Custom-Made Devices Represent a Promising Tool to Increase Correction Accuracy of High Tibial Osteotomy: A Systematic Review of the Literature and Presentation of Pilot Cases with a New 3D-Printed System
Abstract
:1. Introduction
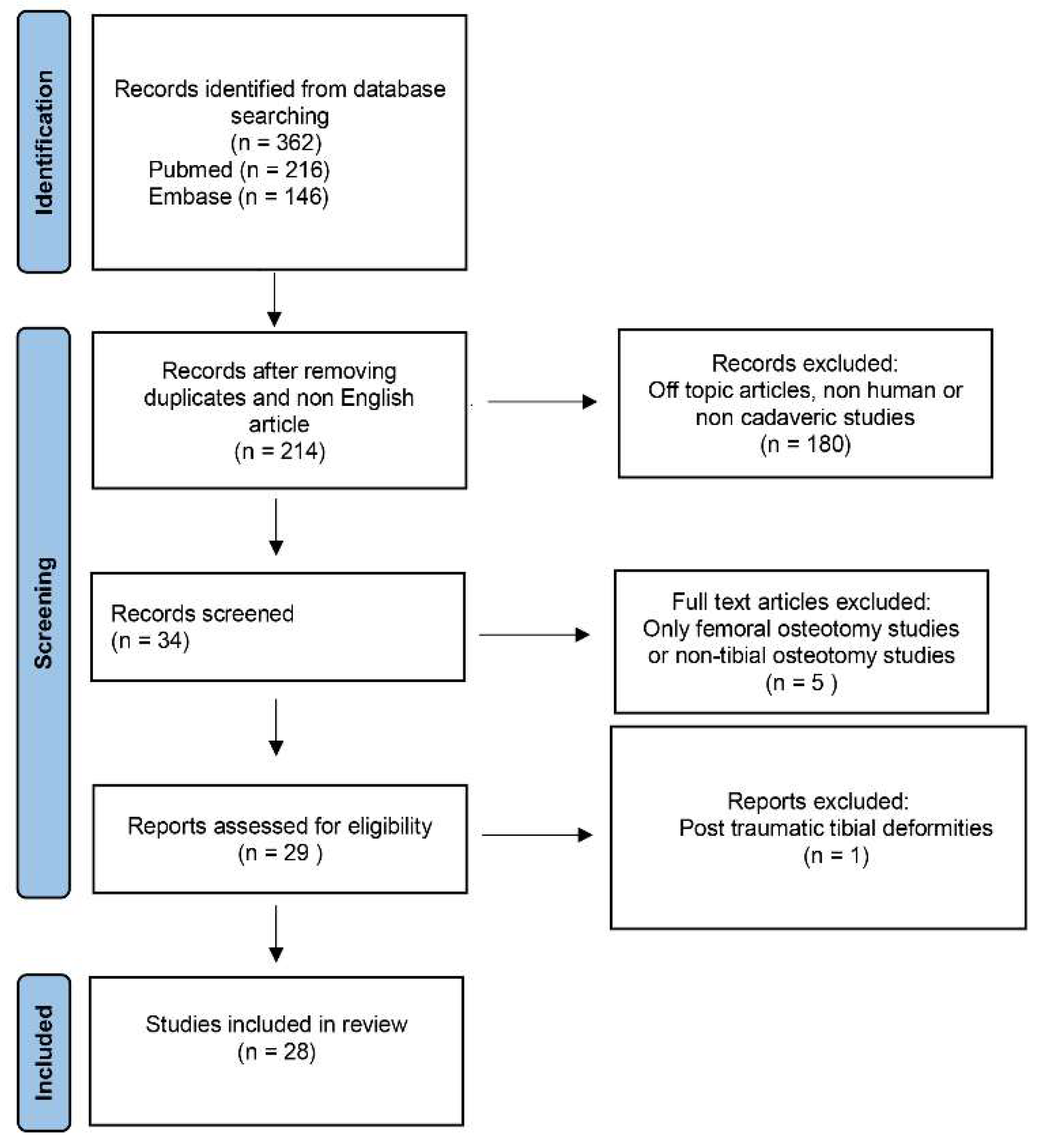
2. Materials and Methods
2.1. Research Strategy
2.2. Study Selection
2.3. Data Extraction and Synthesis
3. Results
4. Preliminary Cases of HTO with a New 3D-Printed Customized Device
4.1. Ethics
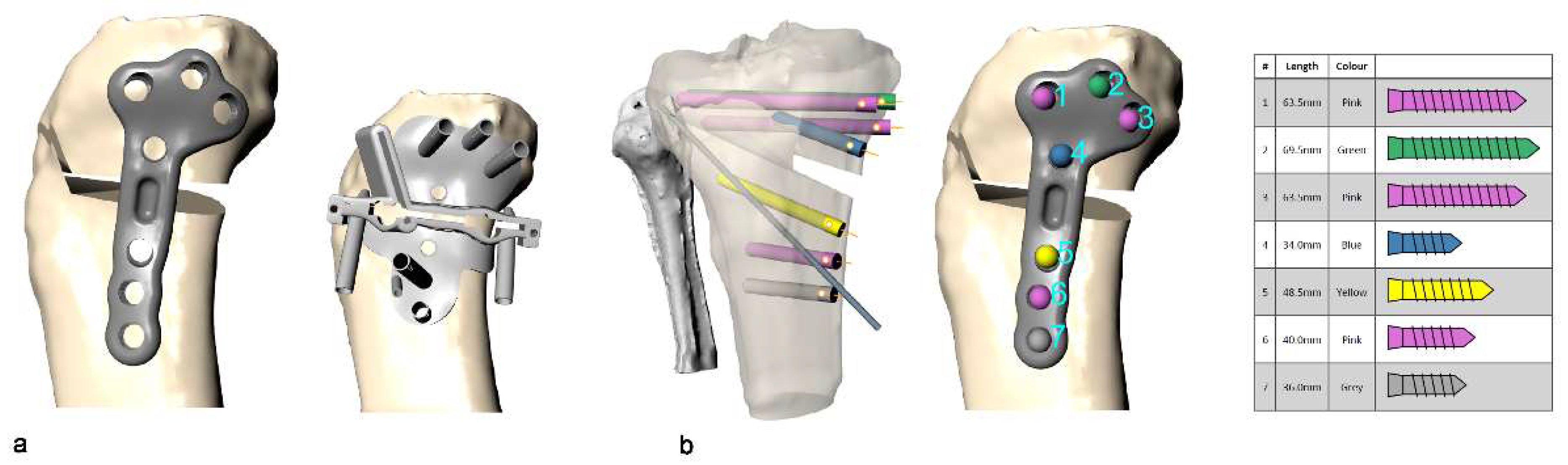
4.2. Customized System for Valgus HTO
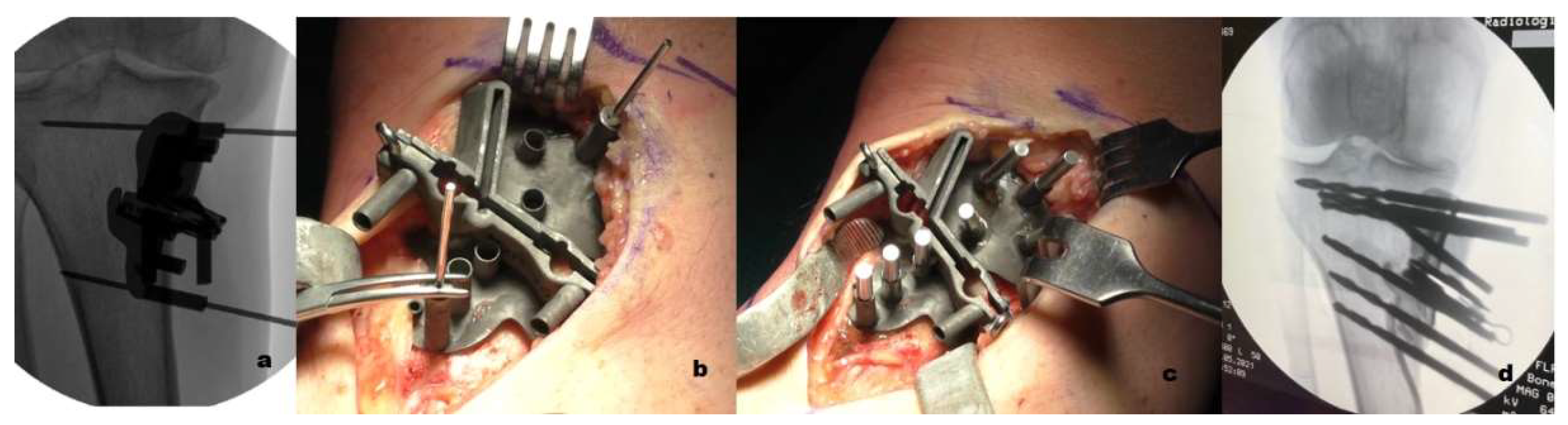
4.3. Surgical Technique
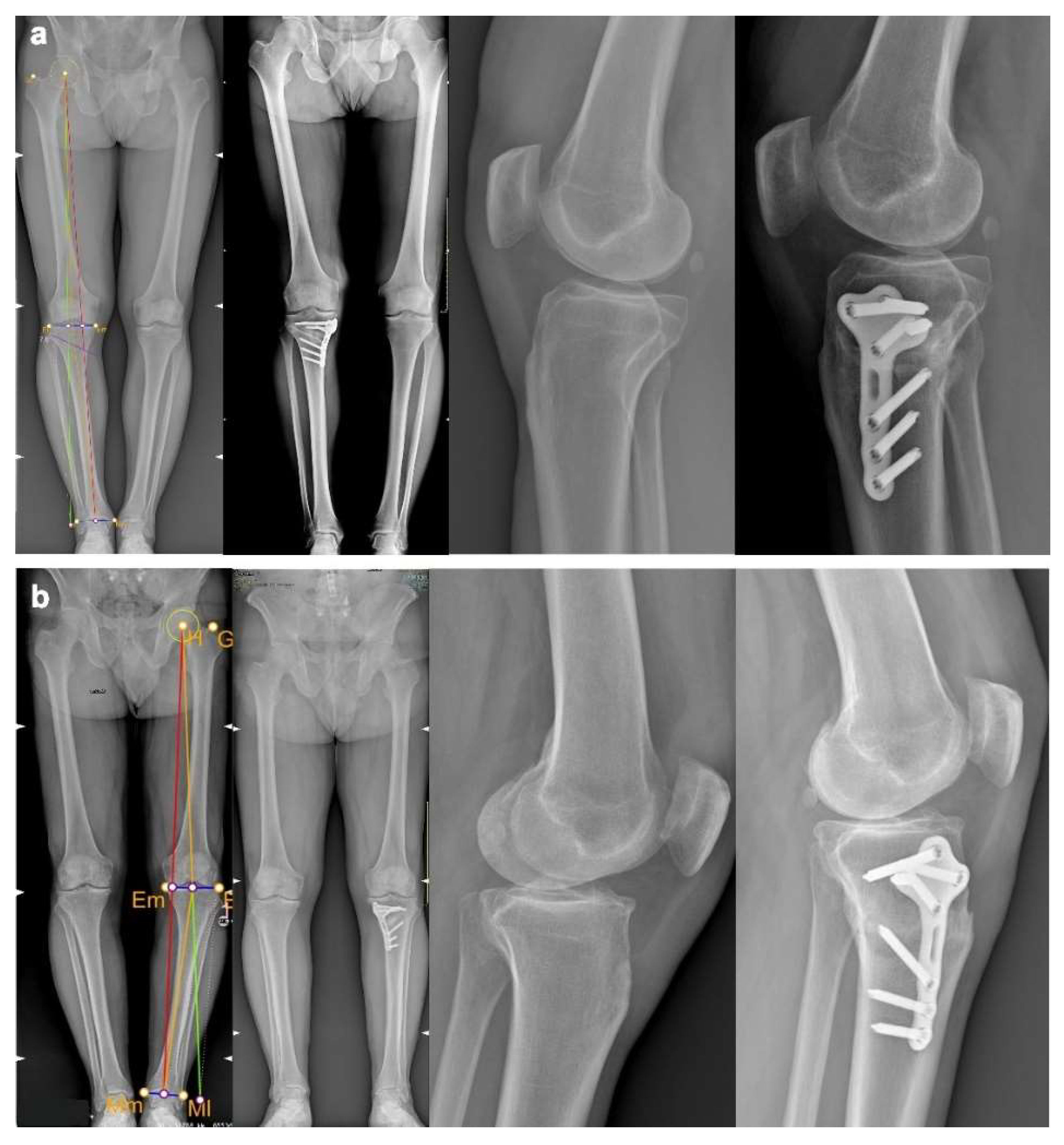
4.4. Imaging Evaluation
4.5. Clinical Evaluation
4.6. Preliminary Cases
5. Discussion
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Ollivier, B.; Berger, P.; Depuydt, C.; Vandenneucker, H. Good Long-Term Survival and Patient-Reported Outcomes after High Tibial Osteotomy for Medial Compartment Osteoarthritis. Knee Surg. Sports Traumatol. Arthrosc. 2021, 29, 3569–3584. [Google Scholar] [CrossRef] [PubMed]
- Sprenger, T.R.; Doerzbacher, J.F. Tibial Osteotomy for the Treatment of Varus Gonarthrosis. Survival and Failure Analysis to Twenty-Two Years. J. Bone Joint Surg. Am. 2003, 85, 469–474. [Google Scholar] [CrossRef] [PubMed]
- Van den Bempt, M.; Van Genechten, W.; Claes, T.; Claes, S. How Accurately Does High Tibial Osteotomy Correct the Mechanical Axis of an Arthritic Varus Knee? A Systematic Review. Knee 2016, 23, 925–935. [Google Scholar] [CrossRef] [PubMed]
- Schubert, I.; Ferner, F.; Dickschas, J. The Effect of Open-Wedge and Closed-Wedge High Tibial Osteotomies on the Tibial Posterior Slope-a Study of Two Hundred Seventy-Nine Cases. Int. Orthop. 2020, 44, 1077–1082. [Google Scholar] [CrossRef] [PubMed]
- Cerciello, S.; Ollivier, M.; Corona, K.; Kaocoglu, B.; Seil, R. CAS and PSI Increase Coronal Alignment Accuracy and Reduce Outliers When Compared to Traditional Technique of Medial Open Wedge High Tibial Osteotomy: A Meta-Analysis. Knee Surg. Sports Traumatol. Arthrosc. 2022, 30, 555–566. [Google Scholar] [CrossRef] [PubMed]
- Victor, J.; Premanathan, A. Virtual 3D Planning and Patient Specific Surgical Guides for Osteotomies around the Knee: A Feasibility and Proof-of-Concept Study. Bone Jt. J. 2013, 95-B, 153–158. [Google Scholar] [CrossRef]
- Jones, G.G.; Jaere, M.; Clarke, S.; Cobb, J. 3D Printing and High Tibial Osteotomy. EFORT Open Rev. 2018, 3, 254–259. [Google Scholar] [CrossRef]
