Exercise Hypertension in Athletes
Abstract
1. Introduction
2. Materials and Methods
2.1. Enrolled Subjects
2.2. Ethical Aspects
2.3. Definitions
- American Heart Association (AHA) guidelines [23]: systolic peak BP >210 mmHg in men, >190 mmHg in women, and/or >90 mmHg diastolic peak BP in both sexes.
- The systolic BP/MET slope method [44,45,46,47]: The Δ regarding systolic BP was calculated as maximum systolic BP during exercise—systolic BP at rest and was indexed by the increase in MET from rest (Δ regarding MET was calculated as peak MET-1) to obtain the systolic BP/MET slope [46]. In accordance with previous studies, a cutoff value > 6.2 mmHg/MET was used to define an EBPR [44,46]. The MET value was calculated based on the athletes’ VO2 maximum values during exercise testing as recommended by the ACSM guideline (MET = VO2max/3.5 mL·kg−1·min−1) [48].
2.4. Statistics
3. Results
3.1. Athletes’ Characteristics
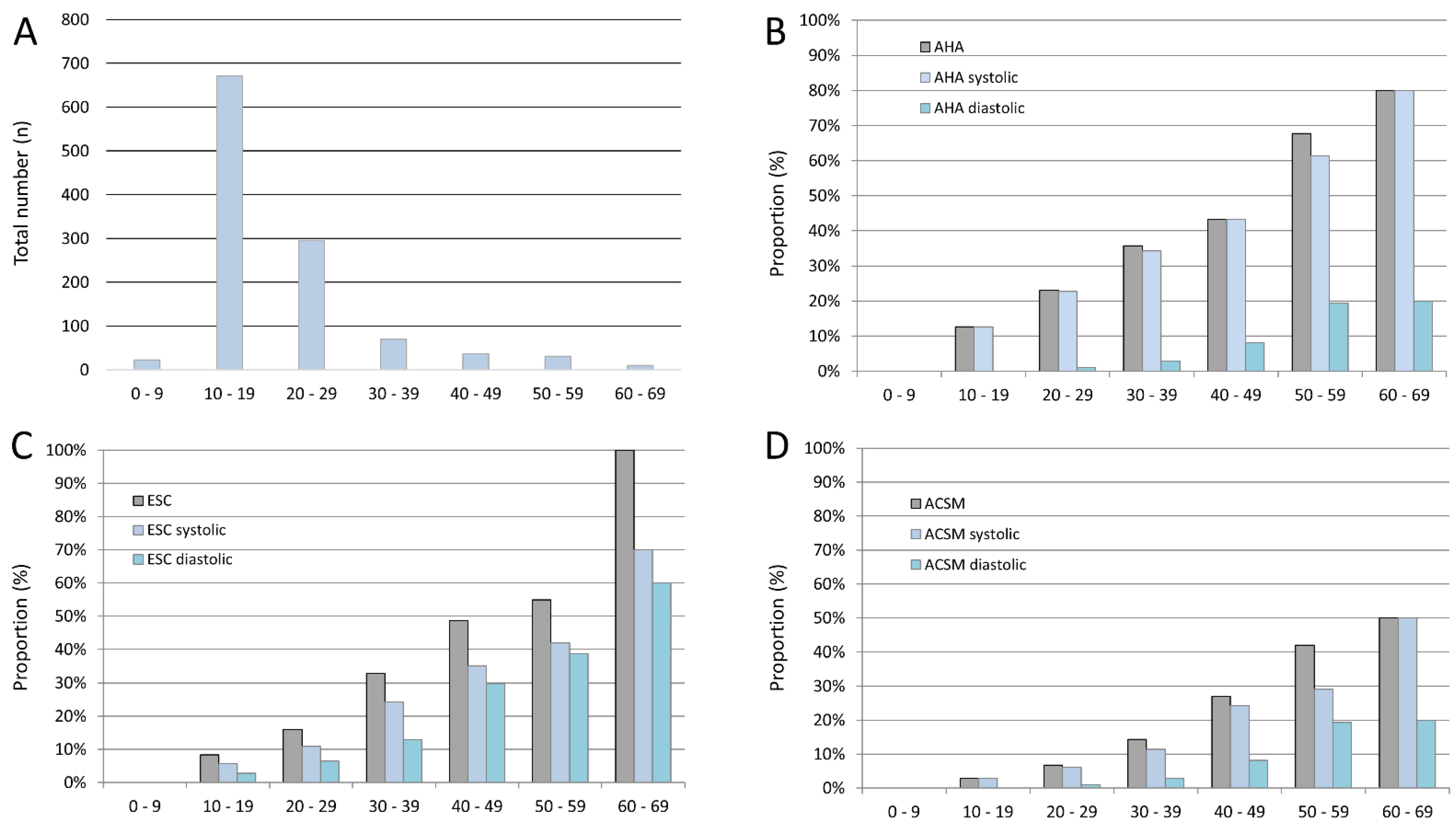
3.2. Prevalence of Exaggerated Blood Pressure Response (EBPR) during Exercise Testing
3.3. Comparison of Athletes with and without Exaggerated Blood Pressure Response (EBPR) during Exercise Testing
3.4. Prevalence of Left Ventricular Hypertrophy (LVH) in Athletes
3.5. Association of Exaggerated Blood Pressure Response (EBPR) during Exercise Testing and Left Ventricular Hypertrophy (LVH) in Athletes
3.6. Prevalence of Exaggerated Blood Pressure Response (EBPR) during Exercise Testing and Left Ventricular Hypertrophy (LVH) in Adult Athletes
3.7. Association of Exaggerated Blood Pressure Response (EBPR) during Exercise Testing and Left Ventricular Hypertrophy (LVH) in Adult Athletes
3.8. Prevalence of Exaggerated Blood Pressure Response (EBPR) during Exercise Testing Identified by Systolic BP/MET Slope Method with a Cutoff Value > 6.2 mmHg/MET
3.9. Association of Exaggerated Blood Pressure Response (EBPR) during Exercise Testing Identified by Systolic BP/MET Slope Method with a Cutoff Value > 6.2 mmHg/MET and Left Ventricular Hypertrophy (LVH) in Athletes
4. Discussion
- (I)
- EBPR was diagnosed between 6.8% and 19.6% of all athletes in our study according to the different guideline recommendations. Prevalence was highest when categorized according to the ESC guidelines (19.6%) and lowest according to the ACSM guidelines (6.8%).
