Extraperitoneal Laparoscopic Approach in Inguinal Hernia—The Ideal Solution?
Abstract
1. Introduction
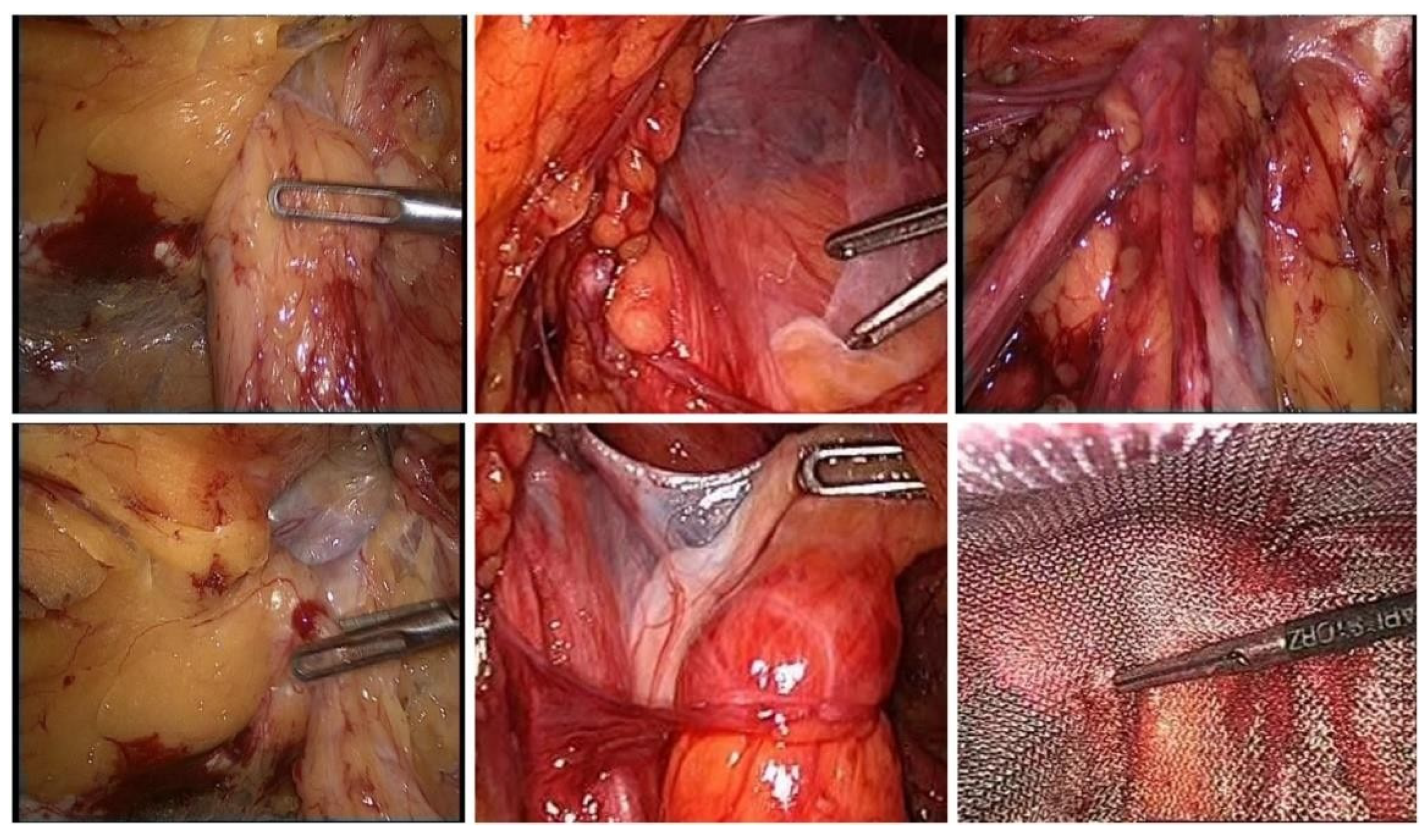
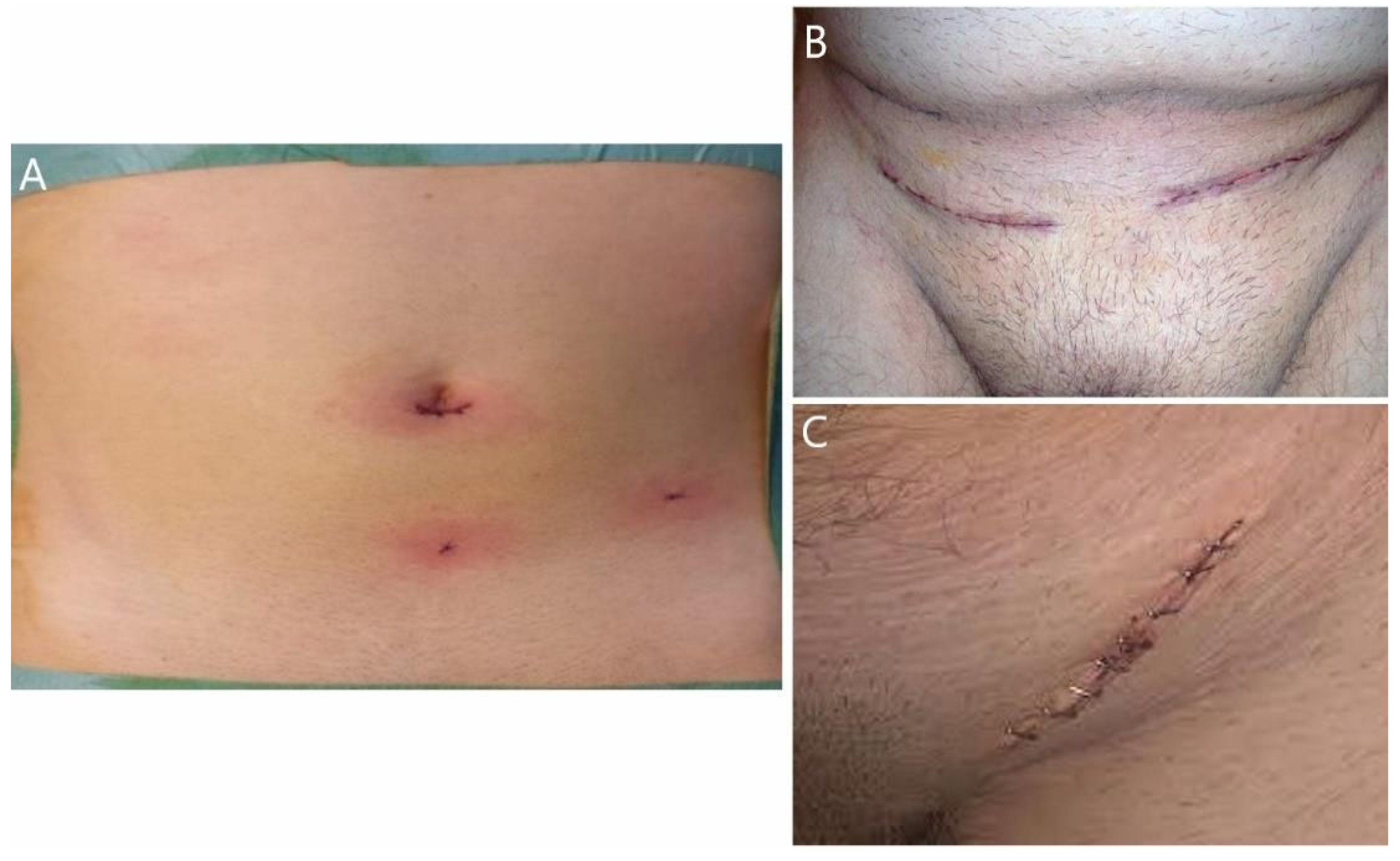
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- A Reiner, M.; Bresnahan, E.R. Laparoscopic Total Extraperitoneal Hernia Repair Outcomes. J. Soc. Laparoendosc. Surg. 2016, 20, e2016.00043. [Google Scholar] [CrossRef] [PubMed]
- Bittner, R.; Schwarz, J. Inguinal hernia repair: Current surgical techniques. Langenbecks Arch. Surg. 2012, 397, 271–282. [Google Scholar] [CrossRef] [PubMed]
- Bobo, Z.; Nan, W.; Qin, Q.; Tao, W.; Jianguo, L.; Xianli, H. Meta-analysis of randomized controlled trials comparing Lichtenstein and totally extraperitoneal laparoscopic hernioplasty in treatment of inguinal hernias. J. Surg. Res. 2014, 192, 409–420. [Google Scholar] [CrossRef] [PubMed]
- Köckerling, F.; Bittner, R.; Jacob, D.A.; Seidelmann, L.; Keller, T.; Adolf, D.; Kraft, B.; Kuthe, A. TEP versus TAPP: Comparison of the perioperative outcome in 17,587 patients with a primary unilateral inguinal hernia. Surg. Endosc. 2015, 29, 3750–3760. [Google Scholar] [CrossRef] [PubMed]
- Bittner, R.; Arregui, M.E.; Bisgaard, T.; Dudai, M.; Ferzli, G.S.; Fitzgibbons, R.J.; Fortelny, R.H.; Klinge, U.; Kockerling, F.; Kuhry, E.; et al. Guidelines for laparoscopic (TAPP) and endoscopic (TEP) treatment of inguinal Hernia [International Endohernia Society (IEHS)]. Surg. Endosc. 2011, 25, 2773–2843. [Google Scholar] [CrossRef] [PubMed]
- Poelman, M.M.; Heuvel, B.V.D.; Deelder, J.D.; Abis, G.S.A.; Beudeker, N.; Bittner, R.R.; Campanelli, G.; van Dam, D.; Dwars, B.J.; Eker, H.H.; et al. EAES Consensus Development Conference on endoscopic repair of groin hernias. Surg. Endosc. 2013, 27, 3505–3519. [Google Scholar] [CrossRef]
- Simons, M.P.; Aufenacker, T.; Bay-Nielsen, M.; Bouillot, J.L.; Campanelli, G.; Conze, J.; De Lange, D.; Fortelny, R.; Heikkinen, T.; Kingsnorth, A.; et al. European Hernia Society guidelines on the treatment of inguinal hernia in adult patients. Hernia 2009, 13, 343–403. [Google Scholar] [CrossRef] [PubMed]