- Liu, G.-B.; Liu, S.; Zhu, C.-H.; Li, J.; Li, J.; Jia, G.-X.; Dong, W.; Zhao, F.; Huang, Y. A Novel 3D-Printed Patient-Specific Instrument Based on “H-Point” for Medial Opening Wedge High Tibial Osteotomy: A Cadaver Study. J. Orthop. Surg. 2022, 17, 169. [Google Scholar] [CrossRef]
- Jörgens, M.; Keppler, A.M.; Ahrens, P.; Prall, W.C.; Bergstraesser, M.; Bachmeier, A.T.; Zeckey, C.; Cavalcanti Kußmaul, A.; Böcker, W.; Fürmetz, J. 3D Osteotomies-Improved Accuracy with Patient-Specific Instruments (PSI). Eur. J. Trauma Emerg. Surg. 2022. [Google Scholar] [CrossRef]
- Chaouche, S.; Jacquet, C.; Fabre-Aubrespy, M.; Sharma, A.; Argenson, J.-N.; Parratte, S.; Ollivier, M. Patient-Specific Cutting Guides for Open-Wedge High Tibial Osteotomy: Safety and Accuracy Analysis of a Hundred Patients Continuous Cohort. Int. Orthop. 2019, 43, 2757–2765. [Google Scholar] [CrossRef]
- Shamseer, L.; Moher, D.; Clarke, M.; Ghersi, D.; Liberati, A.; Petticrew, M.; Shekelle, P.; Stewart, L.A. PRISMA-P Group Preferred Reporting Items for Systematic Review and Meta-Analysis Protocols (PRISMA-P) 2015: Elaboration and Explanation. BMJ 2015, 350, g7647. [Google Scholar] [CrossRef] [PubMed]
- Wang, H.; Newman, S.; Wang, J.; Wang, Q.; Wang, Q. Corrective Osteotomies for Complex Intra-Articular Tibial Plateau Malunions Using Three-Dimensional Virtual Planning and Novel Patient-Specific Guides. J. Knee Surg. 2018, 31, 642–648. [Google Scholar] [CrossRef] [PubMed]
- Chernchujit, B.; Tharakulphan, S.; Prasetia, R.; Chantarapanich, N.; Jirawison, C.; Sitthiseripratip, K. Preoperative Planning of Medial Opening Wedge High Tibial Osteotomy Using 3D Computer-Aided Design Weight-Bearing Simulated Guidance: Technique and Preliminary Result. J. Orthop. Surg. Hong Kong 2019, 27. [Google Scholar] [CrossRef] [PubMed]
- Corin, B.; Wilson, A.; Khakha, R.; Kley, K.; Parratte, S.; Ollivier, M. Posteromedial Opening-Wedge Tibial Osteotomy for Metaphyseal Varus and Abnormal Posterior Slope Correction in Failed Anterior Cruciate Ligament Reconstructions Using a Custom Cutting Guide. Arthrosc. Tech. 2020, 9, e1101–e1108. [Google Scholar] [CrossRef]
- Donnez, M.; Ollivier, M.; Munier, M.; Berton, P.; Podgorski, J.-P.; Chabrand, P.; Parratte, S. Are Three-Dimensional Patient-Specific Cutting Guides for Open Wedge High Tibial Osteotomy Accurate? An In Vitro Study. J. Orthop. Surg. 2018, 13, 171. [Google Scholar] [CrossRef]
- Duan, D.; Cao, Y.; Li, R.; Wang, G.; Zhang, Y.; Xiang, K.; Hu, Y.; Li, Y.; Peng, P.; Zhang, P.; et al. Opening Wedge High Tibial Osteotomy with Combined Use of Patient-Specific 3D-Printed Plates and Taylor Spatial Frame for the Treatment of Knee Osteoarthritis. Pain Res. Manag. 2021, 2021, 8609921. [Google Scholar] [CrossRef]
