Suprapubic Cholecystectomy Improves Cosmetic Outcome Compared to Classic Cholecystectomy
Abstract
:1. Introduction
2. Material and Methods
2.1. Patients
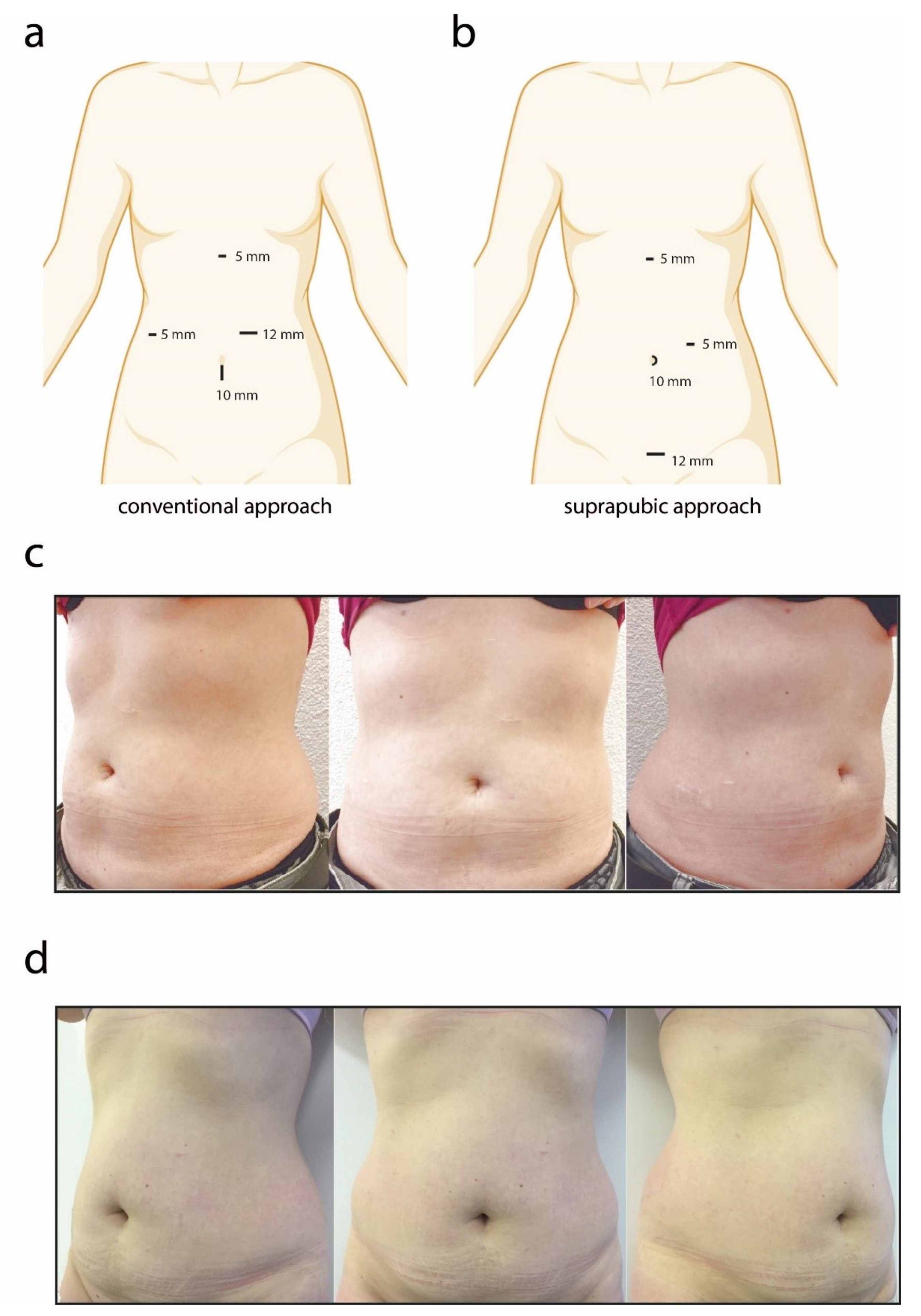
2.2. Conventional Approach (CA)
2.3. Suprapubic Approach (SA)
2.4. Outcome Measures
2.5. Statistical Analysis
3. Results
3.1. Cohort
3.2. Aesthetic Outcome
3.3. Interrater Agreement
4. Discussion
5. Limitations
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Brunt, L.M.; Deziel, D.J.; Telem, D.A.; Strasberg, S.M.; Aggarwal, R.; Asbun, H.; Bonjer, J.; McDonald, M.; Alseidi, A.; Ujiki, M.; et al. Safe Cholecystectomy Multi-society Practice Guideline and State of the Art Consensus Conference on Prevention of Bile Duct Injury During Cholecystectomy. Ann. Surg. 2020, 272, 3–23. [Google Scholar] [CrossRef]
- Litwin, D.E.; Cahan, M.A. Laparoscopic cholecystectomy. Surg. Clin. N. Am. 2008, 88, 1295–1313. [Google Scholar] [CrossRef] [PubMed]
- Soper, N.J.; Stockmann, P.T.; Dunnegan, D.L.; Ashley, S.W. Laparoscopic cholecystectomy. The new ‘gold standard’? Arch. Surg. 1992, 127, 917–921. [Google Scholar] [CrossRef] [PubMed]
- Litynski, G.S. Erich Mühe and the rejection of laparoscopic cholecystectomy (1985): A surgeon ahead of his time. J. Soc. Laparoendosc. Surg. 1998, 2, 341–346. [Google Scholar]
- Roy, P.; De, A. Transumbilical multiple-port laparoscopic cholecystectomy (TUMP-LC): A prospective analysis of 50 initial patients. J. Laparoendosc. Adv. Surg. Tech. A 2010, 20, 211–217. [Google Scholar] [CrossRef]
- Thakur, V.; Schlachta, C.M.; Jayaraman, S. Minilaparoscopic versus conventional laparoscopic cholecystectomy a systematic review and meta-analysis. Ann. Surg. 2011, 253, 244–258. [Google Scholar] [CrossRef]
- Bulian, D.R.; Knuth, J.; Cerasani, N.; Lange, J.; Ströhlein, M.A.; Sauerwald, A.; Heiss, M.M. Transvaginal hybrid NOTES cholecystectomy—Results of a randomized clinical trial after 6 months. Langenbecks Arch. Surg. 2014, 399, 717–724. [Google Scholar] [CrossRef]
- Sinan, H.; Demirbas, S.; Ozer, M.T.; Sucullu, I.; Akyol, M. Single-incision laparoscopic cholecystectomy versus laparoscopic cholecystectomy: A prospective randomized study. Surg. Laparosc. Endosc. Percutaneous Tech. 2012, 22, 12–16. [Google Scholar] [CrossRef]
- Lehmann, K.S.; Ritz, J.P.; Wibmer, A.; Gellert, K.; Zornig, C.; Burghardt, J.; Büsing, M.; Runkel, N.; Kohlhaw, K.; Albrecht, R.; et al. The German registry for natural orifice translumenal endoscopic surgery: Report of the first 551 patients. Ann. Surg. 2010, 252, 263–270. [Google Scholar] [CrossRef]