- (II)
- CVRF, such as nicotine abuse and obesity, were more prevalent in athletes with EBPR.
- (III)
- The proportion of athletes with EBPR increased with inclining age regardless of the chosen definition.
- (IV)
- EBPR was more often diagnosed due to maximum systolic in comparison to maximum diastolic BP values during exercise.
- (V)
- Only the EBPR definition of the AHA guideline was able to predict LVH independently of age and sex in both the overall sample as well as in adult athletes as the only guideline recommended threshold.
- (VI)
- In addition, the recently implemented systolic BP/MET slope method with a cutoff value > 6.2 mmHg/MET to define an EBPR, was able to predict LVH in adult athletes independently of age and sex.
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Mancia, G.; Fagard, R.; Narkiewicz, K.; Redon, J.; Zanchetti, A.; Bohm, M.; Christiaens, T.; Cifkova, R.; De Backer, G.; Dominiczak, A.; et al. 2013 ESH/ESC guidelines for the management of arterial hypertension: The Task Force for the Management of Arterial Hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). Eur. Heart J. 2013, 34, 2159–2219. [Google Scholar] [CrossRef] [PubMed]
- Schmieder, R.E. End organ damage in hypertension. Dtsch. Arztebl. Int. 2010, 107, 866–873. [Google Scholar] [CrossRef] [PubMed]
- Kearney, P.M.; Whelton, M.; Reynolds, K.; Muntner, P.; Whelton, P.K.; He, J. Global burden of hypertension: Analysis of worldwide data. Lancet 2005, 365, 217–223. [Google Scholar] [CrossRef]
- Keller, K.; Stelzer, K.; Ostad, M.A.; Post, F. Impact of exaggerated blood pressure response in normotensive individuals on future hypertension and prognosis: Systematic review according to PRISMA guideline. Adv. Med. Sci. 2017, 62, 317–329. [Google Scholar] [CrossRef]
- Wolf-Maier, K.; Cooper, R.S.; Banegas, J.R.; Giampaoli, S.; Hense, H.W.; Joffres, M.; Kastarinen, M.; Poulter, N.; Primatesta, P.; Rodriguez-Artalejo, F.; et al. Hypertension prevalence and blood pressure levels in 6 European countries, Canada, and the United States. JAMA 2003, 289, 2363–2369. [Google Scholar] [CrossRef]
- Go, A.S.; Mozaffarian, D.; Roger, V.L.; Benjamin, E.J.; Berry, J.D.; Borden, W.B.; Bravata, D.M.; Dai, S.; Ford, E.S.; Fox, C.S.; et al. Heart disease and stroke statistics--2013 update: A report from the American Heart Association. Circulation 2013, 127, e6–e245. [Google Scholar] [CrossRef]
- Sacks, F.M.; Campos, H. Dietary therapy in hypertension. N. Engl. J. Med. 2010, 362, 2102–2112. [Google Scholar] [CrossRef]
- Mahfoud, F.; Himmel, F.; Ukena, C.; Schunkert, H.; Bohm, M.; Weil, J. Treatment strategies for resistant arterial hypertension. Dtsch. Arztebl. Int. 2011, 108, 725–731. [Google Scholar] [CrossRef]
- Mancia, G.; De Backer, G.; Dominiczak, A.; Cifkova, R.; Fagard, R.; Germano, G.; Grassi, G.; Heagerty, A.M.; Kjeldsen, S.E.; Laurent, S.; et al. 2007 ESH-ESC Practice Guidelines for the Management of Arterial Hypertension: ESH-ESC Task Force on the Management of Arterial Hypertension. J. Hypertens. 2007, 25, 1751–1762. [Google Scholar] [CrossRef]
- Moebus, S.; Hanisch, J.; Bramlage, P.; Losch, C.; Hauner, H.; Wasem, J.; Jockel, K.H. Regional differences in the prevalence of the metabolic syndrome in primary care practices in Germany. Dtsch. Arztebl. Int. 2008, 105, 207–213. [Google Scholar] [CrossRef]
- Niebauer, J.; Borjesson, M.; Carre, F.; Caselli, S.; Palatini, P.; Quattrini, F.; Serratosa, L.; Adami, P.E.; Biffi, A.; Pressler, A.; et al. Recommendations for participation in competitive sports of athletes with arterial hypertension: A position statement from the sports cardiology section of the European Association of Preventive Cardiology (EAPC). Eur. Heart J. 2018, 39, 3664–3671. [Google Scholar] [CrossRef]
- Whelton, P.K.; Carey, R.M.; Aronow, W.S.; Casey, D.E., Jr.; Collins, K.J.; Dennison Himmelfarb, C.; DePalma, S.M.; Gidding, S.; Jamerson, K.A.; Jones, D.W.; et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J. Am. Coll. Cardiol. 2018, 71, 2199–2269. [Google Scholar] [CrossRef]
- Cuspidi, C. Is exaggerated exercise blood pressure increase related to masked hypertension? Am. J. Hypertens. 2011, 24, 861. [Google Scholar] [CrossRef]
- Matthews, C.E.; Pate, R.R.; Jackson, K.L.; Ward, D.S.; Macera, C.A.; Kohl, H.W.; Blair, S.N. Exaggerated blood pressure response to dynamic exercise and risk of future hypertension. J. Clin. Epidemiol. 1998, 51, 29–35. [Google Scholar] [CrossRef]