- Fortier, L.M.; Gursoy, S.; Knapik, D.M.; Chahla, J. Three-Dimensional Patient Specific Instrumentation and Cutting Guide for Medial Closing Wedge High Tibial Osteotomy to Correct Valgus Malalignment. Arthrosc. Tech. 2022, 11, e13–e23. [Google Scholar] [CrossRef]
- Fucentese, S.F.; Meier, P.; Jud, L.; Köchli, G.-L.; Aichmair, A.; Vlachopoulos, L.; Fürnstahl, P. Accuracy of 3D-Planned Patient Specific Instrumentation in High Tibial Open Wedge Valgisation Osteotomy. J. Exp. Orthop. 2020, 7, 7. [Google Scholar] [CrossRef]
- Gerbers, J.G.; Pijpker, P.a.J.; Brouwer, R.W.; van der Veen, H.C. Anterolateral Proximal Tibial Opening Wedge Osteotomy for Biplanar Correction in Genu Valgum Recurvatum Using Patient Specific Instrumentation (PSI). A Technical Note. Knee 2021, 33, 58–64. [Google Scholar] [CrossRef]
- Jacquet, C.; Sharma, A.; Fabre, M.; Ehlinger, M.; Argenson, J.-N.; Parratte, S.; Ollivier, M. Patient-Specific High-Tibial Osteotomy’s “cutting-Guides” Decrease Operating Time and the Number of Fluoroscopic Images Taken after a Brief Learning Curve. Knee Surg. Sports Traumatol. Arthrosc. 2020, 28, 2854–2862. [Google Scholar] [CrossRef]
- Jeong, S.H.; Samuel, L.T.; Acuña, A.J.; Kamath, A.F. Patient-Specific High Tibial Osteotomy for Varus Malalignment: 3D-Printed Plating Technique and Review of the Literature. Eur. J. Orthop. Surg. Traumatol. Orthop. Traumatol. 2022, 32, 845–855. [Google Scholar] [CrossRef]
- Kim, H.-J.; Park, J.; Shin, J.-Y.; Park, I.-H.; Park, K.-H.; Kyung, H.-S. More Accurate Correction Can Be Obtained Using a Three-Dimensional Printed Model in Open-Wedge High Tibial Osteotomy. Knee Surg. Sports Traumatol. Arthrosc. 2018, 26, 3452–3458. [Google Scholar] [CrossRef] [PubMed]
- Kuriyama, S.; Morimoto, N.; Shimoto, T.; Takemoto, M.; Nakamura, S.; Nishitani, K.; Ito, H.; Matsuda, S.; Higaki, H. Clinical Efficacy of Preoperative 3D Planning for Reducing Surgical Errors during Open-Wedge High Tibial Osteotomy. J. Orthop. Res. 2019, 37, 898–907. [Google Scholar] [CrossRef] [PubMed]
- Lau, L.C.M.; Chui, E.C.S.; Fan, J.C.H.; Man, G.C.W.; Hung, Y.W.; Ho, K.K.W.; Chung, K.Y.; Wan, S.Y.C.; Chau, J.W.W.; Yung, P.S.H.; et al. Patient-Specific Instrumentation (PSI) Referencing High Tibial Osteotomy Technological Transfer and Education: Protocol for a Double-Blind, Randomised Controlled Trial (PROTECTED HTO Trial). BMJ Open 2021, 11, e041129. [Google Scholar] [CrossRef]
