Second- and Third-Tier Therapies for Severe Traumatic Brain Injury
Abstract
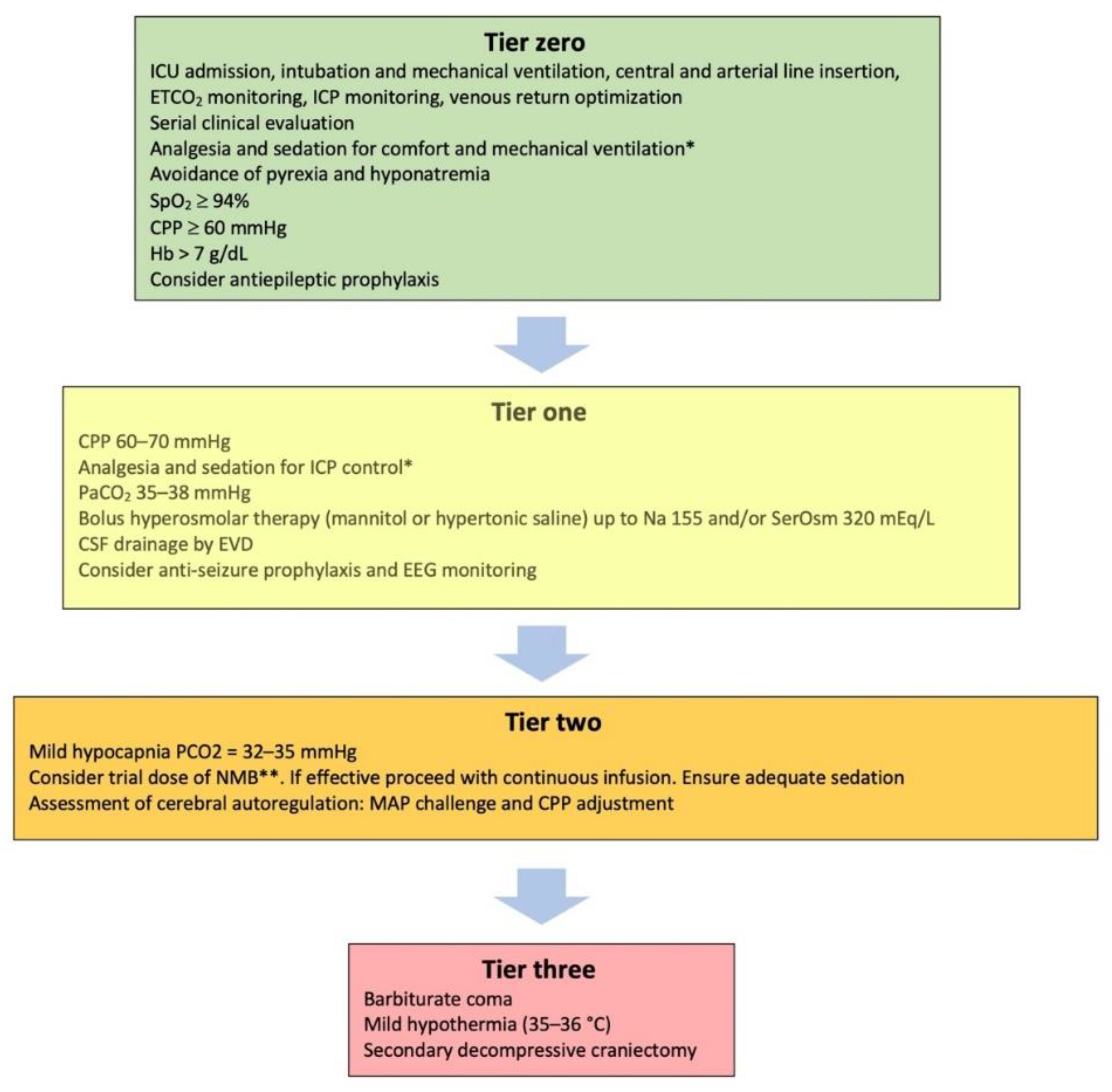
:1. Introduction
2. Tier-Two Therapies
2.1. Mild Hypocapnia (PaCO2 32–35 mmHg)
2.2. Neuromuscular Blockade (NMB)
2.3. Assessment of Static Autoregulation—The Mean Arterial Pressure (MAP) Challenge
3. Tier-Three Therapies
3.1. Therapeutic Hypothermia
3.2. Metabolic Suppression with Barbiturates
3.3. Decompressive Craniectomy
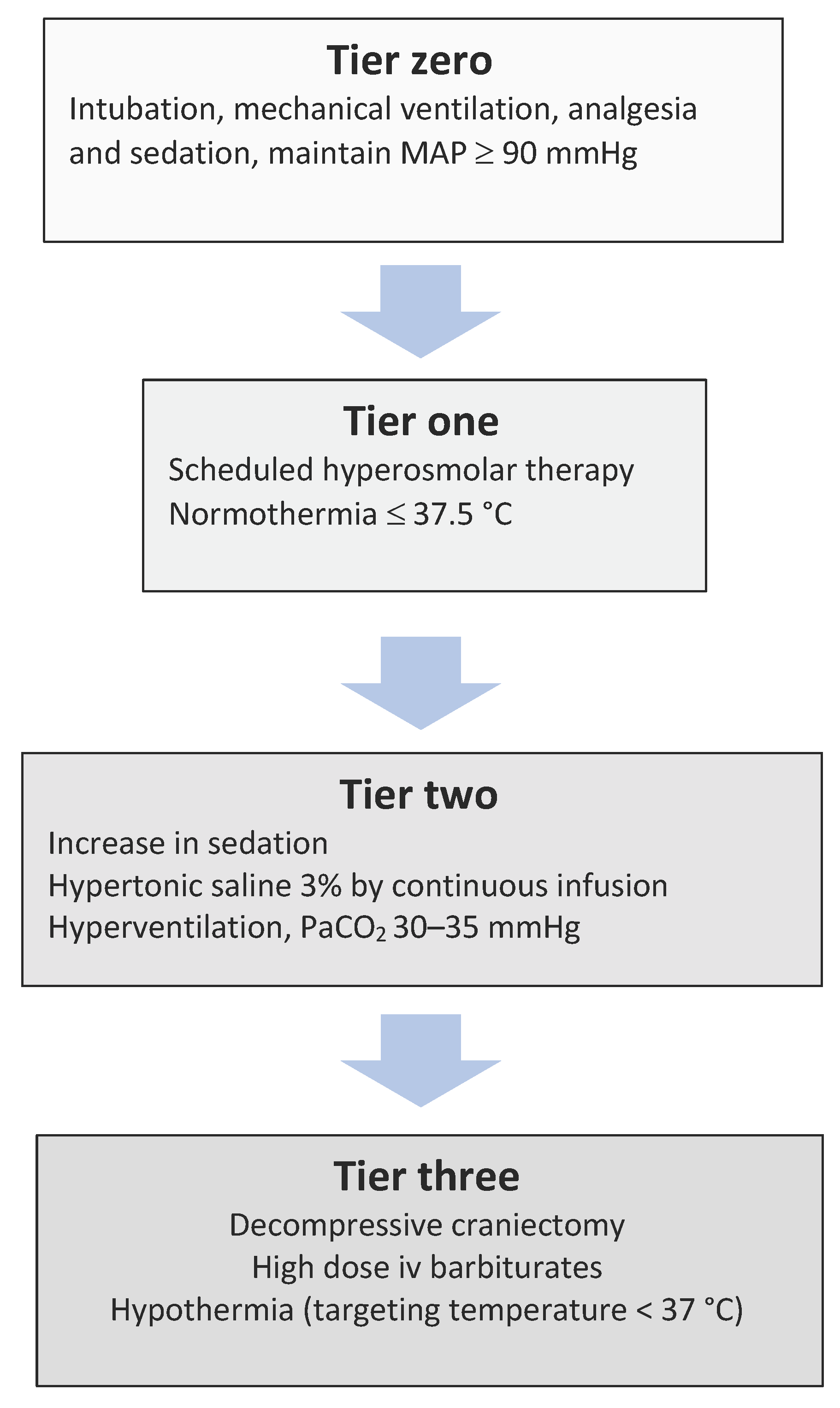
4. Second- and Third-Tier Therapies in Low- and Middle-Income Countries (LMICs)
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Menon, D.K.; Schwab, K.; Wright, D.W.; Maas, A.I. Position Statement: Definition of Traumatic Brain Injury. Arch. Phys. Med. Rehabil. 2010, 91, 1637–1640. [Google Scholar] [CrossRef] [PubMed]
- Clark, D.; Joannides, A.; Adeleye, A.O.; Bajamal, A.H.; Bashford, T.; Biluts, H.; Budohoski, K.; Ercole, A.; Fernández-Méndez, R.; Figaji, A.; et al. Casemix, Management, and Mortality of Patients Receiving Emergency Neurosurgery for Traumatic Brain Injury in the Global Neurotrauma Outcomes Study: A Prospective Observational Cohort Study. Lancet Neurol. 2022, 21, 438–449. [Google Scholar] [CrossRef]
- Menon, D.K.; Ercole, A. Critical Care Management of Traumatic Brain Injury. In Handbook of Clinical Neurology; Elsevier B.V.: Amsterdam, The Netherlands, 2017; Volume 140, pp. 239–274. [Google Scholar]
- Maas, A.I.R.; Menon, D.K.; David Adelson, P.D.; Andelic, N.; Bell, M.J.; Belli, A.; Bragge, P.; Brazinova, A.; Büki, A.; Chesnut, R.M.; et al. Traumatic Brain Injury: Integrated Approaches to Improve Prevention, Clinical Care, and Research. Lancet Neurol. 2017, 16, 987–1048. [Google Scholar] [CrossRef]
- Vik, A.; Nag, T.; Fredriksli, O.A.; Skandsen, T.; Moen, K.G.; Schirmer-Mikalsen, K.; Manley, G.T. Relationship of “Dose” of Intracranial Hypertension to Outcome in Severe Traumatic Brain Injury. J. Neurosurg. 2008, 109, 678–684. [Google Scholar] [CrossRef] [PubMed]
- Kahraman, S.; Dutton, R.P.; Hu, P.; Xiao, Y.; Aarabi, B.; Stein, D.M.; Scalea, T.M. Automated Measurement of “Pressure Times Time Dose” of Intracranial Hypertension Best Predicts Outcome after Severe Traumatic Brain Injury. J. Trauma-Inj. Infect. Crit. Care 2010, 69, 110–118. [Google Scholar] [CrossRef]
- Güiza, F.; Depreitere, B.; Piper, I.; Citerio, G.; Chambers, I.; Jones, P.A.; Lo, T.Y.M.; Enblad, P.; Nillson, P.; Feyen, B.; et al. Visualizing the Pressure and Time Burden of Intracranial Hypertension in Adult and Paediatric Traumatic Brain Injury. Intensive Care Med. 2015, 41, 1067–1076. [Google Scholar] [CrossRef]
- Hawryluk, G.W.J.; Aguilera, S.; Buki, A.; Bulger, E.; Citerio, G.; Cooper, D.J.; Arrastia, R.D.; Diringer, M.; Figaji, A.; Gao, G.; et al. A Management Algorithm for Patients with Intracranial Pressure Monitoring: The Seattle International Severe Traumatic Brain Injury Consensus Conference (SIBICC). Intensive Care Med. 2019, 45, 1783–1794. [Google Scholar] [CrossRef]