- Basile, F.; Biondi, A.; Donati, M. Surgical approach to abdominal wall defects: History and new trends. Int. J. Surg. 2013, 11 (Suppl. S1), S20–S23. [Google Scholar] [CrossRef]
- Kouhia, S.; Vironen, J.; Hakala, T.; Paajanen, H. Open Mesh Repair for Inguinal Hernia is Safer than Laparoscopic Repair or Open Non-mesh Repair: A Nationwide Registry Study of Complications. World J. Surg. 2015, 39, 1878–1884. [Google Scholar] [CrossRef] [PubMed]
- Shah, N.S.; Fullwood, C.; Siriwardena, A.K.; Sheen, A.J. Mesh Fixation at Laparoscopic Inguinal Hernia Repair: A Meta-Analysis Comparing Tissue Glue and Tack Fixation. World J. Surg. 2014, 38, 2558–2570. [Google Scholar] [CrossRef] [PubMed]
- Eker, H.H.; Langeveld, H.R.; Klitsie, P.J.; van’t Riet, M.; Stassen, L.P.; Weidema, W.F.; Steyerberg, E.W.; Lange, J.F.; Bonjer, H.J.; Jeekel, J. Randomized clinical trial of total extraperitoneal inguinal hernioplasty vs Lichten-stein repair: A long-term follow-up study. Arch. Surg. 2012, 147, 256–260. [Google Scholar] [CrossRef]
- O’Reilly, E.A.; Burke, J.P.; O’Connell, P.R. A Meta-Analysis of Surgical Morbidity and Recurrence after Laparoscopic and Open Repair of Primary Unilateral Inguinal Hernia. Ann. Surg. 2012, 255, 846–853, Erratum in: Ann. Surg. 2012, 256, 393. [Google Scholar] [CrossRef]
- Tolver, M.A.; Rosenberg, J.; Bisgaard, T. Early pain after laparoscopic inguinal hernia repair. A qualitative systematic review. Acta Anaesthesiol. Scand. 2012, 56, 549–557. [Google Scholar] [CrossRef] [PubMed]
- Köckerling, F.; Koch, A.; Adolf, D.; Keller, T.; Lorenz, R.; Fortelny, R.H.; Schug-Pass, C. Has Shouldice Repair in a Selected Group of Patients with Inguinal Hernia Comparable Results to Lichtenstein, TEP and TAPP Techniques? World J. Surg. 2018, 42, 2001–2010. [Google Scholar] [CrossRef]
- Shah, M.Y.; Raut, P.; Wilkinson, T.R.V. Agrawal V-Surgical outcames of laparoscopic total extraperitoneal (TEP) inguinal hernia repair compared with Lichtenstein tension free open mesh inguinal hernia reapir: A prospective randomized study. Medicine 2022, 101, e29746. [Google Scholar] [CrossRef] [PubMed]
