The Efficacy of Exercise Training for Cutaneous Microvascular Reactivity in the Foot in People with Diabetes and Obesity: Secondary Analyses from a Randomized Controlled Trial
Abstract
:1. Introduction
2. Materials and Methods
2.1. Design
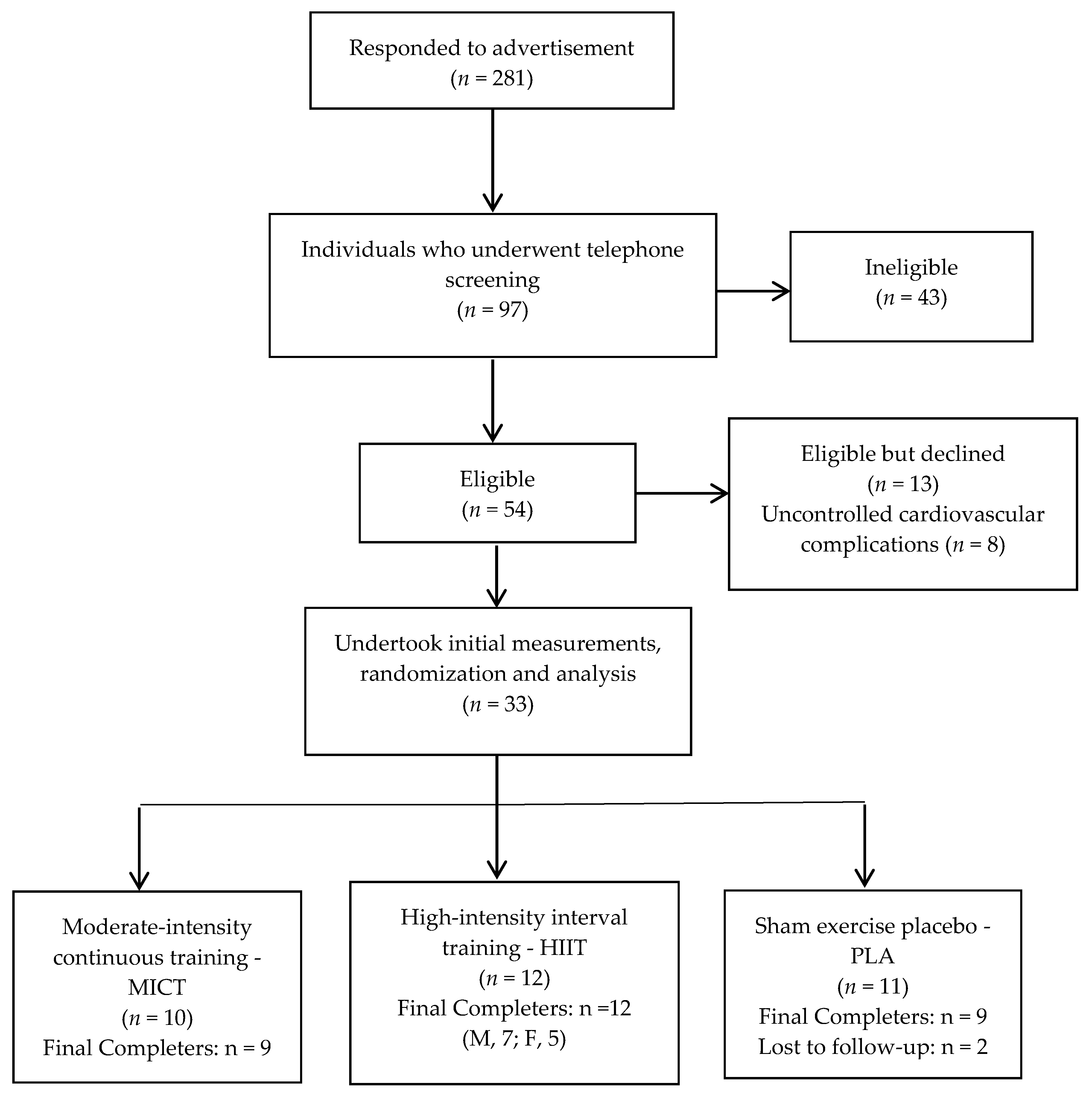
2.2. Participants
2.3. Cutaneous Microvascular Reactivity
2.4. Peripheral Arterial Measures
2.5. Anthropometric Measures, Cardiorespiratory Fitness and Neuropathic Status
2.6. Interventions
2.6.1. High-Intensity, Low-Volume Interval Training (HIIT)
2.6.2. Moderate Intensity Continuous Training (MICT)
2.6.3. Sham-Exercise Placebo (PLA)
2.7. Sample Size
2.8. Statistical Analysis
3. Results
Primary and Secondary Outcomes
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Saeedi, P.; Salpea, P.; Karuranga, S.; Persohn, I.; Malanda, B.; Greg, E.W.; Unwin, N.; Wild, S.H.; Williams, R. Mortality attributable to diabetes in 20–79 years old adults, 2019 estimates: Results from the International Diabetes Federation Diabetes Atlas. Diabetes Res. Clin. Pract. 2020, 162, 108086. [Google Scholar] [CrossRef] [PubMed]
- Driver, V.R.; Fabbi, M.; Lavery, L.A.; Gibbons, G. The costs of diabetic foot: The economic case for the limb salvage team. J. Vasc. Surg. 2010, 52, 17S–22S. [Google Scholar] [CrossRef] [PubMed]
- Sharma, S.; Schaper, N.; Rayman, G. Microangiopathy: Is it relevant to wound healing in diabetic foot disease? Diabetes Metab. Res. 2020, 36, e3244. [Google Scholar] [CrossRef] [PubMed]
- Chao, C.Y.; Cheing, G.L. Microvascular dysfunction in diabetic foot disease and ulceration. Diabetes Metab. Res. 2009, 25, 604–614. [Google Scholar] [CrossRef] [PubMed]
- Van Dam, P.S.; Cotter, M.A.; Bravenboer, B.; Cameron, N.E. Pathogenesis of diabetic neuropathy: Focus on neurovascular mechanisms. Eur. J. Pharmacol. 2013, 719, 180–186. [Google Scholar] [CrossRef] [PubMed]
- Vinik, A.I.; Erbas, T.; Park, T.S.; Pierce, K.K.; Stansberry, K.B. Methods for evaluation of peripheral neurovascular dysfunction. Diabetes Technol. Ther. 2001, 3, 29–50. [Google Scholar] [CrossRef]
- Uccioli, L.; Mancini, L.; Giordano, A.; Solini, A.; Magnani, P.; Manto, A.; Cotroneo, P.; Greco, A.V.; Ghirlanda, G. Lower limb arterio-venous shunts, autonomic neuropathy and diabetic foot. Diabetes Res. Clin. Pract. 1992, 16, 123–130. [Google Scholar] [CrossRef]
- Vinik, A.I.; Maser, R.E.; Mitchell, B.D.; Freeman, R. Diabetic autonomic neuropathy. Diabetes Care 2003, 26, 1553–1579. [Google Scholar] [CrossRef]
