Adaptive Posture-Balance Cardiac Rehabilitation Exercise Significantly Improved Physical Tolerance in Patients with Cardiovascular Diseases
Abstract
:1. Introduction
2. Materials and Methods
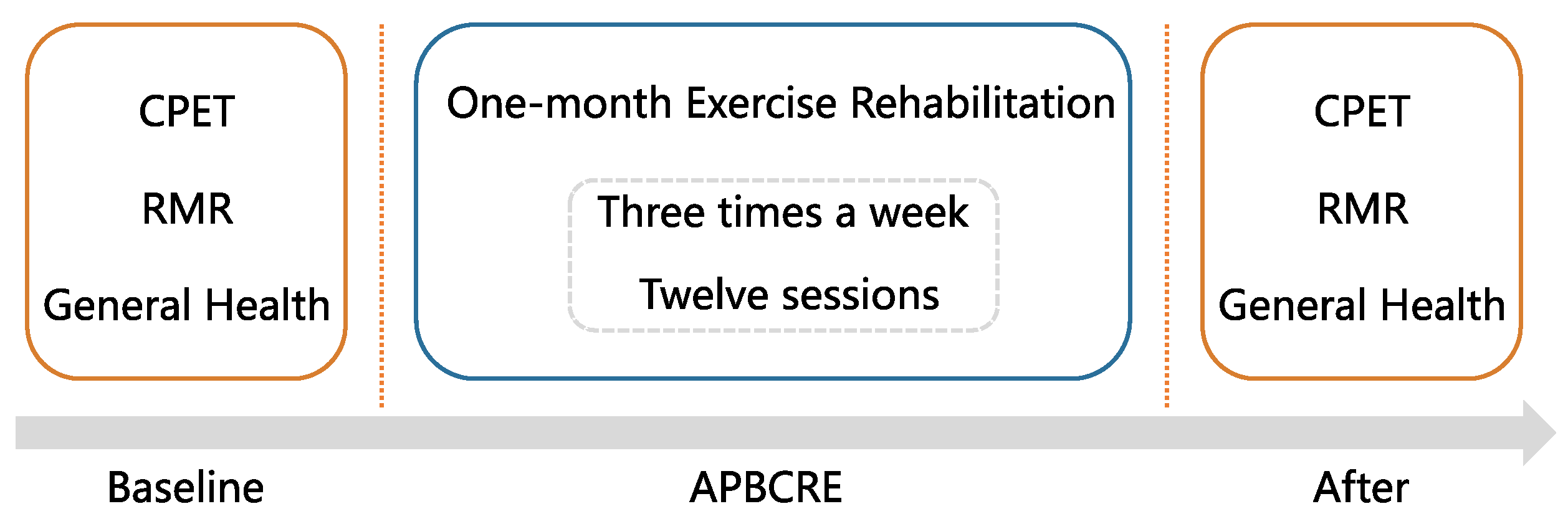
2.1. Study Design
2.2. Patient Selection
2.3. Rehabilitation Protocol
2.4. Outcome Measure
- Cardiopulmonary Exercise Testing (CPET)
- Resting Metabolic Rate (RMR)
- General health assessment of quality of life, anxiety and depression
2.5. Sample Size
2.6. Statistical Analysis
3. Results
3.1. Participants Characteristics
3.2. Physical Tolerance
3.3. Secondary Endpoints
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
| Danger Level | Symptoms | Clinical Indicator | Standard |
|---|---|---|---|
| Low |
|
| Complies with all standards |
| Medium |
|
| Does not comply with low-level and high-level |
| High |
|
| Complies with one standard |
References
- Montalescot, G.; Sechtem, U.; Achenbach, S.; Andreotti, F.; Arden, C.; Budaj, A.; Bugiardini, R.; Crea, F.; Cuisset, T.; Di Mario, C.; et al. 2013 ESC Guidelines on the Management of Stable Coronary Artery Disease: The Task Force on the Management of Stable Coronary Artery Disease of the European Society of Cardiology. Eur. Heart J. 2013, 34, 2949–3003. [Google Scholar] [CrossRef] [PubMed]
- Hao, G.; Wang, X.; Chen, Z.; Zhang, L.; Zhang, Y.; Wei, B.; Zheng, C.; Kang, Y.; Jiang, L.; Zhu, Z.; et al. Prevalence of Heart Failure and Left Ventricular Dysfunction in China: The China Hypertension Survey, 2012–2015. Eur. J. Heart Fail. 2019, 21, 1329–1337. [Google Scholar] [CrossRef] [PubMed]
- Snoek, J.A.; Prescott, E.I.; van der Velde, A.E.; Eijsvogels, T.M.H.; Mikkelsen, N.; Prins, L.F.; Bruins, W.; Meindersma, E.; González-Juanatey, J.R.; Peña-Gil, C.; et al. Effectiveness of Home-Based Mobile Guided Cardiac Rehabilitation as Alternative Strategy for Nonparticipation in Clinic-Based Cardiac Rehabilitation Among Elderly Patients in Europe: A Randomized Clinical Trial. JAMA Cardiol. 2021, 6, 463–468. [Google Scholar] [CrossRef] [PubMed]
- Ma, L.-Y.; Chen, W.-W.; Gao, R.-L.; Liu, L.-S.; Zhu, M.-L.; Wang, Y.-J.; Wu, Z.-S.; Li, H.-J.; Gu, D.-F.; Yang, Y.-J.; et al. China Cardiovascular Diseases Report 2018: An Updated Summary. J. Geriatr. Cardiol. 2020, 17, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Prescott, E.; Eser, P.; Mikkelsen, N.; Holdgaard, A.; Marcin, T.; Wilhelm, M.; Gil, C.P.; González-Juanatey, J.R.; Moatemri, F.; Iliou, M.C.; et al. Cardiac Rehabilitation of Elderly Patients in Eight Rehabilitation Units in Western Europe: Outcome Data from the EU-CaRE Multi-Centre Observational Study. Eur. J. Prev. Cardiol. 2020, 27, 1716–1729. [Google Scholar] [CrossRef]