- Chung, R.S.; Rowland, D.Y. Meta-analyses of randomized controlled trials of laparoscopic vs conventional inguinal hernia repairs. Surg. Endosc. 1999, 13, 689–694. [Google Scholar] [CrossRef]
- Schmedt, C.G.; Sauerland, S.; Bittner, R. Comparison of endoscopic procedures vs Lichtenstein and other open mesh techniques for inguinal hernia repair: A meta-analysis of randomized controlled trials. Surg. Endosc. 2004, 19, 188–199. [Google Scholar] [CrossRef] [PubMed]
- Stoker, D.L.; Spiegelhalter, D.J.; Singh, R.; Wellwood, J.M. Laparoscopic versus open inguinal hernia repair: Randomised prospective trial. Lancet 1994, 343, 1243–1245. [Google Scholar] [CrossRef]
- Salma, U.; Ahmed, I.; Ishtiaq, S.A. comparison of post-operative pain and hospital stay between Lichtenstein‘s repair and laparoscopic transabdominal preperitoneal (TAPP) repair of inguinal hernia. A randomized controlled trial. Pak. J. Med. Sci. 2015, 31, 1062. [Google Scholar] [PubMed]
- Champault, G.G.; Rizk, N.; Catheline, J.M.; Turner, R.; Boutelier, P. Inguinal hernia repair: Totally preperitoneal laparoscopic approach versus Stoppa operation: Randomized trial of 100 cases. Surg. Laparosc. Endosc. Percutaneous Technol. 1997, 7, 445–450. [Google Scholar] [CrossRef]
- Wellwood, J.; Sculpher, M.J.; Stoker, D.; Nicholls, G.J.; Geddes, C.; Whitehead, A.; Singh, R.; Spiegelhalter, D. Randomised controlled trial of laparoscopic versus open mesh repair for inguinal hernia: Outcome and cost. BMJ 1998, 317, 103–110. [Google Scholar] [CrossRef] [PubMed]
- Courtney, C.A.; Duffy, K.; Serpell, M.G.; O’dwyer, P.J. Outcome of patients with severe chronic pain following repair of groin hernia. Br. J. Surg. 2002, 89, 1310–1314. [Google Scholar] [CrossRef] [PubMed]
- Karthikesalingam, A.; Markar, S.R.; Holt, P.J.E.; Praseedom, R.K. Meta-analysis of randomized controlled trials comparing laparoscopic with open mesh repair of recurrent inguinal hernia. Br. J. Surg. 2010, 97, 4–11. [Google Scholar] [CrossRef] [PubMed]
