Comparison of Operative Times in Primary Bilateral Total Knee Arthroplasty Performed by a Single Surgeon
Abstract
:1. Introduction
2. Materials and Methods
2.1. Surgical Procedure
2.2. Statistical Analysis
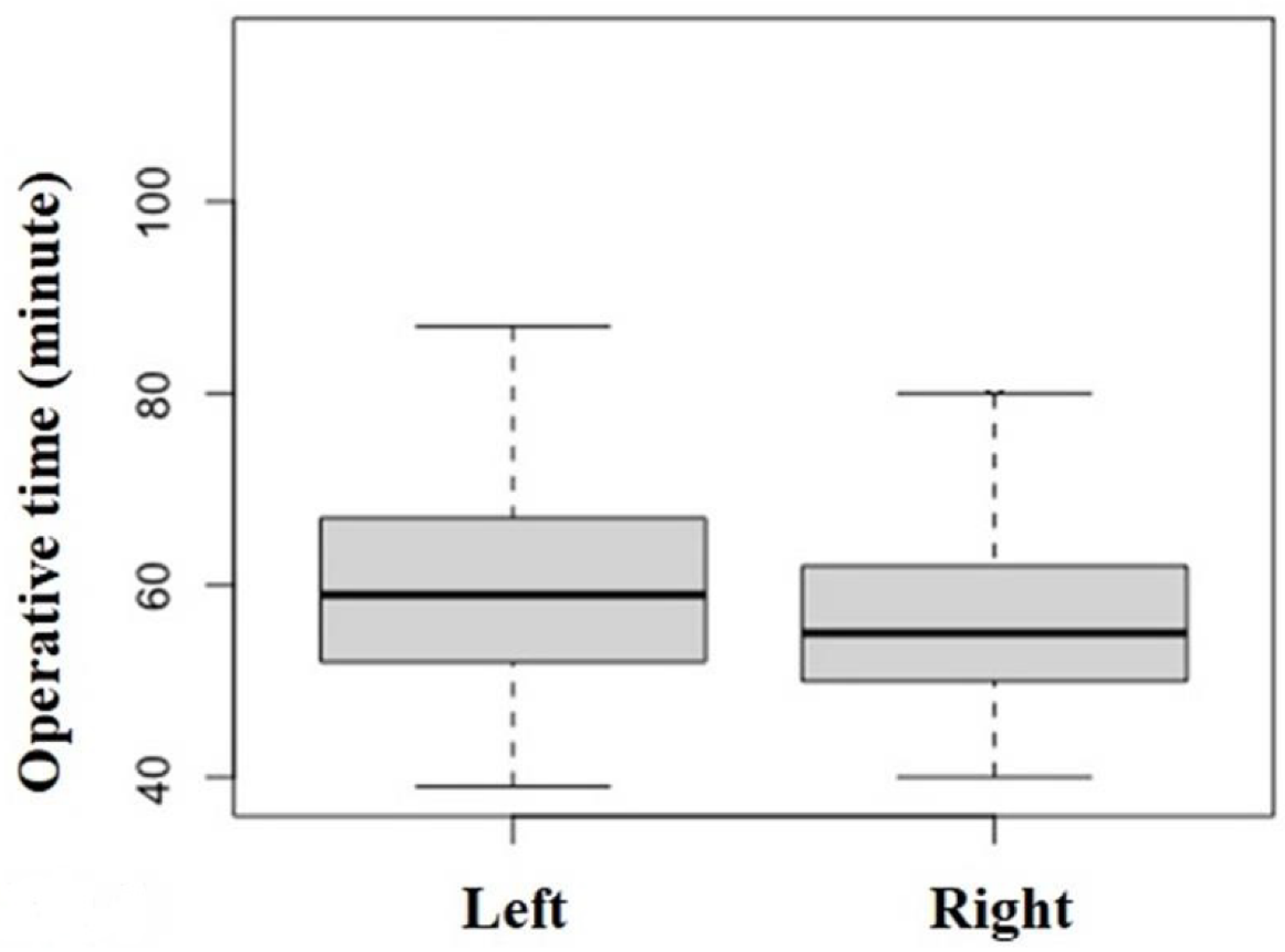
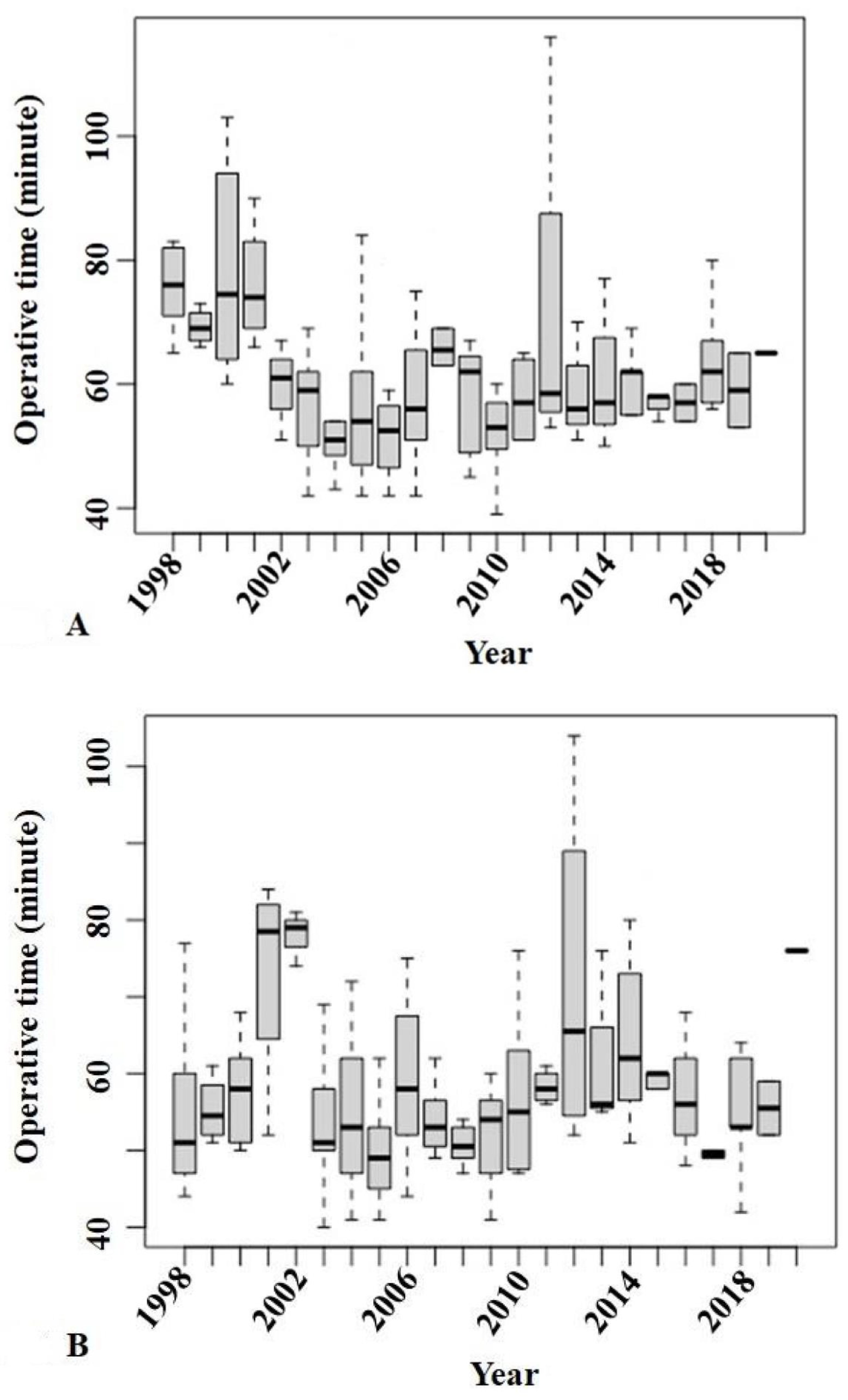
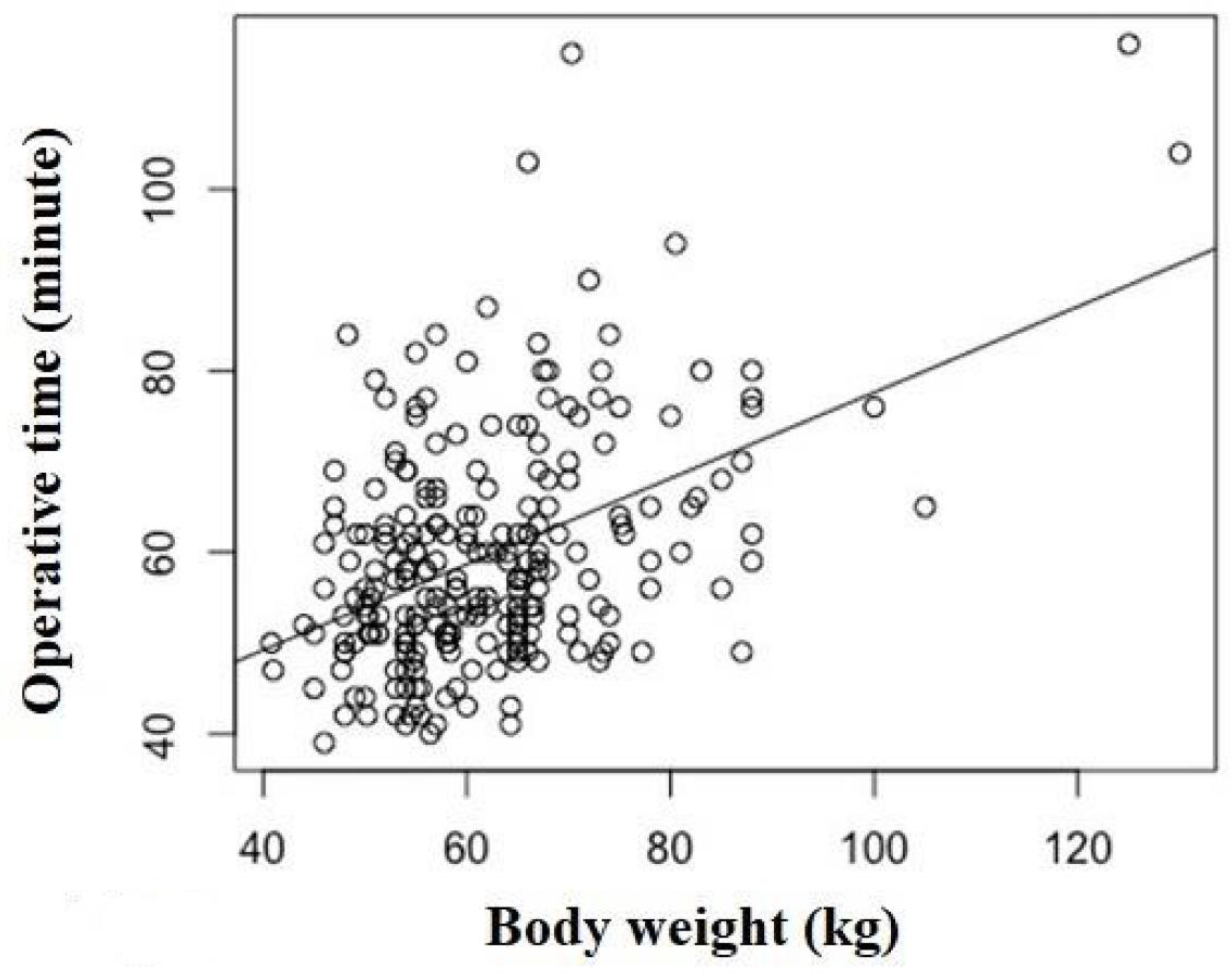
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Badawy, M.; Espehaug, B.; Fenstad, A.M.; Indrekvam, K.; Dale, H.; Havelin, L.I.; Furnes, O. Patient and surgical factors affecting procedure duration and revision risk due to deep infection in primary total knee arthroplasty. BMC Muscoskel. Disord. 2017, 18, 544. [Google Scholar] [CrossRef] [PubMed]
- Namba, R.S.; Inacio, M.C.; Paxton, E.W. Risk factors associated with deep surgical site infections after primary total knee arthroplasty: An analysis of 56,216 knees. J. Bone Jt. Surg. Am. 2013, 95, 775–782. [Google Scholar] [CrossRef] [PubMed]
- Naranje, S.; Lendway, L.; Mehle, S.; Gioe, T.J. Does operative time affect infection rate in primary total knee arthroplasty? Clin. Orthop. Relat. Res. 2015, 473, 64–69. [Google Scholar] [CrossRef] [PubMed]
- Jaffer, A.K.; Barsoum, W.K.; Krebs, V.; Hurbanek, J.G.; Morra, N.; Brotman, D.J. Duration of anesthesia and venous thromboembolism after hip and knee arthroplasty. Mayo Clin. Proc. 2005, 80, 732–738. [Google Scholar] [CrossRef]
- Horlocker, T.T.; Hebl, J.R.; Gali, B.; Jankowski, C.J.; Burkle, C.M.; Berry, D.J.; Zepeda, F.A.; Stevens, S.R.; Schroeder, D.R. Anesthetic, patient, and surgical risk factors for neurologic complications after prolonged total tourniquet time during total knee arthroplasty. Anesth. Analg. 2006, 102, 950–955. [Google Scholar] [CrossRef]
