Prevalence and Long-Term Prognosis of Post-Intensive Care Syndrome after Sepsis: A Single-Center Prospective Observational Study
Abstract
:1. Introduction
2. Material and Methods
2.1. Study Design and Setting
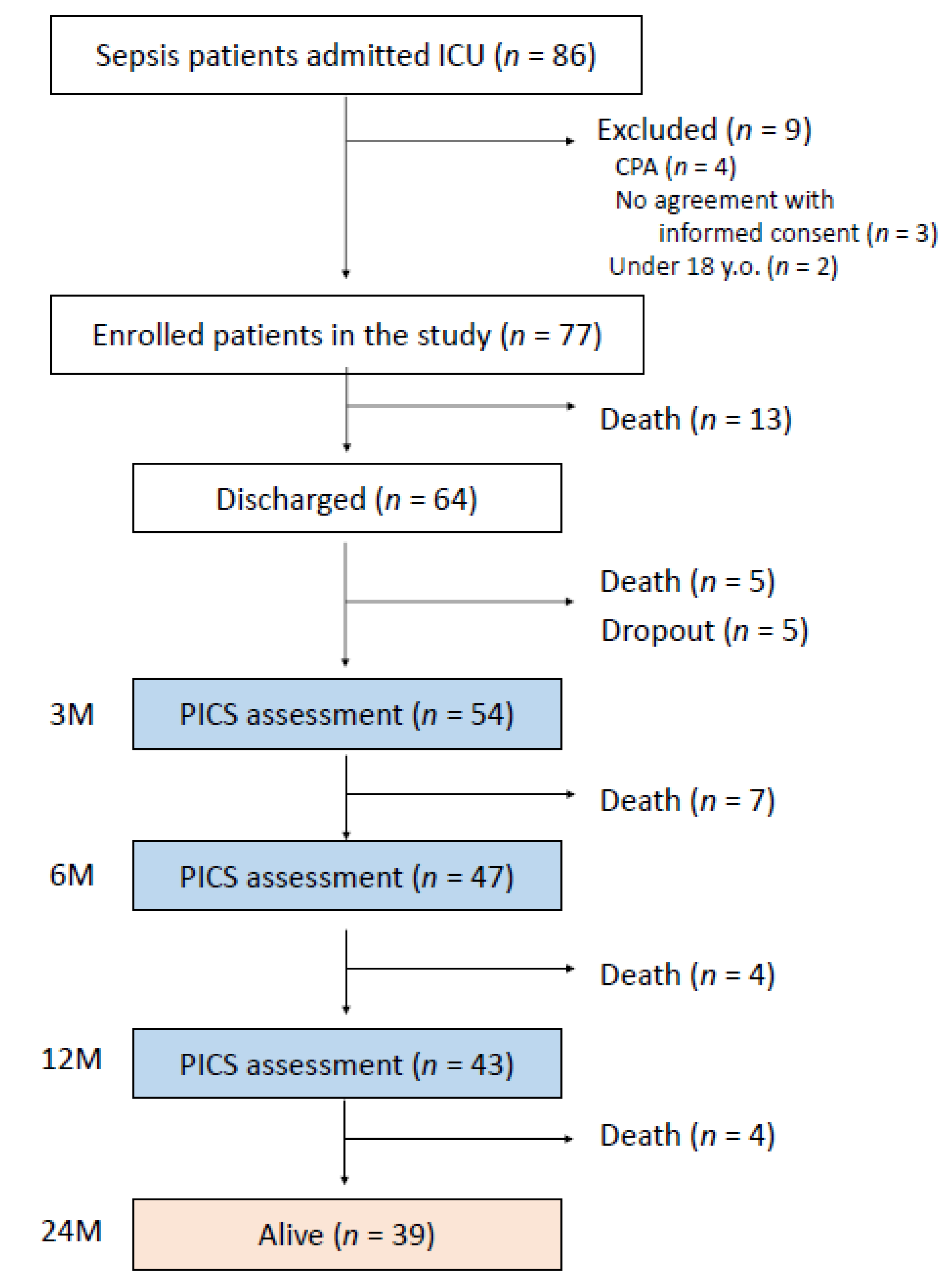
2.2. Study Population and Eligibility Criteria
2.3. Procedures
2.4. Outcomes
2.5. Statistical Analysis
3. Results
3.1. 2-Year Survival after Sepsis
3.2. Prevalence of PICS after Sepsis
3.3. Risk Factors for PICS
3.4. Patients with PICS at 3 Months after Sepsis Showed Poorer Long-Term Outcome
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| PICS | post-intensive care syndrome |
| ICU | intensive care unit |
| ICDSC | Intensive Care Delirium Screening Checklist |
| SMQ | Short-Memory Questionnaire |
| HADS | Hospital Anxiety and Depression Scale |
| GCS | Glasgow Coma Scale |
| CPA | cardiopulmonary arrest |
| SAE | septic encephalopathy |
References
- Malik, S.S.; Maqbool, M.; Rafi, A.; Kokab, N. Prevalence and outcome of infections in intensive care units of a tertiary care hospital in north India. Crit. Care Innov. 2022, 5, 20–28. [Google Scholar]
- Singer, M.; Deutschman, C.S.; Seymour, C.W.; Shankar-Hari, M.; Annane, D.; Bauer, M.; Bellomo, R.; Bernard, G.R.; Chiche, J.D.; Coopersmith, C.M.; et al. The third international consensus definitions for sepsis and septic shock (Sepsis-3). JAMA J. Am. Med. Assoc. 2016, 315, 801–810. [Google Scholar] [CrossRef] [PubMed]
- Fleischmann, C.; Scherag, A.; Adhikari, N.K.; Hartog, C.S.; Tsaganos, T.; Schlattmann, P.; Angus, D.C.; Reinhart, K. Assessment of global incidence and mortality of hospital-treated sepsis. Current estimates and limitations. Am. J. Respir. Crit. Care Med. 2016, 193, 259–272. [Google Scholar] [CrossRef] [PubMed]
- Imaeda, T.; Nakada, T.A.; Takahashi, N.; Yamao, Y.; Nakagawa, S.; Ogura, H.; Shime, N.; Umemura, Y.; Matsushima, A.; Fushimi, K. Trends in the incidence and outcome of sepsis using data from a Japanese nationwide medical claims database-the Japan Sepsis Alliance (JaSA) study group. Crit. Care 2021, 25, 338. [Google Scholar] [CrossRef]
- Evans, L.; Rhodes, A.; Alhazzani, W.; Antonelli, M.; Coopersmith, C.M.; French, C.; Machado, F.R.; McIntyre, L.; Ostermann, M.; Prescott, H.C.; et al. Surviving sepsis campaign: International guidelines for management of sepsis and septic shock 2021. Intensive Care Med. 2021, 47, 1181–1247. [Google Scholar] [CrossRef] [PubMed]
- Prescott, H.C.; Angus, D.C. Enhancing recovery from sepsis: A review. JAMA J. Am. Med. Assoc. 2018, 319, 62–75. [Google Scholar] [CrossRef]
- Mostel, Z.; Perl, A.; Marck, M.; Mehdi, S.F.; Lowell, B.; Bathija, S.; Santosh, R.; Pavlov, V.A.; Chavan, S.S.; Roth, J. Post-sepsis syndrome—An evolving entity that afflicts survivors of sepsis. Mol. Med. 2019, 26, 6. [Google Scholar] [CrossRef]