- Stocchetti, N.; Maas, A.I.R. Traumatic Intracranial Hypertension. N. Engl. J. Med. 2014, 370, 2121–2130. [Google Scholar] [CrossRef]
- Meyfroidt, G.; Bouzat, P.; Casaer, M.P.; Chesnut, R.; Hamada, S.R.; Helbok, R.; Hutchinson, P.; Maas, A.I.R.; Manley, G.; Menon, D.K.; et al. Management of Moderate to Severe Traumatic Brain Injury: An Update for the Intensivist. Intensive Care Med. 2022, 48, 649–666. [Google Scholar] [CrossRef]
- Stocchetti, N.; Carbonara, M.; Citerio, G.; Ercole, A.; Skrifvars, M.B.; Smielewski, P.; Zoerle, T.; Menon, D.K. Severe Traumatic Brain Injury: Targeted Management in the Intensive Care Unit. Lancet Neurol. 2017, 16, 452–464. [Google Scholar] [CrossRef]
- Stocchetti, N.; Zoerle, T.; Carbonara, M. Intracranial Pressure Management in Patients with Traumatic Brain Injury: An Update. Curr. Opin. Crit. Care 2017, 23, 110–114. [Google Scholar] [CrossRef] [PubMed]
- Carney, N.; Totten, A.M.; O’Reilly, C.; Ullman, J.S.; Hawryluk, G.W.J.; Bell, M.J.; Bratton, S.L.; Chesnut, R.; Harris, O.A.; Kissoon, N.; et al. Guidelines for the Management of Severe Traumatic Brain Injury, Fourth Edition. Neurosurgery 2017, 80, 6–15. [Google Scholar] [CrossRef] [PubMed]
- Huijben, J.A.; Dixit, A.; Stocchetti, N.; Maas, A.I.R.; Lingsma, H.F.; van der Jagt, M.; Nelson, D.; Citerio, G.; Wilson, L.; Menon, D.K.; et al. Use and Impact of High Intensity Treatments in Patients with Traumatic Brain Injury across Europe: A CENTER-TBI Analysis. Crit. Care 2021, 25, 78. [Google Scholar] [CrossRef] [PubMed]
- Gelormini, C.; Caricato, A. “Tier-Three” Therapies in Intracranial Hypertension: Is It Worthwhile? Minerva Anestesiol. 2021, 87, 1287–1289. [Google Scholar] [CrossRef] [PubMed]
- Robba, C.; Iannuzzi, F.; Taccone, F.S. Tier-Three Therapies for Refractory Intracranial Hypertension in Adult Head Trauma. Minerva Anestesiol. 2021, 87, 1359–1366. [Google Scholar] [CrossRef]
- Adatia, K.; Newcombe, V.F.J.; Menon, D.K. Contusion Progression Following Traumatic Brain Injury: A Review of Clinical and Radiological Predictors, and Influence on Outcome. Neurocrit. Care 2021, 34, 312–324. [Google Scholar] [CrossRef]
- Iaccarino, C.; Lippa, L.; Munari, M.; Castioni, C.A.; Robba, C.; Caricato, A.; Pompucci, A.; Signoretti, S.; Zona, G.; Rasulo, F.A.; et al. Management of Intracranial Hypertension Following Traumatic Brain Injury: A Best Clinical Practice Adoption Proposal for Intracranial Pressure Monitoring and Decompressive Craniectomy: Joint Statements by the Traumatic Brain Injury Section of the Italian Society of Neurosurgery (SINch) and the Neuroanesthesia and Neurocritical Care Study Group of the Italian Society of Anesthesia, Analgesia, Resuscitation and Intensive Care (SIAARTI). J. Neurosurg. Sci. 2021, 65, 219–238. [Google Scholar]