- Dhankhar, D.S.; Sharma, N.; Mishra, T.; Kaur, N.; Singh, S.; Gupta, S. Totally extraperitoneal repair under general anesthesia versus Lichtenstein repair under local anesthesia for unilateral inguinal hernia: A prospective randomized controlled trial. Surg. Endosc. 2013, 28, 996–1002. [Google Scholar] [CrossRef] [PubMed]
- Ceith, N.; Urmas, L. Chronic pain after open inguinal hernia repair. Postgrad. Med. 2016, 128, 69–75. [Google Scholar]
- Lal, P.; Kajla, R.; Chander, J.; Saha, R.; Ramteke, V. Randomized controlled study of laparoscopic total extraperitoneal versus open lichtenstein inguinal hernia repair. Surg. Endosc. 2003, 17, 850–856. [Google Scholar] [CrossRef]
- Elmessiry, M.; Gebaly, A. Laparoscopic versus open mesh repair of bilateral primary inguinal hernia: A three-armed Randomized controlled trial. Ann. Med. Surg. 2020, 59, 145–150. [Google Scholar] [CrossRef]
- Aiolfi, A.; Cavalli, M.; Ferraro, S.D.; Manfredini, L.; Bonitta, G.; Bruni, P.G.; Bona, D.; Campanelli, G. Treatment of inguinal hernia: Systematic review and updated network meta-analysis of randomized controlled trials. Ann. Surg. 2021, 274, 954–961. [Google Scholar] [CrossRef]
- Maghrebi, H.; Makni, A.; Sebai, A.; Chebbi, F.; Rebai, W.; Daghfous, A.; Ksantini, R.; Jouini, M.; Kacem, M.; Safta, Z.B. Outcomes of laparoscopic surgery for groin hernia repair: Our experience in Tunisia. Pan. Afr. Med. J. 2018, 29, 43. [Google Scholar]
- Bariş, S.; Nurullah, D.; Murat, G.; Ömer, K. Comparison of early and long term outcomes of open Lichtenstein repair and totally extraperitoneal herniorrhaphy for primary inguinal hernias. Turk. J. Med. Sci. 2019, 49, 38–41. [Google Scholar]
- Swedish Multicentre Trial of Inguinal Hernia Repair by Laparoscopy (SMIL) study group. Chronic pain 5 years after randomized comparison of laparoscopic and Lichtenstein inguinal hernia repair. Swedish Multicentre Trial of Inguinal Hernia Repair by Laparoscopy (SMIL) study group. Br. J. Surg. 2010, 97, 600–608. [Google Scholar] [CrossRef]
