Effectiveness of High-Intensity Laser Therapy Plus Ultrasound-Guided Peritendinous Hyaluronic Acid Compared to Therapeutic Exercise for Patients with Lateral Elbow Tendinopathy
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Population
2.3. Outcomes
2.4. Interventions
2.4.1. HILT Plus Hyaluronic Acid (HILT + Hy-A) Group
2.4.2. Therapeutic Exercise Group
2.4.3. Treatments-Related Adverse Events
2.5. Sample Size
2.6. Statistical Analysis
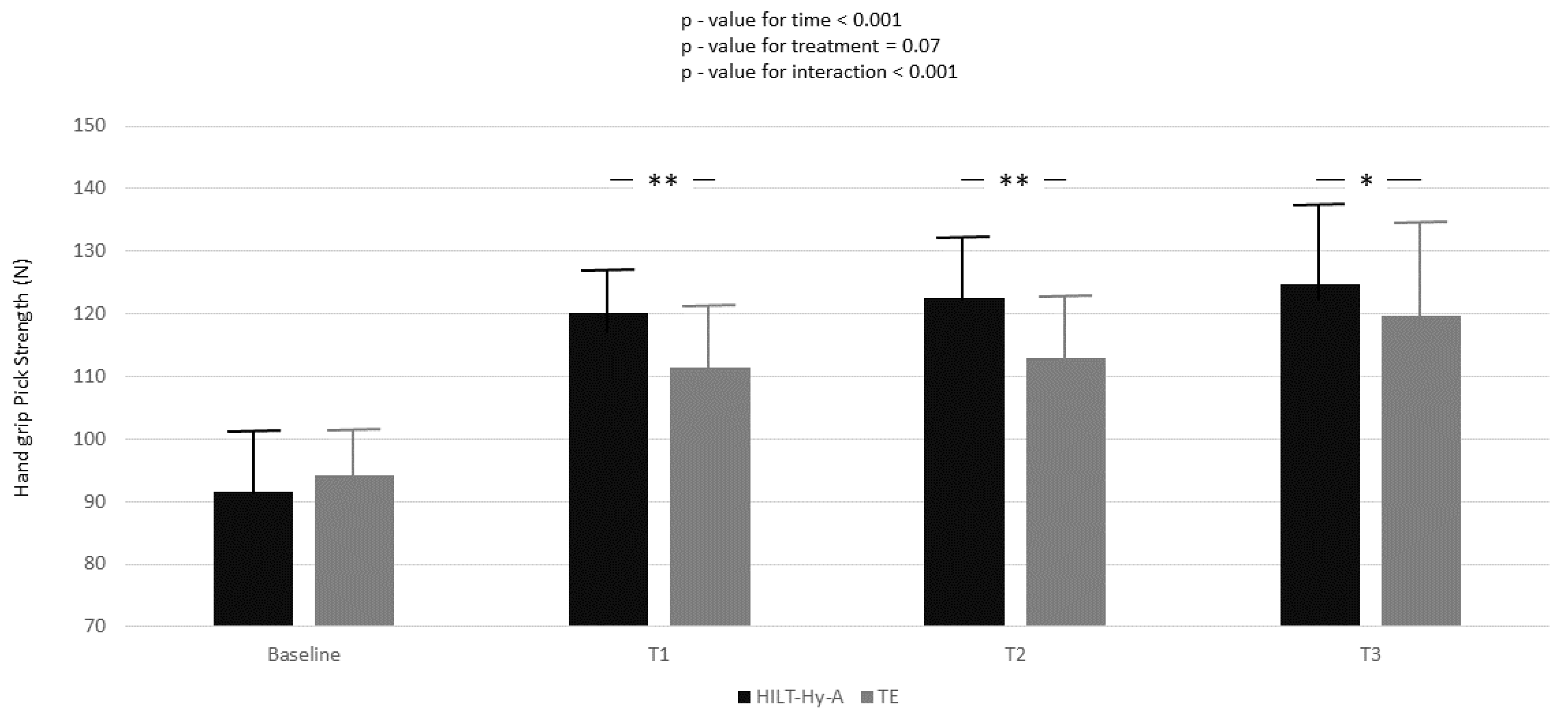
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Cutts, S.; Gangoo, S.; Modi, N.; Pasapula, C. Tennis elbow: A clinical review article. J. Orthop. 2019, 17, 203–207. [Google Scholar] [CrossRef]
- Descatha, A.; Albo, F.; Leclerc, A.; Carton, M.; Godeau, D.; Roquelaure, Y.; Petit, A.; Aublet-Cuvelier, A. Lateral Epicondylitis and Physical Exposure at Work? A Review of Prospective Studies and Meta-Analysis. Arthritis Care Res. 2016, 68, 1681–1687. [Google Scholar] [CrossRef] [PubMed]
- Fahmy, F.S.; ElAttar, M.; Salem, H.F. Hand-Grip Strength and Return to Heavy Manual Work at a Mean 5-Year Follow-up After Arthroscopic Release of Recalcitrant Lateral Epicondylitis. Orthop. J. Sport. Med 2022, 10, 23259671221078586. [Google Scholar] [CrossRef] [PubMed]
- Kheiran, A.; Pandey, A.; Pandey, R. Common tendinopathies around the elbow; what does current evidence say? J. Clin. Orthop. Trauma 2021, 19, 216–223. [Google Scholar] [CrossRef] [PubMed]
- Karabinov, V.; Georgiev, G.P. Lateral epicondylitis: New trends and challenges in treatment. World J. Orthop. 2022, 13, 354–364. [Google Scholar] [CrossRef]
- Stratford, P.W.; Levy, D.R. Assessing valid change over time in patients with lateral epicondylitis at the elbow. Clin. J. Sport Med. 1994, 4, 88–91. [Google Scholar] [CrossRef]
- Ikonen, J.; Lähdeoja, T.; Ardern, C.L.; Buchbinder, R.; Reito, A.; Karjalainen, T. Persistent Tennis Elbow Symptoms Have Little Prognostic Value: A Systematic Review and Meta-analysis. Clin. Orthop. Relat. Res 2022, 480, 647–660. [Google Scholar] [CrossRef]
- Lian, J.; Mohamadi, A.; Chan, J.J.; Hanna, P.; Hemmati, D.; Lechtig, A.; Nazarian, A. Comparative Efficacy and Safety of Nonsurgical Treatment Options for Enthesopathy of the Extensor Carpi Radialis Brevis: A Systematic Review and Meta-analysis of Randomized Placebo-Controlled Trials. Am. J. Sports Med. 2019, 47, 3019–3029. [Google Scholar] [CrossRef]