- Cnossen, M.C.; Huijben, J.A.; van der Jagt, M.; Volovici, V.; van Essen, T.; Polinder, S.; Nelson, D.; Ercole, A.; Stocchetti, N.; Citerio, G.; et al. Variation in Monitoring and Treatment Policies for Intracranial Hypertension in Traumatic Brain Injury: A Survey in 66 Neurotrauma Centers Participating in the CENTER-TBI Study. Crit. Care 2017, 21, 233. [Google Scholar] [CrossRef]
- Roberts, D.J.; Hall, R.I.; Kramer, A.H.; Robertson, H.L.; Gallagher, C.N.; Zygun, D.A. Sedation for Critically Ill Adults with Severe Traumatic Brain Injury: A Systematic Review of Randomized Controlled Trials. Crit. Care Med. 2011, 39, 2743–2751. [Google Scholar] [CrossRef]
- Sanfilippo, F.; Santonocito, C.; Veenith, T.; Astuto, M.; Maybauer, M.O. The Role of Neuromuscular Blockade in Patients with Traumatic Brain Injury: A Systematic Review. Neurocrit. Care 2015, 22, 325–334. [Google Scholar] [CrossRef]
- Brain Trauma Foundation; American Association of Neurological Surgeons; Congress of Neurological Surgeons. Guidelines for the management of severe traumatic brain injury. J. Neurotrauma. 2007, 24 (Suppl. S1), S1–S106, Erratum in J. Neurotrauma 2008, 25, 276–278. [Google Scholar] [CrossRef]
- AlAzri, A.; Mok, K.; Chankowsky, J.; Mullah, M.; Marcoux, J. Placement Accuracy of External Ventricular Drain When Comparing Freehand Insertion to Neuronavigation Guidance in Severe Traumatic Brain Injury. Acta Neurochir. 2017, 159, 1399–1411. [Google Scholar] [CrossRef] [PubMed]
- Ramanan, M.; Lipman, J.; Shorr, A.; Shankar, A. A Meta-Analysis of Ventriculostomy-Associated Cerebrospinal Fluid Infections. BMC Infect. Dis. 2015, 15, 3. [Google Scholar] [CrossRef]
- Godoy, D.A.; Seifi, A.; Garza, D.; Lubillo-Montenegro, S.; Murillo-Cabezas, F. Hyperventilation Therapy for Control of Posttraumatic Intracranial Hypertension. Front. Neurol. 2017, 8, 250. [Google Scholar] [CrossRef] [PubMed]
- Coles, J.P.; Fryer, T.D.; Coleman, M.R.; Smielewski, P.; Gupta, A.K.; Minhas, P.S.; Aigbirhio, F.; Chatfield, D.A.; Williams, G.B.; Boniface, S.; et al. Hyperventilation Following Head Injury: Effect on Ischemic Burden and Cerebral Oxidative Metabolism. Crit. Care Med. 2007, 35, 568–578. [Google Scholar] [CrossRef]
- Beqiri, E.; Czosnyka, M.; Lalou, A.D.; Zeiler, F.A.; Fedriga, M.; Steiner, L.A.; Chieregato, A.; Smielewski, P. Influence of Mild-Moderate Hypocapnia on Intracranial Pressure Slow Waves Activity in TBI. Acta Neurochir. 2020, 162, 345–356. [Google Scholar] [CrossRef]
- Geeraerts, T. Moderate Hypocapnia for Intracranial Pressure Control after Traumatic Brain Injury: A Common Practice Requiring Further Investigations. Intensive Care Med. 2021, 47, 1009–1010. [Google Scholar] [CrossRef]
- Godoy, D.A.; Badenes, R.; Robba, C.; Murillo Cabezas, F. Hyperventilation in Severe Traumatic Brain Injury Has Something Changed in the Last Decade or Uncertainty Continues? A Brief Review. Front. Neurol. 2021, 12, 573237. [Google Scholar] [CrossRef]
- Brandi, G.; Stocchetti, N.; Pagnamenta, A.; Stretti, F.; Steiger, P.; Klinzing, S. Cerebral Metabolism Is Not Affected by Moderate Hyperventilation in Patients with Traumatic Brain Injury. Crit. Care 2019, 23, 45. [Google Scholar] [CrossRef]
