Comparison of Emergency Room Visits and Rehospitalization for Bleeding Complications following Transurethral Procedures for the Treatment of Benign Prostatic Hyperplasia: A Population-Based Retrospective Cohort Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Data Sources
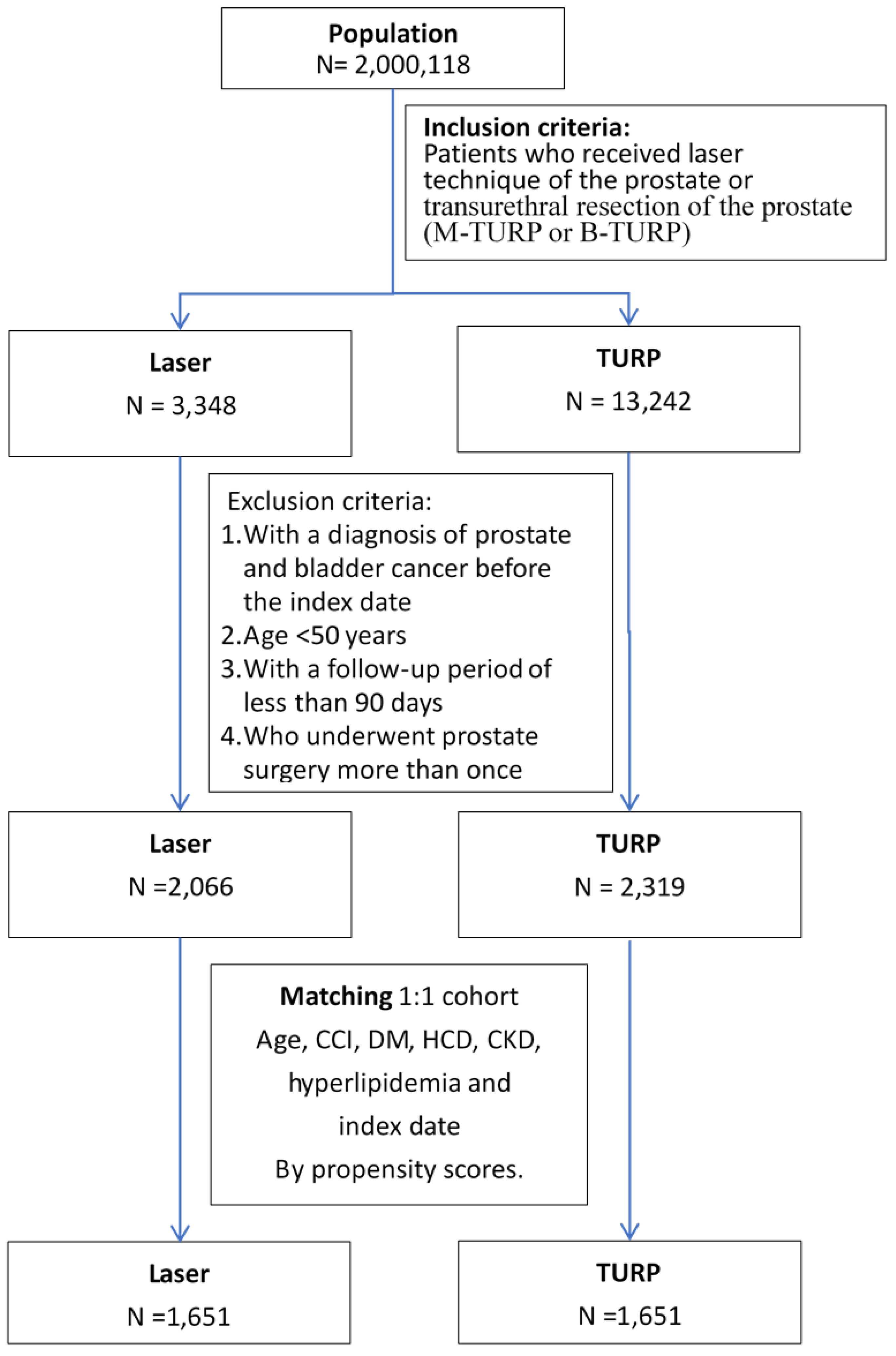
2.2. Study Design
2.3. Surgery Types
2.4. Covariate Assessment
2.5. Main Outcome Measurements
2.5.1. Postoperative Bleeding Complications Leading to ER Visits
2.5.2. Postoperative Bleeding Complications Leading to Rehospitalization
2.6. Statistical Methods
Propensity Score Matching
3. Results
3.1. Patient Characteristics
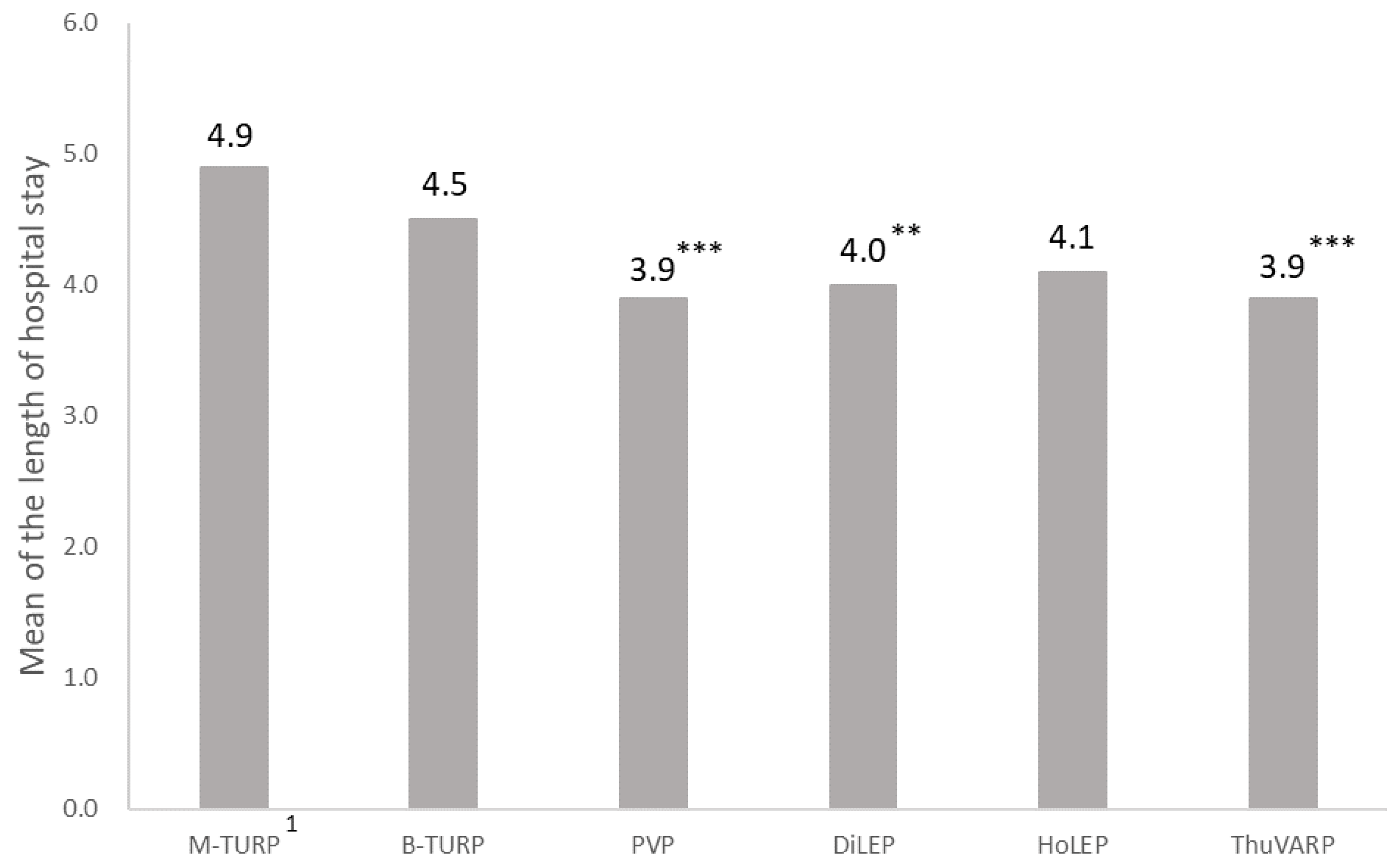
3.2. Comparison of the Length of Hospital Stay among Different Surgery Types
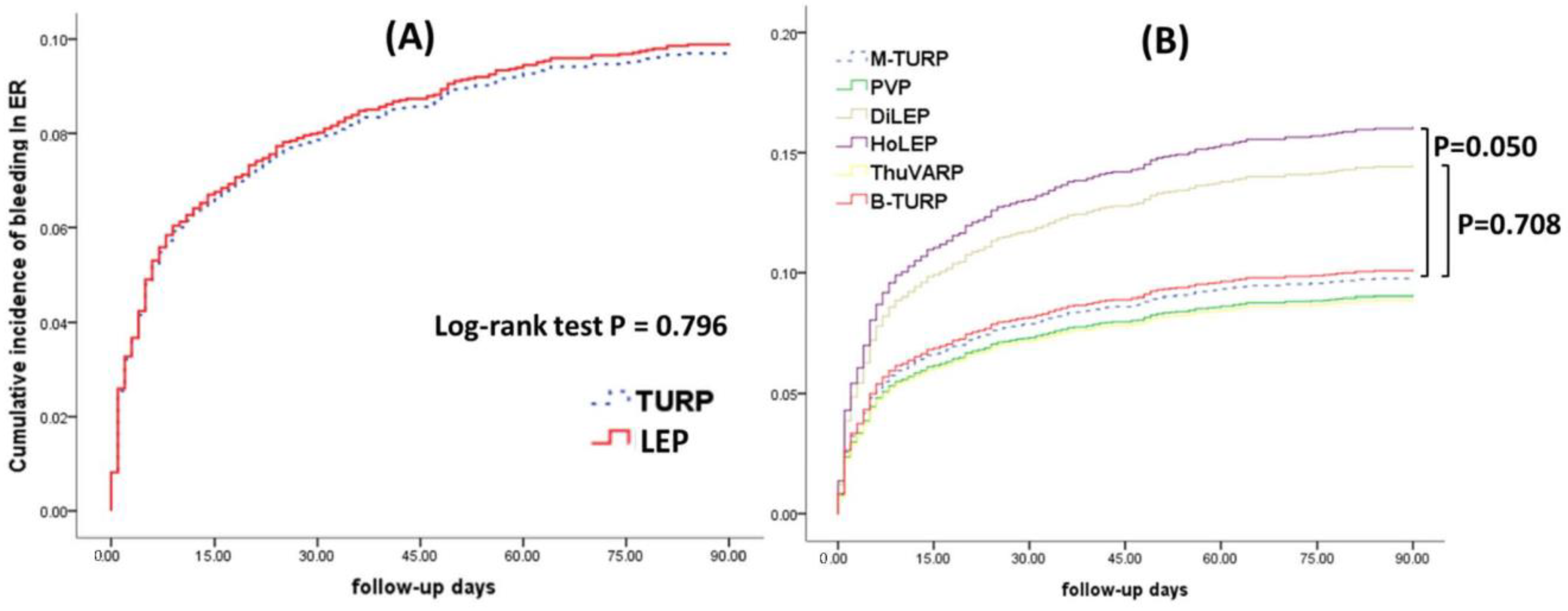
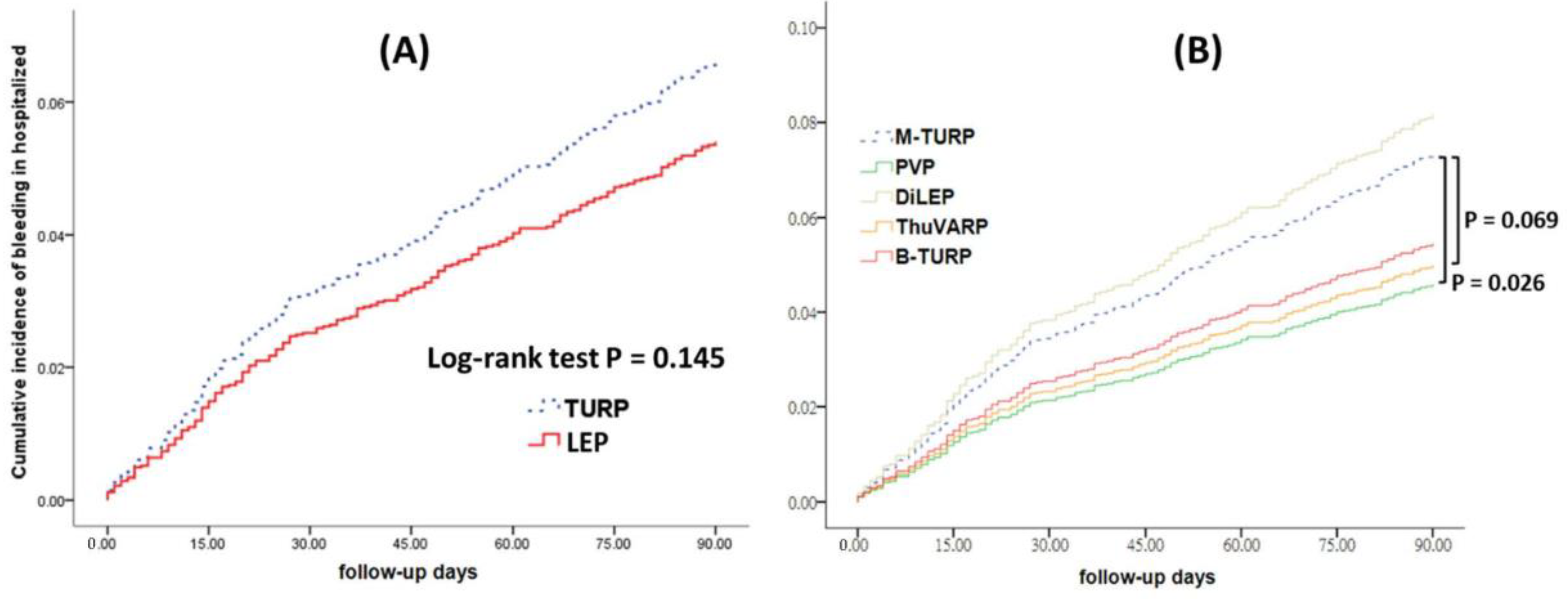
3.3. Comparison of ER Visits with Rehospitalization Due to Postoperative Bleeding
3.4. Effect of Surgery Type on Bleeding Events
3.5. Comparison of Postoperative Bleeding between the Subgroups of Demographics, Comorbidities, and Comedications
4. Discussion
4.1. Participants in Balanced Groups
4.2. Main Results
4.3. Differences in Postoperative Bleeding between Different Surgery Types
4.4. Comparison between the Subgroups of Demographics, Comorbidities, and Comedications
4.5. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| Abbreviation | Meaning |
| ACEIs | angiotensin-converting enzyme inhibitors |
| BPH | benign prostatic hyperplasia |
| B-TURP | bipolar transurethral resection of the prostate |
| CCI | Charlson comorbidity index |
| CI | confidence interval |
| CKD | chronic kidney disease |
| DiLEP | diode laser (980 nm) enucleation of the prostate |
| DM | diabetes mellitus |
| ER | emergency room |
| HCD | hypertensive cardiovascular disease |
| HoLEP | holmium laser enucleation of the prostate |
| HR | hazard ratio |
| ICD-10-CM | International Classification of Diseases, Ten Revision, Clinical Modification |
| ICD-9-CM | International Classification of Diseases, Ninth Revision, Clinical Modification |
| IRB | Institutional Review Board |
| M-TURP | monopolar transurethral resection of the prostate |
| NHI | National Health Insurance |
| NHIRD | National Health Insurance Research Database |
| PSM | propensity score matching |
| PVP | GreenLight photovaporization of the prostate |
| SD | standard deviation |
| ThuVARP | thulium laser vaporesection of the prostate |
| TURP | transurethral resection of the prostate |
References
- McVary, K.T. BPH: Epidemiology and comorbidities. Am. J. Manag. Care 2006, 12 (Suppl. S5), S122–S128. [Google Scholar] [PubMed]
- Kailavasan, M.; Berridge, C.; Athanasiadis, G.; Gkentzis, A.; Rai, B.; Jain, S.; Biyani, C.S.; Nabi, G. Design, implementation, and evaluation of a novel curriculum to teach transurethral resection of the prostate (TURP): A 3-year experience of urology simulation bootcamp course. World J. Urol. 2020, 38, 2899–2906. [Google Scholar] [CrossRef] [PubMed]
- Akman, T.; Binbay, M.; Tekinarslan, E.; Tepeler, A.; Akcay, M.; Ozgor, F.; Ugurlu, M.; Muslumanoglu, A. Effects of bipolar and monopolar transurethral resection of the prostate on urinary and erectile function: A prospective randomized comparative study. BJU Int. 2013, 111, 129–136. [Google Scholar] [CrossRef] [PubMed]
- Chin, P.T.; Bolton, D.M.; Jack, G.; Rashid, P.; Thavaseelan, J.; Yu, R.J.; Roehrborn, C.G.; Woo, H.H. Prostatic urethral lift: Two-year results after treatment for lower urinary tract symptoms secondary to benign prostatic hyperplasia. Urology 2012, 79, 5–11. [Google Scholar] [CrossRef]