- Neumayer, L.; Giobbie-Hurder, A.; Jonasson, O.; Fitzgibbons, R., Jr.; Dunlop, D.; Gibbs, J.; Reda, D.; Henderson, W. Open mesh versus laparoscopic mesh repair of inguinal hernia. Veterans affairs cooperative studies program 456 investigators. N. Engl. J. Med. 2004, 350, 1819–1827. [Google Scholar] [CrossRef] [PubMed]
- Bullen, N.L.; Massey, L.H.; Antoniou, S.A.; Smart, N.J.; Fortelny, R.H. Open versus laparoscopic mesh repair of primary unilateral uncomplicated inguinal hernia: A systematic review with meta-analysis and trial sequential analysis. Hernia 2019, 23, 461–472. [Google Scholar] [CrossRef]
- Feliu, X.; Torres, G.; Pie, J. Preperitoneal repair for recurrent inguinal hernia: Laparoscopic and open approach. Hernia 2003, 8, 113–116. [Google Scholar] [CrossRef]
- Miserez, M.; Peeters, E.; Aufenacker, T.; Bouillot, J.L.; Campanelli, G.; Conze, J.; Fortelny, R.; Heikkinen, T.; Jorgensen, L.N.; Kukleta, J.; et al. Update with level 1 studies of the European Hernia Society guidelines on the treatment of inguinal hernia in adult patients. Hernia 2014, 18, 151–163. [Google Scholar] [CrossRef]
- Saleh, F.; Okrainec, A.; D’Souza, N.; Kwong, J.; Jackson, T.D. Safety of laparoscopic and open approaches for repair of the unilateral primary inguinal hernia: An analysis of short-term outcomes. Am. J. Surg. 2014, 208, 195–201. [Google Scholar] [CrossRef] [PubMed]
- Li, J.; Wang, X.; Feng, X.; Gu, Y.; Tang, R. Comparison of open and laparoscopic preperitoneal repair of groin hernia. Surg. Endosc. 2013, 27, 4702–4710. [Google Scholar] [CrossRef] [PubMed]
- Gass, M.; Banz, V.M.; Rosella, L.; Adamina, M.; Candinas, D.; Güller, U. TAPP or TEP? Population-Based Analysis of Prospective Data on 4,552 Patients Undergoing Endoscopic Inguinal Hernia Repair. World J. Surg. 2012, 36, 2782–2786. [Google Scholar] [CrossRef]
- Antoniou, S.A.; Antoniou, G.A.; Bartsch, D.K.; Fendrich, V.; Koch, O.O.; Pointner, R.; Granderath, F.A. Transabdominal preperitoneal versus totally extraperitoneal repair of inguinal hernia: A meta-analysis of randomized studies. Am. J. Surg. 2013, 206, 245–252.e1. [Google Scholar] [CrossRef]