- Mao, Y.; Xiong, Y.; Li, Q.; Chen, G.; Fu, W.; Tang, X.; Yang, L.; Li, J. 3D-Printed Patient-Specific Instrumentation Technique Vs. Conventional Technique in Medial Open Wedge High Tibial Osteotomy: A Prospective Comparative Study. BioMed Res. Int. 2020, 2020, 1923172. [Google Scholar] [CrossRef]
- Miao, Z.; Li, S.; Luo, D.; Lu, Q.; Liu, P. The Validity and Accuracy of 3D-Printed Patient-Specific Instruments for High Tibial Osteotomy: A Cadaveric Study. J. Orthop. Surg. 2022, 17, 62. [Google Scholar] [CrossRef]
- Munier, M.; Donnez, M.; Ollivier, M.; Flecher, X.; Chabrand, P.; Argenson, J.-N.; Parratte, S. Can Three-Dimensional Patient-Specific Cutting Guides Be Used to Achieve Optimal Correction for High Tibial Osteotomy? Pilot Study. Orthop. Traumatol. Surg. Res. 2017, 103, 245–250. [Google Scholar] [CrossRef]
- Pérez-Mañanes, R.; Burró, J.A.; Manaute, J.R.; Rodriguez, F.C.; Martín, J.V. 3D Surgical Printing Cutting Guides for Open-Wedge High Tibial Osteotomy: Do It Yourself. J. Knee Surg. 2016, 29, 690–695. [Google Scholar] [CrossRef]
- Predescu, V.; Grosu, A.-M.; Gherman, I.; Prescura, C.; Hiohi, V.; Deleanu, B. Early Experience Using Patient-Specific Instrumentation in Opening Wedge High Tibial Osteotomy. Int. Orthop. 2021, 45, 1509–1515. [Google Scholar] [CrossRef]
- Bin Abd Razak, H.R.; Jacquet, C.; Wilson, A.J.; Khakha, R.S.; Kley, K.; Parratte, S.; Ollivier, M. Minimally Invasive High Tibial Osteotomy Using a Patient-Specific Cutting Guide. Arthrosc. Tech. 2021, 10, e431–e435. [Google Scholar] [CrossRef]
- Ruggeri, M.; Gill, H.S.; Leardini, A.; Zaffagnini, S.; MacLeod, A.; Ortolani, M.; Faccia, F.; Grassi, A.; Fabbro, G.D.; Durante, S.; et al. Superimposition of Ground Reaction Force on Tibial-Plateau Supporting Diagnostics and Post-Operative Evaluations in High-Tibial Osteotomy. A Novel Methodology. Gait Posture 2022, 94, 144–152. [Google Scholar] [CrossRef] [PubMed]
- Savov, P.; Hold, M.; Petri, M.; Horstmann, H.; von Falck, C.; Ettinger, M. CT Based PSI Blocks for Osteotomies around the Knee Provide Accurate Results When Intraoperative Imaging Is Used. J. Exp. Orthop. 2021, 8, 47. [Google Scholar] [CrossRef] [PubMed]
- Tardy, N.; Steltzlen, C.; Bouguennec, N.; Cartier, J.-L.; Mertl, P.; Batailler, C.; Hanouz, J.-L.; Rochcongar, G.; Fayard, J.-M. Francophone Arthroscopy Society Is Patient-Specific Instrumentation More Precise than Conventional Techniques and Navigation in Achieving Planned Correction in High Tibial Osteotomy? Orthop. Traumatol. Surg. Res. 2020, 106, S231–S236. [Google Scholar] [CrossRef] [PubMed]
