two Protocols for Maxillary Molar Intrusion with Mini-Implants. Dent. Press J. Orthod. 2016, 21, 56–66. [Google Scholar] [CrossRef] [Green Version]
- Pinzan-Vercelino, C.R.; Gurgel, J.A.; Carvalho, K.R.; Tiago, C.M.; Pinzan, A. Clinical Evaluation of a Direct Method for the Intrusion of Supraerupted Maxillary Molars: A Preliminary Study. Int. J. Prosthodont. 2015, 28, 610–611. [Google Scholar] [CrossRef] [Green Version]
- Scheffler, N.R.; Proffit, W.R.; Phillips, C. Outcomes and Stability in Patients with Anterior Open Bite and Long Anterior Face Height Treated with Temporary Anchorage Devices and a Maxillary Intrusion Splint. Am. J. Orthod. Dentofac. Orthop. 2014, 146, 594–602. [Google Scholar] [CrossRef] [Green Version]
- Seres, L.; Kocsis, A. Closure of Severe Skeletal Anterior Open Bite with Zygomatic Anchorage. J. Craniofacial Surg. 2009, 20, 478–482. [Google Scholar] [CrossRef]
- Sherwood, K.H.; Burch, J.G.; Thompson, W.J. Closing Anterior Open Bites by Intruding Molars with Titanium Miniplate Anchorage. Am. J. Orthod. Dentofac. Orthop. 2002, 122, 593–600. [Google Scholar] [CrossRef]
- Turkkahraman, H.; Sarioglu, M. Are Temporary Anchorage Devices Truly Effective in the Treatment of Skeletal Open Bites? Eur. J. Dent. 2016, 10, 447–453. [Google Scholar] [CrossRef] [Green Version]
- Xun, C.L.; Zhao, H.; Zeng, X.L.; Wang, X. Intrusion of Overerupted Maxillary Molars with Miniscrew Implant Anchorage: A Radiographic Evaluation. J. Huazhong Univ. Sci. Technol. Med. Sci. 2013, 33, 780–785. [Google Scholar] [CrossRef] [PubMed]
- Wells, G.; Shea, B.; O’Connell, D.; Peterson, J.; Welch, V.; Losos, M.; Tugwell, P. Ottawa Hospital Research Institute. Available online: http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp (accessed on 29 April 2022).
- Baumgaertel, S.; Smuthkochorn, S.; Palomo, J.M. Intrusion Method for a Single Overerupted Maxillary Molar Using Only Palatal Mini-Implants and Partial Fixed Appliances. Am. J. Orthod. Dentofac. Orthop. 2016, 149, 411–415. [Google Scholar] [CrossRef] [PubMed]
- Dalstra, M.; Cattaneo, P.; Melsen, B. Load Transfer of Miniscrews for Orthodontic Anchorage. Orthodontics 2004, 1, 53–62. [Google Scholar]
- Melsen, B.; Fiorelli, G. Upper Molar Intrusion. J. Clin. Orthod. 1996, 30, 91–96. [Google Scholar]
- Tseng, Y.-C.; Hsieh, C.-H.; Chen, C.-H.; Shen, Y.-S.; Huang, I.-Y.; Chen, C.-M. The Application of Mini-Implants for Orthodontic Anchorage. Int. J. Oral Maxillofac. Surg. 2006, 35, 704–707. [Google Scholar] [CrossRef]
- Park, Y.-C.; Lee, S.-Y.; Kim, D.-H.; Jee, S.-H. Intrusion of Posterior Teeth Using Mini-Screw Implants. Am. J. Orthod. Dentofac. Orthop. 2003, 123, 690–694. [Google Scholar] [CrossRef]
- Büchter, A.; Wiechmann, D.; Koerdt, S.; Wiesmann, H.P.; Piffko, J.; Meyer, U. Load-Related Implant Reaction of Mini-Implants Used for Orthodontic Anchorage. Clin. Oral Implant. Res. 2005, 16, 473–479. [Google Scholar] [CrossRef]
- Erverdi, N.; Usumez, S.; Solak, A. New Generation Open-Bite Treatment with Zygomatic Anchorage. Angle Orthod. 2006, 76, 519–526. [Google Scholar] [CrossRef]