- Mampuya, W.M. Cardiac Rehabilitation Past, Present and Future: An Overview. Cardiovasc. Diagn. Ther. 2012, 2, 38–49. [Google Scholar]
- Sibilitz, K.L.; Berg, S.K.; Rasmussen, T.B.; Risom, S.S.; Thygesen, L.C.; Tang, L.; Hansen, T.B.; Johansen, P.P.; Gluud, C.; Lindschou, J.; et al. Cardiac Rehabilitation Increases Physical Capacity but Not Mental Health after Heart Valve Surgery: A Randomised Clinical Trial. Heart 2016, 102, 1995–2003. [Google Scholar] [CrossRef]
- Pratesi, A.; Baldasseroni, S.; Burgisser, C.; Orso, F.; Barucci, R.; Silverii, M.V.; Venturini, S.; Ungar, A.; Marchionni, N.; Fattirolli, F. Long-Term Functional Outcomes after Cardiac Rehabilitation in Older Patients. Data from the Cardiac Rehabilitation in Advanced AGE: EXercise TRaining and Active Follow-up (CR-AGE EXTRA) Randomised Study. Eur. J. Prev. Cardiol. 2019, 26, 1470–1478. [Google Scholar] [CrossRef]
- Yang, X.; Li, Y.; Ren, X.; Xiong, X.; Wu, L.; Li, J.; Wang, J.; Gao, Y.; Shang, H.; Xing, Y. Effects of Exercise-Based Cardiac Rehabilitation in Patients after Percutaneous Coronary Intervention: A Meta-Analysis of Randomized Controlled Trials. Sci. Rep. 2017, 7, 44789. [Google Scholar] [CrossRef]
- Chen, Y.-W.; Wang, C.-Y.; Lai, Y.-H.; Liao, Y.-C.; Wen, Y.-K.; Chang, S.-T.; Huang, J.-L.; Wu, T.-J. Home-Based Cardiac Rehabilitation Improves Quality of Life, Aerobic Capacity, and Readmission Rates in Patients with Chronic Heart Failure. Medicine 2018, 97, e9629. [Google Scholar] [CrossRef]
- Campo, G.; Tonet, E.; Chiaranda, G.; Sella, G.; Maietti, E.; Bugani, G.; Vitali, F.; Serenelli, M.; Mazzoni, G.; Ruggiero, R.; et al. Exercise Intervention Improves Quality of Life in Older Adults after Myocardial Infarction: Randomised Clinical Trial. Heart 2020, 106, 1658–1664. [Google Scholar] [CrossRef] [PubMed]
- Hammill, B.G.; Curtis, L.H.; Schulman, K.A.; Whellan, D.J. Relationship Between Cardiac Rehabilitation and Long-Term Risks of Death and Myocardial Infarction Among Elderly Medicare Beneficiaries. Circulation 2010, 121, 63–70. [Google Scholar] [CrossRef]
- Clark, R.A.; Conway, A.; Poulsen, V.; Keech, W.; Tirimacco, R.; Tideman, P. Alternative Models of Cardiac Rehabilitation: A Systematic Review. Eur. J. Prev. Cardiol. 2015, 22, 35–74. [Google Scholar] [CrossRef] [PubMed]