- de Sire, A.; Lippi, L.; Mezian, K.; Calafiore, D.; Pellegrino, R.; Mascaro, G.; Cisari, C.; Invernizzi, M. Ultrasound-guided platelet-rich-plasma injections for reducing sacroiliac joint pain: A paradigmatic case report and literature review. J. Back Musculoskelet. Rehabil. 2022, 35, 977–982. [Google Scholar] [CrossRef]
- Sanders, T.L.; Maradit Kremers, H.; Bryan, A.J.; Ransom, J.E.; Smith, J.; Morrey, B.F. The epidemiology and health care burden of tennis elbow: A population-based study. Am. J. Sports Med. 2015, 43, 1066–1071. [Google Scholar] [CrossRef]
- Landesa-Piñeiro, L.; Leirós-Rodríguez, R. Physiotherapy treatment of lateral epicondylitis: A systematic review. J. Back Musculoskelet. Rehabil. 2022, 35, 463–477. [Google Scholar] [CrossRef] [PubMed]
- Kachanathu, S.J.; Alenazi, A.M.; Hafez, A.R.; Algarni, A.D.; Alsubiheen, A.M. Comparison of the effects of short-duration wrist joint splinting combined with physical therapy and physical therapy alone on the management of patients with lateral epicondylitis. Eur. J. Phys. Rehabil. Med. 2019, 55, 488–493. [Google Scholar] [CrossRef] [PubMed]
- Ahmad, M.A.; Mohamad, M.S.; Yusof, A. Effects of low-level and high-intensity laser therapy as adjunctive to rehabilitation exercise on pain, stiffness and function in knee osteoarthritis: A systematic review and meta-analysis. Physiotherapy 2022, 114, 85–95. [Google Scholar] [CrossRef]
- Pellegrino, R.; Brindisino, F.; Barassi, G.; Sparvieri, E.; DI Iorio, A.; de Sire, A.; Ruosi, C. Combined ultrasound guided peritendinous hyaluronic acid (500–730 Kda) injection with extracorporeal shock waves therapy vs. extracorporeal shock waves therapy-only in the treatment of shoulder pain due to rotator cuff tendinopathy. A randomized clinical. J. Sports Med. Phys. Fitness 2022, 62, 1211–1218. [Google Scholar] [CrossRef]
- Urdiales-Gálvez, F.; Martín-Sánchez, S.; Maíz-Jiménez, M.; Castellano-Miralla, A.; Lionetti-Leone, L. Concomitant Use of Hyaluronic Acid and Laserin Facial Rejuvenation. Aesthetic Plast. Surg 2019, 43, 1061. [Google Scholar] [CrossRef] [PubMed]
- Oliva, F.; Marsilio, E.; Asparago, G.; Frizziero, A.; Berardi, A.C.; Maffulli, N. The Impact of Hyaluronic Acid on Tendon Physiology and Its Clinical Application in Tendinopathies. Cells 2021, 10, 3081. [Google Scholar] [CrossRef]