- Van Genechten, W.; Van Tilborg, W.; Van den Bempt, M.; Van Haver, A.; Verdonk, P. Feasibility and 3D Planning of a Novel Patient-Specific Instrumentation Technique in Medial Opening-Wedge High Tibial Osteotomy. J. Knee Surg. 2021, 34, 1560–1569. [Google Scholar] [CrossRef] [PubMed]
- Yang, J.C.-S.; Chen, C.-F.; Luo, C.-A.; Chang, M.-C.; Lee, O.K.; Huang, Y.; Lin, S.-C. Clinical Experience Using a 3D-Printed Patient-Specific Instrument for Medial Opening Wedge High Tibial Osteotomy. BioMed Res. Int. 2018, 2018, 9246529. [Google Scholar] [CrossRef] [PubMed]
- Elson, D.W.; Petheram, T.G.; Dawson, M.J. High Reliability in Digital Planning of Medial Opening Wedge High Tibial Osteotomy, Using Miniaci’s Method. Knee Surg. Sports Traumatol. Arthrosc. 2015, 23, 2041–2048. [Google Scholar] [CrossRef]
- Feucht, M.J.; Minzlaff, P.; Saier, T.; Cotic, M.; Südkamp, N.P.; Niemeyer, P.; Imhoff, A.B.; Hinterwimmer, S. Degree of Axis Correction in Valgus High Tibial Osteotomy: Proposal of an Individualised Approach. Int. Orthop. 2014, 38, 2273–2280. [Google Scholar] [CrossRef]
- Floerkemeier, S.; Staubli, A.E.; Schroeter, S.; Goldhahn, S.; Lobenhoffer, P. Outcome after High Tibial Open-Wedge Osteotomy: A Retrospective Evaluation of 533 Patients. Knee Surg. Sports Traumatol. Arthrosc. 2013, 21, 170–180. [Google Scholar] [CrossRef]
- Vena, G.; D’Adamio, S.; Amendola, A. Complications of Osteotomies about the Knee. Sports Med. Arthrosc. Rev. 2013, 21, 113–120. [Google Scholar] [CrossRef]



| STUDY | DESIGN | LEVEL OF EVIDENCE | OSTEOTOMY TECHNIQUE | CUSTOMISED DEVICE |
|---|---|---|---|---|
| Chaouche 2019 [10] | Prospective cohort | IV | VALGUS MOW | Cutting guide (Newclip Technics, Haute-Goulaine, France) |
| Chernchujit 2019 [13] | Prospective cohort | IV | VALGUS MOW | Planning system (3D CAD weight bearing simulated guidance) |
| Corin 2020 [14] | Case report | IV | VALGUS MOW | Cutting guide (Newclip Technics, Haute-Goulaine, France) |
| Donnez 2018 [15] | Cadaveric study | IV | VALGUS MOW | Cutting guide (Newclip Technics, Haute-Goulaine, France) |
| Duan 2021 [16] | Prospective cohort | IV | VALGUS MOW | Cutting guide (Formlabs, Somerville, MA, USA) Taylored spatial frame (Tianjin Xinzhong, Tianjin, China) |
| Fortier 2021 [17] | technical note | V | VARUS MCW | Cutting guide (Newclip Technics, Haute-Goulaine, France) |
| Fucentese 2020 [18] | Retrospective case series | IV | VALGUS MOW | Cutting guide (Medacta, Castel San Pietro, Switzerland) |