- Morcos, M.W.; Nowak, L.; Schemitsch, E. Prolonged surgical time increases the odds of complications following total knee arthroplasty. Can. J. Surg. 2021, 64, E273–E279. [Google Scholar] [CrossRef]
- Duchman, K.R.; Pugely, A.J.; Martin, C.T.; Gao, Y.; Bedard, N.A.; Callaghan, J.J. Operative Time Affects Short-Term Complications in Total Joint Arthroplasty. J. Arthroplast. 2017, 32, 1285–1291. [Google Scholar] [CrossRef]
- D’Ambrosi, R.; Menon, P.H.; Salunke, A.; Mariani, I.; Palminteri, G.; Basile, G.; Ursino, N.; Mangiavini, L.; Hantes, M. Octogenarians Are the New Sexagenarians: Cruciate-Retaining Total Knee Arthroplasty Is Not Inferior to Posterior-Stabilized Arthroplasty in Octogenarian Patients. J. Clin. Med. 2022, 11, 3795. [Google Scholar] [CrossRef]
- Yi, S.; Tan, J.; Chen, C.; Chen, H.; Huang, W. The use of pneumatic tourniquet in total knee arthroplasty: A meta-analysis. Arch. Orthop. Trauma Surg. 2014, 134, 1469–1476. [Google Scholar] [CrossRef]
- Hamilton, W.G.; Parks, N.L.; Saxena, A. Patient-specific instrumentation does not shorten surgical time: A prospective, randomized trial. J. Arthroplast. 2013, 28 (Suppl. S8), 96–100. [Google Scholar] [CrossRef]
- King, J.; Stamper, D.L.; Schaad, D.C.; Leopold, S.S. Minimally invasive total knee arthroplasty compared with traditional total knee arthroplasty. Assessment of the learning curve and the postoperative recuperative period. J. Bone Jt. Surg. Am. 2007, 89, 1497–1503. [Google Scholar] [CrossRef]