- Gouvea Bogossian, E.; Peluso, L.; Creteur, J.; Taccone, F.S. Hyperventilation in Adult TBI Patients: How to Approach It? Front. Neurol. 2021, 11, 580859. [Google Scholar] [CrossRef]
- Imberti, R.; Bellinzona, G.; Langer, M. Cerebral tissue PO2 and SjvO2 changes during moderate hyperventilation in patients with severe traumatic brain injury. J. Neurosurg. 2002, 96, 97–102. [Google Scholar] [CrossRef]
- Meyer, N.J.; Gattinoni, L.; Calfee, C.S. Acute Respiratory Distress Syndrome. Lancet 2021, 398, 622–637. [Google Scholar] [CrossRef]
- Cai, G.; Zhang, X.; Ou, Q.; Zhou, Y.; Huang, L.; Chen, S.; Zeng, H.; Jiang, W.; Wen, M. Optimal Targets of the First 24-h Partial Pressure of Carbon Dioxide in Patients with Cerebral Injury: Data from the MIMIC-III and IV Database. Neurocrit. Care 2022, 36, 412–420. [Google Scholar] [CrossRef] [PubMed]
- Papazian, L.; Forel, J.-M.; Gacouin, A.; Penot-Ragon, C.; Perrin, G.; Loundou, A.; Jaber, S.; Arnal, J.-M.; Perez, D.; Seghboyan, J.-M.; et al. Neuromuscular Blockers in Early Acute Respiratory Distress Syndrome. N. Engl. J. Med. 2010, 363, 1107–1116. [Google Scholar] [CrossRef]
- Hsiang, J.K.; Chesnut, R.M.; Crisp, C.B.; Klauber, M.R.; Blunt, B.A.; Marshall, L.F. Early, routine paralysis for intracranial pressure control in severe head injury: Is it necessary? Crit. Care Med. 1994, 22, 1471–1476. [Google Scholar] [CrossRef] [PubMed]
- Murray, M.J.; Deblock, H.; Erstad, B.; Gray, A.; Jacobi, J.; Jordan, C.; McGee, W.; McManus, C.; Meade, M.; Nix, S.; et al. Clinical Practice Guidelines for Sustained Neuromuscular Blockade in the Adult Critically Ill Patient. Crit. Care Med. 2016, 44, 2079–2103. [Google Scholar] [CrossRef]
- Hermans, G.; van den Berghe, G. Clinical Review: Intensive Care Unit Acquired Weakness. Crit. Care 2015, 19, 274. [Google Scholar] [CrossRef]
- Inoue, S.; Hatakeyama, J.; Kondo, Y.; Hifumi, T.; Sakuramoto, H.; Kawasaki, T.; Taito, S.; Nakamura, K.; Unoki, T.; Kawai, Y.; et al. Post-intensive Care Syndrome: Its Pathophysiology, Prevention, and Future Directions. Acute Med. Surg. 2019, 6, 233–246. [Google Scholar] [CrossRef]
- Lee, M.; Kang, J.; Jeong, Y.J. Risk Factors for Post–Intensive Care Syndrome: A Systematic Review and Meta-Analysis. Aust. Crit. Care 2020, 33, 287–294. [Google Scholar] [CrossRef]
- Price, D.R.; Mikkelsen, M.E.; Umscheid, C.A.; Armstrong, E.J. Neuromuscular Blocking Agents and Neuromuscular Dysfunction Acquired in Critical Illness: A Systematic Review and Meta-Analysis. Crit. Care Med. 2016, 44, 2070–2078. [Google Scholar] [CrossRef]
- De Laet, I.; Hoste, E.; Verholen, E.; de Waele, J.J. The Effect of Neuromuscular Blockers in Patients with Intra-Abdominal Hypertension. Intensive Care Med. 2007, 33, 1811–1814. [Google Scholar] [CrossRef] [PubMed]
- Oddo, M.; Crippa, I.A.; Mehta, S.; Menon, D.; Payen, J.F.; Taccone, F.S.; Citerio, G. Optimizing Sedation in Patients with Acute Brain Injury. Crit. Care 2016, 20, 128. [Google Scholar] [CrossRef]