- Jonk, A.M.; Houben, A.J.; De Jongh, R.T.; Serné, E.H.; Schaper, N.C.; Stehouwer, C.D. Microvascular dysfunction in obesity: A potential mechanism in the pathogenesis of obesity-associated insulin resistance and hypertension. Physiology 2007, 22, 252–260. [Google Scholar] [CrossRef]
- Candela, J.; Wang, R.; White, C. Microvascular endothelial dysfunction in obesity is driven by macrophage-dependent hydrogen sulfide depletion. Arterioscl. Throm. Vas. 2017, 37, 889–899. [Google Scholar] [CrossRef] [Green Version]
- Flynn, M.; Tooke, J. Aetiology of diabetic foot ulceration: A role for the microcirculation? Diabetic Med. 1992, 9, 320–329. [Google Scholar] [CrossRef]
- Rayman, G.; Williams, S.; Spencer, P.; Smaje, L.; Wise, P.; Tooke, J. Impaired microvascular hyperaemic response to minor skin trauma in type I diabetes. Brit. Med. J. 1986, 292, 1295. [Google Scholar] [CrossRef]
- Lanting, S.M.; Johnson, N.A.; Baker, M.K.; Caterson, I.D.; Chuter, V.H. The effect of exercise training on cutaneous microvascular reactivity: A systematic review and meta-analysis. J. Sci. Med. Sport 2016, 20, 170–177. [Google Scholar] [CrossRef]
- Tew, G.A.; Saxton, J.M.; Hodges, G.J. Exercise training and the control of skin blood flow in older adults. J. Nutr. Health Aging 2012, 16, 237–241. [Google Scholar] [CrossRef]
- Joyner, M.J.; Green, D.J. Exercise protects the cardiovascular system: Effects beyond traditional risk factors. J. Physiol. 2009, 587, 5551–5558. [Google Scholar] [CrossRef]
- Ignarro, L. Nitric oxide as a unique signalling molecule in the vascular system: A historical overview. J. Physiol. Pharmacol. 2002, 53, 503–514. [Google Scholar]
- Colberg, S.R.; Parson, H.K.; Holton, D.R.; Nunnold, T.; Vinik, A.I. Cutaneous blood flow in type 2 diabetic individuals after an acute bout of maximal exercise. Diabetes Care 2003, 26, 1883–1888. [Google Scholar] [CrossRef]
- Colberg, S.R.; Stansberry, K.B.; McNitt, P.M.; Vinik, A.I. Chronic exercise is associated with enhanced cutaneous blood flow in Type 2 diabetes. J. Diabetes Complicat. 2002, 16, 139–145. [Google Scholar] [CrossRef]
- Middlebrooke, A.; Elston, L.; Macleod, K.; Mawson, D.M.; Ball, C.I.; Shore, A.C.; Tooke, J.E. Six months of aerobic exercise does not improve microvascular function in type 2 diabetes mellitus. Diabetologia 2006, 49, 2263–2271. [Google Scholar] [CrossRef]
- Mitranun, W.; Deerochanawong, C.; Tanaka, H.; Suksom, D. Continuous vs interval training on glycemic control and macro- and microvascular reactivity in type 2 diabetic patients. Scand. J. Med. Sci. Sports 2014, 24, e69–e76. [Google Scholar] [CrossRef]