- Needham, D.M.; Davidson, J.; Cohen, H.; Hopkins, R.O.; Weinert, C.; Wunsch, H.; Zawistowski, C.; Bemis-Dougherty, A.; Berney, S.C.; Bienvenu, O.J.; et al. Improving long-term outcomes after discharge from intensive care unit: Report from a stakeholders’ conference. Crit. Care Med. 2012, 40, 502–509. [Google Scholar] [CrossRef]
- Inoue, S.; Hatakeyama, J.; Kondo, Y.; Hifumi, T.; Sakuramoto, H.; Kawasaki, T.; Taito, S.; Nakamura, K.; Unoki, T.; Kawai, Y.; et al. Post-intensive care syndrome: Its pathophysiology, prevention, and future directions. Acute Med. Surg. 2019, 6, 233–246. [Google Scholar] [CrossRef]
- Nakanishi, N.; Liu, K.; Kawakami, D.; Kawai, Y.; Morisawa, T.; Nishida, T.; Sumita, H.; Unoki, T.; Hifumi, T.; Iida, Y.; et al. Post-intensive care syndrome and its new challenges in coronavirus disease 2019 (COVID-19) pandemic: A review of recent advances and perspectives. J. Clin. Med. 2021, 10, 3870. [Google Scholar] [CrossRef]
- Vrettou, C.S.; Mantziou, V.; Vassiliou, A.G.; Orfanos, S.E.; Kotanidou, A.; Dimopoulou, I. Post-intensive care syndrome in survivors from critical illness including COVID-19 patients: A narrative review. Life 2022, 12, 107. [Google Scholar] [CrossRef] [PubMed]
- Katz, S.; Ford, A.B.; Moskowitz, R.W.; Jackson, B.A.; Jaffe, M.W. Studies of illness in the aged. The index of ADL: A standardized measure of biological and psychosocial function. JAMA J. Am. Med. Assoc. 1963, 185, 914–919. [Google Scholar] [CrossRef] [PubMed]
- Mahoney, F.I.; Barthel, D.W. Functional evaluation: The barthel index. Md. State Med. J. 1965, 14, 61–65. [Google Scholar]
- Jorm, A.F. The informant questionnaire on cognitive decline in the elderly (IQCODE): A review. Int. Psychogeriatr. 2004, 16, 275–293. [Google Scholar] [PubMed]
- Koss, E.; Patterson, M.B.; Ownby, R.; Stuckey, J.C.; Whitehouse, P.J. Memory evaluation in Alzheimer’s disease. Caregivers’ appraisals and objective testing. Arch. Neurol. 1993, 50, 92–97. [Google Scholar] [CrossRef]
- Zigmond, A.S.; Snaith, R.P. The hospital anxiety and depression scale. Acta Psychiatr. Scand. 1983, 67, 361–370. [Google Scholar] [CrossRef]
- Cilloniz, C.; Peroni, H.J.; Gabarrús, A.; García-Vidal, C.; Pericàs, J.M.; Bermejo-Martin, J.; Torres, A. Lymphopenia is associated with poor outcomes of patients with community-acquired pneumonia and sepsis. Open Forum Infect. Dis. 2021, 8, ofab169. [Google Scholar] [CrossRef]
- Drewry, A.M.; Samra, N.; Skrupky, L.P.; Fuller, B.M.; Compton, S.M.; Hotchkiss, R.S. Persistent lymphopenia after diagnosis of sepsis predicts mortality. Shock 2014, 42, 383–391. [Google Scholar] [CrossRef]