- Cornu, J.-N.; Ahyai, S.; Bachmann, A.; de la Rosette, J.; Gilling, P.; Gratzke, C.; McVary, K.; Novara, G.; Woo, H.; Madersbacher, S. A systematic review and meta-analysis of functional outcomes and complications following transurethral procedures for lower urinary tract symptoms resulting from benign prostatic obstruction: An update. Eur. Urol. 2015, 67, 1066–1096. [Google Scholar] [CrossRef]
- Kim, M.; Lee, H.-E.; Oh, S.-J. Technical aspects of holmium laser enucleation of the prostate for benign prostatic hyperplasia. Korean J. Urol. 2013, 54, 570–579. [Google Scholar] [CrossRef]
- Nair, S.M.; Pimentel, M.A.; Gilling, P.J. A review of laser treatment for symptomatic BPH (benign prostatic hyperplasia). Curr. Urol. Rep. 2016, 17, 45. [Google Scholar] [CrossRef]
- Kahokehr, A.A.; Gilling, P.J. Which laser works best for benign prostatic hyperplasia? Curr. Urol. Rep. 2013, 14, 614–619. [Google Scholar] [CrossRef]
- Gravas, S.; Bachmann, A.; Reich, O.; Roehrborn, C.G.; Gilling, P.J.; De La Rosette, J. Critical review of lasers in benign prostatic hyperplasia (BPH). BJU Int. 2011, 107, 1030–1043. [Google Scholar] [CrossRef]
- Hsieh, C.-Y.; Su, C.-C.; Shao, S.-C.; Sung, S.-F.; Lin, S.-J.; Yang, Y.-H.K.; Lai, E.C.-C. Taiwan’s national health insurance research database: Past and future. Clin. Epidemiol. 2019, 11, 349. [Google Scholar] [CrossRef]
- Hsiao, F.-Y.; Yang, C.-L.; Huang, Y.-T.; Huang, W.-F. Using Taiwan’s national health insurance research databases for pharmacoepidemiology research. J. Food Drug Analysis. 2007, 15, 7. [Google Scholar] [CrossRef]
- Hsu, M.C.; Wang, C.C.; Huang, L.Y.; Lin, C.Y.; Lin, F.J.; Toh, S. Effect of ICD-9-CM to ICD-10-CM coding system transition on identification of common conditions: An interrupted time series analysis. Pharmacoepidemiol. Drug Safety. 2021, 30, 1653–1674. [Google Scholar] [CrossRef]
- Issa, M.M. Technological advances in transurethral resection of the prostate: Bipolar versus monopolar TURP. J. Endourol. 2008, 22, 1587–1596. [Google Scholar] [CrossRef]
- Alexander, C.E.; Scullion, M.M.F.; Omar, M.I.; Yuan, Y.; Mamoulakis, C.; N’Dow, J.M.O.; Lam, T.B.L. Cochrane Urology Group Bipolar versus monopolar transurethral resection of the prostate for lower urinary tract symptoms secondary to benign prostatic obstruction. Cochrane Database Syst. Rev. 2019, 12, 12. [Google Scholar]
- Foster, H.E.; Barry, M.J.; Dahm, P.; Gandhi, M.C.; Kaplan, S.A.; Kohler, T.S.; McVary, K.T. Surgical management of lower urinary tract symptoms attributed to benign prostatic hyperplasia: AUA guideline. J. Urol. 2018, 200, 612–619. [Google Scholar] [CrossRef]
- Lerner, L.B.; McVary, K.T.; Barry, M.J.; Bixler, B.R.; Dahm, P.; Das, A.K.; Wilt, T.J. Management of lower urinary tract symptoms attributed to benign prostatic hyperplasia: AUA guideline part II—surgical evaluation and treatment. J. Urol. 2021, 206, 818–826. [Google Scholar] [CrossRef]
- Austin, P.C. A critical appraisal of propensity-score matching in the medical literature between 1996 and 2003. Stat. Med. 2008, 27, 2037–2049. [Google Scholar] [CrossRef]
- Redelmeier, D.A.; Tibshirani, R.J. A simple method for analyzing matched designs with double controls: McNemar’s test can be extended. J. Clin. Epidemiol. 2017, 81, 51–55. [Google Scholar] [CrossRef]
- Martens, E.P.; de Boer, A.; Pestman, W.R.; Belitser, S.V.; Stricker, B.H.C.; Klungel, O.H. Comparing treatment effects after adjustment with multivariable Cox proportional hazards regression and propensity score methods. Pharmacoepidemiol. Drug Saf. 2008, 17, 1–8. [Google Scholar] [CrossRef]