- Egan, A.; Mahmood, W.; Fenton, R.; Redziniak, N.; Kyaw Tun, T.; Sreenan, S.; McDermott, J.H. Barriers to exercise in obese patients with type 2 diabetes. QJM Int. J. Med. 2013, 106, 635–638. [Google Scholar] [CrossRef] [PubMed]
- Weston, K.S.; Wisløff, U.; Coombes, J.S. High-intensity interval training in patients with lifestyle-induced cardiometabolic disease: A systematic review and meta-analysis. Brit. J. Sport Med. 2014, 48, 1227–1234. [Google Scholar] [CrossRef] [PubMed]
- Way, K.L.; Sabag, A.; Sultana, R.N.; Baker, M.K.; Keating, S.E.; Lanting, S.; Gerofi, J.; Chuter, V.H.; Caterson, I.D.; Twigg, S.M.; et al. The effect of low-volume high-intensity interval training on cardiovascular health outcomes in type 2 diabetes: A randomised controlled trial. Int. J. Cardiol. 2020, 320, 148–154. [Google Scholar] [CrossRef] [PubMed]
- Barwick, A.; Lanting, S.; Chuter, V. Intra-tester and inter-tester reliability of post-occlusive reactive hyperaemia measurement at the hallux. Microvasc. Res. 2015, 99, 67–71. [Google Scholar] [CrossRef]
- Aboyans, V.; Criqui, M.H.; Abraham, P.; Allison, M.A.; Creager, M.A.; Diehm, C.; Fowkes, F.G.; Hiatt, W.R.; Jönsson, B.; Lacroix, P.; et al. Measurement and interpretation of the ankle-brachial index: A scientific statement from the American Heart Association. Circulation 2012, 126, 2890–2909. [Google Scholar] [CrossRef]
- Sabag, A.; Way, K.L.; Sultana, R.N.; Keating, S.E.; Gerofi, J.A.; Chuter, V.H.; Byrne, N.M.; Baker, M.K.; George, J.; Caterson, I.D.; et al. The effect of a novel low-volume aerobic exercise intervention on liver fat in type 2 diabetes: A randomized controlled trial. Diabetes Care. 2020, 43, 2371–2378. [Google Scholar] [CrossRef]
- Boulton, A.J.; Armstrong, D.G.; Albert, S.F.; Frykberg, R.G.; Hellman, R.; Kirkman, M.S.; Lavery, L.A.; LeMaster, J.W.; Mills, J.L., Sr.; Mueller, M.J.; et al. Comprehensive foot examination and risk assessment: A report of the task force of the foot care interest group of the American Diabetes Association, with endorsement by the American Association of Clinical Endocrinologists. Diabetes Care 2008, 31, 1679–1685. [Google Scholar] [CrossRef]
- Armijo-Olivo, S.; Warren, S.; Magee, D. Intention to treat analysis, compliance, drop-outs and how to deal with missing data in clinical research: A review. Phys. Ther. Rev. 2009, 14, 36–49. [Google Scholar] [CrossRef]