- Pierrakos, C.; Velissaris, D.; Bisdorff, M.; Marshall, J.C.; Vincent, J.L. Biomarkers of sepsis: Time for a reappraisal. Crit. Care 2020, 24, 287. [Google Scholar] [CrossRef]
- Koozi, H.; Lengquist, M.; Frigyesi, A. C-reactive protein as a prognostic factor in intensive care admissions for sepsis: A Swedish multicenter study. J. Crit. Care 2020, 56, 73–79. [Google Scholar] [CrossRef]
- Huang, Y.; Chen, R.; Jiang, L.; Li, S.; Xue, Y. Basic research and clinical progress of sepsis-associated encephalopathy. J. Intensive Med. 2021, 1, 90–95. [Google Scholar] [CrossRef]
- Kanda, Y. Investigation of the freely available easy-to-use software ‘EZR’ for medical statistics. Bone Marrow Transplant. 2013, 48, 452–458. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Korosec Jagodic, H.; Jagodic, K.; Podbregar, M. Long-term outcome and quality of life of patients treated in surgical intensive care: A comparison between sepsis and trauma. Crit. Care 2006, 10, R134. [Google Scholar] [CrossRef] [PubMed]
- Rahmel, T.; Schmitz, S.; Nowak, H.; Schepanek, K.; Bergmann, L.; Halberstadt, P.; Horter, S.; Peters, J.; Adamzik, M. Long-term mortality and outcome in hospital survivors of septic shock, sepsis, and severe infections: The importance of aftercare. PLoS ONE 2020, 15, e0228952. [Google Scholar]
- Stremitzer, S.; Strobl, S.; Kure, V.; Birsan, T.; Puhalla, H.; Herbst, F.; Stift, A. Treatment of perianal sepsis and long-term outcome of recurrence and continence. Colorectal Dis. 2011, 13, 703–707. [Google Scholar] [CrossRef] [PubMed]
- Gritte, R.B.; Souza-Siqueira, T.; Curi, R.; Machado, M.C.C.; Soriano, F.G. Why septic patients remain sick after hospital discharge? Front. Immunol. 2020, 11, 605666. [Google Scholar] [CrossRef] [PubMed]
- Bowles, K.H.; Murtaugh, C.M.; Jordan, L.; Barron, Y.; Mikkelsen, M.E.; Whitehouse, C.R.; Chase, J.D.; Ryvicker, M.; Feldman, P.H. Sepsis survivors transitioned to home health care: Characteristics and early readmission risk factors. J. Am. Med. Dir. Assoc. 2020, 21, 84–90.e82. [Google Scholar] [CrossRef] [PubMed]
- Jones, T.K.; Fuchs, B.D.; Small, D.S.; Halpern, S.D.; Hanish, A.; Umscheid, C.A.; Baillie, C.A.; Kerlin, M.P.; Gaieski, D.F.; Mikkelsen, M.E. Post-acute care use and hospital readmission after sepsis. Ann. Am. Thorac. Soc. 2015, 12, 904–913. [Google Scholar] [PubMed]
- Kim, J.S.; Kim, Y.J.; Ryoo, S.M.; Sohn, C.H.; Ahn, S.; Seo, D.W.; Lim, K.S.; Kim, W.Y. Risk factors for same pathogen sepsis readmission following hospitalization for septic shock. J. Clin. Med. 2019, 8, 181. [Google Scholar] [CrossRef]