- Crimaldi, S.; Liguori, S.; Tamburrino, P.; Moretti, A.; Paoletta, M.; Toro, G.; Iolascon, G. The Role of Hyaluronic Acid in Sport-Related Tendinopathies: A Narrative Review. Medicina 2021, 57, 1088–2021. [Google Scholar] [CrossRef]
- Cuschieri, S. The STROBE guidelines. Saudi J. Anaesth. 2019, 13, 31–34. [Google Scholar] [CrossRef]
- Karanasios, S.; Korakakis, V.; Moutzouri, M.; Drakonaki, E.; Koci, K.; Pantazopoulou, V.; Tsepis, E.; Gioftsos, G. Diagnostic accuracy of examination tests for lateral elbow tendinopathy (LET)—A systematic review. J. Hand Ther. 2021, in press. [Google Scholar] [CrossRef]
- Cacchio, A.; Necozione, S.; MacDermid, J.C.; Rompe, J.D.; Maffulli, N.; di Orio, F.; Santilli, V.; Paoloni, M. Cross-cultural adaptation and measurement properties of the italian version of the Patient-Rated Tennis Elbow Evaluation (PRTEE) questionnaire. Phys. Ther. 2012, 92, 1036–1045. [Google Scholar] [CrossRef]
- Pahor, M.; Chrischilles, E.A.; Guralnik, J.M.; Brown, S.L.; Wallace, R.B.; Carbonin, P. Drug data coding and analysis in epidemiologic studies. Eur. J. Epidemiol. 1994, 10, 405–411. [Google Scholar] [CrossRef]
- Stroup, W.W. Generalized Linear Mixed Models Modern Concepts, Methods and Applications; Taylor & Francis Group: Boca Raton, FL, USA, 2013. [Google Scholar]
- Singer, J.D. Using SAS PROC MIXED to Fit Multilevel Models, Hierarchical Models, and Individual Growth Models. J. Educ. Behav. Stat. 1998, 23, 323–355. [Google Scholar] [CrossRef]
- Millar, N.L.; Silbernagel, K.G.; Thorborg, K.; Kirwan, P.D.; Galatz, L.M.; Abrams, G.D.; Murrell, G.A.C.; McInnes, I.B.; Rodeo, S.A. Tendinopathy. Nat. Rev. Dis. Prim. 2021, 7, 1. [Google Scholar] [CrossRef] [PubMed]
- Frizziero, A.; Salamanna, F.; Della Bella, E.; Vittadini, F.; Gasparre, G.; Aldini, N.N.; Masiero, S.; Fini, M. The Role of Detraining in Tendon Mechanobiology. Front. Aging Neurosci. 2016, 8, 43. [Google Scholar] [CrossRef] [PubMed]
- Karanasios, S.; Korakakis, V.; Whiteley, R.; Vasilogeorgis, I.; Woodbridge, S.; Gioftsos, G. Exercise interventions in lateral elbow tendinopathy have better outcomes than passive interventions, but the effects are small: A systematic review and meta-analysis of 2123 subjects in 30 trials. Br. J. Sports Med. 2021, 55, 477–485. [Google Scholar] [CrossRef] [PubMed]
- Chen, Z.; Baker, N.A. Effectiveness of eccentric strengthening in the treatment of lateral elbow tendinopathy: A systematic review with meta-analysis. J. Hand Ther. 2021, 34, 18–28. [Google Scholar] [CrossRef]