- Binggeli, C.; Spieker, L.E.; Corti, R.; Sudano, I.; Stojanovic, V.; Hayoz, D.; Lüscher, T.F.; Noll, G. Statins enhance postischemic hyperemia in the skin circulation of hypercholesterolemic patients. J. Am. Coll. Cardiol. 2003, 42, 71–77. [Google Scholar] [CrossRef]
- Cracowski, J.-L.; Minson, C.T.; Salvat-Melis, M.; Halliwill, J.R. Methodological issues in the assessment of skin microvascular endothelial function in humans. Trends Pharmacol. Sci. 2006, 27, 503–508. [Google Scholar] [CrossRef]
- Yamamoto-Suganuma, R.; Aso, Y. Relationship between post-occlusive forearm skin reactive hyperaemia and vascular disease in patients with type 2 diabetes—A novel index for detecting micro- and macrovascular dysfunction using laser Doppler flowmetry. Diabetic Med. 2009, 26, 83–88. [Google Scholar] [CrossRef]
- Lanting, S.M.; Way, K.L.; Sabag, A.; Sultana, R.N.; Johnson, N.A.; Baker, M.K.; Gerofi, J.A.; Caterson, I.D.; Twigg, S.M.; Chuter, V.H. Degree of adiposity and obesity severity is associated with cutaneous microvascular dysfunction in type 2 diabetes. Microvasc. Res. 2021, 136, 104149. [Google Scholar] [CrossRef]
- Kraemer-Aguiar, L.G.; Laflor, C.M.; Bouskela, E. Skin microcirculatory dysfunction is already present in normoglycemic subjects with metabolic syndrome. Metabolis 2008, 57, 1740–1746. [Google Scholar] [CrossRef]
- Van Der Heijden, D.J.; van Leeuwen, M.A.; Janssens, G.N.; Lenzen, M.J.; van de Ven, P.M.; Eringa, E.C.; van Royen, N. Body mass index is associated with microvascular endothelial dysfunction in patients with treated metabolic risk factors and suspected coronary artery disease. J. Am. Heart Assoc. 2017, 6, e006082. [Google Scholar] [CrossRef]
- Cohen, N.; Dunstan, D.; Robinson, C.; Vulikh, E.; Zimmet, P.; Shaw, J. Improved endothelial function following a 14-month resistance exercise training program in adults with type 2 diabetes. Diabetes Res. Clin. Pract. 2008, 79, 405–411. [Google Scholar] [CrossRef]
- Vinet, A.; Obert, P.; Courteix, D.; Chapier, R.; Lesourd, B.; Verney, J.; Dutheil, F.; Walther, G. Different modalities of exercise improve macrovascular function but not microvascular function in metabolic syndrome: The RESOLVE randomized trial. Int. J. Cardiol. 2018, 267, 165–170. [Google Scholar] [CrossRef]
| Characteristic | Moderate-Intesity Continuous Training—MICT (n = 10) | High-Intensity Interval Training—HIIT (n = 12) | Control Group Placebo—PLA (n = 11) | Between-Group (p-Value) |
|---|---|---|---|---|
| Age (year), mean (SD) | 56.8 (6.8) | 58.3 (6.9) | 52.9 (8.7) | 0.26 |
| Sex, number male (%) | 4 (40) | 7 (58) | 7 (64) | 0.53 |
| Weight (kg), mean (SD) | 95.6 (16.9) | 110.4 (14.5) | 106.0 (16.9) | 0.13 |
