Intrapatient Comparison of Coblation versus Electrocautery Tonsillectomy in Children: A Randomized, Controlled Trial
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Participants
2.2. Randomization and Blinding
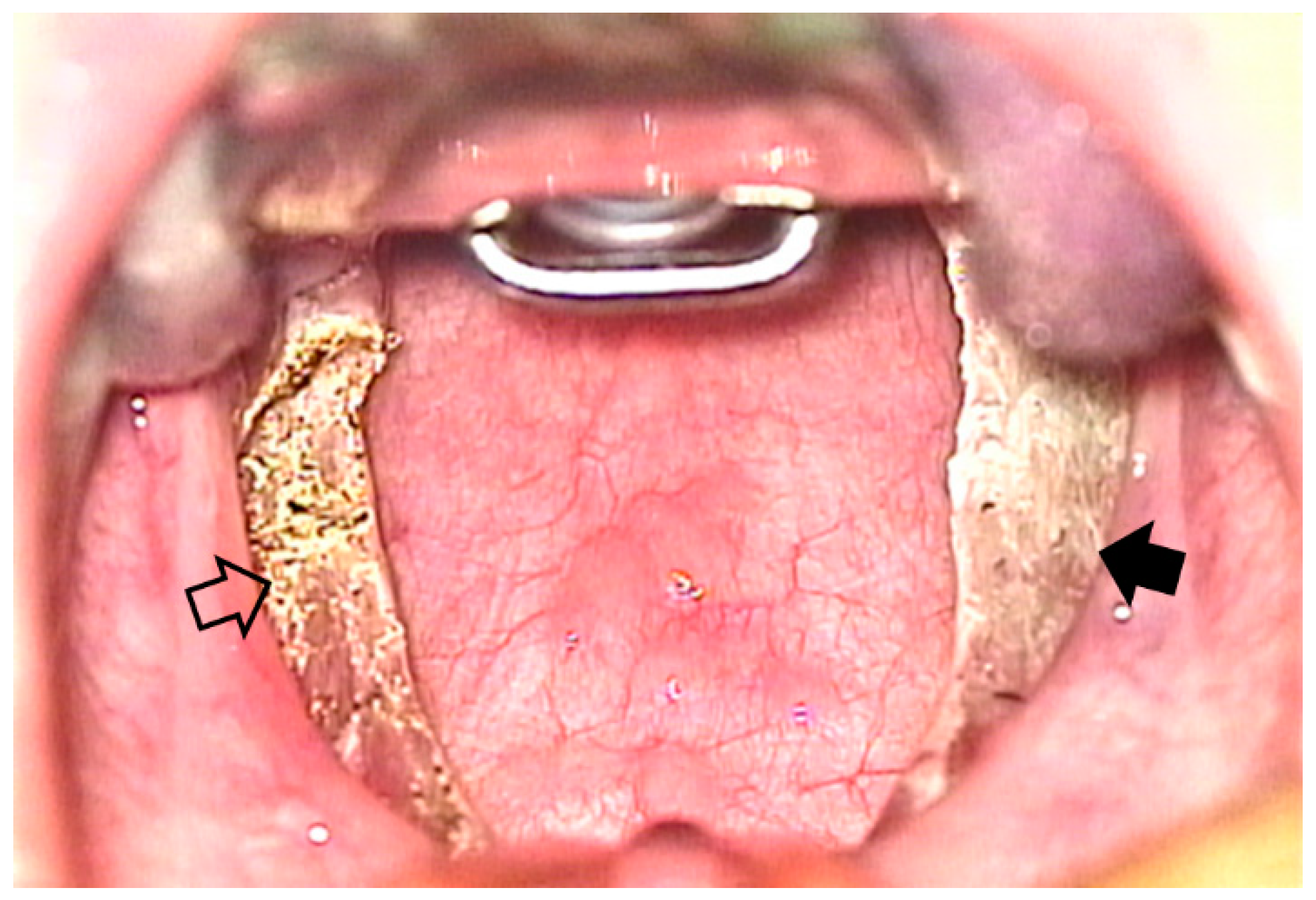
2.3. Surgical Procedures
2.4. Postoperative Pain Assessment
2.5. Statistical Analysis
3. Results
3.1. Demographic Data
3.2. Outcomes
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Subasi, B.; Oghan, F.; Tasli, H.; Akbal, S.; Karaman, N.E. Comparison of three tonsillectomy techniques in children. Eur. Arch. Otorhinolaryngol. 2021, 278, 2011–2015. [Google Scholar] [CrossRef] [PubMed]
- Salley, J.R.; Johnson, R.; Mitchell, R.B.; Shah, G.; Coffey, A.R. Comparison of outcomes between thermal welding forceps, controlled ablation and monopolar electrosurgery for tonsillectomy in children. Int. J. Pediatr. Otorhinolaryngol. 2022, 152, 110941. [Google Scholar] [CrossRef] [PubMed]
- Hong, S.M.; Cho, J.G.; Chae, S.W.; Lee, H.M.; Woo, J.S. Coblation vs. electrocautery tonsillectomy: A prospective randomized study comparing clinical outcomes in adolescents and adults. Clin. Exp. Otorhinolaryngol. 2013, 6, 90–93. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.W.; Kim, H.J.; Lee, W.H.; Kim, D.K.; Kim, S.W.; Kim, Y.H.; Nam, J.G.; Park, S.W.; Park, C.S.; Bae, W.Y.; et al. Comparative study for efficacy and safety of adenoidectomy according to the surgical method: A prospective multicenter study. PLoS ONE 2015, 10, e0135304. [Google Scholar] [CrossRef] [PubMed]
- Mularczyk, C.; Walner, D.L.; Hamming, K.K. Coblation versus microdebrider in pediatric adenoidectomy. Int. J. Pediatr. Otorhinolaryngol. 2018, 104, 29–31. [Google Scholar] [CrossRef]
- Parker, N.P.; Walner, D. Post-operative pain following coblation or monopolar electrocautery tonsillectomy in children: A prospective, single-blinded, randomised comparison. Clin. Otolaryngol. 2011, 36, 468–474. [Google Scholar] [CrossRef]
- Polites, N.; Joniau, S.; Wabnitz, D.; Fassina, R.; Smythe, C.; Varleyet, P.; Carney, A.S. Postoperative pain following coblation tonsillectomy: Randomized clinical trial. ANZ J. Surg. 2006, 76, 226–229. [Google Scholar] [CrossRef]
- Mitic, S.; Tvinnereim, M.; Lie, E.; Šaltytė, B. A pilot randomized controlled trial of coblation tonsillectomy versus dissection tonsillectomy with bipolar diathermy haemostasis. Clin. Otolaryngol. 2007, 32, 261–267. [Google Scholar] [CrossRef]
- Ahmad, M.; Wardak, A.; Hampton, T.; Siddiqui, M.; Street, I. Coblation versus cold dissection in paediatric tonsillectomy: A systematic review and meta-analysis. J. Laryngol. Otol. 2020, 134, 197–204. [Google Scholar] [CrossRef]
- Thottam, P.J.; Christenson, J.R.; Cohen, D.S.; Metz, C.M.; Saraiya, S.S.; Haupert, M.S. The utility of common surgical instruments for pediatric adenotonsillectomy. Laryngoscope 2015, 125, 475–479. [Google Scholar] [CrossRef]