- Kleinbaum, D.G.; Klein, M. Kaplan-Meier survival curves and the log-rank test. In Survival Analysis; Springer: New York, NY, USA, 2012; pp. 55–96. [Google Scholar]
- Caliendo, M.; Kopeinig, S. Some practical guidance for the implementation of propensity score matching. J. Econ. Surv. 2008, 22, 31–72. [Google Scholar] [CrossRef]
- Abadie, A.; Spiess, J. Robust post-matching inference. J. Am. Stat. Assoc. 2022, 117, 983–995. [Google Scholar] [CrossRef]
- Austin, S.R.; Wong, Y.-N.; Uzzo, R.G.; Beck, J.R.; Egleston, B.L. Why summary comorbidity measures such as the Charlson comorbidity index and Elixhauser score work. Med. Care 2015, 53, e65. [Google Scholar] [CrossRef]
- Chen, Y.-B.; Chen, Q.; Wang, Z.; Peng, Y.-B.; Ma, L.-M.; Zheng, D.-C.; Cai, Z.-K.; Li, W.-J.; Ma, L.-H. A prospective, randomized clinical trial comparing plasmakinetic resection of the prostate with holmium laser enucleation of the prostate based on a 2-year followup. J. Urol. 2013, 189, 217–222. [Google Scholar] [CrossRef]
- Yang, Z.; Wang, X.; Liu, T. Thulium laser enucleation versus plasmakinetic resection of the prostate: A randomized prospective trial with 18-month follow-up. Urology 2013, 81, 396–401. [Google Scholar] [CrossRef]
- Castellani, D.; Pirola, G.M.; Rubilotta, E.; Gubbiotti, M.; Scarcella, S.; Maggi, M.; Gauhar, V.; Teoh, J.Y.-C.; Galosi, A.B. GreenLight Laser™ Photovaporization versus Transurethral Resection of the Prostate: A Systematic Review and Meta-Analysis. Res. Rep. Urol. 2021, 13, 263. [Google Scholar] [CrossRef]
- Wu, G.; Hong, Z.; Li, C.; Bian, C.; Huang, S.; Wu, D. A comparative study of diode laser and plasmakinetic in transurethral enucleation of the prostate for treating large volume benign prostatic hyperplasia: A randomized clinical trial with 12-month follow-up. Lasers Med. Sci. 2016, 31, 599–604. [Google Scholar] [CrossRef]
- Habib, E.; Abdallah, M.F.; ElSheemy, M.S.; Badawy, M.H.; Nour, H.H.; Kamal, A.M.; AbdelMohsen, M.; Roshdy, M.A.; Meshref, A. Holmium laser enucleation versus bipolar resection in the management of large-volume benign prostatic hyperplasia: A randomized controlled trial. Int. J. Urol. 2022, 29, 128–135. [Google Scholar] [CrossRef]
- Shamout, S.; Carlson, K.; Brotherhood, H.L.; Crump, T.; Baverstock, R. Incidence and predictors of early and late hospital readmission after transurethral resection of the prostate: A population-based cohort study. BJU Int. 2021, 127, 238–246. [Google Scholar] [CrossRef]
- Okamura, K.; Nojiri, Y.; Seki, N.; Arai, Y.; Matsuda, T.; Hattori, R.; Naito, S. Perioperative management of transurethral surgery for benign prostatic hyperplasia: A nationwide survey in Japan. Int. J. Urol. 2011, 18, 304–310. [Google Scholar] [CrossRef]
- Fu, Y.; Wen, X.; Yin, Y.; Wang, C.; Mai, J. Comparison of effectiveness and postoperative complications of different surgical methods in the treatment of benign prostatic hyperplasia: A systematic review and meta-analysis based on randomized controlled trials. Transl. Androl. Urol. 2022, 11, 842. [Google Scholar] [CrossRef]
- Koguchi, D.; Nishi, M.; Satoh, T.; Shitara, T.; Matsumoto, K.; Fujita, T.; Yoshida, K.; Iwamura, M. Bone dissemination of prostate cancer after holmium laser enucleation of the prostate: A case report and a review of the literature. Int. J. Urol. 2014, 21, 215–217. [Google Scholar] [CrossRef] [PubMed]