- Mccall, M.; Jeejeebhoy, K.; Pencharz, P.; Moulton, R. Effect of Neuromuscular Blockade on Energy Expenditure in Patients With Severe Head Injury. J. Parenter. Enteral Nutr. 2003, 27, 27–35. [Google Scholar] [CrossRef] [PubMed]
- Rangel-Castilla, L.; Gasco, J.; Nauta, H.J.W.; Okonkwo, D.O.; Robertson, C.S. Cerebral Pressure Autoregulation in Traumatic Brain Injury. Neurosurg. Focus 2008, 25, E7. [Google Scholar] [CrossRef] [PubMed]
- Donnelly, J.; Czosnyka, M.; Adams, H.; Robba, C.; Steiner, L.A.; Cardim, D.; Cabella, B.; Liu, X.; Ercole, A.; Hutchinson, P.J.; et al. Individualizing Thresholds of Cerebral Perfusion Pressure Using Estimated Limits of Autoregulation. Crit. Care Med. 2017, 45, 1464–1471. [Google Scholar] [CrossRef]
- Robba, C.; Cardim, D.; Sekhon, M.; Budohoski, K.; Czosnyka, M. Transcranial Doppler: A Stethoscope for the Brain-Neurocritical Care Use. J. Neurosci. Res. 2018, 96, 720–730. [Google Scholar] [CrossRef]
- Rosenthal, G.; Sanchez-Mejia, R.O.; Phan, N.; Hemphill, J.C.; Martin, C.; Manley, G.T. Incorporating a Parenchymal Thermal Diffusion Cerebral Blood Flow Probe in Bedside Assessment of Cerebral Autoregulation and Vasoreactivity in Patients with Severe Traumatic Brain Injury: Clinical Article. J. Neurosurg. 2011, 114, 62–70. [Google Scholar] [CrossRef]
- Hawryluk, G.W.J.; Rubiano, A.M.; Totten, A.M.; O’Reilly, C.; Ullman, J.S.; Bratton, S.L.; Chesnut, R.; Harris, O.A.; Kissoon, N.; Shutter, L.; et al. Guidelines for the Management of Severe Traumatic Brain Injury: 2020 Update of the Decompressive Craniectomy Recommendations. Neurosurgery 2020, 87, 427–434. [Google Scholar] [CrossRef]
- Lang, E.W.; Chesnut, R.M. A Bedside Method for Investigating the Integrity and Critical Thresholds of Cerebral Pressure Autoregulation in Severe Traumatic Brain Injury Patients. Br. J. Neurosurg. 2000, 14, 117–126. [Google Scholar]
- Annane, D.; Ouanes-Besbes, L.; de Backer, D.; Gordon, A.C.; Hernández, G.; Olsen, K.M.; Osborn, T.M.; Russell, J.A.; Zanotti Cavazzoni, S.; Peake, S.; et al. A Global Perspective on Vasoactive Agents in Shock. Intensive Care Med. 2018, 44, 833–846. [Google Scholar] [CrossRef]
- Depreitere, B.; Citerio, G.; Smith, M.; Adelson, P.D.; Aries, M.J.; Bleck, T.P.; Bouzat, P.; Chesnut, R.; de Sloovere, V.; Diringer, M.; et al. Cerebrovascular Autoregulation Monitoring in the Management of Adult Severe Traumatic Brain Injury: A Delphi Consensus of Clinicians. Neurocrit. Care 2021, 34, 731–738. [Google Scholar] [CrossRef] [PubMed]
- Moerman, A.; de Hert, S. Why and How to Assess Cerebral Autoregulation? Best Pract. Res. Clin. Anaesthesiol. 2019, 33, 211–220. [Google Scholar] [CrossRef]
- Hirst, T.C.; Klasen, M.G.; Rhodes, J.K.; MacLeod, M.R.; Andrews, P.J.D. A Systematic Review and Meta-Analysis of Hypothermia in Experimental Traumatic Brain Injury: Why Have Promising Animal Studies Not Been Replicated in Pragmatic Clinical Trials? J. Neurotrauma 2020, 37, 2057–2068. [Google Scholar] [CrossRef]