- Kraal, J.J.; Van den Akker-Van Marle, M.E.; Abu-Hanna, A.; Stut, W.; Peek, N.; Kemps, H.M. Clinical and Cost-Effectiveness of Home-Based Cardiac Rehabilitation Compared to Conventional, Centre-Based Cardiac Rehabilitation: Results of the FIT@Home Study. Eur. J. Prev. Cardiol. 2017, 24, 1260–1273. [Google Scholar] [CrossRef] [PubMed]
- Bravo-Escobar, R.; González-Represas, A.; Gómez-González, A.M.; Montiel-Trujillo, A.; Aguilar-Jimenez, R.; Carrasco-Ruíz, R.; Salinas-Sánchez, P. Effectiveness and Safety of a Home-Based Cardiac Rehabilitation Programme of Mixed Surveillance in Patients with Ischemic Heart Disease at Moderate Cardiovascular Risk: A Randomised, Controlled Clinical Trial. BMC Cardiovasc. Disord. 2017, 17, 66. [Google Scholar] [CrossRef] [PubMed]
- Kato, M.; Ogano, M.; Mori, Y.; Kochi, K.; Morimoto, D.; Kito, K.; Green, F.N.; Tsukamoto, T.; Kubo, A.; Takagi, H.; et al. Exercise-Based Cardiac Rehabilitation for Patients with Catheter Ablation for Persistent Atrial Fibrillation: A Randomized Controlled Clinical Trial. Eur. J. Prev. Cardiol. 2019, 26, 1931–1940. [Google Scholar] [CrossRef] [PubMed]
- Villelabeitia-Jaureguizar, K.; Campos, D.V.; Senen, A.B.; Jiménez, V.H.; Bautista, L.R.; Garrido-Lestache, M.E.B.; Chicharro, J.L. Mechanical Efficiency of High versus Moderate Intensity Aerobic Exercise in Coronary Heart Disease Patients: A Randomized Clinical Trial. Cardiol. J. 2019, 26, 130–137. [Google Scholar] [CrossRef]
- Taylor, J.L.; Holland, D.J.; Keating, S.E.; Leveritt, M.D.; Gomersall, S.R.; Rowlands, A.V.; Bailey, T.G.; Coombes, J.S. Short-Term and Long-Term Feasibility, Safety, and Efficacy of High-Intensity Interval Training in Cardiac Rehabilitation: The FITR Heart Study Randomized Clinical Trial. JAMA Cardiol. 2020, 5, 1382–1389. [Google Scholar] [CrossRef]
- Prabhakaran, D.; Chandrasekaran, A.M.; Singh, K.; Mohan, B.; Chattopadhyay, K.; Chadha, D.S.; Negi, P.C.; Bhat, P.; Sadananda, K.S.; Ajay, V.S.; et al. Yoga-Based Cardiac Rehabilitation After Acute Myocardial Infarction. J. Am. Coll. Cardiol. 2020, 75, 1551–1561. [Google Scholar] [CrossRef]
- Chandrasekaran, A.M.; Kinra, S.; Ajay, V.S.; Chattopadhyay, K.; Singh, K.; Singh, K.; Praveen, P.A.; Soni, D.; Devarajan, R.; Kondal, D.; et al. Effectiveness and Cost-Effectiveness of a Yoga-Based Cardiac Rehabilitation (Yoga-CaRe) Program Following Acute Myocardial Infarction: Study Rationale and Design of a Multi-Center Randomized Controlled Trial. Int. J. Cardiol. 2019, 280, 14–18. [Google Scholar] [CrossRef]