- Stenholt, P.O.O.; Abdullah, S.; Sorensen, R.H.; Nielsen, F.E. Independent predictors for 90-day readmission of emergency department patients admitted with sepsis: A prospective cohort study. BMC Infect. Dis. 2021, 21, 315. [Google Scholar] [CrossRef]
- Prescott, H.C.; Langa, K.M.; Iwashyna, T.J. Readmission diagnoses after hospitalization for severe sepsis and other acute medical conditions. JAMA J. Am. Med. Assoc. 2015, 313, 1055–1057. [Google Scholar] [CrossRef] [PubMed]
- Davidson, J.E.; Harvey, M.A.; Schuller, J.; Black, G. Post-intensive care syndrome: What is it and how to help prevent it. Am. Nurse Today 2013, 8, 32–38. [Google Scholar]
- Granja, C.; Dias, C.; Costa-Pereira, A.; Sarmento, A. Quality of life of survivors from severe sepsis and septic shock may be similar to that of others who survive critical illness. Crit. Care 2004, 8, R91–R98. [Google Scholar] [CrossRef] [PubMed]
- Huang, C.Y.; Daniels, R.; Lembo, A.; Hartog, C.; O’Brien, J.; Heymann, T.; Reinhart, K.; Nguyen, H.B. Sepsis survivors engagement P: Life after sepsis: An international survey of survivors to understand the post-sepsis syndrome. Int. J. Qual. Health Care 2019, 31, 191–198. [Google Scholar] [CrossRef]
- Iwashyna, T.J.; Ely, E.W.; Smith, D.M.; Langa, K.M. Long-term cognitive impairment and functional disability among survivors of severe sepsis. JAMA J. Am. Med. Assoc. 2010, 304, 1787–1794. [Google Scholar] [CrossRef]
- Hopkins, R.O.; Key, C.W.; Suchyta, M.R.; Weaver, L.K.; Orme, J.F., Jr. Risk factors for depression and anxiety in survivors of acute respiratory distress syndrome. Gen. Hosp. Psychiatry 2010, 32, 147–155. [Google Scholar] [CrossRef]
- Jackson, J.C.; Hart, R.P.; Gordon, S.M.; Shintani, A.; Truman, B.; May, L.; Ely, E.W. Six-month neuropsychological outcome of medical intensive care unit patients. Crit. Care Med. 2003, 31, 1226–1234. [Google Scholar] [CrossRef]
- Weinert, C.; Meller, W. Epidemiology of depression and antidepressant therapy after acute respiratory failure. Psychosomatics 2006, 47, 399–407. [Google Scholar] [CrossRef]
- Marra, A.; Pandharipande, P.P.; Girard, T.D.; Patel, M.B.; Hughes, C.G.; Jackson, J.C.; Thompson, J.L.; Chandrasekhar, R.; Ely, E.W.; Brummel, N.E. Co-occurrence of post-intensive care syndrome problems among 406 survivors of critical illness. Crit. Care Med. 2018, 46, 1393–1401. [Google Scholar] [CrossRef]
- Kawakami, D.; Fujitani, S.; Morimoto, T.; Dote, H.; Takita, M.; Takaba, A.; Hino, M.; Nakamura, M.; Irie, H.; Adachi, T.; et al. Prevalence of post-intensive care syndrome among Japanese intensive care unit patients: A prospective, multicenter, observational J-PICS study. Crit. Care 2021, 25, 69. [Google Scholar] [CrossRef]