| Gerbers 2021 [19] | Case report | IV | VARUS LOW | Cutting guide (Materialise, Leuven, Belgium) Repositioning guide (Materialise, Leuven, Belgium) |
| Jacquet 2019 (same patients of Chaouche) [20] | Prospective cohort | IV | VALGUS MOW | Cutting guide (Newclip Technics, Haute-Goulaine, France) |
| Jeong 2022 [21] | Case report | IV | VALGUS MOW | Cutting guide 3D-printed Plate 3D-printed |
| Jones 2018 [7] | Technical note | V | VALGUS MOW | Cutting guide (Embody, London, UK) |
| Jörgens 2022 [9] | Cadaveric study | IV | VALGUS MOW | Cutting guide (Autodesk Inc., Mill Valley, CA, USA) Spacers (Autodesk Inc., Mill Valley, CA, USA) |
| Kim 2018 [22] | Retrospective comparative | III | VALGUS MOW | Printed 3D spacer model (Fortus 450 mc, Stratasys, Eden Prairie, MN, USA) |
| Kuriyama 2019 [23] | Prospective cohort | IV | VALGUS MOW | Planning system (3D Template, Kyocera, Kyoto, Japan) |
| Lau 2021 [24] | Technical note | V | VALGUS MOW | Cutting guide (Materialise, Leuven, Belgium) Open wedges (Materialise, Leuven, Belgium) |
| Liu 2022 [8] | Cadaveric study | IV | VALGUS MOW | Cutting guide (Johnson & Johnosn, New Brunswick, NJ, USA) |
| Mao 2020 [25] | Prospective comparative | II | VALGUS MOW | Cutting guide 3 D-printed |
| Miao 2022 [26] | Cadaveric study | IV | VALGUS MOW | Cutting guide 3D-printed Angular bracing spacer 3D-printed |
| Munier 2017 [27] | Prospective cohort | IV | VALGUS MOW | Cutting guide (Newclip Technics, Haute-Goulaine, France) |
| Pérez-Mañanes 2016 [28] | Prospective comparative | II | VALGUS MOW | Cutting guide (DaVinci 1.0, XYZ Printing, Taipei, Taiwan) Polyhedral wedges (DaVinci 1.0, XYZ Printing, Taipei, Taiwan) |
| Predescu 2021 [29] | Retrospective observational | IV | VALGUS MOW | Cutting guide (Newclip Technics, Haute-Goulaine, France) |
| Rahmatullah Bin Abd Razak 2021 [30] | Technical note | V | VALGUS MOW | Cutting guide (Newclip Technics, Haute-Goulaine, France) |
| Ruggeri 2022 [31] | Prospective cohort | IV | VALGUS MOW | Cutting guide (T.O.K.A. 3D Metal Printing, Bath, UK) Plate (T.O.K.A. 3D Metal Printing, Bath, UK) |
| Savov 2021 (in vivo series) [32] | Retrospective observational | IV | VALGUS MOW VARUS LOW VARUS MCW | Cutting guide (Newclip Technics, Haute-Goulaine, France) |
| Savov 2021 (cadaveric series) [32] | Cadaveric study | IV | VALGUS MOW VARUS LOW | Cutting guide (Newclip Technics, Haute-Goulaine, France) |
| Tardy 2020 [33] | Prospective comparative (multicenter) | II | VALGUS MOW | Cutting guide (Newclip Technics, Haute-Goulaine, France) |