- Reich, O.; Gratzke, C.; Bachmann, A.; Seitz, M.; Schlenker, B.; Hermanek, P.; Lack, N.; Stief, C.G.; Urology Section of the Bavarian Working Group for Quality Assurance. Morbidity, mortality and early outcome of transurethral resection of the prostate: A prospective multicenter evaluation of 10,654 patients. J. Urol. 2008, 180, 246–249. [Google Scholar] [CrossRef] [PubMed]
- Cornu, J.N.; Herrmann, T.; Traxer, O.; Matlaga, B. Prevention and management following complications from endourology procedures. Eur. Urol. Focus 2016, 2, 49–59. [Google Scholar] [CrossRef] [PubMed]
- Teng, T.-C.; Shao, I.-H.; Hsu, Y.-C.; Chen, Y.; Tsao, S.-H.; Kang, Y.-T.; Hsieh, M.-L. Risk Factors of Emergency Room Visits for Bleeding Complications Following Transurethral Procedures in the Treatment of Benign Prostatic Hyperplasia: A Retrospective Cohort Study. Clin. Interv. Aging 2021, 16, 1747. [Google Scholar] [CrossRef]
- Kim, A.; Hak, A.-J.; Choi, W.S.; Paick, S.H.; Kim, H.G.; Park, H. Comparison of long-term effect and complications between holmium laser enucleation and transurethral resection of prostate: Nations-wide health insurance study. Urology 2021, 154, 300–307. [Google Scholar] [CrossRef]
- Kuntz, R.M.; Ahyai, S.; Lehrich, K.; Fayad, A.M.R. Transurethral holmium laser enucleation of the prostate versus transurethral electrocautery resection of the prostate: A randomized prospective trial in 200 patients. J. Urol. 2004, 172, 1012–1016. [Google Scholar] [CrossRef]
- Rieken, M.; Bachmann, A. Laser treatment of benign prostate enlargement—Which laser for which prostate? Nat. Rev. Urol. 2014, 11, 142–152. [Google Scholar] [CrossRef]
- Elkoushy, M.A.; Elhilali, M.M. Management of Benign Prostatic Hyperplasia Larger than 100 ml: Simple Open Enucleation Versus Transurethral Laser Prostatectomy. Curr. Urol. Reports. 2016, 17, 44. [Google Scholar] [CrossRef]
- Rivera, M.; Krambeck, A.; Lingeman, J. Holmium laser enucleation of the prostate in patients requiring anticoagulation. Curr. Urol. Rep. 2017, 18, 77. [Google Scholar] [CrossRef]
- Yin, L.; Teng, J.; Huang, C.-J.; Zhang, X.; Xu, D. Holmium laser enucleation of the prostate versus transurethral resection of the prostate: A systematic review and meta-analysis of randomized controlled trials. J. Endourol. 2013, 27, 604–611. [Google Scholar] [CrossRef]
- Gilling, P.J.; Wilson, L.C.; King, C.J.; Westenberg, A.M.; Frampton, C.M.; Fraundorfer, M.R. Long-term results of a randomized trial comparing holmium laser enucleation of the prostate and transurethral resection of the prostate: Results at 7 years. BJU Int. 2012, 109, 408–411. [Google Scholar]
- Elterman, D.S.; Chughtai, B.; Lee, R.; Kurlander, L.; Yip-Bannicq, M.; Kaplan, S.A.; Te, A.E. Comparison of techniques for transurethral laser prostatectomy: Standard photoselective vaporization of the prostate versus transurethral laser enucleation of the prostate. J. Endourol. 2013, 27, 751–755. [Google Scholar] [CrossRef]
- Elmansy, H.; Baazeem, A.; Kotb, A.; Badawy, H.; Riad, E.; Emran, A.; Elhilali, M. Holmium laser enucleation versus photoselective vaporization for prostatic adenoma greater than 60 ml: Preliminary results of a prospective, randomized clinical trial. J. Urol. 2012, 188, 216–221. [Google Scholar] [CrossRef]
- Kreydin, E.I.; Chyu, J.; Lerner, L. Laser prostate ablation and enucleation: Analysis of a national cohort. Int. J. Urol. 2018, 25, 549–553. [Google Scholar]
- Malik, R.; Wang, C.; Lapin, B.; Gerber, G.; Helfand, B. Comparison of patients undergoing laser vaporization of the prostate versus TURP using the ACS-NSQIP database. Prostate Cancer Prostatic Dis. 2015, 18, 18–24. [Google Scholar]