- Ülker, K.; Aksoy, O.; Çeçen, K.; Ermutlu, C.; Temur, I.; Kiliç, E. CO2 Flow Dynamics of Bladder Injury During Laparoscopy and the Effect of the Content of the Abdominal Viscera During Injury—Experimental Study. Adv. Clin. Exp. Med. 2015, 24, 775–781. [Google Scholar] [CrossRef]
| Type of Surgery | Number of Patients | Percentage |
|---|---|---|
| Unilateral TEP | 243 | 49.2 |
| Bilateral TEP | 226 | 45.84 |
| Unilateral TAPP | 5 | 1.01 |
| Bilateral TAPP | 3 | 0.6 |
| Lichtenstein “tension free”—bilateral | 3 | 0.60 |
| Lichtenstein “tension free”—unilateral | 13 | 2.63 |
| Total | 493 | 100.0 |
| Descriptives | |||
|---|---|---|---|
| Type of Surgery | Statistic | ||
| AGE | TEP unilateral | Mean | 47.63 |
| Median | 44 | ||
| Std. deviation | 14.98 | ||
| TEP bilateral | Mean | 48.83 | |
| Median | 46 | ||
| Std. deviation | 13.959 | ||
| Type of Surgery | Valid | ||
|---|---|---|---|
| n = 152 | % of Elderly Patients | % Total (493) | |
| Unilateral TEP | 46 | 30.2 | 9.33 |
| Bilateral TEP | 82 | 63.2 | 16.6 |
| Unilateral TAPP | 5 | 3.28 | 1.01 |
| Bilateral TAPP | 3 | 1.97 | 0.60 |
| Lichtenstein “tension free“—bilateral | 3 | 1.97 | 0.60 |
| Lichtenstein “tension free“—unilateral | 13 | 8.55 | 2.63 |
| Type of Surgery * Sex Crosstabulation | |||||
|---|---|---|---|---|---|
| Gender | Total (n = 493) | ||||
| Female | Male | ||||
| Type of surgery | Uni/bilateral TEP | Count | 55 | 414 | 469 |
| % of Total | 11.15% | 83.97% | 95.13% | ||
| Uni/bilateral TAPP | Count | 2 | 6 | 8 | |
| % of Total | 0.40% | 1.21% | 1.62% | ||
| Lichtenstein “tension free”—uni/bilateral | Count | 3 | 13 | 16 | |
| % of Total | 0.60% | 2.63% | 37.20% | ||
| Total | Count | 60 | 433 | 493 | |
| % of Total | 12.17% | 87.83% | 100% | ||
| TEP | TAPP | ||
|---|---|---|---|
| Type of hernia | Indirect hernia—NYHUS I,II | 28 | 4 |
| Direct hernia—NYHUS III A | 210 | 2 | |
| Complex hernia—NYHUS IIIB | 205 | 1 | |
| Femoral hernia—NYHUS IIIC | 2 | 0 | |
| Recurrent hernias NYHUS IV | 24 | 1 | |
| Total | 469 | 8 | |
| Reductible | Incarcerated | Strangulated | Total | ||
|---|---|---|---|---|---|
| Surgery type | TEP | 249 | 220 | 0 | 469 |
| TAPP | 3 | 5 | 0 | 8 | |