- Williams, B.; Mancia, G.; Spiering, W.; Agabiti Rosei, E.; Azizi, M.; Burnier, M.; Clement, D.L.; Coca, A.; de Simone, G.; Dominiczak, A.; et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension. Eur. Heart J. 2018, 39, 3021–3104. [Google Scholar] [CrossRef]
- Kindermann, W. Arterielle Hypertonie. In Sportkardiologie; Kindermann, W., Dickhuth, H.-H., Niess, A., Röcker, K., Urhausen, A., Eds.; Steinkopf-Verlag: Darmstadt, Germany, 2007; Volume 2, pp. 227–240. [Google Scholar]
- Mancia, G.; De Backer, G.; Dominiczak, A.; Cifkova, R.; Fagard, R.; Germano, G.; Grassi, G.; Heagerty, A.M.; Kjeldsen, S.E.; Laurent, S.; et al. 2007 Guidelines for the management of arterial hypertension: The Task Force for the Management of Arterial Hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). Eur. Heart J. 2007, 28, 1462–1536. [Google Scholar] [CrossRef]
- Le, V.V.; Mitiku, T.; Sungar, G.; Myers, J.; Froelicher, V. The blood pressure response to dynamic exercise testing: A systematic review. Prog. Cardiovasc. Dis. 2008, 51, 135–160. [Google Scholar] [CrossRef]
- Sieira, M.C.; Ricart, A.O.; Estrany, R.S. Blood pressure response to exercise testing. Apunts Med. Esport 2010, 45, 191–200. [Google Scholar]
- Lea & Febiger. American College of Sports Medicine. ACSM’s Guidelines for Exercise Testing and Prescription; Wolters Kluwer: Philadelphia, PA, USA, 1991; Volume 4. [Google Scholar]
- Currie, K.D.; Floras, J.S.; La Gerche, A.; Goodman, J.M. Exercise Blood Pressure Guidelines: Time to Re-evaluate What is Normal and Exaggerated? Sports Med. 2018, 48, 1763–1771. [Google Scholar] [CrossRef]
- Pelliccia, A.; Sharma, S.; Gati, S.; Back, M.; Borjesson, M.; Caselli, S.; Collet, J.P.; Corrado, D.; Drezner, J.A.; Halle, M.; et al. 2020 ESC Guidelines on sports cardiology and exercise in patients with cardiovascular disease. Eur. Heart J. 2021, 42, 17–96. [Google Scholar] [CrossRef]
- Fletcher, G.F.; Ades, P.A.; Kligfield, P.; Arena, R.; Balady, G.J.; Bittner, V.A.; Coke, L.A.; Fleg, J.L.; Forman, D.E.; Gerber, T.C.; et al. Exercise standards for testing and training: A scientific statement from the American Heart Association. Circulation 2013, 128, 873–934. [Google Scholar] [CrossRef]
- Caselli, S.; Serdoz, A.; Mango, F.; Lemme, E.; Vaquer Segui, A.; Milan, A.; Attenhofer Jost, C.; Schmied, C.; Spataro, A.; Pelliccia, A. High blood pressure response to exercise predicts future development of hypertension in young athletes. Eur. Heart J. 2019, 40, 62–68. [Google Scholar] [CrossRef]
- Laukkanen, J.A.; Kurl, S.; Rauramaa, R.; Lakka, T.A.; Venalainen, J.M.; Salonen, J.T. Systolic blood pressure response to exercise testing is related to the risk of acute myocardial infarction in middle-aged men. Eur. J. Prev. Cardiol. 2006, 13, 421–428. [Google Scholar] [CrossRef]
- Laukkanen, J.A.; Rauramaa, R. Systolic blood pressure during exercise testing and the risk of sudden cardiac death. Int. J. Cardiol. 2013, 168, 3046–3047. [Google Scholar] [CrossRef]
- Gupta, M.P.; Polena, S.; Coplan, N.; Panagopoulos, G.; Dhingra, C.; Myers, J.; Froelicher, V. Prognostic significance of systolic blood pressure increases in men during exercise stress testing. Am. J. Cardiol. 2007, 100, 1609–1613. [Google Scholar] [CrossRef]
- Kjeldsen, S.E.; Mundal, R.; Sandvik, L.; Erikssen, G.; Thaulow, E.; Erikssen, J. Supine and exercise systolic blood pressure predict cardiovascular death in middle-aged men. J. Hypertens. 2001, 19, 1343–1348. [Google Scholar] [CrossRef]
- Schultz, M.G.; Otahal, P.; Cleland, V.J.; Blizzard, L.; Marwick, T.H.; Sharman, J.E. Exercise-induced hypertension, cardiovascular events, and mortality in patients undergoing exercise stress testing: A systematic review and meta-analysis. Am. J. Hypertens. 2013, 26, 357–366. [Google Scholar] [CrossRef]
- Allison, T.G.; Cordeiro, M.A.; Miller, T.D.; Daida, H.; Squires, R.W.; Gau, G.T. Prognostic significance of exercise-induced systemic hypertension in healthy subjects. Am. J. Cardiol. 1999, 83, 371–375. [Google Scholar] [CrossRef]
- Kurl, S.; Laukkanen, J.A.; Rauramaa, R.; Lakka, T.A.; Sivenius, J.; Salonen, J.T. Systolic blood pressure response to exercise stress test and risk of stroke. Stroke A J. Cereb. Circ. 2001, 32, 2036–2041. [Google Scholar] [CrossRef]
- Palatini, P. Blood pressure behaviour during physical activity. Sports Med. 1988, 5, 353–374. [Google Scholar] [CrossRef]