- Li, Z.; Cheng, W.; Sun, L.; Yao, Y.; Cao, Q.; Ye, S.; Qi, L.; Xu, S.; Wu, X.; Jing, J. Mini-subvastus versus medial parapatellar approach for total knee arthroplasty: A prospective randomized controlled study. Int. Orthop. 2018, 42, 543–549. [Google Scholar] [CrossRef] [PubMed]
- Kaidi, A.C.; Hammoor, B.T.; Tatka, J.; Neuwirth, A.L.; Levine, W.N.; Hickernell, T.R. Intraoperative scrub nurse handoffs are associated with increased operative times for total joint arthroplasty patients. Arthroplast. Today 2021, 10, 35–40. [Google Scholar] [CrossRef] [PubMed]
- Basques, B.A.; Bell, J.A.; Sershon, R.A.; Della Valle, C.J. The influence of patient gender on morbidity following total hip or total knee arthroplasty. J. Arthroplast. 2018, 33, 345–349. [Google Scholar] [CrossRef] [PubMed]
- Kosashvili, Y.; Mayne, I.P.; Trajkovski, T.; Lackstein, D.; Safir, O.; Backstein, D. Influence of sex on surgical time in primary total knee arthroplasty. Can. J. Surg. 2010, 53, 256–260. [Google Scholar] [PubMed]
- Hanly, R.J.; Marvi, S.K.; Whitehouse, S.L.; Crawford, R.W. Morbid obesity in total knee arthroplasty: Joint-specific variance in outcomes for operative time, length of stay, and readmission. J. Arthroplast. 2017, 32, 2712–2716. [Google Scholar] [CrossRef]
- Ishii, Y.; Noguchi, H.; Sato, J.; Ishii, H.; Ishii, R.; Toyabe, S.I. Predictive factors for longer operative times in patients with medial knee osteoarthritis undergoing total knee arthroplasty. J. Orthop. 2020, 20, 181–185. [Google Scholar] [CrossRef] [PubMed]