- Salmoirago-Blotcher, E.; Wayne, P.M.; Dunsiger, S.; Krol, J.; Breault, C.; Bock, B.C.; Wu, W.; Yeh, G.Y. Tai Chi Is a Promising Exercise Option for Patients with Coronary Heart Disease Declining Cardiac Rehabilitation. JAHA 2017, 6, e006603. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Piña, I.L.; Apstein, C.S.; Balady, G.J.; Belardinelli, R.; Chaitman, B.R.; Duscha, B.D.; Fletcher, B.J.; Fleg, J.L.; Myers, J.N.; Sullivan, M.J. Exercise and Heart Failure: A Statement from the American Heart Association Committee on Exercise, Rehabilitation, and Prevention. Circulation 2003, 107, 1210–1225. [Google Scholar] [CrossRef] [PubMed]
- Donelli da Silveira, A.; Beust de Lima, J.; da Silva Piardi, D.; dos Santos Macedo, D.; Zanini, M.; Nery, R.; Laukkanen, J.A.; Stein, R. High-Intensity Interval Training Is Effective and Superior to Moderate Continuous Training in Patients with Heart Failure with Preserved Ejection Fraction: A Randomized Clinical Trial. Eur. J. Prev. Cardiol. 2020, 27, 1733–1743. [Google Scholar] [CrossRef] [PubMed]
- Song, Y.; Ren, C.; Liu, P.; Tao, L.; Zhao, W.; Gao, W. Effect of Smartphone-Based Telemonitored Exercise Rehabilitation among Patients with Coronary Heart Disease. J. Cardiovasc. Trans. Res. 2020, 13, 659–667. [Google Scholar] [CrossRef]
- Tang, L.H.; Kikkenborg Berg, S.; Christensen, J.; Lawaetz, J.; Doherty, P.; Taylor, R.S.; Langberg, H.; Zwisler, A.-D. Patients’ Preference for Exercise Setting and Its Influence on the Health Benefits Gained from Exercise-Based Cardiac Rehabilitation. Int. J. Cardiol. 2017, 232, 33–39. [Google Scholar] [CrossRef]
- Pelliccia, A.; Sharma, S.; Gati, S.; Bäck, M.; Börjesson, M.; Caselli, S.; Collet, J.-P.; Corrado, D.; Drezner, J.A.; Halle, M.; et al. 2020 ESC Guidelines on Sports Cardiology and Exercise in Patients with Cardiovascular Disease. Eur. Heart J. 2021, 42, 17–96. [Google Scholar] [CrossRef]
- Price, K.J.; Gordon, B.A.; Bird, S.R.; Benson, A.C. A Review of Guidelines for Cardiac Rehabilitation Exercise Programmes: Is There an International Consensus? Eur. J. Prev. Cardiol. 2016, 23, 1715–1733. [Google Scholar] [CrossRef]
- Reibis, R.; Salzwedel, A.; Buhlert, H.; Wegscheider, K.; Eichler, S.; Völler, H. Impact of Training Methods and Patient Characteristics on Exercise Capacity in Patients in Cardiovascular Rehabilitation. Eur. J. Prev. Cardiol. 2016, 23, 452–459. [Google Scholar] [CrossRef]
- Boidin, M.; Trachsel, L.-D.; Nigam, A.; Juneau, M.; Tremblay, J.; Gayda, M. Non-Linear Is Not Superior to Linear Aerobic Training Periodization in Coronary Heart Disease Patients. Eur. J. Prev. Cardiol. 2020, 27, 1691–1698. [Google Scholar] [CrossRef]