- Moesgaard, L.; Mirz, F. No clinical advantages of coblation tonsillectomy compared with traditional tonsillectomy. Dan. Med. J. 2012, 59, A4355. [Google Scholar] [PubMed]
- Jones, D.T.; Kenna, M.A.; Guidi, J.; Huang, L.; Johnston, P.R.; Licameli, G.R. Comparison of postoperative pain in pediatric patients undergoing coblation tonsillectomy versus cautery tonsillectomy. Otolaryngol. Head Neck Surg. 2011, 144, 972–977. [Google Scholar] [CrossRef] [PubMed]
- Lee, Y.C.; Hsin, L.J.; Lin, W.N.; Fang, T.J.; Tsai, Y.T.; Luo, C.M. Adolescents and adults undergoing temperature-controlled surgical instruments vs electrocautery in tonsillectomy: A systematic review and meta-analysis of randomized clinical trials. JAMA Otolaryngol. Head Neck Surg. 2020, 146, 339–346. [Google Scholar] [CrossRef] [PubMed]
- Cai, F.G.; Hong, W.; Ye, Y.; Liu, Y.S. Comparative systematic review and meta-analysis of the therapeutic effects of coblation tonsillectomy versus electrocautery tonsillectomy. Gland. Surg. 2022, 11, 175–185. [Google Scholar] [CrossRef] [PubMed]
- Jeon, Y.J.; Song, J.J.; Ahn, J.C.; Kong, I.G.; Kim, J.W.; Park, G.H.; Won, T.B. Immediate and sustained improvement in behavior and life quality by adenotonsillectomy in children with sleep-disordered breathing. Clin. Exp. Otorhinolaryngol. 2016, 9, 136–142. [Google Scholar] [CrossRef] [Green Version]
- Kumar, D.S.; Valenzuela, D.; Kozak, F.K.; Ludemann, J.P.; Moxham, J.P.; Lea, J.; Chadha, N.K. The reliability of clinical tonsil size grading in children. JAMA Otolaryngol. Head Neck Surg. 2014, 140, 1034–1037. [Google Scholar] [CrossRef] [Green Version]
- Karam, M.; Abul, A.; Althuwaini, A.; Almuhanna, A.; Alenezi, T.; Aljadi, A.; Al-Naseem, A.; Alwael, A. Coblation versus bipolar diathermy hemostasis in pediatric tonsillectomy patients: Systematic review and meta-analysis. Cureus 2022, 14, e23066. [Google Scholar] [CrossRef]
- Sakki, A.J.; Mäkinen, L.K.; Kanerva, M.; Nokso-Koivisto, J. Monopolar tonsillotomy versus cold dissection tonsillectomy in children: Prospective study on postoperative recovery. Int. J. Pediatr. Otorhinolaryngol. 2021, 141, 110513. [Google Scholar] [CrossRef]
- Vaughan, A.H.; Derkay, C.S. Microdebrider intracapsular tonsillectomy. ORL J. Otorhinolaryngol. Relat. Spec. 2007, 69, 358–363. [Google Scholar] [CrossRef]
- Temple, R.H.; Timms, M.S. Paediatric coblation tonsillectomy. Int. J. Pediatr. Otorhinolaryngol. 2001, 61, 195–198. [Google Scholar] [CrossRef]
- Chinpairoj, S.; Feldman, M.D.; Saunders, J.C.; Thaler, E.R. A comparison of monopolar electrosurgery to a new multipolar electrosurgical system in a rat model. Laryngoscope 2001, 111, 213–217. [Google Scholar] [CrossRef] [PubMed]