- Ceulemans, A.G.; Zgavc, T.; Kooijman, R.; Hachimi-Idrissi, S.; Sarre, S.; Michotte, Y. The Dual Role of the Neuroinflammatory Response after Ischemic Stroke: Modulatory Effects of Hypothermia. J. Neuroinflamm. 2010, 7, 74. [Google Scholar] [CrossRef]
- Zhu, Y.; Yin, H.; Zhang, R.; Ye, X.; Wei, J. Therapeutic Hypothermia versus Normothermia in Adult Patients with Traumatic Brain Injury: A Meta-Analysis. Springerplus 2016, 5, 801. [Google Scholar] [CrossRef]
- Andrews, P.J.D.; Sinclair, H.L.; Rodriguez, A.; Harris, B.A.; Battison, C.G.; Rhodes, J.K.J.; Murray, G.D. Hypothermia for Intracranial Hypertension after Traumatic Brain Injury. N. Engl. J. Med. 2015, 373, 2403–2412. [Google Scholar] [CrossRef]
- Cooper, D.J.; Nichol, A.D.; Bailey, M.; Bernard, S.; Cameron, P.A.; Pili-Floury, S.; Forbes, A.; Gantner, D.; Higgins, A.M.; Huet, O.; et al. Effect of Early Sustained Prophylactic Hypothermia on Neurologic Outcomes among Patients with Severe Traumatic Brain Injury. JAMA-J. Am. Med. Assoc. 2018, 320, 2211–2220. [Google Scholar] [CrossRef]
- Polderman, K.H. Application of Therapeutic Hypothermia in the Intensive Care Unit: Opportunities and Pitfalls of a Promising Treatment Modality-Part 2: Practical Aspects and Side Effects. Intensive Care Med. 2004, 30, 757–769. [Google Scholar] [CrossRef]
- Rubiano, A.M.; Sanchez, A.I.; Estebanez, G.; Peitzman, A.; Sperry, J.; Puyana, J.C. The Effect of Admission Spontaneous Hypothermia on Patients with Severe Traumatic Brain Injury. Injury 2013, 44, 1219–1225. [Google Scholar] [CrossRef]
- Zwerus, R.; Absalom, A. Update on Anesthetic Neuroprotection. Curr. Opin. Anaesthesiol. 2015, 28, 424–430. [Google Scholar] [CrossRef]
- Almaas, R.; Saugstad, O.D.; Pleasure, D.; Rootwelt, T. Effect of Barbiturates on Hydroxyl Radicals, Lipid Peroxidation, and Hypoxic Cell Death in Human NT2-N Neurons. Anesthesiology 2000, 92, 764–774. [Google Scholar] [CrossRef]
- Léger, M.; Frasca, D.; Roquilly, A.; Seguin, P.; Cinotti, R.; Dahyot-Fizelier, C.; Asehnoune, K.; le Borgne, F.; Gaillard, T.; Foucher, Y.; et al. Early Use of Barbiturates Is Associated with Increased Mortality in Traumatic Brain Injury Patients from a Propensity Score-Based Analysis of a Prospective Cohort. PLoS ONE 2022, 17, e0268013. [Google Scholar] [CrossRef]
- Majdan, M.; Mauritz, W.; Wilbacher, I.; Brazinova, A.; Rusnak, M.; Leitgeb, J. Barbiturates Use and Its Effects in Patients with Severe Traumatic Brain Injury in Five European Countries. J. Neurotrauma 2013, 30, 23–29. [Google Scholar] [CrossRef] [PubMed]
- Roberts, I.; Sydenham, E. Barbiturates for Acute Traumatic Brain Injury. Cochrane Database Syst. Rev. 2012, 2012, CD000033. [Google Scholar] [CrossRef]
- Cairns, C.J.; Thomas, B.; Fletcher, S.; Parr, M.J.; Finfer, S.R. Life-Threatening Hyperkalaemia Following Therapeutic Barbiturate Coma. Intensive Care Med. 2002, 28, 1357–1360. [Google Scholar] [CrossRef]