- Hollenberg, M.; Tager, I.B. Oxygen Uptake Efficiency Slope: An Index of Exercise Performance and Cardiopulmonary Reserve Requiring Only Submaximal Exercise. J. Am. Coll. Cardiol. 2000, 36, 194–201. [Google Scholar] [CrossRef]
- Marchionni, N.; Fattirolli, F.; Fumagalli, S.; Oldridge, N.; Del Lungo, F.; Morosi, L.; Burgisser, C.; Masotti, G. Improved Exercise Tolerance and Quality of Life with Cardiac Rehabilitation of Older Patients After Myocardial Infarction: Results of a Randomized, Controlled Trial. Circulation 2003, 107, 2201–2206. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Campo, G.; Tonet, E.; Chiaranda, G.; Sella, G.; Maietti, E.; Mazzoni, G.; Biscaglia, S.; Pavasini, R.; Myers, J.; Grazzi, G. Exercise Intervention to Improve Functional Capacity in Older Adults After Acute Coronary Syndrome. J. Am. Coll. Cardiol. 2019, 74, 2948–2950. [Google Scholar] [CrossRef] [PubMed]
- Lachman, S.; Boekholdt, S.M.; Luben, R.N.; Sharp, S.J.; Brage, S.; Khaw, K.-T.; Peters, R.J.; Wareham, N.J. Impact of Physical Activity on the Risk of Cardiovascular Disease in Middle-Aged and Older Adults: EPIC Norfolk Prospective Population Study. Eur. J. Prev. Cardiol. 2018, 25, 200–208. [Google Scholar] [CrossRef] [PubMed]




| Characteristics | Normal |
|---|---|
| Sex (Male) | 75 (80.65%) |
| Mean age (years) | 53.03 (12.02) |
| Mean body mass index (kg/m2) | |
| <18.5 | 3 (3.22%) |
| 18.5~24.0 | 18 (19.35%) |
| 24.0~28.0 | 45 (48.39%) |
| 28.0 | 27 (29.03%) |
| Coronary Heart Disease (%) | 72 (77.42%) |
| Old Myocardial Infarction (%) | 47 (50.54%) |
| Arrhythmias (%) | 21 (22.58%) |
| Heart Valve disease (%) | 7 (7.53%) |
| Hypertension (%) | 44 (47.31%) |
| Diabetes (%) | 17 (18.28%) |
| Percutaneous Coronary Intervention (%) | 41 (44.09%) |
| Coronary Artery Bypass Graft (%) | 14 (15.05%) |
| Overall | 55 year | >55 year | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Before | After | Before vs. After p (t Test) | Before | After | Before vs. After p (t Test) | Before | After | Before vs. After p (t Test) | |||||||
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD | ||||
| Resting State (RS) a | |||||||||||||||
| HR (cpm) | 78.52 | 11.88 | 76.18 | 10.70 | 0.06 | 78.54 | 11.98 | 77.83 | 11.51 | 0.65 | 78.49 | 11.88 | 73.90 | 9.13 | 0.01 * |
| VO2 (mL/min/kg) | 4.33 | 1.18 | 4.25 | 1.28 | 0.57 | 4.20 | 0.95 | 4.12 | 1.10 | 0.63 | 4.52 | 1.43 | 4.42 | 1.50 | 0.73 |