- Hu, H.; Zhu, J.F.; Huang, A.H.; Xin, Y.; Xu, A.A.; Chen, B. Covert laparoscopic cholecystectomy: A new minimally invasive technique. Acta Med. Okayama 2011, 65, 325–328. [Google Scholar] [CrossRef]
- Ma, J.; Cassera, M.A.; Spaun, G.O.; Hammill, C.W.; Hansen, P.D.; Aliabadi-Wahle, S. Randomized controlled trial comparing single-port laparoscopic cholecystectomy and four-port laparoscopic cholecystectomy. Ann. Surg. 2011, 254, 22–27. [Google Scholar] [CrossRef]
- Le Roy, B.; Fetche, N.; Buc, E.; Pereira, B.; Genty, F.; Antomarchi, O.; Gagnière, J.; Pezet, D.; Slim, K. Feasibility prospective study of laparoscopic cholecystectomy with suprapubic approach. J. Visc. Surg. 2016, 153, 327–331. [Google Scholar] [CrossRef]
- Streitberg, B.; Röhmel, J. Exact distributions for permutation and rank tests: An introduction to some recently published algorithms. Stat. Softw. Newsl. 1986, 12, 10–17. [Google Scholar]
- Shrout, P.E.; Fleiss, J.L. Intraclass correlations: Uses in assessing rater reliability. Psychol. Bull. 1979, 86, 420–428. [Google Scholar] [CrossRef]
- R Core Team. R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2020. [Google Scholar]
- Tenconi, S.M.; Boni, L.; Colombo, E.M.; Dionigi, G.; Rovera, F.; Cassinotti, E. Laparoscopic cholecystectomy as day-surgery procedure: Current indications and patients’ selection. Int. J. Surg. 2008, 6 (Suppl. S1), S86–S88. [Google Scholar] [CrossRef] [Green Version]
- Hao, L.; Liu, M.; Zhu, H.; Li, Z. Single-incision versus conventional laparoscopic cholecystectomy in patients with uncomplicated gallbladder disease: A meta-analysis. Surg. Laparosc. Endosc. Percutaneous Tech. 2012, 22, 487–497. [Google Scholar] [CrossRef]
- Degano, G.; Santarelli, E.; Ceraudo, E.; Iantosca, F.; Taccaliti, F.; Monaco, M. Colecistectomia per via videolaparoscopica con approccio sovrapubico. Note di tecnica [Video-laparoscopic cholecystectomy with suprapubic approach. Technical note]. Minerva Chir. 1995, 50, 1109–1114. (In Italian) [Google Scholar]
- Phillips, M.S.; Marks, J.M.; Roberts, K.; Tacchino, R.; Onders, R.; DeNoto, G.; Rivas, H.; Islam, A.; Soper, N.; Gecelter, G.; et al. Intermediate results of a prospective randomized controlled trial of traditional four-port laparoscopic cholecystectomy versus single-incision laparoscopic cholecystectomy. Surg. Endosc. 2012, 26, 1296–1303. [Google Scholar] [CrossRef]