- Syme, A.N.; Blanchard, B.E.; Guidry, M.A.; Taylor, A.W.; Vanheest, J.L.; Hasson, S.; Thompson, P.D.; Pescatello, L.S. Peak systolic blood pressure on a graded maximal exercise test and the blood pressure response to an acute bout of submaximal exercise. Am. J. Cardiol. 2006, 98, 938–943. [Google Scholar] [CrossRef]
- Wilson, N.V.; Meyer, B.M. Early prediction of hypertension using exercise blood pressure. Prev. Med. 1981, 10, 62–68. [Google Scholar] [CrossRef]
- Singh, J.P.; Larson, M.G.; Manolio, T.A.; O’Donnell, C.J.; Lauer, M.; Evans, J.C.; Levy, D. Blood pressure response during treadmill testing as a risk factor for new-onset hypertension. The Framingham heart study. Circulation 1999, 99, 1831–1836. [Google Scholar] [CrossRef] [PubMed]
- Smith, R.G.; Rubin, S.A.; Ellestad, M.H. Exercise hypertension: An adverse prognosis? J. Am. Soc. Hypertens. JASH 2009, 3, 366–373. [Google Scholar] [CrossRef] [PubMed]
- Levy, D.; Garrison, R.J.; Savage, D.D.; Kannel, W.B.; Castelli, W.P. Prognostic implications of echocardiographically determined left ventricular mass in the Framingham Heart Study. N. Engl. J. Med. 1990, 322, 1561–1566. [Google Scholar] [CrossRef] [PubMed]
- Okwuosa, T.M.; Soliman, E.Z.; Lopez, F.; Williams, K.A.; Alonso, A.; Ferdinand, K.C. Left ventricular hypertrophy and cardiovascular disease risk prediction and reclassification in blacks and whites: The Atherosclerosis Risk in Communities Study. Am. Heart J. 2015, 169, 155–161. [Google Scholar] [CrossRef] [PubMed]
- Scharhag, J.; Lollgen, H.; Kindermann, W. Competitive sports and the heart: Benefit or risk? Dtsch. Arztebl. Int. 2013, 110, 14–23. [Google Scholar] [CrossRef][Green Version]
- Galderisi, M.; Cardim, N.; D’Andrea, A.; Bruder, O.; Cosyns, B.; Davin, L.; Donal, E.; Edvardsen, T.; Freitas, A.; Habib, G.; et al. The multi-modality cardiac imaging approach to the Athlete’s heart: An expert consensus of the European Association of Cardiovascular Imaging. Eur. Heart J. Cardiovasc. Imaging 2015, 16, 353. [Google Scholar] [CrossRef]
- Marwick, T.H.; Gillebert, T.C.; Aurigemma, G.; Chirinos, J.; Derumeaux, G.; Galderisi, M.; Gottdiener, J.; Haluska, B.; Ofili, E.; Segers, P.; et al. Recommendations on the use of echocardiography in adult hypertension: A report from the European Association of Cardiovascular Imaging (EACVI) and the American Society of Echocardiography (ASE). Eur. Heart J. Cardiovasc. Imaging 2015, 16, 577–605. [Google Scholar] [CrossRef]
- Williams, B.; Mancia, G.; Spiering, W.; Agabiti Rosei, E.; Azizi, M.; Burnier, M.; Clement, D.L.; Coca, A.; de Simone, G.; Dominiczak, A.; et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension: The Task Force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension: The Task Force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension. J. Hypertens. 2018, 36, 1953–2041. [Google Scholar] [CrossRef]
- Lang, R.M.; Badano, L.P.; Mor-Avi, V.; Afilalo, J.; Armstrong, A.; Ernande, L.; Flachskampf, F.A.; Foster, E.; Goldstein, S.A.; Kuznetsova, T.; et al. Recommendations for cardiac chamber quantification by echocardiography in adults: An update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J. Am. Soc. Echocardiogr. 2015, 28, 1–39.e14. [Google Scholar] [CrossRef]
- Bauer, P.; Kraushaar, L.; Hoelscher, S.; Weber, R.; Akdogan, E.; Keranov, S.; Dorr, O.; Nef, H.; Hamm, C.W.; Most, A. Blood Pressure Response and Vascular Function of Professional Athletes and Controls. Sports Med. Int. Open 2021, 5, E45–E52. [Google Scholar] [CrossRef]
- Bauer, P.; Kraushaar, L.; Dorr, O.; Nef, H.; Hamm, C.W.; Most, A. Workload-indexed blood pressure response to a maximum exercise test among professional indoor athletes. Eur. J. Prev. Cardiol. 2021, 28, 1487–1494. [Google Scholar] [CrossRef]
- Hedman, K.; Cauwenberghs, N.; Christle, J.W.; Kuznetsova, T.; Haddad, F.; Myers, J. Workload-indexed blood pressure response is superior to peak systolic blood pressure in predicting all-cause mortality. Eur. J. Prev. Cardiol. 2020, 27, 978–987. [Google Scholar] [CrossRef]
- Hedman, K.; Lindow, T.; Elmberg, V.; Brudin, L.; Ekstrom, M. Age- and gender-specific upper limits and reference equations for workload-indexed systolic blood pressure response during bicycle ergometry. Eur. J. Prev. Cardiol. 2021, 28, 1360–1369. [Google Scholar] [CrossRef]
- ACSM’s Guidelines for Exercise Testing: American College of Sports Medicine; Wolters Kluwer: Philadelphia, PA, USA, 2010.