- Nanwani-Nanwani, K.; López-Pérez, L.; Giménez-Esparza, C.; Ruiz-Barranco, I.; Carrillo, E.; Arellano, M.S.; Díaz-Díaz, D.; Hurtado, B.; García-Muñoz, A.; Relucio, M.Á.; et al. Prevalence of post-intensive care syndrome in mechanically ventilated patients with COVID-19. Sci. Rep. 2022, 12, 7977. [Google Scholar] [CrossRef] [PubMed]
- Chao, P.W.; Shih, C.J.; Lee, Y.J.; Tseng, C.M.; Kuo, S.C.; Shih, Y.N.; Chou, K.T.; Tarng, D.C.; Li, S.Y.; Ou, S.M.; et al. Association of postdischarge rehabilitation with mortality in intensive care unit survivors of sepsis. Am. J. Respir. Crit. Care Med. 2014, 190, 1003–1011. [Google Scholar] [CrossRef] [PubMed]
- Gofton, T.E.; Young, G.B. Sepsis-associated encephalopathy. Nat. Rev. Neurol. 2012, 8, 557–566. [Google Scholar] [CrossRef]
- Salluh, J.I.; Soares, M.; Teles, J.M.; Ceraso, D.; Raimondi, N.; Nava, V.S.; Blasquez, P.; Ugarte, S.; Ibanez-Guzman, C.; Centeno, J.V.; et al. Delirium epidemiology in critical care (DECCA): An international study. Crit. Care 2010, 14, R210. [Google Scholar] [CrossRef] [Green Version]
- Widmann, C.N.; Heneka, M.T. Long-term cerebral consequences of sepsis. Lancet Neurol. 2014, 13, 630–636. [Google Scholar] [CrossRef]
- Lund-Sørensen, H.; Benros, M.E.; Madsen, T.; Sørensen, H.J.; Eaton, W.W.; Postolache, T.T.; Nordentoft, M.; Erlangsen, A. A nationwide cohort study of the association between hospitalization with infection and risk of death by suicide. JAMA Psychiatry 2016, 73, 912–919. [Google Scholar] [CrossRef] [PubMed]
- Ziaja, M. Septic encephalopathy. Curr. Neurol. Neurosci. Rep. 2013, 13, 383. [Google Scholar] [CrossRef]
- Inoue, S.; Suzuki, K.; Komori, Y.; Morishita, Y.; Suzuki-Utsunomiya, K.; Hozumi, K.; Inokuchi, S.; Sato, T. Persistent inflammation and T cell exhaustion in severe sepsis in the elderly. Crit. Care 2014, 18, R130. [Google Scholar] [CrossRef]
- Inoue, S.; Suzuki-Utsunomiya, K.; Okada, Y.; Iida, Y.; Taira, T.; Miura, N.; Tsuji, T.; Yamagiwa, T.; Morita, S.; Chiba, T.; et al. Reduction of immunocompetent T cells followed by prolonged lymphopenia in severe sepsis in the elderly. Crit. Care Med. 2013, 41, 810–819. [Google Scholar] [CrossRef]
- Spoden, M.; Hartog, C.S.; Schlattmann, P.; Freytag, A.; Ostermann, M.; Wedekind, L.; Storch, J.; Reinhart, K.; Gunster, C.; Fleischmann-Struzek, C. Occurrence and risk factors for new dependency on chronic care, respiratory support, dialysis and mortality in the first year after sepsis. Front. Med. 2022, 9, 878337. [Google Scholar] [CrossRef]
- Voiriot, G.; Oualha, M.; Pierre, A.; Salmon-Gandonnière, C.; Gaudet, A.; Jouan, Y.; Kallel, H.; Radermacher, P.; Vodovar, D.; Sarton, B.; et al. Chronic critical illness and post-intensive care syndrome: From pathophysiology to clinical challenges. Ann. Intensive Care 2022, 12, 58. [Google Scholar] [CrossRef] [PubMed]