- Ryan, C.G.; Gray, H.G.; Newton, M.; Granat, M.H. Pain biology education and exercise classes compared to pain biology education alone for individuals with chronic low back pain: A pilot randomised controlled trial. Man. Ther. 2010, 15, 382–387. [Google Scholar] [CrossRef]
- Yoon, S.Y.; Kim, Y.W.; Shin, I.S.; Kang, S.; Moon, H.I.; Lee, S.C. The Beneficial Effects of Eccentric Exercise in the Management of Lateral Elbow Tendinopathy: A Systematic Review and Meta-Analysis. J. Clin. Med. 2021, 10, 3968. [Google Scholar] [CrossRef]
- Evans, J.P.; Maffulli, N.; Smith, C.; Watts, A.; Valderas, J.; Goodwin, V. Even experts cannot agree on the optimal use of platelet-rich plasma in lateral elbow tendinopathy: An international Delphi study. J. Orthop. Traumatol. 2021, 22, 47. [Google Scholar] [CrossRef]
- Mitsui, Y.; Gotoh, M.; Nakama, K.; Yamada, T.; Higuchi, F.; Nagata, K. Hyaluronic acid inhibits mRNA expression of proinflammatory cytokines and cyclooxygenase-2/prostaglandin E(2) production via CD44 in interleukin-1-stimulated subacromial synovial fibroblasts from patients with rotator cuff disease. J. Orthop. Res. 2008, 26, 1032–1037. [Google Scholar] [CrossRef]
- Cotler, H.B. The Use of Low Level Laser Therapy (LLLT) For Musculoskeletal Pain. MOJ Orthop. Rheumatol. 2015, 2, 188–194. [Google Scholar] [CrossRef]
- Mamais, I.; Papadopoulos, K.; Lamnisos, D.; Stasinopoulos, D. Effectiveness of Low Level Laser Therapy (LLLT) in the treatment of Lateral elbow tendinopathy (LET): An umbrella review. Laser Ther. 2018, 27, 174–186. [Google Scholar] [CrossRef] [PubMed]
- Dundar, U.; Turkmen, U.; Toktas, H.; Ulasli, A.M.; Solak, O. Effectiveness of high-intensity laser therapy and splinting in lateral epicondylitis: A prospective, randomized, controlled study. Lasers Med. Sci. 2015, 30, 1097–1107. [Google Scholar] [CrossRef] [PubMed]
- Akkurt, E.; Kucuksen, S.; Yılmaz, H.; Parlak, S.; Sallı, A.; Karaca, G. Long term effects of high intensity laser therapy in lateral epicondylitis patients. Lasers Med. Sci. 2016, 31, 249–253. [Google Scholar] [CrossRef] [PubMed]


| HILT + Hy-A | TE | p-Value | |
|---|---|---|---|
| 40 | 40 | ||
| Age (year) | 47.3 ± 9.5 | 50.3 ± 8.1 | 0.13 |
| Sex female n (%) | 25 (62.5) | 21 (52.5) | 0.37 |
| Side pain (right) n (%) | 19 (47.5) | 22 (55.0) | 0.50 |
| Weight (kg) | 74.1 ± 6.3 | 74.0 ± 5.5 | 0.97 |
| Height (m) | 1.68 ± 0.1 | 1.69 ± 0.1 | 0.75 |