- Heidar, N.A.; Labban, M.; Misrai, V.; Mailhac, A.; Tamim, H.; El-Hajj, A. Laser enucleation of the prostate versus transurethral resection of the prostate: Perioperative outcomes from the ACS NSQIP database. World J. Urol. 2020, 38, 2891–2897. [Google Scholar] [CrossRef]
| Laser | % | TURP | % | p | ||
|---|---|---|---|---|---|---|
| Age, year (mean ± SD) | 70.9 ± 8.4 | 70.9 ± 8.4 | 1.000 | |||
| Age | 50–59 | 145 | 8.8 | 145 | 8.8 | 1.000 |
| 60–69 | 605 | 36.6 | 605 | 36.6 | ||
| 70–79 | 594 | 36.0 | 594 | 36.0 | ||
| >80 | 307 | 18.6 | 307 | 18.6 | ||
| CCI (mean ± SD) | 3.2 ± 2.6 | 3.2 ± 2.6 | 1.000 | |||
| CCI | 0 | 258 | 15.6 | 258 | 15.6 | 1.000 |
| 1–2 | 513 | 31.1 | 513 | 31.1 | ||
| 3–4 | 397 | 24.0 | 397 | 24.0 | ||
| >4 | 483 | 29.3 | 483 | 29.3 | ||
| DM | N | 1162 | 70.4 | 1162 | 70.4 | 1.000 |
| Y | 489 | 29.6 | 489 | 29.6 | ||
| HCD | N | 542 | 32.8 | 542 | 32.8 | 1.000 |
| Y | 1109 | 67.2 | 1109 | 67.2 | ||
| CKD | N | 1471 | 89.1 | 1471 | 89.1 | 1.000 |
| Y | 180 | 10.9 | 180 | 10.9 | ||
| Hyperlipidemia | N | 793 | 48.0 | 793 | 48.0 | 1.000 |
| Y | 858 | 52.0 | 858 | 52.0 | ||
| Heart failure | N | 1066 | 64.6 | 1086 | 65.8 | 0.465 |
| Y | 585 | 35.4 | 565 | 34.2 | ||
| Statins | N | 1008 | 61.1 | 1029 | 62.3 | 0.452 |
| Y | 643 | 38.9 | 622 | 37.7 | ||
| ACEI | N | 856 | 51.8 | 856 | 51.8 | 1.000 |
| Y | 795 | 48.2 | 795 | 48.2 | ||
| β-blocker | N | 628 | 38.0 | 645 | 39.1 | 0.543 |
| Y | 1023 | 62.0 | 1006 | 60.9 | ||
| Anticoagulant | N | 1527 | 92.5 | 1506 | 91.2 | 0.182 |
| Y | 124 | 7.5 | 145 | 8.8 | ||
| Antiplatelet | N | 736 | 44.6 | 755 | 45.7 | 0.506 |
| Y | 915 | 55.4 | 896 | 54.3 | ||
| Spironolactone | N | 1491 | 90.3 | 1476 | 89.4 | 0.387 |
| Y | 160 | 9.7 | 175 | 10.6 | ||
| 5α reductase inhibitors | N | 992 | 60.1 | 1043 | 63.2 | 0.068 |
| Y | 659 | 39.9 | 608 | 36.8 |
| M-TURP | % | PVP | % | DiLEP | % | HoLEP | % | ThuVARP | % | B-TURP | % | p | ||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Age | 50–59 | 100 | 9.9 | 31 | 8.1 | 28 | 9.9 | 5 | 10.9 | 81 | 8.6 | 45 | 7.1 | 0.854 |
| 60–69 | 355 | 35 | 136 | 35.4 | 112 | 39.7 | 16 | 34.8 | 341 | 36.3 | 250 | 39.2 | ||
| 70–79 | 367 | 36.2 | 138 | 35.9 | 94 | 33.3 | 17 | 37 | 345 | 36.7 | 227 | 35.6 | ||
| >80 | 192 | 18.9 | 79 | 20.6 | 48 | 17 | 8 | 17.4 | 172 | 18.3 | 115 | 18.1 | 0.898 | |
| CCI | 0 | 147 | 14.5 | 54 | 14.1 | 42 | 14.9 | 7 | 15.2 | 155 | 16.5 | 111 | 17.4 | |
| 1–2 | 325 | 32.1 | 119 | 31 | 80 | 28.4 | 12 | 26.1 | 302 | 32.2 | 188 | 29.5 | ||
| 3–4 | 239 | 23.6 | 92 | 24 | 76 | 27 | 13 | 28.3 | 216 | 23 | 158 | 24.8 | ||
| >4 | 303 | 29.9 | 119 | 31 | 84 | 29.8 | 14 | 30.4 | 266 | 28.3 | 180 | 28.3 | ||
| DM | N | 705 | 69.5 | 269 | 70.1 | 197 | 69.9 | 28 | 60.9 | 668 | 71.1 | 457 | 71.7 | 0.664 |
| Y | 309 | 30.5 | 115 | 29.9 | 85 | 30.1 | 18 | 39.1 | 271 | 28.9 | 180 | 28.3 | ||
| HCD | N | 330 | 32.5 | 122 | 31.8 | 98 | 34.8 | 13 | 28.3 | 309 | 32.9 | 212 | 33.3 | 0.945 |
| Y | 684 | 67.5 | 262 | 68.2 | 184 | 65.2 | 33 | 71.7 | 630 | 67.1 | 425 | 66.7 | ||
| CKD | N | 900 | 88.8 | 341 | 88.8 | 253 | 89.7 | 37 | 80.4 | 840 | 89.5 | 571 | 89.6 | 0.53 |
| Y | 114 | 11.2 | 43 | 11.2 | 29 | 10.3 | 9 | 19.6 | 99 | 10.5 | 66 | 10.4 | ||
| Hyperlipidemia | N | 485 | 47.8 | 189 | 49.2 | 133 | 47.2 | 15 | 32.6 | 456 | 48.6 | 308 | 48.4 | 0.436 |
| Y | 529 | 52.2 | 195 | 50.8 | 149 | 52.8 | 31 | 67.4 | 483 | 51.4 | 329 | 51.6 | ||