- Marks, J.M.; Phillips, M.S.; Tacchino, R.; Roberts, K.; Onders, R.; DeNoto, G.; Gecelter, G.; Rubach, E.; Rivas, H.; Islam, A.; et al. Single-incision laparoscopic cholecystectomy is associated with improved cosmesis scoring at the cost of significantly higher hernia rates: 1-year results of a prospective randomized, multicenter, single-blinded trial of traditional multiport laparoscopic cholecystectomy vs. single-incision laparoscopic cholecystectomy. J. Am. Coll. Surg. 2013, 216, 1037–1047, discussion 1047–1048. [Google Scholar] [CrossRef]
- Pucher, P.H.; Sodergren, M.H.; Singh, P.; Darzi, A.; Parakseva, P. Have we learned from lessons of the past? A systematic review of training for single incision laparoscopic surgery. Surg. Endosc. 2013, 27, 1478–1484. [Google Scholar] [CrossRef]
- Yang, E.; Nie, D.; Li, Z. Comparison of Major Clinical Outcomes Between Transvaginal NOTES and Traditional Laparoscopic Surgery: A Systematic Review and Meta-analysis. J. Surg. Res. 2019, 244, 278–290. [Google Scholar] [CrossRef]
- Zhang, L.; Sah, B.; Ma, J.; Shang, C.; Huang, Z.; Chen, Y. A prospective, randomized, controlled, trial comparing occult-scar incision laparoscopic cholecystectomy and classic three-port laparoscopic cholecystectomy. Surg. Endosc. 2014, 28, 1131–1135. [Google Scholar] [CrossRef]
- Sales, L.A.; Pinto, J.O.; Queiroz, C.E.; Castro, M.; Dourado, P.H.; Pinheiro, F.A. Suprapubic laparoscopic cholecystectomy: Technique and preliminary results. Arq. Bras. Cir. Dig. 2014, 27, 22–25. [Google Scholar] [CrossRef] [Green Version]
- Rabbany, J.; Kim, T.; Koh, S.; Zaghiyan, K.; Fleshner, P. Cosmesis in Patients after Multiport Laparoscopic Colorectal Surgery: Does the Extraction Incision Matter? Am. Surg. 2019, 85, 162–166. [Google Scholar] [CrossRef]
- De la Cruz-Munoz, N.; Koniaris, L. Alternative port site selection (APSS) for improved cosmesis in laparoscopic surgery. J. Gastrointest. Surg. 2010, 14, 2004–2008. [Google Scholar] [CrossRef]
- Hipp, J.; Laniewski, J.; Gitei, E.; Elhabash, S.; Akkermann, O.; Gerdes, B. Operationszeit bei der suprapubisch-transumbilikalen Cholezystektomie: Ergebnisse einer prospektiv-randomisierten Studie [Operation time for suprapubic transumbilical cholecystectomy: Results of a prospective randomized trial]. Die Chir. 2015, 86, 866–873. [Google Scholar] [CrossRef]
- Griffith, K.C.; Clark, N.V.; Mushinski, A.A.; Gu, X.; Ajao, M.O.; Brown, D.N.; Einarsson, J.I.; Cohen, S.L. Incisional Outcomes of Umbilical vs. Suprapubic Mini-laparotomy for Tissue Extraction: A Retrospective Cohort Study. J. Minim. Invasive Gynecol. 2018, 25, 1024–1030. [Google Scholar] [CrossRef]