- MacMahon, S.; Peto, R.; Cutler, J.; Collins, R.; Sorlie, P.; Neaton, J.; Abbott, R.; Godwin, J.; Dyer, A.; Stamler, J. Blood pressure, stroke, and coronary heart disease. Part 1, Prolonged differences in blood pressure: Prospective observational studies corrected for the regression dilution bias. Lancet 1990, 335, 765–774. [Google Scholar] [CrossRef]
- Lewington, S.; Clarke, R.; Qizilbash, N.; Peto, R.; Collins, R. Age-specific relevance of usual blood pressure to vascular mortality: A meta-analysis of individual data for one million adults in 61 prospective studies. Lancet 2002, 360, 1903–1913. [Google Scholar]
- Middeke, M. Antihypertensive drug therapy: Where do we stand? Der. Internist. 2015, 56, 230–239. [Google Scholar] [CrossRef]
- Rocchini, A.P.; Key, J.; Bondie, D.; Chico, R.; Moorehead, C.; Katch, V.; Martin, M. The effect of weight loss on the sensitivity of blood pressure to sodium in obese adolescents. N. Engl. J. Med. 1989, 321, 580–585. [Google Scholar] [CrossRef]
- Heymsfield, S.B.; Wadden, T.A. Mechanisms, Pathophysiology, and Management of Obesity. N. Engl. J. Med. 2017, 376, 254–266. [Google Scholar] [CrossRef]
- Carter, B.D.; Abnet, C.C.; Feskanich, D.; Freedman, N.D.; Hartge, P.; Lewis, C.E.; Ockene, J.K.; Prentice, R.L.; Speizer, F.E.; Thun, M.J.; et al. Smoking and mortality--beyond established causes. N. Engl. J. Med. 2015, 372, 631–640. [Google Scholar] [CrossRef] [PubMed]
- Bowman, T.S.; Gaziano, J.M.; Buring, J.E.; Sesso, H.D. A prospective study of cigarette smoking and risk of incident hypertension in women. J. Am. Coll. Cardiol. 2007, 50, 2085–2092. [Google Scholar] [CrossRef] [PubMed]
- Whelton, P.K. Epidemiology of hypertension. Lancet 1994, 344, 101–106. [Google Scholar] [CrossRef]
- Jackson, L.V.; Thalange, N.K.; Cole, T.J. Blood pressure centiles for Great Britain. Arch. Dis. Child. 2007, 92, 298–303. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.; Rajadurai, V.S.; Tan, K.W. Blood pressure standards for very low birthweight infants during the first day of life. Arch. Dis. Child. Fetal Neonatal Ed. 1999, 81, F168–F170. [Google Scholar] [CrossRef] [PubMed]
- Hajjar, I.; Kotchen, T.A. Trends in prevalence, awareness, treatment, and control of hypertension in the United States, 1988-2000. JAMA J. Am. Med. Assoc. 2003, 290, 199–206. [Google Scholar] [CrossRef] [PubMed]
- Jordan, J. Pathophysiology of hypertension: What are our current concepts? Der. Internist. 2015, 56, 219–223. [Google Scholar] [CrossRef] [PubMed]
- Balady, G.J.; Arena, R.; Sietsema, K.; Myers, J.; Coke, L.; Fletcher, G.F.; Forman, D.; Franklin, B.; Guazzi, M.; Gulati, M.; et al. Clinician’s Guide to cardiopulmonary exercise testing in adults: A scientific statement from the American Heart Association. Circulation 2010, 122, 191–225. [Google Scholar] [CrossRef]
- Schultz, M.G.; Sharman, J.E. Exercise Hypertension. Pulse 2014, 1, 161–176. [Google Scholar] [CrossRef]
- Gibbons, R.J.; Balady, G.J.; Bricker, J.T.; Chaitman, B.R.; Fletcher, G.F.; Froelicher, V.F.; Mark, D.B.; McCallister, B.D.; Mooss, A.N.; O’Reilly, M.G.; et al. ACC/AHA 2002 guideline update for exercise testing: Summary article. A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee to Update the 1997 Exercise Testing Guidelines). J. Am. Coll. Cardiol. 2002, 40, 1531–1540. [Google Scholar] [CrossRef]
- Löllgen, H.; Gerke, R. Belastungs-EKG (Ergometrie). Herzschr. Elektrophys. 2008, 19, 98–106. [Google Scholar] [CrossRef]
- Bauer, P.; Kraushaar, L.; Dorr, O.; Nef, H.; Hamm, C.W.; Most, A. Sex differences in workload-indexed blood pressure response and vascular function among professional athletes and their utility for clinical exercise testing. Eur. J. Appl. Physiol. 2021, 121, 1859–1869. [Google Scholar] [CrossRef]
- Reckelhoff, J.F. Gender differences in the regulation of blood pressure. Hypertension 2001, 37, 1199–1208. [Google Scholar] [CrossRef]
- Gleim, G.W.; Stachenfeld, N.S.; Coplan, N.L.; Nicholas, J.A. Gender differences in the systolic blood pressure response to exercise. Am. Heart J. 1991, 121, 524–530. [Google Scholar] [CrossRef]

| Parameters | Normal Blood Pressure Response According to AHA Classification (n = 914; 80.4%) | Exaggerated Blood Pressure Response According to AHA Classification (n = 223; 19.6%) | p-Value |
|---|---|---|---|
| Age (in years) | 17.0 (15.0/22.0) | 22.0 (18.0/33.0) | <0.001 |
| Female sex | 321 (35.1%) | 74 (33.2%) | 0.586 |
| Body height (cm) | 174.0 (166.9/181.0) | 179.0 (173.0/184.0) | <0.001 |