- Timms, M.; Temple, R. Coblation tonsillectomy: A double blind randomized controlled study. J. Laryngol. Otol. 2002, 116, 450–452. [Google Scholar] [CrossRef] [PubMed]
- Noordzij, J.P.; Affleck, B.D. Coblation versus unipolar electrocautery tonsillectomy: A prospective, randomized, single-blind study in adult patients. Laryngoscope 2006, 116, 1303–1309. [Google Scholar] [CrossRef] [PubMed]
- Rakesh, S.; Anand, T.; Payal, G.; Pranjal, K. A prospective, randomized, double-blind study of coblation versus dissection tonsillectomy in adult patients. Indian J. Otolaryngol. Head Neck Surg. 2012, 64, 290–294. [Google Scholar] [CrossRef] [PubMed] [Green Version]




| Characteristic | Number of Participants, n (%) |
|---|---|
| Total | 30 |
| Sex | |
| Female | 10 (33.3) |
| Male | 20 (66.7) |
| Age, years | |
| 6−7 | 12 (40.0) |
| 8−10 | 10 (33.3) |
| 11−17 | 8 (26.7) |
| Indication of surgery | |
| Sleep-disordered breathing | 26 (86.7) |
| Recurrent tonsillitis | 4 (13.3) |
| Allergic rhinitis | |
| No | 10 (33.3) |
| Yes | 20 (66.7) |
| KOSA-18 score | |
| <60 | 22 (77.3) |
| 60–80 | 6 (20.0) |
| ≥80 | 2 (6.7) |
| Characteristic | Coblation Side, n (%) | Electrocautery Side, n (%) |
|---|---|---|
| Tonsil size | ||
| Grade 1 | 0 (0) | 0 (0) |
| Grade 2 | 2 (6.7) | 2 (6.7) |
| Grade 3 | 11 (36.7) | 11 (36.7) |
| Grade 4 | 17 (56.7) | 17 (56.7) |
| Tonsillar adhesion | ||
| Mild | 9 (30.0) | 9 (30.0) |
| Moderate | 15 (50.0) | 16 (53.3) |
| Severe | 6 (20.0) | 5 (16.7) |
| Postoperative Day | Coblation Side, VAS | Electrocautery Side, VAS | p-Value |
|---|---|---|---|
| 0 | 3.7 ± 0.5 | 6.5 ± 0.5 | <0.001 |
| 1 | 4.2 ± 0.4 | 5.5 ± 0.5 | 0.022 |
| 2 | 4.5 ± 0.4 | 5.8 ± 0.5 | 0.010 |
| 3 | 3.9 ± 0.4 | 5.1 ± 0.4 | 0.003 |
| 4 | 3.3 ± 0.4 | 4.7 ± 0.5 | 0.004 |
| 5 | 3.2 ± 0.4 | 4.7 ± 0.5 | 0.003 |
| 6 | 3.2 ± 0.5 | 3.7 ± 0.4 | 0.332 |
| 7 | 2.6 ± 0.4 | 3.9 ± 0.5 | 0.030 |
| 8 | 2.6 ± 0.4 | 3.1 ± 0.5 | 0.161 |
| 9 | 2.3 ± 0.4 | 2.7 ± 0.5 | 0.025 |
| 10 | 1.4 ± 0.3 | 2.0 ± 0.4 | 0.032 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Choi, K.Y.; Ahn, J.-C.; Rhee, C.-S.; Han, D.H. Intrapatient Comparison of Coblation versus Electrocautery Tonsillectomy in Children: A Randomized, Controlled Trial. J. Clin. Med. 2022, 11, 4561. https://doi.org/10.3390/jcm11154561
Choi KY, Ahn J-C, Rhee C-S, Han DH. Intrapatient Comparison of Coblation versus Electrocautery Tonsillectomy in Children: A Randomized, Controlled Trial. Journal of Clinical Medicine. 2022; 11(15):4561. https://doi.org/10.3390/jcm11154561
Chicago/Turabian StyleChoi, Kyu Young, Jae-Cheul Ahn, Chae-Seo Rhee, and Doo Hee Han. 2022. "Intrapatient Comparison of Coblation versus Electrocautery Tonsillectomy in Children: A Randomized, Controlled Trial" Journal of Clinical Medicine 11, no. 15: 4561. https://doi.org/10.3390/jcm11154561