- Liabaud, B.; Patrick, D.A., Jr.; Geller, J.A. Higher body mass index leads to longer operative time in total knee arthroplasty. J. Arthroplast. 2013, 28, 563–565. [Google Scholar] [CrossRef]
- Anonymous. American Society of Anaesthesiologists Physical Status Classification System. Available online: http://www.asahq.org/resources/clinical-information/asa-physical-statusclassification-system (accessed on 24 March 2022).
- Alicea, J. Scoring systems and their validation for the arthritic knee. In Surgery of the Knee, 3rd ed.; Insall, J.N., Scott, W.N., Eds.; Churchill Livingstone: New York, NY, USA, 2001; Volume 2, pp. 1507–1515. [Google Scholar]
- Ishii, Y.; Noguchi, H.; Takeda, M.; Sato, J.; Ezawa, N.; Toyabe, S. Changes in lower extremity 3-dimensional load-bearing axes before and after mobile-bearing total knee arthroplasty. J. Arthroplast. 2012, 27, 1203–1209. [Google Scholar] [CrossRef]
- Ishii, Y.; Noguchi, H.; Sato, J.; Ishii, H.; Todoroki, K.; Toyabe, S.I. Association between body weight and proximal tibial bone mineral density after bilateral total knee arthroplasty. Knee 2017, 24, 1153–1159. [Google Scholar] [CrossRef]
- Thiengwittayaporn, S.; Uthaitas, P.; Senwiruch, C.; Hongku, N.; Tunyasuwanakul, R. Imageless robotic-assisted total knee arthroplasty accurately restores the radiological alignment with a short learning curve: A randomized controlled trial. Int. Orthop. 2021, 45, 2851–2858. [Google Scholar] [CrossRef] [PubMed]
- Ishii, Y.; Matsuda, Y.; Sakata, S.; Onda, N.; Omori, G. Primary total knee arthroplasty using the Genesis I total knee prosthesis: A 5- to 10-year follow-up study. Knee 2005, 12, 341–345. [Google Scholar] [CrossRef] [PubMed]