| Height (m), mean (SD) | 1.67 (0.1) | 1.72 (0.09) | 172 (0.09) | 0.44 |
| Body mass index (kg/m2) | 33.9 (3.2) | 37.5 (5.2) | 35.8 (5.4) | 0.26 |
| Waist circumference (cm), mean (SD) | 110.2 (9.7) | 122.0 (11.3) | 116.2 (13.1) | 0.09 |
| Hip circumference (cm), mean (SD) | 118.4 (8.6) | 123.4 (11.6) | 118.7 (10.6) | 0.49 |
| Visceral adipose tissue (cm3), mean (SD) | 6327 (2489) | 8535 (2935) | 7983 (2816) | 0.21 |
| Abdominal subcutaneous adipose tissue (cm3), mean (SD) | 11,574 (2682) | 11,810 (3203) | 12,118 (3969) | 0.94 |
| Diabetes duration (year), mean (SD) | 7.3 (5.3) | 9.3 (7.0) | 6.9 (5.9) | 0.65 |
| HbA1c [% National Glycohemoglobin Standardaization Program (NGSP) units], mean (SD) | 7.2 (1.3) | 7.1 (1.4) | 7.6 (1.5) | 0.63 |
| Fasting blood glucose (mmol/L), mean (SD) | 7.7 (2.0) | 7.6 (2.7) | 9.1 (3.9) | 0.49 |
| VO2peak (mL/kg/min), mean (SD) | 21.2 (5.3) | 20.8 (2.5) | 19.6 (4.3) | 0.69 |
| Resting heart rate (bpm), mean (SD) | 69 (8) | 68 (8) | 74 (12) | 0.33 |
| Oral hypoglycaemic agents alone or in combination with insulin, number (%) | 8 (80) | 12 (100) | 11 (100) | 0.86 |
| Anti-hypertensive therapy, number (%) | 5 (50) | 10 (83) | 7 (64) | 0.25 |
| Lipid-lowering therapy, number (%) | 8 (80) | 5 (42) | 7 (64) | 0.06 |
| Current smoker, number (%) | 0 (0) | 1(8) | 0 (0) | 0.41 |
| Systolic blood pressure (mmHg), mean (SD) | 129 (11.4) | 142 (9.8) | 137 (18.6) | 0.12 |
| Toe systolic pressure (mmHg), mean, (SD) | 102 (21.0) | 114 (20) | 104.4 (29.6) | 0.50 |
| Ankle-brachial index, mean (SD) | 1.08 (0.06) | 1.03 (0.13) | 1.06 (0.13) | 0.60 |
| Toe-brachial index, mean (SD) | 0.79 (0.15) | 0.80 (0.11) | 0.76 (0.21) | 0.87 |
| Sensory neuropathy, number (%) | 1 (10) | 0 (0) | 0 (0) | 0.31 |
| Post-occlusive reactive hyperaemia | ||||
| Baseline [FU (Flux Units)], mean (SD) | 37.2 (35.1) | 27.6 (21.6) | 37.15 (21.15) | 0.63 |
| AuC, index (post FU:pre FU), mean (SD) | 3.60 (2.33) | 3.83 (2.44) | 3.08 (0.96) | 0.69 |
| P%BL, mean (SD) | 501.1 (200.0) | 542.3 (307.9) | 447.9 (154.1) | 0.66 |
| Peak (FU), mean (SD) | 150.4 (117.2) | 119.3 (79.2) | 152.9 (87.2) | 0.67 |
| Time to peak (s), mean (SD) | 42.5 (43.0) | 30.1 (22.9) | 21.5 (11.3) | 0.28 |
| MICT (n = 10) | HIIT (n = 12) | PLA (n = 11) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Pre | Post | Change | Pre | Post | Change | Pre | Post | Change | p Value | |
| AuC index | 3.6 ± 2.3 | 4.1 ± 1.8 | 0.48 ± 1.52 | 3.8 ± 2.4 | 3.8 ± 1.9 | −0.07 ± 1.72 | 3.1 ± 1.0 | 2.9 ± 1.0 | −0.20 ± 0.82 | 0.25 |