- Aytuluk, H.G.; Topcu, H. Severe Hypokalemia and Rebound Hyperkalemia during Barbiturate Coma in Patients with Severe Traumatic Brain Injury. Neurocirugia 2020, 31, 216–222. [Google Scholar] [CrossRef]
- Stover, J.F.; Stocker, R. PHARMACOD YNAMICS Barbiturate Coma May Promote Reversible Bone Marrow Suppression in Patients with Severe Isolated Traumatic Brain Injury. Eur. J. Clin. Pharmacol. 1998, 54, 529–534. [Google Scholar] [CrossRef]
- Stover, J.F.; Lenzlinger, P.M.; Stocker, R.; Morganti-Kossmann, M.C.; Imhof, H.G.; Trentz, O.; Kossmann, T. Thiopental in CSF and Serum Correlates with Prolonged Loss of Cortical Activity. Eur. Neurol. 1998, 39, 223–228. [Google Scholar] [CrossRef]
- Wheeler, D.W.; Thompson, A.J.; Corletto, F.; Reckless, J.; Loke, J.C.T.; Lapaque, N.; Grant, A.J.; Mastroeni, P.; Grainger, D.J.; Padgett, C.L.; et al. Anaesthetic Impairment of Immune Function Is Mediated via GABAA Receptors. PLoS ONE 2011, 6, e17152. [Google Scholar] [CrossRef]
- Loop, T.; Humar, M.; Pischke, S.; Hoetzel, A.; Schmidt, R.; Pahl, H.L.; Geiger, K.K.; Pannen, B.H.J. Thiopental Inhibits Tumor Necrosis Factor-Induced Activation of Nuclear Factor B through Suppression of IB Kinase Activity. Anesthesiology 2003, 99, 360–367. [Google Scholar] [CrossRef]
- Andrefsky, J.C.; Frank, J.I.; Chyatte, D. The ciliospinal reflex in pentobarbital coma. J. Neurosurg. 1999, 90, 644–646. [Google Scholar] [CrossRef]
- Ellington, A.L. Electroencephalographic pattern of burst suppression in a case of barbiturate coma. Electroencephalogr. Clin. Neurophysiol. 1968, 25, 491–493. [Google Scholar] [CrossRef]
- Zeiler, F.A.; Akoth, E.; Gillman, L.M.; West, M. Burst Suppression for ICP Control: A Systematic Review. J. Intensive Care Med. 2017, 32, 130–139. [Google Scholar] [CrossRef] [PubMed]
- Wechsler, R.L.; Dripps, R.D.; Kety, S.S. Blood flow and oxygen consumption of the human brain during anesthesia produced by thiopental. Anesthesiology 1951, 12, 308–314. [Google Scholar] [CrossRef] [PubMed]
- Hemphill, S.; McMenamin, L.; Bellamy, M.C.; Hopkins, P.M. Propofol Infusion Syndrome: A Structured Literature Review and Analysis of Published Case Reports. Br. J. Anaesth. 2019, 122, 448–459. [Google Scholar] [CrossRef]
- Cooper, D.J.; Rosenfeld, J.V.; Murray, L.; Arabi, Y.M.; Davies, A.R.; D’Urso, P.; Kossmann, T.; Ponsford, J.; Seppelt, I.; Reilly, P.; et al. Decompressive Craniectomy in Diffuse Traumatic Brain Injury. N. Engl. J. Med. 2011, 364, 1493–1502. [Google Scholar] [CrossRef]
- Hutchinson, P.J.; Kolias, A.G.; Timofeev, I.S.; Corteen, E.A.; Czosnyka, M.; Timothy, J.; Anderson, I.; Bulters, D.O.; Belli, A.; Eynon, C.A.; et al. Trial of Decompressive Craniectomy for Traumatic Intracranial Hypertension. N. Engl. J. Med. 2016, 375, 1119–1130. [Google Scholar] [CrossRef]