- Matsuda, Y.; Ishii, Y.; Noguchi, H.; Ishii, R. Varus-valgus balance and range of movement after total knee arthroplasty. J. Bone Jt. Surg. Br. 2005, 87, 804–808. [Google Scholar] [CrossRef] [PubMed]
- Ishii, Y.; Noguchi, H.; Sato, J.; Ishii, H.; Takayama, S.; Toyabe, S.I. Life Expectancy of Osteoarthritic Patients after Primary Total Knee Arthroplasty. J. Clin. Orthop. Trauma 2017, 8 (Suppl. 2), S57–S61. [Google Scholar] [CrossRef] [PubMed]
- Slick, G.S.; Davis Iii, C.M.; Elfar, J.C.; Nikkel, L.E. Process mapping total knee arthroplasty: A comparison of instrument designs. J. Arthroplast. 2021, 36, 941–945. [Google Scholar] [CrossRef]
| Patients | Knees | ||
|---|---|---|---|
| Gender M/F | 15/104 | 30/208 | |
| Side R/L | 119/119 | 238/238 | |
| ASA (I/II) [19] | 6/113 | 12/226 | |
| Median | Interquartile Range | Range | |
| Interval (days) | 628 | 315, 1460 | 35–5110 |
| Age (year) | 73 | 69, 77 | 34–88 |
| BH (cm) | 151 | 146, 155 | 135–184 |
| BW (kg) | 59 | 54, 67 | 41–130 |
| BMI (cm/kg2) | 26 | 24, 29 | 19–42 |
| HSS score [20] | 45 | 37, 51 | 19–67 |
| TFA (°) | 181 | 179, 184 | 162–199 |
| B | S.E. | β | Sig. | 95%CI | ||
|---|---|---|---|---|---|---|
| (Constant) | 1025.183 | 255.308 | 0.000 | 522.188 | 1528.179 | |
| Body weight | 0.505 | 0.058 | 0.488 | <0.001 | 0.391 | 0.619 |
| Calendar year of surgery | –0.495 | 0.127 | –0.218 | <0.001 | –0.746 | –0.245 |
| Side of surgery (left; 0, right 1) | –3.815 | 1.407 | –0.151 | 0.007 | –6.586 | –1.044 |
| Variable | r | P |