| Heart failure | N | 674 | 66.5 | 246 | 64.1 | 182 | 64.5 | 30 | 65.2 | 608 | 64.7 | 412 | 64.7 | 0.949 |
| Y | 340 | 33.5 | 138 | 35.9 | 100 | 35.5 | 16 | 34.8 | 331 | 35.3 | 225 | 35.3 | ||
| Statins | N | 624 | 61.5 | 232 | 60.4 | 181 | 64.2 | 23 | 50 | 572 | 60.9 | 405 | 63.6 | 0.431 |
| Y | 390 | 38.5 | 152 | 39.6 | 101 | 35.8 | 23 | 50 | 367 | 39.1 | 232 | 36.4 | ||
| ACEI | N | 536 | 52.9 | 179 | 46.6 | 150 | 53.2 | 21 | 45.7 | 506 | 53.9 | 320 | 50.2 | 0.17 |
| Y | 478 | 47.1 | 205 | 53.4 | 132 | 46.8 | 25 | 54.3 | 433 | 46.1 | 317 | 49.8 | ||
| β-blocker | N | 378 | 37.3 | 156 | 40.6 | 91 | 32.3 | 18 | 39.1 | 363 | 38.7 | 267 | 41.9 | 0.104 |
| Y | 636 | 62.7 | 228 | 59.4 | 191 | 67.7 | 28 | 60.9 | 576 | 61.3 | 370 | 58.1 | ||
| Anticoagulant | N | 923 | 91 | 340 | 88.5 | 263 | 93.3 | N/A 1 | N/A | 880 | 93.7 | 583 | 91.5 | 0.027 |
| Y | 91 | 9 | 44 | 11.5 | 19 | 6.7 | N/A | N/A | 59 | 6.3 | 54 | 8.5 | ||
| Antiplatelet | N | 448 | 44.2 | 161 | 41.9 | 122 | 43.3 | 18 | 39.1 | 435 | 46.3 | 307 | 48.2 | 0.308 |
| Y | 566 | 55.8 | 223 | 58.1 | 160 | 56.7 | 28 | 60.9 | 504 | 53.7 | 330 | 51.8 | ||
| Spironolactone | N | 902 | 89 | 348 | 90.6 | 256 | 90.8 | 43 | 93.5 | 844 | 89.9 | 574 | 90.1 | 0.832 |
| Y | 112 | 11 | 36 | 9.4 | 26 | 9.2 | 3 | 6.5 | 95 | 10.1 | 63 | 9.9 | ||
| 5α reductase | N | 655 | 64.6 | 244 | 63.5 | 162 | 57.4 | 27 | 58.7 | 559 | 59.5 | 388 | 60.9 | 0.13 |
| inhibitor | Y | 359 | 35.4 | 140 | 36.5 | 120 | 42.6 | 19 | 41.3 | 380 | 40.5 | 249 | 39.1 |
| M-TURP 1 (n = 1014) | % | PVP (n = 384) | % | p | DiLEP (n = 282) | % | p | HoLEP 2 (n = 46) | % | p | ThuVARP (n = 939) | % | p | B-TURP (n = 637) | % | p | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Emergency room 3 | |||||||||||||||||
| 15 days | 68 | 6.7 | 28 | 7.3 | 0.389 | 33 | 11.7 | 0.008 | 5 | 10.9 | 0.239 | 60 | 6.4 | 0.425 | 44 | 6.9 | 0.92 |
| 30 days | 86 | 8.5 | 30 | 7.8 | 0.388 | 37 | 13.1 | 0.022 | 6 | 13 | 0.28 | 72 | 7.7 | 0.283 | 51 | 8 | 0.784 |
| 60 days | 98 | 9.7 | 35 | 9.1 | 0.421 | 43 | 15.2 | 0.009 | 8 | 17.4 | 0.124 | 83 | 8.8 | 0.291 | 65 | 10.2 | 0.735 |
| 90 days | 105 | 10.4 | 37 | 9.6 | 0.387 | 43 | 15.2 | 0.026 | 8 | 17.4 | 0.104 | 88 | 9.4 | 0.257 | 67 | 10.5 | 0.934 |
| Rehospitalization 4 | |||||||||||||||||
| 15 days | 23 | 2.3 | 7 | 1.8 | 0.391 | 5 | 1.8 | 0.817 | N/A | N/A | 0.72 | 15 | 1.6 | 0.182 | 10 | 1.6 | 0.37 |
| 30 days | 41 | 4 | 13 | 3.4 | 0.346 | 9 | 3.2 | 0.602 | N/A | N/A | 0.446 | 25 | 2.7 | 0.059 | 14 | 2.2 | 0.048 |
| 60 days | 59 | 5.8 | 17 | 4.4 | 0.187 | 19 | 6.7 | 0.572 | N/A | N/A | 0.251 | 40 | 4.3 | 0.071 | 29 | 4.6 | 0.311 |
| 90 days | 82 | 8.1 | 20 | 5.2 | 0.039 | 25 | 8.9 | 0.714 | N/A | N/A | 0.277 | 52 | 5.5 | 0.016 | 38 | 6 | 0.119 |
| 15 Days | 30 Days | 60 Days | 90 Days | |||||
|---|---|---|---|---|---|---|---|---|
| HR (95% CI) | p | HR (95% CI) | p | HR (95% CI) | p | HR (95% CI) | p | |
| Age | ||||||||
| 50–59 (As Reference) | ||||||||
| 60–69 | 0.94 (0.55–1.60) | 0.824 | 0.98 (0.60–1.60) | 0.941 | 1.00 (0.63–1.59) | 0.992 | 1.03 (0.66–1.62) | 0.894 |
| 70–79 | 0.98 (0.58–1.68) | 0.947 | 0.95 (0.58–1.55) | 0.832 | 1.14 (0.72–1.81) | 0.585 | 1.12 (0.71–1.77) | 0.615 |
| >80 | 1.11 (0.63–1.97) | 0.715 | 1.12 (0.66–1.88) | 0.684 | 1.29 (0.79–2.11) | 0.316 | 1.32 (0.81–2.13) | 0.265 |
| Charlson Comorbidity Index | ||||||||
| 0 (As Reference) | ||||||||
| 1–2 | 1.87 (1.06–3.29) | 0.03 | 1.91 (1.14–3.20) | 0.014 | 1.92 (1.20–3.08) | 0.007 | 1.97 (1.24–3.12) | 0.004 |
| 3–4 | 2.01 (1.10–3.67) | 0.023 | 1.88 (1.08–3.28) | 0.026 | 1.96 (1.19–3.25) | 0.009 | 2.06 (1.26–3.37) | 0.004 |