- Sugawara, J.; Baik, U.B.; Umemori, M.; Takahashi, I.; Nagasaka, H.; Kawamura, H.; Mitani, H. Treatment and Posttreatment Dentoalveolar Changes Following Intrusion of Mandibular Molars with Application of a Skeletal Anchorage System (SAS) for Open Bite Correction. Int. J. Adult Orthodon. Orthognath. Surg. 2002, 17, 243–253. [Google Scholar]
- Baek, M.S.; Choi, Y.J.; Yu, H.S.; Lee, K.J.; Kwak, J.; Park, Y.C. Long-Term Stability of Anterior Open-Bite Treatment by Intrusion of Maxillary Posterior Teeth. Am. J. Orthod. Dentofac. Orthop. 2010, 138, 396.e1–396.e9. [Google Scholar] [CrossRef]
- Erverdi, N.; Keles, A.; Nanda, R. The Use of Skeletal Anchorage in Open Bite Treatment: A Cephalometric Evaluation. Angle Orthod. 2004, 74, 381–390. [Google Scholar] [PubMed]
- Burstone, C.R. Deep Overbite Correction by Intrusion. Am. J. Orthod. 1977, 72, 1–22. [Google Scholar] [CrossRef]
- Malara, P.; Bierbaum, S.; Malara, B. Outcomes and Stability of Anterior Open Bite Treatment with Skeletal Anchorage in Non-Growing Patients and Adults Compared to the Results of Orthognathic Surgery Procedures: A Systematic Review. J. Clin. Med. 2021, 10, 5682. [Google Scholar] [CrossRef] [PubMed]
- Abdulghani, E.A.; Al-Sosowa, A.A.; Alhammadi, M.S.; Al-Fakeh, H.; Al-Gumaei, W.S.; Almashraqi, A.A.; Sharhan, H.M.; Cao, B. Three-Dimensional Assessment of the Favorability of Maxillary Posterior Teeth Intrusion in Different Skeletal Classes Limited by the Vertical Relationship with the Maxillary Sinus Floor. Head Face Med. 2022, 18, 13. [Google Scholar] [CrossRef]
- Son, W.-S.; Kim, Y.-I.; Kim, S.-S.; Park, S.-B.; Kim, S.-H. Anatomical Relationship between the Maxillary Posterior Teeth and the Sinus Floor According to an Anterior Overbite. Orthod. Craniofac. Res. 2020, 23, 160–165. [Google Scholar] [CrossRef]
- González Espinosa, D.; de Oliveira Moreira, P.E.; da Sousa, A.S.; Flores-Mir, C.; Normando, D. Stability of Anterior Open Bite Treatment with Molar Intrusion Using Skeletal Anchorage: A Systematic Review and Meta-Analysis. Prog. Orthod. 2020, 21, 35. [Google Scholar] [CrossRef]








| Author, Year of Publication | Akan B et al., 2020 [27] | Akl HE et al., 2020 [28] | Al-Falahi B et al., 2018 [29] | Ari-Demirkaya A et al., 2005 [30] | Ding WH et al., 2015 [31] | Heravi F et al., 2011 [32] | Kim K et al., 2018 [33] | Li W et al., 2013 [34] | Marzouk ES et al., 2015 [35] |
|---|---|---|---|---|---|---|---|---|---|
| 1. Is the case definition adequate? | * | * | * | * | * | * | * | * | |
| 2. Representativeness of the cases | * | * | * | * | * | * | * | * | |
| 3. Selection of controls | * | * | * | ||||||
| 4. Definition of controls | * | * | |||||||
| 1. Comparability of cases and controls on the basis of the design or analysis | * | * | * | ||||||
| 1. Ascertainment of exposure | * | * | * | * | * | * | * | * | * |
| 2. Same method of ascertainment for cases and controls | * | * | |||||||
| 3. Non-response rate | |||||||||
| Author, Year of Publication | de Oliveira TFM et al., 2015 [36] | Paccini JV et al., 2016 [37] | Pinzan-Vercelino CRM et al., 2015 [38] | Scheffler NR et al., 2014 [39] | Seres L, Kocsis A, 2009 [40] | Sherwood K.H. et al., 2002 [41] | Turkahraman H., Sarioglu M, 2016 [42] | Xun CL et al., 2013 [43] | Yao CC, et al., 2005 [3] |
| Selection | |||||||||
| 1. Is the case definition adequate? | * | * | * | * | * | * | * | * | * |