|---|---|---|
| Sex | 0.188 | 0.004 |
| Age (years) | –0.144 | 0.026 |
| Body Height (cm) | 0.212 | 0.001 |
| Body Weight (kg) | 0.352 | <0.001 |
| Body Mass index (kg/cm2) | 0.290 | <0.001 |
| HSS score [20] | 0.042 | 0.517 |
| Tibiofemoral angle | 0.090 | 0.167 |
| ASA grade [19] | –0.112 | 0.084 |
| Order (1st/2nd) | –0.120 | 0.065 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ishii, Y.; Noguchi, H.; Sato, J.; Takahashi, I.; Ishii, H.; Ishii, R.; Ishii, K.; Toyabe, S.-i. Comparison of Operative Times in Primary Bilateral Total Knee Arthroplasty Performed by a Single Surgeon. J. Clin. Med. 2022, 11, 4867. https://doi.org/10.3390/jcm11164867
Ishii Y, Noguchi H, Sato J, Takahashi I, Ishii H, Ishii R, Ishii K, Toyabe S-i. Comparison of Operative Times in Primary Bilateral Total Knee Arthroplasty Performed by a Single Surgeon. Journal of Clinical Medicine. 2022; 11(16):4867. https://doi.org/10.3390/jcm11164867
Chicago/Turabian StyleIshii, Yoshinori, Hideo Noguchi, Junko Sato, Ikuko Takahashi, Hana Ishii, Ryo Ishii, Kei Ishii, and Shin-ichi Toyabe. 2022. "Comparison of Operative Times in Primary Bilateral Total Knee Arthroplasty Performed by a Single Surgeon" Journal of Clinical Medicine 11, no. 16: 4867. https://doi.org/10.3390/jcm11164867
APA StyleIshii, Y., Noguchi, H., Sato, J., Takahashi, I., Ishii, H., Ishii, R., Ishii, K., & Toyabe, S.-i. (2022). Comparison of Operative Times in Primary Bilateral Total Knee Arthroplasty Performed by a Single Surgeon. Journal of Clinical Medicine, 11(16), 4867. https://doi.org/10.3390/jcm11164867