- Renard, Y.; Simonneau, A.C.; de Mestier, L.; Teuma, L.; Meffert, J.L.; Palot, J.P.; Kianmanesh, R. Standard of Open Surgical Repair of Suprapubic Incisional Hernias. World J. Surg. 2017, 41, 1466–1474. [Google Scholar] [CrossRef]
- Langhorst, M.; Bialas, E.; Bergmann, J.; Ansorg, J. Prozessdaten im OP am Beispiel der Cholezystekotmie. Professional Association of German Surgeons. Available online: https://www.bdc.de/prozessdaten-im-op-am-beispiel-der-cholecystektomie-3/ (accessed on 1 November 2021).
- Voyles, C.R.; Boyd, K.B. Criteria and benchmarks for laparoscopic cholecystectomy in a free-standing ambulatory center. JSLS 1999, 3, 315–318. [Google Scholar]
- Chatzimavroudis, G.; Papaziogas, B.; Galanis, I.; Koutelidakis, I.; Atmatzidis, S.; Evangelatos, P.; Voloudakis, N.; Ananiadis, A.; Doundis, A.; Christoforidis, E. Trocar site hernia following laparoscopic cholecystectomy: A 10-year single center experience. Hernia 2017, 21, 925–932. [Google Scholar] [CrossRef]
- Coletta, D.; Mascioli, F.; Balla, A.; Guerra, F.; Ossola, P. Minilaparoscopic Cholecystectomy Versus Conventional Laparoscopic Cholecystectomy: An Endless Debate. J. Laparoendosc. Adv. Surg. Tech. Part A 2021, 31, 648–656. [Google Scholar] [CrossRef] [PubMed]
- Bender, K.; Lewin, J.; O’Rourke, H.; Hugh, F.C.; O’Rourke, N.; Hugh, T.J. Total 5-mm port approach: A feasible technique for both elective and emergency laparoscopic cholecystectomy. ANZ J. Surg. 2018, 88, E751–E755. [Google Scholar] [CrossRef] [PubMed]
- El-Dhuwaib, Y.; Hamade, A.M.; Issa, M.E.; Balbisi, B.M.; Abid, G.; Ammori, B.J. An “all 5-mm ports” selective approach to laparoscopic cholecystectomy, appendectomy, and anti-reflux surgery. Surg. Laparosc. Endosc. Percutaneous Tech. 2004, 14, 141–144. [Google Scholar] [CrossRef] [PubMed]
- Hung, T.; Chang, W.; Vlantis, A.C.; Tong, M.C.; van Hasselt, C.A. Patient satisfaction after closed reduction of nasal fractures. Arch. Facial Plast. Surg. 2007, 9, 40–43. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sharma, S.D.; Kwame, I.; Almeyda, J. Patient aesthetic satisfaction with timing of nasal fracture manipulation. Surg. Res. Pract. 2014, 2014, 238520. [Google Scholar] [CrossRef] [PubMed]
- Hauters, P.; Auvray, S.; Cardin, J.L.; Papillon, M.; Delaby, J.; Dabrowski, A.; Framery, D.; Valverde, A.; Rubay, R.; Siriser, F.; et al. Comparison between single-incision and conventional laparoscopic cholecystectomy: A prospective trial of the Club Coelio. Surg. Endosc. 2013, 27, 1689–1694. [Google Scholar] [CrossRef] [PubMed]