- Ely, E.W.; Shintani, A.; Truman, B.; Speroff, T.; Gordon, S.M.; Harrell, F.E.; Jr Inouye, S.K.; Bernard, G.R.; Dittus, R.S. Delirium as a predictor of mortality in mechanically ventilated patients in the intensive care unit. JAMA J. Am. Med. Assoc. 2004, 291, 1753–1762. [Google Scholar] [CrossRef] [PubMed] [Green Version]




| Enrolled Patients | Non-PICS at 3 Months | PICS at 3 Months | p. Value | ||
|---|---|---|---|---|---|
| (n = 77) | (n = 17) | (n = 37) | |||
| Age | 73.00 (67.00, 79.00) | 70.00 (67.00, 73.00) | 77.00 (72.00, 82.00) | 0.02 | |
| Male (%) | 50 (64.9) | 15 (88.2) | 21 (56.8) | 0.03 | |
| Race (%) | Japanese | 75 (98.7) | 17 (100.0) | 37 (100.0) | |
| Guatemalan | 1 (1.3) | 0 (0.0) | 0 (0.0) | 1 | |
| Height (cm) | 160.70 (147.90, 168.15) | 172.00 (162.15, 176.35) | 147.80 (144.50, 162.90) | 0.11 | |
| Body weight (kg) | 54.00 (45.05, 60.25) | 50.00 (48.25, 58.20) | 52.00 (40.90, 54.25) | 0.57 | |
| Severity | |||||
| Septic shock on admission (%) | 42 (54.5) | 6 (35.3) | 23 (62.2) | 0.08 | |
| APACHE II score | 20.00 (16.00, 22.00) | 19.00 (16.00, 21.50) | 18.50 (16.00, 21.00) | 0.90 | |
| SOFA score at day 1 | 8.00 (6.75, 11.00) | 7.00 (5.25, 9.50) | 7.00 (6.25, 9.75) | 0.82 | |
| SOFA score at day 3 | 7.00 (5.00, 12.50) | 5.50 (4.25, 6.75) | 6.00 (5.00, 11.00) | 0.61 | |
| SOFA score at day 7 | 6.00 (4.50, 9.75) | 6.00 (6.00, 6.00) | 4.50 (3.00, 6.00) | 0.41 | |
| Comorbidity | |||||
| Hypertension (%) | 27 (35.1) | 4 (23.5) | 16 (43.2) | 0.23 | |
| Diabetes (%) | 22 (28.6) | 5 (29.4) | 11 (29.7) | 1 | |
| Cancer (%) | 18 (23.4) | 5 (29.4) | 6 (16.2) | 0.29 | |
| Autoimmune disorder (%) | 15 (19.5) | 5 (29.4) | 8 (21.6) | 0.73 | |
| Stroke (%) | 15 (19.5) | 3 (17.6) | 11 (29.7) | 0.51 | |
| Infection (%) | 11 (14.3) | 4 (23.5) | 5 (13.5) | 0.44 | |
| Renal failure (%) | 9 (11.7) | 3 (17.6) | 5 (13.5) | 0.70 | |
| COPD (%) | 7 (9.1) | 2 (11.8) | 3 (8.1) | 0.65 | |
| Asthma (%) | 5 (6.5) | 1 (5.9) | 2 (5.4) | 1 | |
| Mental disorder (%) | 3 (3.9) | 0 (0.0) | 2 (5.4) | 1 | |
| Dementia (%) | 3 (3.9) | 0 (0.0) | 3 (8.1) | 0.54 | |
| Trauma (%) | 2 (2.6) | 1 (5.9) | 0 (0.0) | 0.32 | |
| Liver failure (%) | 2 (2.6) | 0 (0.0) | 1 (2.7) | 1 | |
| Hematological disease (%) | 2 (2.6) | 2 (11.8) | 0 (0.0) | 0.10 | |
| CNS degenerative disease (%) | 2 (2.6) | 0 (0.0) | 0 (0.0) | 1 | |
| Endocrine disorder (%) | 2 (2.6) | 0 (0.0) | 1 (2.7) | 1 | |
| Medication before admission | |||||
| Immunosuppressant (%) | 4 (5.2) | 2 (11.8) | 0 (0.0) | 0.10 | |
| Steroids (%) | 11 (14.3) | 2 (11.8) | 6 (16.2) | 1 | |
| Causes of sepsis | |||||
| Pneumonia (%) | 29 (37.7) | 5 (29.4) | 16 (43.2) | 0.38 | |