| Van Genechten 2020 [34] | Prospective cohort | IV | VALGUS MOW | Fitting wedge (Materialise, Leuven, Belgium) Cast (Materialise, Leuven, Belgium) |
| Victor 2013 [6] | Prospective cohort | IV | VALGUS MOW VARUS LOW | Cutting guide (Materialise, Leuven, Belgium) |
| Yang 2018 [35] | Prospective cohort | IV | VALGUS MOW | Cutting guide (Formlabs, Somerville, MA, USA) |
| (a) | ||||
| STUDY | NUMBER OF PATIENTS/KNEES | FU | Δ FROM PLANNED CORRECTION | NOTES |
| Chaouche [10] | 100 | 24 months | ΔHKA 1 ± 0.9 ΔPPTA 0.4 ± 0.8 | N.R. |
| ChernchujIt [13] | 19 | N.R. | ΔMA −0.04 | N.R |
| Corin [14] | 1 | N.R. | N.A. | Associated ACL revision |
| Duan [16] | 25 | 18 months | N.A. | N.R. |
| Fucentese [18] | 23 | 12 weeks | ΔHKA 0.8 ± 1.5 ΔPTS 1.7 ± 2.2 | N.R. |
| Gerbers [19] | 1 | 3 months | ΔHKA 2.76; ΔPTS 1.24 | Valgus and recurvatum preoperative knee deformity |
| Jacquet [20] | 71 | 12 months | Same study populations of Chaouche | Outcomes evaluation: surgical time, surgeon anxiety, and number of fluoroscopic images |
| Kuriyama [23] | 60 | 2 months | ΔMPTA1.4; ΔLPTS 1 ΔMPTS −1 | N.R. |
| Munier [27] | 10 | 3 months | ΔHKA 0.98 ΔPTS 0.96 | N.R. |
| Predescu [29] | 25 | 12 months | ΔHKA, ΔPTS, ΔMPTA <2° | N.R. |
| Ruggeri [31] | 4 | 6 months | N.A. | Lateralization of the ground reaction force at gait analysis |
| Savov [32] | 19 | N.R. | ΔHKA 1.45 ± 1.16° ΔMPTA 0.86 ± 0.6° ΔLDFA 1.98 ± 1.33° | N.R. |
| Van Genechten [34] | 10 | 3 months | ΔHKA 0.9 ± 0.6 ΔMPTA1.3 ± 1.1 ΔPTS 2.7 ± 1.8 | N.R. |
| Victor [6] | 14 | 6 weeks | Δ WEDGE ANGLE (CORONAL) 0° Δ WEDGE ANGLE (SAGITTAL) 0.3° ΔHKA 0.3 ± 0.75 | N.R. |
| Yang [35] | 10 | 3 months | ΔWBL % 4.9% ΔPTS 4.1% | N.R. |
| Jeong [21] | 1 | 6 weeks | ΔHKA 0.7 ΔMPTA 1.9 ΔPTS 0.3 | N.R. |
| (b) | ||||
| STUDY | NUMBER OF PATIENTS/KNEES | FU | Δ FROM PLANNED CORRECTION | CONTROL GROUP AND RESULTS OF PSI GROUP |
| Kim [22] | 20 | 12 months | ΔHKA 2.3 ± 2.5 WBL: 80% ACCEPTABLE RANGE | 20 standard MOW: HIGHER NUMBER OF PATIENTS IN ACCETABLE RANGE (p = 0.028); LOWER MEAN ABSOLUTE DIFFERENCE WITH THE TARGET POINT (p = 0.005) |
| Mao [25] | 18 | 12 months | ΔHKA 0.2 ± 0.6; ΔMPTA 0.1 ± 0.4 | 19 standard MOW SMALLER CORRECTION ERROR (p=0.004) |
| Pérez-Mañanes [28] | 8 | N.R. | ΔCA 0.5 | 20 standard MOW: NO STATISTICALLY SIGNIFICANT DIFFERENCES |
| Tardy [33] | 39 | 12 months | ΔHKA 0.3 ± 3.1 | 61 standard MOW/LCW and a group of 26 MOW with navigation system: NO STATISTICALLY SIGNIFICANT DIFFERENCES |
| STUDY | NUMBER OF PATIENTS/KNEES | Δ FROM PLANNED CORRECTION | NOTES |