| Parameter | Conventional n = 42 | Suprapubic n = 28 | p |
|---|---|---|---|
| Demographics | |||
| Male, n (%) | 6 (14%) | 6 (21%) | 0.650 |
| Age, median (IQR) | 53 (41 to 66) | 54 (42 to 64) | 0.893 |
| BMI, median (IQR) | 27 (25 to 32) | 27 (25 to 32) | 0.898 |
| ASA Grade III, n (%) | 4 (10%) | 4 (14%) | 0.818 |
| Surgical Outcome | |||
| Length of stay (d), median (IQR) | 3 (3 to 4) | 3 (3 to 3) | 0.076 |
| Surgical time (min.), median (IQR) | 66 (50 to 86) | 70 (65 to 82) | 0.245 |
| Complications, n (%) | 6 (14 %) | 1 (3,5%) | 0.290 |
| Aesthetic Outcome | |||
| Overall (Pooled), median (IQR) | 4.2 (3.8 to 4.4) | 4.8 (4.8 to 4.9) | <0.001 * |
| Medical Staff (Pooled), median (IQR) | 4.0 (3.8 to 4.2) | 4.8 (4.6 to 5.0) | <0.001 * |
| Non-Medical Staff (Pooled), median (IQR) | 4.2 (3.8 to 4.6) | 5.0 (4.8 to 5.0) | <0.001 * |
| Plastic Surgeon, median (IQR) | 4.0 (4.0 to 4.0) | 5.0 (5.0 to 5.0) | <0.001 * |
| Complication (n = 7) | Clavien-Dindo Classification | Group |
|---|---|---|
| Renal insufficiency (n = 1) | I | Suprapubic |
| Intractable pain (n = 3) | I | Conventional |
| Pancreatitis (n = 1) | III b | Conventional |
| Hematoma (n = 2) | III b | Conventional |
| Raters | No. of Raters | ICC for Consistency (95% CI) |
|---|---|---|
| Overall | 10 | 0.46 (0.37 to 0.57) |
| Medical Staff | 5 | 0.47 (0.36 to 0.58) |
| Non-Medical Staff | 5 | 0.45 (0.34 to 0.57) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Taha, A.; Taha-Mehlitz, S.; Sternkopf, U.; Sorba, E.; Enodien, B.; Vorburger, S. Suprapubic Cholecystectomy Improves Cosmetic Outcome Compared to Classic Cholecystectomy. J. Clin. Med. 2022, 11, 4579. https://doi.org/10.3390/jcm11154579
Taha A, Taha-Mehlitz S, Sternkopf U, Sorba E, Enodien B, Vorburger S. Suprapubic Cholecystectomy Improves Cosmetic Outcome Compared to Classic Cholecystectomy. Journal of Clinical Medicine. 2022; 11(15):4579. https://doi.org/10.3390/jcm11154579
Chicago/Turabian StyleTaha, Anas, Stephanie Taha-Mehlitz, Ulrich Sternkopf, Elena Sorba, Bassey Enodien, and Stephan Vorburger. 2022. "Suprapubic Cholecystectomy Improves Cosmetic Outcome Compared to Classic Cholecystectomy" Journal of Clinical Medicine 11, no. 15: 4579. https://doi.org/10.3390/jcm11154579
APA StyleTaha, A., Taha-Mehlitz, S., Sternkopf, U., Sorba, E., Enodien, B., & Vorburger, S. (2022). Suprapubic Cholecystectomy Improves Cosmetic Outcome Compared to Classic Cholecystectomy. Journal of Clinical Medicine, 11(15), 4579. https://doi.org/10.3390/jcm11154579