- Hutchinson, P.J.; Kolias, A.G.; Tajsic, T.; Adeleye, A.; Aklilu, A.T.; Apriawan, T.; Bajamal, A.H.; Barthélemy, E.J.; Devi, B.I.; Bhat, D.; et al. Consensus Statement from the International Consensus Meeting on the Role of Decompressive Craniectomy in the Management of Traumatic Brain Injury: Consensus Statement. Acta Neurochir. 2019, 161, 1261–1274. [Google Scholar] [CrossRef]
- Hartings, J.A.; Vidgeon, S.; Strong, A.J.; Zacko, C.; Vagal, A.; Andaluz, N.; Ridder, T.; Stanger, R.; Fabricius, M.; Mathern, B.; et al. Surgical Management of Traumatic Brain Injury: A Comparative-Effectiveness Study of 2 Centers: Clinical Article. J. Neurosurg. 2014, 120, 434–446. [Google Scholar] [CrossRef]
- Li, L.M.; Kolias, A.G.; Guilfoyle, M.R.; Timofeev, I.; Corteen, E.A.; Pickard, J.D.; Menon, D.K.; Kirkpatrick, P.J.; Hutchinson, P.J. Outcome Following Evacuation of Acute Subdural Haematomas: A Comparison of Craniotomy with Decompressive Craniectomy. Acta Neurochir. 2012, 154, 1555–1561. [Google Scholar] [CrossRef]
- Kolias, A.G.; Adams, H.; Timofeev, I.; Czosnyka, M.; Corteen, E.A.; Pickard, J.D.; Turner, C.; Gregson, B.A.; Kirkpatrick, P.J.; Murray, G.D.; et al. Decompressive Craniectomy Following Traumatic Brain Injury: Developing the Evidence Base. Br. J. Neurosurg. 2016, 30, 246–250. [Google Scholar] [CrossRef] [PubMed]
- Chesnut, R.M.; Temkin, N.; Carney, N.; Dikmen, S.; Rondina, C.; Videtta, W.; Petroni, G.; Lujan, S.; Pridgeon, J.; Barber, J.; et al. A Trial of Intracranial-Pressure Monitoring in Traumatic Brain Injury. N. Engl. J. Med. 2012, 367, 2471–2481. [Google Scholar] [CrossRef] [PubMed]
- Chesnut, R.M.; Temkin, N.; Dikmen, S.; Rondina, C.; Videtta, W.; Petroni, G.; Lujan, S.; Alanis, V.; Falcao, A.; de La Fuenta, G.; et al. A Method of Managing Severe Traumatic Brain Injury in the Absence of Intracranial Pressure Monitoring: The Imaging and Clinical Examination Protocol. J. Neurotrauma 2018, 35, 54–63. [Google Scholar] [CrossRef]
- Kolias, A.G.; Viaroli, E.; Rubiano, A.M.; Adams, H.; Khan, T.; Gupta, D.; Adeleye, A.; Iaccarino, C.; Servadei, F.; Devi, B.I.; et al. The Current Status of Decompressive Craniectomy in Traumatic Brain Injury. Curr. Trauma Rep. 2018, 4, 326–332. [Google Scholar] [CrossRef]

Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Vrettou, C.S.; Mentzelopoulos, S.D. Second- and Third-Tier Therapies for Severe Traumatic Brain Injury. J. Clin. Med. 2022, 11, 4790. https://doi.org/10.3390/jcm11164790
Vrettou CS, Mentzelopoulos SD. Second- and Third-Tier Therapies for Severe Traumatic Brain Injury. Journal of Clinical Medicine. 2022; 11(16):4790. https://doi.org/10.3390/jcm11164790
Chicago/Turabian StyleVrettou, Charikleia S., and Spyros D. Mentzelopoulos. 2022. "Second- and Third-Tier Therapies for Severe Traumatic Brain Injury" Journal of Clinical Medicine 11, no. 16: 4790. https://doi.org/10.3390/jcm11164790
APA StyleVrettou, C. S., & Mentzelopoulos, S. D. (2022). Second- and Third-Tier Therapies for Severe Traumatic Brain Injury. Journal of Clinical Medicine, 11(16), 4790. https://doi.org/10.3390/jcm11164790