| Intra-abdominal infection (%) | 13 (16.9) | 3 (17.6) | 7 (18.9) | 1 | |
| Urinary Tract Infection (%) | 10 (13.0) | 1 (5.9) | 7 (18.9) | 0.41 | |
| Soft tissue infection (%) | 10 (13.0) | 3 (17.6) | 4 (10.8) | 0.67 | |
| Burn (%) | 3 (3.9) | 0 (0.0) | 3 (8.1) | 0.54 | |
| CRBSI (%) | 2 (2.6) | 0 (0.0) | 0 (0.0) | 1 | |
| Ventilator | |||||
| at day 1 (%) | 35 (45.5) | 7 (41.2) | 17 (45.9) | 1 | |
| at day 3 (%) | 29 (37.7) | 2 (11.8) | 15 (40.5) | 0.11 | |
| at day 7 (%) | 22 (28.6) | 0 (0.0) | 13 (35.1) | 0.005 | |
| Emergency operation (%) | 4 (5.2) | 2 (11.8) | 0 (0.0) | 0.07 | |
| Hemoperfusion (%) | 9 (11.7) | 2 (11.8) | 4 (10.8) | 1 | |
| Steroid use (%) | 13 (16.9) | 2 (11.8) | 6 (16.2) | 1 | |
| ICU stay (day) | 4.00 (2.00, 8.00) | 3.00 (1.00, 5.50) | 4.00 (3.00, 8.00) | 0.25 | |
| Death in hospital (%) | 13 (16.9) | 0 (0.0) | 0 (0.0) | 1 | |
| Non-PICS at 3 Months | PICS at 3 Months | p. Value | |
|---|---|---|---|
| (n = 17) | (n = 37) | ||
| Barthel index (Physical assessment) | |||
| at 3 months | 96.00 (60.00, 100.00) | 60.00 (10.00, 92.00) | <0.01 |
| at 6 months | 98.00 (40.00, 100.00) | 62.50 (10.00, 98.00) | <0.01 |
| at 12 months | 98.00 (88.00, 100.00) | 70.00 (10.00, 98.00) | <0.01 |
| HADS (Mental assessment) | |||
| at 3 months | 3.50 (0.00, 6.00) | 6.50 (0.00, 14.00) | <0.01 |
| at 6 months | 1.50 (0.00, 5.00) | 3.00 (0.00, 12.00) | 0.08 |
| at 12 months | 1.00 (0.00, 2.00) | 1.00 (0.00, 12.00) | 0.19 |
| SMQ (Cognitive assessment) | |||
| at 3 months | 46.00 (46.00, 46.00) | 46.00 (14.00, 46.00) | <0.01 |
| at 6 months | 46.00 (40.00, 46.00) | 46.00 (15.00, 46.00) | 0.04 |
| at 12 months | 46.00 (38.00, 46.00) | 46.00 (15.00, 46.00) | 0.14 |
| P | M | C | Single | Double | Triple | Total | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| P | M | C | total | P + M | P + C | C + M | total | P + M + C | ||||||
| 3 months | n | 31 | 17 | 14 | 13 | 4 | 1 | 18 | 6 | 6 | 1 | 13 | 6 | 37 |
| % | 57.4 | 31.5 | 25.9 | 24.1 | 7.4 | 1.9 | 33.3 | 11.1 | 11.1 | 1.9 | 24.1 | 11.1 | 68.5 | |
| 6 months | n | 20 | 9 | 10 | 12 | 3 | 4 | 19 | 3 | 3 | 1 | 7 | 2 | 28 |
| % | 37.0 | 16.7 | 18.5 | 25.5 | 6.4 | 8.5 | 40.4 | 6.4 | 6.4 | 2.1 | 14.9 | 4.3 | 59.6 | |
| 12 months | n | 10 | 5 | 6 | 6 | 2 | 2 | 10 | 1 | 2 | 1 | 4 | 1 | 15 |
| % | 18.5 | 9.3 | 11.1 | 14.0 | 4.7 | 4.7 | 23.3 | 2.3 | 4.7 | 2.3 | 9.3 | 2.3 | 34.9 | |
| Enrolled Patients | Non-PICS at 3 Months | PICS at 3 Months | p. Value | |
|---|---|---|---|---|
| (n = 77) | (n = 17) | (n = 37) | ||
| Detection rate of blood culture (%) | ||||
| Day 1 | 34 (44.2) | 7 (41.2) | 19 (51.4) | 0.57 |
| Day 3–4 | 6 (7.8) | 2 (11.8) | 2 (5.4) | 0.58 |
| Day 7–8 | 8 (10.4) | 2 (11.8) | 5 (13.5) | 1 |