| Lichtenstein | 3 | 10 | 3 | 16 | |
| Total | 255 (51.72%) | 235 (47.66%) | 3 (0.60%) | 493 | |
| Type of Complication/Surgical Procedure | TEP: 469 | TAPP: 8 | Lichtenstein: 16 | |
|---|---|---|---|---|
| Intraoperative Complications | 0 | 0 | 0 | |
| Immediate postoperative complications | Wound seroma | 3 (0.63%) | 0 | 2 (12.5%) |
| Urinary retention | 29 (6.18%) | 1 (12.5%) | 1 (6.25%) | |
| Wound/inguinal—scrotal hematoma | 3 (0.63%) | 1 (12.5%) | 2 (12.5%) | |
| Intra/extraperitoneal bleeding | 5 (1.07%) | 0 | 0 | |
| Suppurative complications/mesh infection | 0 | 0 | 0 | |
| Pain/transitory neurological disorders | 6 (1.27%) | 0 | 2 (12.5%) | |
| Late postoperative complications | Pain/persistent neurological disorders | 0 | 0 | 1 (6.25%) |
| Recurrences | 2 (0.42%) | 0 | 0 | |
| Total | 48 (10.23%) | 2 (25%) | 8 (50%) | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Barta, B.; Dumitraș, M.; Bucur, Ș.; Giuroiu, C.; Zlotea, R.; Constantin, M.-M.; Mădan, V.; Constantin, T.; Iorga, C.R. Extraperitoneal Laparoscopic Approach in Inguinal Hernia—The Ideal Solution? J. Clin. Med. 2022, 11, 5652. https://doi.org/10.3390/jcm11195652
Barta B, Dumitraș M, Bucur Ș, Giuroiu C, Zlotea R, Constantin M-M, Mădan V, Constantin T, Iorga CR. Extraperitoneal Laparoscopic Approach in Inguinal Hernia—The Ideal Solution? Journal of Clinical Medicine. 2022; 11(19):5652. https://doi.org/10.3390/jcm11195652
Chicago/Turabian StyleBarta, Bogdan, Marina Dumitraș, Ștefana Bucur, Camelia Giuroiu, Raluca Zlotea, Maria-Magdalena Constantin, Victor Mădan, Traian Constantin, and Cristina Raluca Iorga. 2022. "Extraperitoneal Laparoscopic Approach in Inguinal Hernia—The Ideal Solution?" Journal of Clinical Medicine 11, no. 19: 5652. https://doi.org/10.3390/jcm11195652
APA StyleBarta, B., Dumitraș, M., Bucur, Ș., Giuroiu, C., Zlotea, R., Constantin, M.-M., Mădan, V., Constantin, T., & Iorga, C. R. (2022). Extraperitoneal Laparoscopic Approach in Inguinal Hernia—The Ideal Solution? Journal of Clinical Medicine, 11(19), 5652. https://doi.org/10.3390/jcm11195652