| VE (mL/min/kg) | 13.22 | 4.44 | 13.11 | 4.53 | 0.84 | 13.43 | 4.71 | 13.50 | 4.86 | 0.91 | 12.92 | 4.06 | 12.56 | 4.02 | 0.68 |
| RER | 0.81 | 0.07 | 0.82 | 0.08 | 0.11 | 0.80 | 0.06 | 0.82 | 0.07 | 0.07 | 0.82 | 0.07 | 0.83 | 0.09 | 0.63 |
| Anaerobic Threshold (AT) b | |||||||||||||||
| HR (cpm) | 104.03 | 15.55 | 105.81 | 14.04 | 0.21 | 105.19 | 14.76 | 108.19 | 14.38 | 0.10 | 102.44 | 16.65 | 102.51 | 13.03 | 0.97 |
| VO2 (mL/min/kg) | 11.16 | 2.91 | 12.85 | 3.17 | 0.00 ** | 11.58 | 2.64 | 13.54 | 3.25 | 0.00 ** | 10.58 | 3.19 | 11.90 | 2.81 | 0.00 ** |
| VE (mL/min/kg) | 28.87 | 7.26 | 32.42 | 8.50 | 0.00 ** | 30.59 | 7.46 | 34.02 | 8.51 | 0.01 * | 26.49 | 6.33 | 30.21 | 8.07 | 0.00 ** |
| RER | 0.93 | 0.06 | 0.95 | 0.05 | 0.00 ** | 0.94 | 0.05 | 0.95 | 0.04 | 0.02 * | 0.92 | 0.06 | 0.94 | 0.05 | 0.00 ** |
| Slope | |||||||||||||||
| VE/VCO2 | 29.94 | 5.18 | 29.69 | 5.42 | 0.58 | 28.36 | 3.33 | 28.17 | 3.69 | 0.61 | 32.12 | 6.40 | 31.80 | 6.65 | 0.56 |
| OUES | 1426.75 | 346.30 | 1547.19 | 403.49 | 0.00 ** | 1531.19 | 265.11 | 1706.60 | 363.39 | 0.00 ** | 1282.14 | 394.15 | 1326.47 | 351.94 | 0.22 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ma, M.; Zhang, B.; Yan, X.; Ji, X.; Qin, D.; Pu, C.; Zhao, J.; Zhang, Q.; Lowis, H.; Li, T. Adaptive Posture-Balance Cardiac Rehabilitation Exercise Significantly Improved Physical Tolerance in Patients with Cardiovascular Diseases. J. Clin. Med. 2022, 11, 5345. https://doi.org/10.3390/jcm11185345
Ma M, Zhang B, Yan X, Ji X, Qin D, Pu C, Zhao J, Zhang Q, Lowis H, Li T. Adaptive Posture-Balance Cardiac Rehabilitation Exercise Significantly Improved Physical Tolerance in Patients with Cardiovascular Diseases. Journal of Clinical Medicine. 2022; 11(18):5345. https://doi.org/10.3390/jcm11185345
Chicago/Turabian StyleMa, Mei, Bowen Zhang, Xinxin Yan, Xiang Ji, Deyu Qin, Chaodong Pu, Jingxiang Zhao, Qian Zhang, Heinz Lowis, and Ting Li. 2022. "Adaptive Posture-Balance Cardiac Rehabilitation Exercise Significantly Improved Physical Tolerance in Patients with Cardiovascular Diseases" Journal of Clinical Medicine 11, no. 18: 5345. https://doi.org/10.3390/jcm11185345
APA StyleMa, M., Zhang, B., Yan, X., Ji, X., Qin, D., Pu, C., Zhao, J., Zhang, Q., Lowis, H., & Li, T. (2022). Adaptive Posture-Balance Cardiac Rehabilitation Exercise Significantly Improved Physical Tolerance in Patients with Cardiovascular Diseases. Journal of Clinical Medicine, 11(18), 5345. https://doi.org/10.3390/jcm11185345