| BMI (kg/m2) | 26.2 ± 2.3 | 26.1 ± 1.9 | 0.72 |
| White collar n (%) | 14 (35.0) | 16 (40.0) | 0.64 |
| Education | 0.78 | ||
| Junior high school n (%) | 16 (40.0) | 13 (32.5) | |
| High school n (%) | 15 (37.5) | 17 (42.5) | |
| University degree n (%) | 9 (22.5) | 10 (25.0) | |
| Smoke habits (actually) n (%) | 10 (25.0) | 14 (35.0) | 0.33 |
| Hypertension n (%) | 10 (25.0) | 9 (22.5) | 0.79 |
| Cholesterol mmol/L | 184.6 ± 29.7 | 184.0 ± 28.3 | 0.94 |
| Hand grip Peak strength (Nw) | 91.6 ± 12.2 | 94.1 ± 7.1 | 0.28 |
| Hand grip Mean strength (Nw) | 77.5 ± 10.0 | 77.7 ± 7.0 | 0.96 |
| PRTEE total score | 64.2 ± 6.2 | 63.3 ± 4.7 | 0.43 |
| PRTEE Pain score | 29.6 ± 3.4 | 29.5 ± 3.2 | 0.87 |
| PRTEE Specific activities | 39.7 ± 4.9 | 38.6 ± 3.4 | 0.28 |
| PRTEE Usual activities | 29.6 ± 2.8 | 28.9 ± 2.5 | 0.27 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pellegrino, R.; Paolucci, T.; Brindisino, F.; Mondardini, P.; Di Iorio, A.; Moretti, A.; Iolascon, G. Effectiveness of High-Intensity Laser Therapy Plus Ultrasound-Guided Peritendinous Hyaluronic Acid Compared to Therapeutic Exercise for Patients with Lateral Elbow Tendinopathy. J. Clin. Med. 2022, 11, 5492. https://doi.org/10.3390/jcm11195492
Pellegrino R, Paolucci T, Brindisino F, Mondardini P, Di Iorio A, Moretti A, Iolascon G. Effectiveness of High-Intensity Laser Therapy Plus Ultrasound-Guided Peritendinous Hyaluronic Acid Compared to Therapeutic Exercise for Patients with Lateral Elbow Tendinopathy. Journal of Clinical Medicine. 2022; 11(19):5492. https://doi.org/10.3390/jcm11195492
Chicago/Turabian StylePellegrino, Raffaello, Teresa Paolucci, Fabrizio Brindisino, Paolo Mondardini, Angelo Di Iorio, Antimo Moretti, and Giovanni Iolascon. 2022. "Effectiveness of High-Intensity Laser Therapy Plus Ultrasound-Guided Peritendinous Hyaluronic Acid Compared to Therapeutic Exercise for Patients with Lateral Elbow Tendinopathy" Journal of Clinical Medicine 11, no. 19: 5492. https://doi.org/10.3390/jcm11195492
APA StylePellegrino, R., Paolucci, T., Brindisino, F., Mondardini, P., Di Iorio, A., Moretti, A., & Iolascon, G. (2022). Effectiveness of High-Intensity Laser Therapy Plus Ultrasound-Guided Peritendinous Hyaluronic Acid Compared to Therapeutic Exercise for Patients with Lateral Elbow Tendinopathy. Journal of Clinical Medicine, 11(19), 5492. https://doi.org/10.3390/jcm11195492