| >4 | 2.35 (1.27–4.34) | 0.006 | 2.37 (1.35–4.16) | 0.003 | 2.30 (1.37–3.85) | 0.002 | 2.36 (1.43–3.92) | 0.001 |
| DM | 0.86 (0.63–1.17) | 0.348 | 0.98 (0.74–1.30) | 0.89 | 1.03 (0.80–1.33) | 0.821 | 1.07 (0.83–1.37) | 0.605 |
| HCD | 1.23 (0.83–1.83) | 0.301 | 1.25 (0.88–1.80) | 0.217 | 1.19 (0.86–1.66) | 0.292 | 1.13 (0.82–1.56) | 0.442 |
| CKD | 1.21 (0.84–1.76) | 0.308 | 1.25 (0.89–1.75) | 0.203 | 1.15 (0.84–1.58) | 0.392 | 1.15 (0.84–1.57) | 0.39 |
| Hyperlipidemia | 1.14 (0.82–1.58) | 0.44 | 1.04 (0.77–1.41) | 0.779 | 1.00 (0.75–1.32) | 0.999 | 1.01 (0.76–1.32) | 0.967 |
| Heart failure | 1.06 (0.78-1.44) | 0.702 | 1.01 (0.76-1.34) | 0.947 | 1.01 (0.78-1.31) | 0.95 | 1.03 (0.80-1.33) | 0.803 |
| Statins | 0.96 (0.70-1.32) | 0.802 | 1.02 (0.76-1.36) | 0.911 | 1.08 (0.82-1.41) | 0.598 | 1.03 (0.79-1.34) | 0.835 |
| ACEI | 1.08 (0.79–1.48) | 0.615 | 1.03 (0.77–1.36) | 0.852 | 1.03 (0.79–1.34) | 0.82 | 1.08 (0.83–1.40) | 0.569 |
| β-blocker | 1.38 (1.00–1.92) | 0.05 | 1.39 (1.03–1.87) | 0.033 | 1.29 (0.98–1.69) | 0.065 | 1.26 (0.96–1.64) | 0.09 |
| Anticoagulant | 0.64 (0.39–1.08) | 0.093 | 0.75 (0.48–1.17) | 0.201 | 0.69 (0.45–1.05) | 0.084 | 0.69 (0.45–1.04) | 0.077 |
| Antiplatelet | 1.59 (0.76–3.34) | 0.217 | 1.34 (0.68–2.67) | 0.4 | 1.43 (0.76–2.68) | 0.268 | 1.28 (0.69–2.37) | 0.44 |
| Spironolactone | 1.20 (0.82–1.76) | 0.353 | 1.22 (0.86–1.73) | 0.262 | 1.28 (0.93–1.76) | 0.136 | 1.23 (0.90–1.69) | 0.195 |
| 5α reductase inhibitors | 1.20 (0.93–1.55) | 0.165 | 1.20 (0.95–1.52) | 0.129 | 1.17 (0.94–1.45) | 0.162 | 1.13 (0.91–1.40) | 0.254 |
| Surgery type | ||||||||
| M-TURP (As Reference) | ||||||||
| PVP | 1.09 (0.70–1.69) | 0.712 | 0.92 (0.61–1.40) | 0.708 | 0.94 (0.64–1.38) | 0.745 | 0.92 (0.63–1.34) | 0.677 |
| DiLEP | 1.74 (1.15–2.65) | 0.009 | 1.57 (1.06–2.31) | 0.023 | 1.63 (1.13–2.33) | 0.008 | 1.52 (1.06–2.16) | 0.022 |
| HoLEP | 1.59 (0.64–3.96) | 0.319 | 1.53 (0.67–3.51) | 0.315 | 1.82 (0.88–3.74) | 0.106 | 1.70 (0.83–3.50) | 0.15 |
| ThuVARP | 0.95 (0.67–1.35) | 0.774 | 0.91 (0.66–1.24) | 0.544 | 0.91 (0.68–1.22) | 0.545 | 0.91 (0.68–1.20) | 0.493 |
| B-TURP | 1.04 (0.71–1.53) | 0.829 | 0.97 (0.68–1.37) | 0.842 | 1.08 (0.79–1.48) | 0.645 | 1.04 (0.76–1.41) | 0.826 |
| 15 Days | 30 Days | 60 Days | 90 Days | |||||
|---|---|---|---|---|---|---|---|---|
| HR (95% CI) | p | HR (95% CI) | p | HR (95% CI) | p | HR (95% CI) | p | |
| Age | ||||||||
| 50–59 (As Reference) | ||||||||
| 60–69 | 1.61 (0.37–7.11) | 0.528 | 1.39 (0.54–3.60) | 0.498 | 1.38 (0.65–2.93) | 0.408 | 1.21 (0.63–2.31) | 0.571 |
| 70–79 | 2.63 (0.61–11.2) | 0.194 | 1.43 (0.55–3.73) | 0.46 | 1.58 (0.74–3.35) | 0.238 | 1.68 (0.88–3.19) | 0.115 |
| >80 | 2.69 (0.6–12.14) | 0.198 | 2.20 (0.83–5.87) | 0.114 | 2.69 (1.24–5.81) | 0.012 | 2.93 (1.52–5.65) | 0.001 |
| Charlson Comorbidity Index | ||||||||
| 0 (As Reference) | ||||||||
| 1–2 | 1.19 (0.41–3.44) | 0.752 | 1.00 (0.47–2.11) | 0.998 | 1.01 (0.58–1.77) | 0.973 | 1.06 (0.64–1.73) | 0.829 |
| 3–4 | 1.34 (0.43–4.18) | 0.609 | 1.21 (0.54–2.70) | 0.638 | 1.07 (0.58–1.97) | 0.84 | 1.14 (0.66–1.95) | 0.641 |
| >4 | 1.82 (0.57–5.77) | 0.309 | 1.49 (0.65–3.40) | 0.349 | 1.25 (0.66–2.38) | 0.496 | 1.15 (0.65–2.03) | 0.639 |
| DM | 1.15 (0.63–2.10) | 0.654 | 1.08 (0.67–1.73) | 0.748 | 1.08 (0.74–1.58) | 0.688 | 1.20 (0.87–1.66) | 0.274 |
| HCD | 0.67 (0.32–1.42) | 0.296 | 0.97 (0.54–1.73) | 0.917 | 0.81 (0.52–1.27) | 0.362 | 0.77 (0.52–1.14) | 0.188 |