|---|---|---|---|
| Donnez [15] | 10 | ΔMPTA 0.2 ΔPTS −0.1 | N.R. |
| Jörgens [9] | 13 | ΔMPTA 0.57 ΔMPTS 0.98 ΔLPTS 1.26 | N.R. |
| Liu [8] | 15 | ΔHKA 0.62 ± 0.56; ΔPTS 1.24 ± 0.7 | Control group of 11 standard HTO: PSI GROUP MORE ACCURATE FOR HKA CORRECTION (p = 0.032) AND PTS CORRECTION (p = 0.015) |
| Miao | 10 | ΔMPTA −0.72 | |
| Savov [32] | 8 | ΔMPTA 3.47 ± 1.07° ΔLDFA 2.18 ± 1.9° | PERFORMED WITHOUT USE OF INTRAOPERATIVE FLUOROSCOPY;Compared to human retrospective series by Savov with intra-operative fluoroscopy: SIGNIFICANT HIGHER ACCURACY WAS OBTAINED USING INTRAOPERATIVE FLUOROSCOPY (p < 0.001) |
| PATIENT ID | AGE | BMI | VAS PRE-OP | VAS POST-OP | KOOS TOTAL PRE-OP | KOOS TOTAL POST-OP | HKA PRE-OP | HKA PLANNED | HKA POST-OP | PTS PRE-OP | PTS PLANNED | PTS POST-OP |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Patient 1 | 48 years old | 23.5 | 3 | 0 | 76 | 86 | 185.6° | 180.6° | 180.1° | 10° | 10° | 9.9° |
| Patient 2 | 60 years old | 27.7 | 3 | 0 | 51 | 74 | 190.1° | 180.3° | 181.9° | 8° | 8° | 8° |
| Patient 3 | 47 years old | 24.7 | 4 | 0 | 51 | 90 | 194.3° | 181.3 | 181.1° | 18° | 13.5° | 15° |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zaffagnini, S.; Dal Fabbro, G.; Belvedere, C.; Leardini, A.; Caravelli, S.; Lucidi, G.A.; Agostinone, P.; Mosca, M.; Neri, M.P.; Grassi, A. Custom-Made Devices Represent a Promising Tool to Increase Correction Accuracy of High Tibial Osteotomy: A Systematic Review of the Literature and Presentation of Pilot Cases with a New 3D-Printed System. J. Clin. Med. 2022, 11, 5717. https://doi.org/10.3390/jcm11195717
Zaffagnini S, Dal Fabbro G, Belvedere C, Leardini A, Caravelli S, Lucidi GA, Agostinone P, Mosca M, Neri MP, Grassi A. Custom-Made Devices Represent a Promising Tool to Increase Correction Accuracy of High Tibial Osteotomy: A Systematic Review of the Literature and Presentation of Pilot Cases with a New 3D-Printed System. Journal of Clinical Medicine. 2022; 11(19):5717. https://doi.org/10.3390/jcm11195717
Chicago/Turabian StyleZaffagnini, Stefano, Giacomo Dal Fabbro, Claudio Belvedere, Alberto Leardini, Silvio Caravelli, Gian Andrea Lucidi, Piero Agostinone, Massimiliano Mosca, Maria Pia Neri, and Alberto Grassi. 2022. "Custom-Made Devices Represent a Promising Tool to Increase Correction Accuracy of High Tibial Osteotomy: A Systematic Review of the Literature and Presentation of Pilot Cases with a New 3D-Printed System" Journal of Clinical Medicine 11, no. 19: 5717. https://doi.org/10.3390/jcm11195717