| Body weight (kg) | 67.0 (57.6/77.7) | 75.8 (68.0/85.8) | <0.001 |
| Body mass index (kg/m2) | 22.0 (20.2/24.1) | 23.4 (22.0/25.4) | <0.001 |
| Body fat (%) | 11.3 (8.5/16.4) | 11.9 (9.0/16.3) | 0.140 |
| Leading athletes at a regional or national level | 707 (77.4%) | 146 (65.5%) | <0.001 |
| Training years | 8.0 (5.0/11.0) | 11.0 (6.0/15.0) | <0.001 |
| Cardiovascular risk factors | |||
| Nicotine abuse | 20 (2.2%) | 14 (6.3%) | 0.003 |
| Obesity | 8 (0.9%) | 6 (2.7%) | 0.039 |
| Blood pressure values | |||
| Systolic blood pressure (mmHg) | 115.0 (110.0/120.0) | 120.0 (115.0/130.0) | <0.001 |
| Diastolic blood pressure (mmHg) | 70.0 (60.0/75.0) | 70.0 (70.0/80.0) | <0.001 |
| Maximum systolic blood pressure during exercise (mmHg) | 180.0 (160.0/190.0) | 220.0 (210.0/230.0) | <0.001 |
| Maximum diastolic blood pressure during exercise (mmHg) | 70.0 (70.0/80.0) | 80.0 (70.0/85.0) | <0.001 |
| Exercise parameters | |||
| VO2 maximum during exercise | 45.5 (39.9/50.5) | 44.0 (37.2/49.5) | 0.031 |
| Respiratory exchange ratio (RER) | 1.15 (1.10/1.20) | 1.15 (1.11/1.21) | 0.864 |
| Maximum lactate value | 9.46 (7.79/11.2) | 9.21 (7.61/11.24) | 0.861 |
| Echocardiographic parameters | |||
| Left ventricular hypertrophy | 151 (16.5%) | 82 (36.8%) | <0.001 |
| Left ventricular mass | 158.8 (128.0/200.4) | 194.2 (164.1/220.8) | <0.001 |
| Aortic valve regurgitation | 48 (5.3%) | 26 (11.7%) | 0.001 |
| Mitral valve regurgitation | 474 (51.9%) | 153 (68.6%) | <0.001 |
| Tricuspid valve regurgitation | 115 (12.6%) | 43 (19.3%) | 0.027 |
| Pulmonary valve regurgitation | 91 (10.0%) | 17 (7.6%) | 0.311 |
| Heart volume in total (mL) | 760.5 (625.8/906.3) | 910.3 (770.2/1004.5) | <0.001 |
| Heart volume related to body weight (mL/kg) | 11.4 (10.2/12.4) | 11.7 (10.6/12.8) | 0.003 |
| Left ventricular ejection fraction (%) | 65.0 (62.0/69.0) | 66.0 (62.0/69.0) | 0.140 |
| Left ventricular end-diastolic diameter (cm) | 49.0 (45.0/53.0) | 51.0 (48.0/54.0) | <0.001 |
| Left atrial area (cm2) | 13.5 (11.1/15.4) | 15.2 (12.9/17.6) | <0.001 |
| Right atrial area (cm2) | 13.2 (11.0/15.5) | 15.1 (13.3/17.7) | <0.001 |
| Tricuspid annular plane systolic excursion (TAPSE, cm) | 2.46 (2.20/2.70) | 2.6 (2.3/2.9) | <0.001 |
| Systolic pulmonary artery pulmonary pressure (mmHg) | 20.0 (17.0/23.0) | 20.3 (17.0/23.6) | 0.274 |
| E/A quotient | 2.7 (1.9/3.7) | 2.6 (1.8/3.6) | 0.215 |
| E/E’ quotient | 4.7 (4.0/5.7) | 4.8 (4.0/5.7) | 0.606 |
| Parameters | Normal Blood Pressure Response According to ESC Classification (n = 966; 85.0%) | Exaggerated Blood Pressure Response According to ESC Classification (n = 171; 15.0%) | p-Value |
|---|---|---|---|
| Age (in years) | 17.0 (15.0/22.0) | 26.0 (18.0/42.0) | <0.001 |
| Female sex | 329 (34.1%) | 66 (38.6%) | 0.251 |
| Body height (cm) | 175.0 (167.0/182.0) | 179.0 (171.0/184.0) | <0.001 |
| Body weight (kg) | 68.2 (58.3/78.5) | 75.8 (66.4/84.0) | <0.001 |
| Body mass index (kg/m2) | 22.1 (20.2/24.2) | 23.7 (22.3/25.5) | <0.001 |
| Body fat (%) | 11.0 (8.5/16.0) | 13.0 (9.5/17.2) | <0.001 |
| Leading athletes at a regional or national level | 754 (78.1%) | 99 (57.9%) | <0.001 |
| Training years | 8.0 (5.0/11.0) | 11.0 (7.0/16.0) | <0.001 |
| Cardiovascular risk factors | |||
| Nicotine abuse | 19 (2.0%) | 15 (8.8%) | <0.001 |
| Obesity | 8 (0.8%) | 6 (3.5%) | 0.011 |
| Blood pressure values | |||
| Systolic blood pressure (mmHg) | 115.0 (110.0/120.0) | 120.0 (110.0/130.0) | <0.001 |
| Diastolic blood pressure (mmHg) | 70.0 (60.0/75.0) | 75.0 (70.0/80.0) | <0.001 |
| Maximum systolic blood pressure during exercise (mmHg) | 180.0 (160.0/195.0) | 220.0 (210.0/230.0) | <0.001 |
| Maximum diastolic blood pressure during exercise (mmHg) | 70.0 (70.0/80.0) | 85.0 (80.0/90.0) | <0.001 |
| Exercise parameters | |||
| VO2 maximum during exercise | 45.6 (40.1/50.6) | 42.0 (35.1/49.1) | <0.001 |
| Respiratory exchange ratio (RER) | 1.15 (1.10/1.20) | 1.15 (1.11/1.21) | 0.497 |
| Maximum lactate value | 9.42 (7.71/11.2) | 9.28 (7.96/11.07) | 0.933 |
| Echocardiographic parameters | |||
| Left ventricular hypertrophy | 177 (18.3%) | 56 (32.7%) | <0.001 |
| Left ventricular mass | 164.3 (132.6/200.8) | 188.0 (153.2/219.7) | <0.001 |
| Aortic valve regurgitation | 50 (5.2%) | 24 (14.0%) | <0.001 |
| Mitral valve regurgitation | 506 (52.4%) | 121 (70.8%) | <0.001 |
| Tricuspid valve regurgitation | 123 (12.7%) | 35 (20.5%) | 0.022 |