| 2. Representativeness of the cases | * | * | * | * | * | * | * | * | * |
| 3. Selection of controls | * | ||||||||
| 4. Definition of controls | * | ||||||||
| Comparability | |||||||||
| 1. Comparability of cases and controls on the basis of the design or analysis | * | ||||||||
| Exposure | |||||||||
| 1. Ascertainment of exposure | * | * | * | * | * | * | * | * | * |
| 2. Same method of ascertainment for cases and controls | * | ||||||||
| 3. Non-response rate | |||||||||
| Parameter | Value | Mean ± SD |
|---|---|---|
| SNA angle | 84.94° | 82 ± 2° |
| ANB angle | 4.23° | 2 ± 2° |
| SNB angle | 80.71° | 80 ± 2° |
| FMA angle | 21.53° | 25 ± 2° |
| Occlusal plane to Gonion–menton | 13.83° | 19.09 ± 4.7° |
| Occlusal plane to Sella–nasion | 16.33° | 14 ± 4° |
| Lower facial height | 65.64 mm | 66.7 ± 4.1 mm |
| Anterior facial height | 114.80 mm | 128.68 ± 6 mm |
| Upper molar to pterygoid vertical plane | 21.39 mm | 21.10 ± 3 mm |
| Interincisal angle | 145.21° | 128.0 ± 5° |
| Overbite | 3.73 mm | 2 ± 2 mm |
| Overjet | 3.3 mm | 2 ± 2 mm |
| Gonion–Gnation to Sella–nasion | 28.91° | 32 ± 4° |
| U1 to Nasion–point A line | 10.27° | 22.0 ± 5° |
| U1 to Sella–nasion | 95.21° | 105.28 ± 6° |
| CBCT Parameter | T0–Before Intrusion (mm) | T1–After Intrusion (mm) | Intrusion Amount (T1-T0; mm) |
|---|---|---|---|
| Mesiobuccal cusp of the left upper first molar | 22.26 | 20.73 | 1.53 |
| Palatal root apex of the left upper first molar | 4.20 | 1.62 | 2.58 |
| Upper left first molar furcation | 11.35 | 8.74 | 2.61 |
| Buccal cusp of the left upper first premolar | 24.8 | 22.16 | 2.64 |
| Palatal root apex of the left upper first premolar | 5.67 | 4.53 | 1.14 |
| Mesiobuccal cusp of the right upper first molar | 23.76 | 20.31 | 3.45 |
| Palatal root apex of the right upper first molar | 4.18 | 2.37 | 1.81 |
| Upper right first molar furcation | 12.79 | 9.74 | 3.05 |
| Buccal cusp of the right upper first premolar | 24.72 | 20.45 | 4.27 |
| Palatal root apex of the right upper first premolar | 6.04 | 3.42 | 2.62 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Manea, A.; Dinu, C.; Băciuţ, M.; Buduru, S.; Almășan, O. Intrusion of Maxillary Posterior Teeth by Skeletal Anchorage: A Systematic Review and Case Report with Thin Alveolar Biotype. J. Clin. Med. 2022, 11, 3787. https://doi.org/10.3390/jcm11133787
Manea A, Dinu C, Băciuţ M, Buduru S, Almășan O. Intrusion of Maxillary Posterior Teeth by Skeletal Anchorage: A Systematic Review and Case Report with Thin Alveolar Biotype. Journal of Clinical Medicine. 2022; 11(13):3787. https://doi.org/10.3390/jcm11133787
Chicago/Turabian StyleManea, Avram, Cristian Dinu, Mihaela Băciuţ, Smaranda Buduru, and Oana Almășan. 2022. "Intrusion of Maxillary Posterior Teeth by Skeletal Anchorage: A Systematic Review and Case Report with Thin Alveolar Biotype" Journal of Clinical Medicine 11, no. 13: 3787. https://doi.org/10.3390/jcm11133787
APA StyleManea, A., Dinu, C., Băciuţ, M., Buduru, S., & Almășan, O. (2022). Intrusion of Maxillary Posterior Teeth by Skeletal Anchorage: A Systematic Review and Case Report with Thin Alveolar Biotype. Journal of Clinical Medicine, 11(13), 3787. https://doi.org/10.3390/jcm11133787