| CKD | 0.98 (0.46–2.10) | 0.962 | 1.39 (0.80–2.39) | 0.24 | 1.39 (0.89–2.16) | 0.149 | 1.44 (0.98–2.11) | 0.065 |
| Hyperlipidemia | 1.00 (0.53–1.88) | 0.988 | 0.87 (0.53–1.43) | 0.585 | 0.80 (0.54–1.20) | 0.28 | 0.92 (0.65–1.30) | 0.633 |
| Heart failure | 1.48 (0.79–2.79) | 0.219 | 1.14 (0.71–1.83) | 0.598 | 1.24 (0.85–1.82) | 0.265 | 1.35 (0.97–1.89) | 0.079 |
| Statins | 0.69 (0.36–1.31) | 0.255 | 0.79 (0.48–1.30) | 0.35 | 0.92 (0.61–1.37) | 0.667 | 0.88 (0.63–1.25) | 0.478 |
| ACEI | 0.89 (0.48–1.65) | 0.706 | 0.90 (0.56–1.46) | 0.68 | 0.99 (0.68–1.44) | 0.952 | 1.04 (0.75–1.45) | 0.795 |
| β-blocker | 1.19 (0.62–2.28) | 0.602 | 1.18 (0.72–1.92) | 0.518 | 0.99 (0.68–1.44) | 0.956 | 1.11 (0.80–1.55) | 0.529 |
| Anticoagulant | 1.33 (0.63–2.82) | 0.454 | 1.21 (0.65–2.24) | 0.547 | 1.01 (0.59–1.71) | 0.977 | 0.91 (0.56–1.46) | 0.685 |
| Antiplatelet | 1.58 (0.35–7.21) | 0.557 | 0.88 (0.30–2.64) | 0.823 | 1.25 (0.53–2.96) | 0.614 | 1.29 (0.61–2.73) | 0.501 |
| Spironolactone | 1.09 (0.52–2.29) | 0.816 | 1.34 (0.77–2.32) | 0.295 | 1.14 (0.72–1.81) | 0.582 | 1.16 (0.78–1.72) | 0.475 |
| 5α reductase inhibitors | 1.65 (1.00–2.74) | 0.052 | 1.48 (1.01–2.19) | 0.047 | 1.56 (1.14–2.11) | 0.005 | 1.30 (0.99–1.69) | 0.057 |
| Surgery type | ||||||||
| M-TURP (As Reference) | ||||||||
| PVP | 0.77 (0.33–1.80) | 0.55 | 0.82 (0.44–1.53) | 0.526 | 0.72 (0.42–1.24) | 0.243 | 0.61 (0.38–1.00) | 0.05 |
| DiLEP | 0.75 (0.28–1.98) | 0.561 | 0.78 (0.38–1.61) | 0.5 | 1.15 (0.69–1.94) | 0.59 | 1.12 (0.71–1.75) | 0.634 |
| HoLEP | 1.00 (0.13–7.45) | 0.996 | 0.57 (0.08–4.19) | 0.584 | 0.38 (0.05–2.74) | 0.337 | 0.54 (0.13–2.22) | 0.397 |
| ThuVARP | 0.69 (0.36–1.33) | 0.271 | 0.65 (0.39–1.07) | 0.089 | 0.71 (0.47–1.06) | 0.092 | 0.67 (0.47–0.95) | 0.024 |
| B-TURP | 0.70 (0.33–1.47) | 0.346 | 0.54 (0.29–1.00) | 0.049 | 0.77 (0.49–1.20) | 0.249 | 0.73 (0.50–1.08) | 0.117 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chen, S.-L.; Hsu, C.-K.; Wang, C.-H.; Yang, C.-J.; Chang, T.-J.; Chuang, Y.-H.; Tseng, Y.-T. Comparison of Emergency Room Visits and Rehospitalization for Bleeding Complications following Transurethral Procedures for the Treatment of Benign Prostatic Hyperplasia: A Population-Based Retrospective Cohort Study. J. Clin. Med. 2022, 11, 5662. https://doi.org/10.3390/jcm11195662
Chen S-L, Hsu C-K, Wang C-H, Yang C-J, Chang T-J, Chuang Y-H, Tseng Y-T. Comparison of Emergency Room Visits and Rehospitalization for Bleeding Complications following Transurethral Procedures for the Treatment of Benign Prostatic Hyperplasia: A Population-Based Retrospective Cohort Study. Journal of Clinical Medicine. 2022; 11(19):5662. https://doi.org/10.3390/jcm11195662
Chicago/Turabian StyleChen, Shih-Liang, Chih-Kai Hsu, Chun-Hsiang Wang, Che-Jui Yang, Ting-Jui Chang, Yu-Hsuan Chuang, and Yuan-Tsung Tseng. 2022. "Comparison of Emergency Room Visits and Rehospitalization for Bleeding Complications following Transurethral Procedures for the Treatment of Benign Prostatic Hyperplasia: A Population-Based Retrospective Cohort Study" Journal of Clinical Medicine 11, no. 19: 5662. https://doi.org/10.3390/jcm11195662
APA StyleChen, S.-L., Hsu, C.-K., Wang, C.-H., Yang, C.-J., Chang, T.-J., Chuang, Y.-H., & Tseng, Y.-T. (2022). Comparison of Emergency Room Visits and Rehospitalization for Bleeding Complications following Transurethral Procedures for the Treatment of Benign Prostatic Hyperplasia: A Population-Based Retrospective Cohort Study. Journal of Clinical Medicine, 11(19), 5662. https://doi.org/10.3390/jcm11195662