| P%BL | 501.1 ± 200.0 | 504.7 ± 161.9 | 3.6 ± 161.6 | 542.3 ± 307.9 | 464.9 ± 269.6 | −75.1 ± 388.0 | 447.9 ± 154.1 | 498.7 ± 228.0 | 50.8 ± 194.3 | 0.80 |
| Peak | 150.4 ± 117.2 | 150.3 ± 130.1 | −0.1 ± 66.0 | 119.3 ± 79.2 | 157.2 ± 115.1 | 37.9 ± 132.8 | 152.9 ± 87.2 | 208.9 ± 151.0 | 56.0 ± 116.0 | 0.44 |
| TtPeak | 42.5 ± 43.0 | 23.4 ± 17.4 | −19.1 ± 34.5 | 30.1 ± 22.9 | 31.0 ± 17.5 | 0.8 ± 34.9 | 21.5 ± 11.3 | 29.2 ± 18.9 | 7.7 ± 13.2 | 0.54 |
| STP | 102 ± 21.0 | 118.6 ± 20.5 | 16.3 ± 20.0 | 114.1 ± 20.0 | 116.7 ± 25.9 | 2.6 ± 28.9 | 104.4 ± 29.6 | 108.3 ± 33.8 | 3.9 ± 25.5 | 0.55 |
| TBI | 0.79 ± 0.15 | 0.88 ± 0.09 | 0.09 ± 0.16 | 0.80 ± 0.10 | 0.78 ± 0.12 | −0.02 ± 0.17 | 0.76 ± 0.21 | 0.78 ± 0.18 | 0.01 ± 0.17 | 0.16 |
| ABI | 1.08 ± 0.06 | 1.05 ± 0.10 | −0.04 ± 0.09 | 1.03 ± 0.13 | 1.09 ± 0.15 | 0.06 ± 0.17 | 1.06 ± 0.13 | 1.06 ± 0.14 | −0.01 ± 0.08 | 0.42 |
| MICT (n = 10) | HIIT (n = 12) | PLA (n = 11) | |||||
|---|---|---|---|---|---|---|---|
| Baseline | Follow-Up | Baseline | Follow-Up | Baseline | Follow-Up | p Value | |
| Body composition | |||||||
| Body weight (Kg) | 95.6 ± 16.9 | 95.3 ± 17.5 | 110.4 ± 14.5 | 110.2 ± 14.1 | 106.0 ± 16.9 | 107.3 ± 18.5 | 0.46 |
| Body mass index (kg/m2) | 33.9 ± 3.2 | 33.8 ± 3.4 | 37.5 ± 5.2 | 37.5 ± 5.1 | 35.8 ± 5.4 | 36.1 ± 5.8 | 0.54 |
| Waist (cm) | 110.2 ± 9.7 | 107.5 ± 9.2 | 122.0 ± 11.3 | 118.1 ± 12.5 | 116.2 ± 13.1 | 115.5 ± 12.3 | 0.11 |
| Hip (cm) | 118.4 ± 8.6 | 116.4 ± 9.6 | 123.4 ± 11.6 | 122.0 ± 9.9 | 118.7 ± 10.6 | 119.6 ± 11.1 | 0.24 |
| Cardiorespiratory fitness | |||||||
| Systolic brachial pressure (mmHg) | 128.9 ± 11.4 | 133.1 ± 12.5 | 142.2 ± 9.8 | 138.5 ± 13.7 | 136.9 ± 18.6 | 142.7 ± 20.0 | 0.50 |
| Heart rate (bpm) | 69 ± 8 | 69 ± 5.9 | 68 ± 7.8 | 70 ± 6.5 | 74 ± 12.4 | 73 ± 13.3 | 0.84 |
| VO2peak (L/min) | 2.1 ± 0.9 | 2.3 ± 0.7 | 2.3 ± 0.4 | 2.4 ± 0.4 | 2.0 ± 0.5 | 2.0 ± 0.6 | 0.40 |
| VO2peak (mL/kg/min) | 21.2 ± 6.2 | 23.7 ± 7.5 | 20.8 ± 2.5 | 21.7 ± 2.3 | 19.5 ± 4.3 | 18.7 ± 4.7 | 0.05 |
| Biochemistry and Lipids | |||||||
| Aspartate transaminase (U/L) | 23 ± 6.1 | 23.1 ± 4.6 | 39.1 ± 29.2 | 27.8 ± 16.5 | 25.6 ± 15.3 | 22.5 ± 7.1 | 0.77 |
| Alanine aminotransferase (U/L) | 32 ± 11.6 | 29.9 ± 12.5 | 44.3 ± 31.8 | 34.7 ± 28.5 | 29.8 ± 15.1 | 31.8 ± 17.1 | 0.38 |
| C-reactive protein (mg/L) | 3.7 ± 4.7 | 3.2 ± 2.5 | 4.5 ± 5.7 | 4.3 ± 3.5 | 4.3 ± 3.7 | 5.3 ± 4.9 | 0.42 |
| Cholesterol (mmol/L) | 4.5 ± 0.8 | 4.5 ± 0.5 | 4.5 ± 0.7 | 4.3 ± 0.9 | 4.5 ± 0.9 | 4.6 ± 1.0 | 0.67 |