| Pulmonary valve regurgitation | 94 (9.7%) | 14 (8.2%) | 0.526 |
| Heart volume in total (mL) | 774.4 (634.6/919.0) | 883.0 (728.4/982.6) | <0.001 |
| Heart volume related to body weight (mL/kg) | 11.5 (10.3/12.5) | 11.5 (10.3/12.5) | 0.790 |
| Left ventricular ejection fraction (%) | 65.0 (62.0/68.0) | 66.0 (63.0/69.0) | 0.012 |
| Left ventricular end-diastolic diameter (cm) | 50.0 (46.0/53.0) | 51.0 (47.0/54.0) | 0.004 |
| Left atrial area (cm2) | 13.6 (11.3/15.6) | 15.0 (12.6/15.6) | <0.001 |
| Right atrial area (cm2) | 13.4 (11.1/15.7) | 15.0 (12.9/17.7) | <0.001 |
| Tricuspid annular plane systolic excursion (TAPSE, cm) | 2.50 (2.20/2.80) | 2.6 (2.4/2.9) | <0.001 |
| Systolic pulmonary artery pulmonary pressure (mmHg) | 20.0 (17.0/23.0) | 21.0 (18.0/24.1) | 0.018 |
| E/A quotient | 2.7 (2.0/3.7) | 2.2 (1.6/3.3) | <0.001 |
| E/E’ quotient | 4.7 (4.0/5.7) | 4.9 (4.1/6.0) | 0.167 |
| Parameters | Normal Blood Pressure Response According to ACSM Classification (n = 1060; 93.2%) | Exaggerated Blood Pressure Response According to ACSM Classification (n = 77; 6.8%) | p-Value |
|---|---|---|---|
| Age (in years) | 18.0 (15.0/23.0) | 29.0 (19.5/48.5) | <0.001 |
| Female sex | 384 (36.2%) | 11 (14.3%) | <0.001 |
| Body height (cm) | 175.0 (167.0/182.0) | 181.0 (175.3/186.5) | <0.001 |
| Body weight (kg) | 68.4 (58.8/78.5) | 80.3 (75.0/87.9) | <0.001 |
| Body mass index (kg/m2) | 22.2 (20.4/24.2) | 24.4 (23.0/26.3) | <0.001 |
| Body fat (%) | 11.3 (8.6/16.7) | 11.5 (9.2/14.0) | 0.884 |
| Leading athletes at a regional or national level | 817 (77.1%) | 36 (46.8%) | <0.001 |
| Training years | 8.0 (5.0/11.0) | 13.0 (8.5/18.8) | <0.001 |
| Cardiovascular risk factors | |||
| Nicotine abuse | 27 (2.5%) | 7 (9.1%) | 0.006 |
| Obesity | 10 (0.9%) | 4 (5.2%) | 0.012 |
| Blood pressure values | |||
| Systolic blood pressure (mmHg) | 115.0 (110.0/120.0) | 125.0 (120.0/135.0) | <0.001 |
| Diastolic blood pressure (mmHg) | 70.0 (60.0/75.0) | 80.0 (70.0/80.0) | <0.001 |
| Maximum systolic blood pressure during exercise (mmHg) | 180.0 (160.0/200.0) | 230.0 (230.0/240.0) | <0.001 |
| Maximum diastolic blood pressure during exercise (mmHg) | 75.0 (70.0/80.0) | 80.0 (80.0/90.0) | <0.001 |
| Exercise parameters | |||
| VO2 maximum during exercise | 45.4 (39.8/50.4) | 43.2 (35.8/49.5) | 0.040 |
| Respiratory exchange ratio (RER) | 1.15 (1.11/1.20) | 1.15 (1.11/1.21) | 0.515 |
| Maximum lactate value | 9.40 (7.75/11.21) | 9.41 (7.85/11.16) | 0.974 |
| Echocardiographic parameters | |||
| Left ventricular hypertrophy | 203 (19.2%) | 30 (39.0%) | <0.001 |
| Left ventricular mass | 164.3 (132.8/200.8) | 207.1 (181.4/227.7) | <0.001 |
| Aortic valve regurgitation | 60 (5.7%) | 14 (18.2%) | <0.001 |
| Mitral valve regurgitation | 571 (53.9%) | 56 (72.7%) | 0.001 |
| Tricuspid valve regurgitation | 141 (13.3%) | 17 (22.1%) | 0.090 |
| Pulmonary valve regurgitation | 101 (9.5%) | 7 (9.1%) | 1.000 |
| Heart volume in total (mL) | 774.6 (642.5/919.0) | 965.4 (829.4/1047.0) | <0.001 |
| Heart volume related to body weight (mL/kg) | 11.5 (10.3/12.5) | 11.7 (10.4/12.6) | 0.350 |
| Left ventricular ejection fraction (%) | 65.0 (62.0/69.0) | 66.0 (62.0/72.0) | 0.037 |
| Left ventricular end-diastolic diameter (cm) | 49.0 (46.0/53.0) | 52.0 (49.5/54.5) | <0.001 |
| Left atrial area (cm2) | 13.6 (11.4/15.7) | 15.7 (14.4/18.2) | <0.001 |
| Right atrial area (cm2) | 13.5 (11.2/15.8) | 16.5 (14.0/18.5) | <0.001 |
| Tricuspid annular plane systolic excursion (TAPSE, cm) | 2.50 (2.20/2.80) | 2.6 (2.3/2.9) | 0.001 |
| Systolic pulmonary artery pulmonary pressure (mmHg) | 20.0 (17.0/23.0) | 22.0 (20.0/25.0) | <0.001 |
| E/A quotient | 2.7 (1.9/3.7) | 2.1 (1.5/3.2) | <0.001 |
| E/E’ quotient | 4.7 (4.0/5.7) | 5.1 (4.1/6.4) | 0.080 |
| Left Ventricular Hypertrophy | ||||
|---|---|---|---|---|
| Univariate Regression Model | Multivariate Regression Model (Adjusted for Age and Sex) | |||
| OR (95% CI) | p-Value | OR (95% CI) | p-Value | |
| AHA guideline classification of exaggerated blood pressure response | 2.939 (2.127–4.060) | <0.001 | 2.351 (1.660–3.328) | <0.001 |
| ESC guideline classification of exaggerated blood pressure response | 2.171 (1.517–3.107) | <0.001 | 1.493 (0.998–2.232) | 0.051 |
| ACSM guideline classification of exaggerated blood pressure response | 2.695 (1.663–4.367) | <0.001 | 1.805 (1.054–3.093) | 0.031 |
| Systolic blood pressure/MET slope (>6.2 mmHg/MET) | 2.120 (1.449–3.101) | <0.001 | 2.257 (0.403–12.655) | 0.355 |