| Strain of bacteria and fungus from blood cultures (%) | ||||
| GPC | ||||
| Staphylococcus aureus | 1 (1.3) | 0 (0.0) | 0 (0.0) | |
| Staphylococcus hominis | 1 (1.3) | 0 (0.0) | 1 (2.7) | |
| Streptococcus constellatus | 1 (1.3) | 0 (0.0) | 1 (2.7) | |
| Streptococcus mitis group | 1 (1.3) | 0 (0.0) | 0 (0.0) | |
| Streptococcus pneumoniae | 1 (1.3) | 1 (5.9) | 0 (0.0) | |
| Streptococcus pyogenes | 1 (1.3) | 1 (5.9) | 0 (0.0) | |
| Streptococcus dysgalactiae | 2 (2.6) | 1 (5.9) | 1 (2.7) | |
| Clostridium perfringens | 1 (1.3) | 0 (0.0) | 1 (2.7) | |
| Total | 9 (11.7) | 3 (17.6) | 4 (23.5) | 0.67 |
| GNR | ||||
| Escherichia coli | 6 (7.8) | 4 (23.5) | 1 (2.7) | |
| Klebsiella pneumoniae | 5 (6.5) | 1 (5.9) | 3 (8.1) | |
| Haemophilus influenzae | 1 (1.3) | 0 (0.0) | 0 (0.0) | |
| Total | 12 (15.6) | 5 (6.5) | 4 (23.5) | 0.19 |
| Opportunistic pathogen | ||||
| MRSA | 5 (6.5) | 0 (0.0) | 5 (22.7) | |
| MRSE | 3 (3.9) | 1 (5.9) | 1 (2.7) | |
| Pseudomonas aeruginosa | 1 (1.3) | 0 (0.0) | 1 (2.7) | |
| Escherichia coli (ESBL) | 4 (5.2) | 0 (0.0) | 2 (5.4) | |
| Enterococcus faecalis | 4 (5.2) | 0 (0.0) | 3 (8.1) | |
| Enterobacter cloacae | 2 (2.6) | 0 (0.0) | 2 (5.4) | |
| Candida albicans | 5 (6.5) | 1 (5.9) | 2 (5.4) | |
| Candida glabrata | 1 (1.3) | 0 (0.0) | 1 (2.7) | |
| Candida tropicali | 2 (2.6) | 0 (0.0) | 1 (2.7) | |
| Total | 27(35.1) | 2 (11.8) | 18(48.6) | 0.01 |
| Outcome: PICS at 3 Months | |||
|---|---|---|---|
| Odds Ratio | 95% CI | p. Value | |
| Age | 1.04 | 0.94–1.14 | 0.45 |
| Male | 1.62 | 0.094–28.1 | 0.74 |
| SOFA | 1.05 | 0.75–1.47 | 0.76 |
| GCS at day 7 | 0.49 | 0.25–0.96 | 0.04 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Inoue, S.; Nakanishi, N.; Sugiyama, J.; Moriyama, N.; Miyazaki, Y.; Sugimoto, T.; Fujinami, Y.; Ono, Y.; Kotani, J. Prevalence and Long-Term Prognosis of Post-Intensive Care Syndrome after Sepsis: A Single-Center Prospective Observational Study. J. Clin. Med. 2022, 11, 5257. https://doi.org/10.3390/jcm11185257
Inoue S, Nakanishi N, Sugiyama J, Moriyama N, Miyazaki Y, Sugimoto T, Fujinami Y, Ono Y, Kotani J. Prevalence and Long-Term Prognosis of Post-Intensive Care Syndrome after Sepsis: A Single-Center Prospective Observational Study. Journal of Clinical Medicine. 2022; 11(18):5257. https://doi.org/10.3390/jcm11185257
Chicago/Turabian StyleInoue, Shigeaki, Nobuto Nakanishi, Jun Sugiyama, Naoki Moriyama, Yusuke Miyazaki, Takashi Sugimoto, Yoshihisa Fujinami, Yuko Ono, and Joji Kotani. 2022. "Prevalence and Long-Term Prognosis of Post-Intensive Care Syndrome after Sepsis: A Single-Center Prospective Observational Study" Journal of Clinical Medicine 11, no. 18: 5257. https://doi.org/10.3390/jcm11185257