| Triglycerides (mmol/L) | 1.6 ± 0.5 | 1.7 ± 0.4 | 1.5 ± 0.5 | 1.6 ± 0.6 | 5.3 ± 11.3 | 2.4 ± 1.4 | 0.28 |
| High-density lipoprotein (mmol/L) | 1.2 ± 0.3 | 1.2 ± 0.2 | 1.1 ± 0.2 | 1.1 ± 0.2 | 1.2 ± 0.3 | 1.2 ± 0.2 | 0.59 |
| Low-density lipoprotein (mmol/L) | 2.6 ± 0.7 | 2.5 ± 0.5 | 2.7 ± 0.6 | 2.5 ± 0.7 | 2.4 ± 0.7 | 2.4 ± 0.8 | 0.90 |
| Fasting blood glucose (mmol/L) | 7.7 ± 2.0 | 7.5 ± 2.3 | 7.6 ± 2.7 | 7.4 ± 1.5 | 9.1 ± 3.9 | 8.9 ± 3.6 | 0.69 |
| Insulin (mU/L) | 12.2 ± 5.5 | 12.4 ± 5.9 | 20.6 ± 30.3 | 34.8 ± 68.4 | 13.7 ± 6.1 | 32.0 ± 59.9 | 0.62 |
| HbA1c—IFCC (mmol/mol) | 53 ± 15 | 51 ± 11 | 54 ± 15 | 51 ± 8 | 60 ± 16 | 62 ± 15 | 0.07 |
| HbA1c—NGSP (%) | 7.0 ± 1.3 | 6.8 ± 1.0 | 7.1 ± 1.4 | 6.8 ± 0.7 | 7.6 ± 1.5 | 7.8 ± 1.4 | 0.07 |
| Free fatty acids (μmol/L) | 493.3 ± 225.1 | 364.4 ± 116.0 | 503.8 ± 196.8 | 488.4 ± 166.6 | 600.6 ± 168.7 | 473.0 ± 160.2 | 0.18 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lanting, S.; Way, K.; Sabag, A.; Sultana, R.; Gerofi, J.; Johnson, N.; Baker, M.; Keating, S.; Caterson, I.; Twigg, S.; et al. The Efficacy of Exercise Training for Cutaneous Microvascular Reactivity in the Foot in People with Diabetes and Obesity: Secondary Analyses from a Randomized Controlled Trial. J. Clin. Med. 2022, 11, 5018. https://doi.org/10.3390/jcm11175018
Lanting S, Way K, Sabag A, Sultana R, Gerofi J, Johnson N, Baker M, Keating S, Caterson I, Twigg S, et al. The Efficacy of Exercise Training for Cutaneous Microvascular Reactivity in the Foot in People with Diabetes and Obesity: Secondary Analyses from a Randomized Controlled Trial. Journal of Clinical Medicine. 2022; 11(17):5018. https://doi.org/10.3390/jcm11175018
Chicago/Turabian StyleLanting, Sean, Kimberley Way, Angelo Sabag, Rachelle Sultana, James Gerofi, Nathan Johnson, Michael Baker, Shelley Keating, Ian Caterson, Stephen Twigg, and et al. 2022. "The Efficacy of Exercise Training for Cutaneous Microvascular Reactivity in the Foot in People with Diabetes and Obesity: Secondary Analyses from a Randomized Controlled Trial" Journal of Clinical Medicine 11, no. 17: 5018. https://doi.org/10.3390/jcm11175018
APA StyleLanting, S., Way, K., Sabag, A., Sultana, R., Gerofi, J., Johnson, N., Baker, M., Keating, S., Caterson, I., Twigg, S., & Chuter, V. (2022). The Efficacy of Exercise Training for Cutaneous Microvascular Reactivity in the Foot in People with Diabetes and Obesity: Secondary Analyses from a Randomized Controlled Trial. Journal of Clinical Medicine, 11(17), 5018. https://doi.org/10.3390/jcm11175018