| Systolic blood pressure at rest (mmHg) | 1.023 (1.010–1.036) | <0.001 | 1.016 (1.001–1.030) | 0.033 |
| Diastolic blood pressure at rest (mmHg) | 1.025 (1.007–1.043) | 0.005 | 1.011 (0.992–1.030) | 0.253 |
| Maximum systolic blood pressure during exercise (mmHg) | 1.024 (1.018–1.030) | <0.001 | 1.026 (1.019–1.033) | <0.001 |
| Maximum diastolic blood pressure during exercise (mmHg) | 1.023 (1.007–1.040) | 0.005 | 1.006 (0.989–1.024) | 0.470 |
| Parameters | Normal Blood Pressure Response According to Systolic Blood Pressure/MET Slope (≤6.2 mmHg/MET) (n = 386; 60.4%) | Exaggerated Blood Pressure Response According to Systolic Blood Pressure/MET Slope (>6.2 mmHg/MET) (n = 253; 39.6%) | p-Value |
|---|---|---|---|
| Age (in years) | 18.0 (15.0/22.0) | 24.0 (18.0/36.5) | <0.001 |
| Female sex | 139 (36.0%) | 80 (31.6%) | 0.253 |
| Body height (cm) | 175.0 (168.0/182.0) | 178.0 (170.0/184.0) | 0.014 |
| Body weight (kg) | 66.8 (58.0/77.7) | 76.0 (66.0/85.9) | <0.001 |
| Body mass index (kg/m2) | 21.7 (20.2/24.0) | 23.8 (22.3/26.0) | <0.001 |
| Body fat (%) | 12.4 (8.2/16.6) | 12.2 (9.2/17.1) | 0.003 |
| Leading athletes at a regional or national level | 295 (76.4%) | 135 (53.4%) | <0.001 |
| Training years | 7.0 (5.0/10.0) | 10.0 (5.0/14.0) | <0.001 |
| Cardiovascular risk factors | |||
| Nicotine abuse | 8 (2.1%) | 18 (7.1%) | 0.003 |
| Obesity | 1 (0.3%) | 9 (3.6%) | 0.001 |
| Blood pressure values | |||
| Systolic blood pressure (mmHg) | 120.0 (110.0/125.0) | 120.0 (110.0/125.0) | 0.908 |
| Diastolic blood pressure (mmHg) | 70.0 (60.0/75.0) | 70.0 (65.0/80.0) | 0.003 |
| Maximum systolic blood pressure during exercise (mmHg) | 170.0 (155.0/180.0) | 210.0 (190.0/220.0) | <0.001 |
| Maximum diastolic blood pressure during exercise (mmHg) | 70.0 (65.0/80.0) | 80.0 (70.0/80.0) | <0.001 |
| Exercise parameters | |||
| VO2 maximum during exercise | 47.5 (42.1/51.5) | 41.9 (36.2/47.0) | <0.001 |
| Respiratory exchange ratio (RER) | 1.15 (1.10/1.19) | 1.15 (1.11/1.21) | 0.037 |
| Maximum lactate value | 9.36 (7.67/11.24) | 9.51 (7.89/11.24) | 0.533 |
| Echocardiographic parameters | |||
| Left ventricular hypertrophy | 64 (16.6%) | 75 (29.6%) | <0.001 |
| Left ventricular mass | 163.6 (132.3/199.3) | 188.1 (153.4/220.6) | <0.001 |
| Aortic valve regurgitation | 20 (5.2%) | 22 (8.7%) | 0.080 |
| Mitral valve regurgitation | 203 (52.6%) | 169 (66.8%) | <0.001 |
| Tricuspid valve regurgitation | 46 (12.0%) | 51 (20.2%) | 0.010 |
| Pulmonary valve regurgitation | 34 (8.8%) | 25 (9.9%) | 0.647 |
| Heart volume in total (mL) | 772.0 (639.0/908.5) | 896.4 (732.9/1000.0) | <0.001 |
| Heart volume related to body weight (mL/kg) | 11.4 (10.2/12.4) | 11.4 (10.2/12.3) | 0.803 |
| Left ventricular ejection fraction (%) | 65.0 (62.0/69.0) | 66.0 (63.0/69.0) | 0.041 |
| Left ventricular end-diastolic diameter (cm) | 50.0 (46.0/53.0) | 51.0 (47.0/54.0) | <0.001 |
| Left atrial area (cm2) | 13.5 (11.0/15.3) | 14.9 (12.6/17.4) | <0.001 |
| Right atrial area (cm2) | 13.3 (11.1/15.5) | 14.9 (12.8/17.9) | <0.001 |
| Tricuspid annular plane systolic excursion (TAPSE, cm) | 2.40 (2.20/2.70) | 2.60 (2.40/2.90) | <0.001 |
| Systolic pulmonary artery pulmonary pressure (mmHg) | 20.0 (16.5/23.0) | 21.5 (18.0/24.0) | 0.002 |
| E/A quotient | 2.5 (1.9/3.4) | 2.4 (1.6/3.6) | 0.111 |
| E/E’ quotient | 4.7 (4.0/5.7) | 4.9 (4.1/5.9) | 0.193 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Keller, K.; Hartung, K.; del Castillo Carillo, L.; Treiber, J.; Stock, F.; Schröder, C.; Hugenschmidt, F.; Friedmann-Bette, B. Exercise Hypertension in Athletes. J. Clin. Med. 2022, 11, 4870. https://doi.org/10.3390/jcm11164870
Keller K, Hartung K, del Castillo Carillo L, Treiber J, Stock F, Schröder C, Hugenschmidt F, Friedmann-Bette B. Exercise Hypertension in Athletes. Journal of Clinical Medicine. 2022; 11(16):4870. https://doi.org/10.3390/jcm11164870
Chicago/Turabian StyleKeller, Karsten, Katharina Hartung, Luis del Castillo Carillo, Julia Treiber, Florian Stock, Chantal Schröder, Florian Hugenschmidt, and Birgit Friedmann-Bette. 2022. "Exercise Hypertension in Athletes" Journal of Clinical Medicine 11, no. 16: 4870. https://doi.org/10.3390/jcm11164870
APA StyleKeller, K., Hartung, K., del Castillo Carillo, L., Treiber, J., Stock, F., Schröder, C., Hugenschmidt, F., & Friedmann-Bette, B. (2022). Exercise Hypertension in Athletes. Journal of Clinical Medicine, 11(16), 4870. https://doi.org/10.3390/jcm11164870