Prevalence and Quality of Endodontic Treatment in Patients with Cardiovascular Disease and Associated Risk Factors
Abstract
1. Introduction
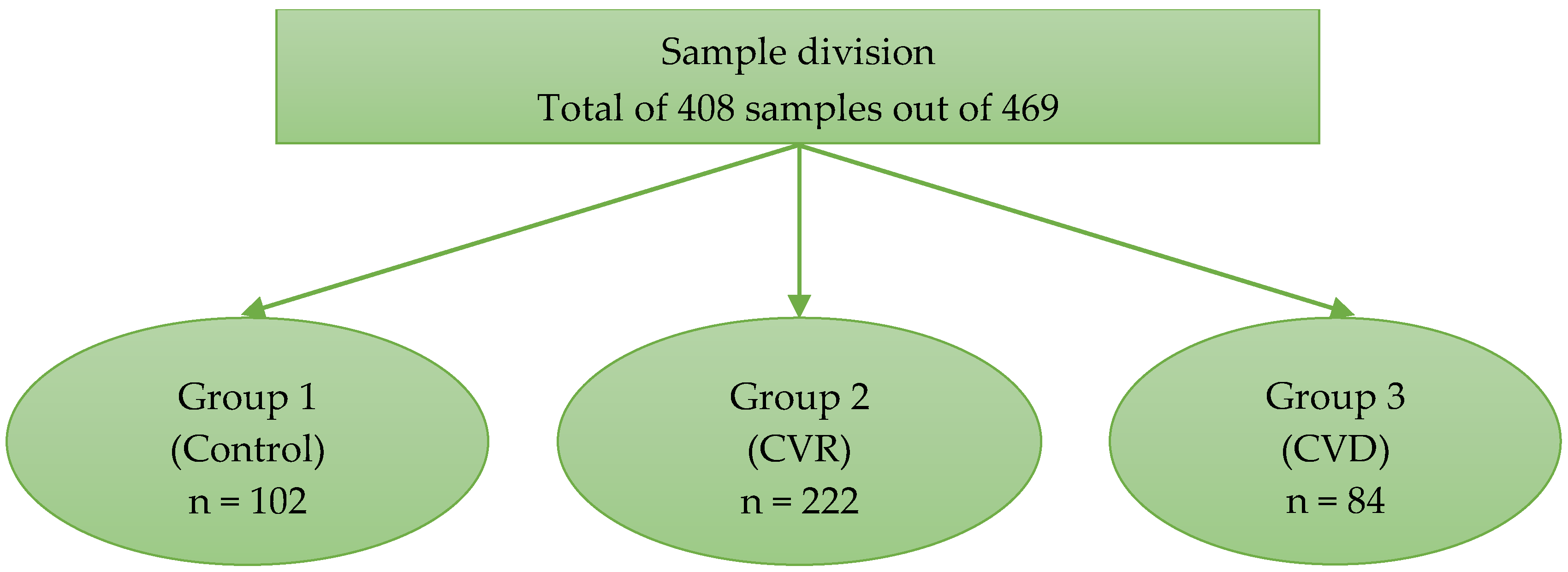
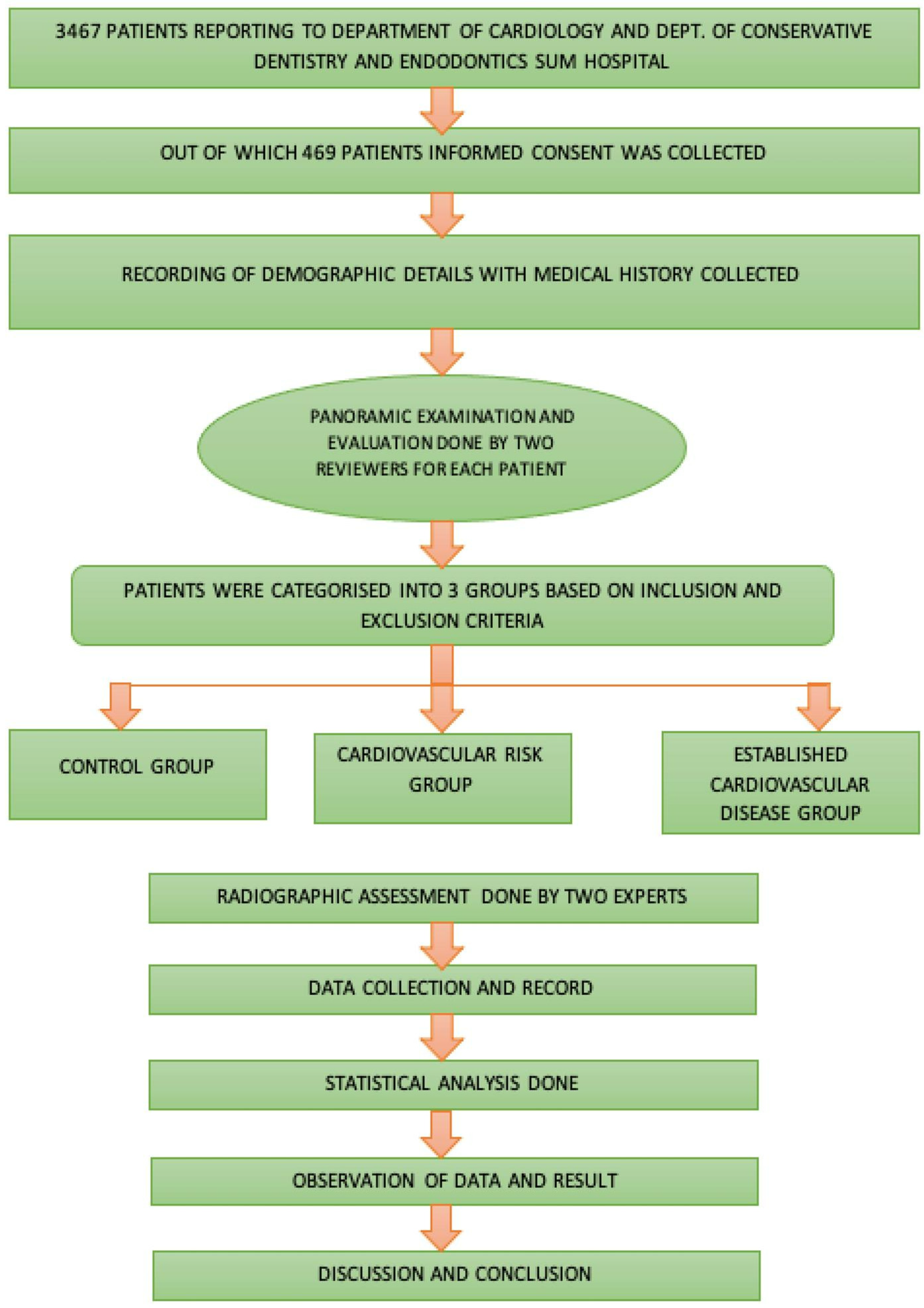
2. Materials and Methods
2.1. Source of Data
2.2. Sample Size Calculation
| Algorithm 1. Formula for calculating sample size |
| Analysis: A priori: Compute the required sample size Input: Tail(s) = Two Effect size |ρ| = 0.18 α err probability = 0.05 Power (1 − β err probability) = 0.95 Output: Noncentrality parameter δ = 3.6183698 Critical t = 1.9660811 Df = 389 Total sample size = 39 Actual power = 0.9504731 |
2.3. Criteria to Evaluate the Cardiovascular Risk Status (Atherosclerotic Cardiovascular Disease Classification, ASCVD)
- low-risk (<5%)
- borderline risk (5% to 7.4%)
- intermediate risk (7.5% to 19.9%)
- high risk (≥20%)
2.4. CVD Group
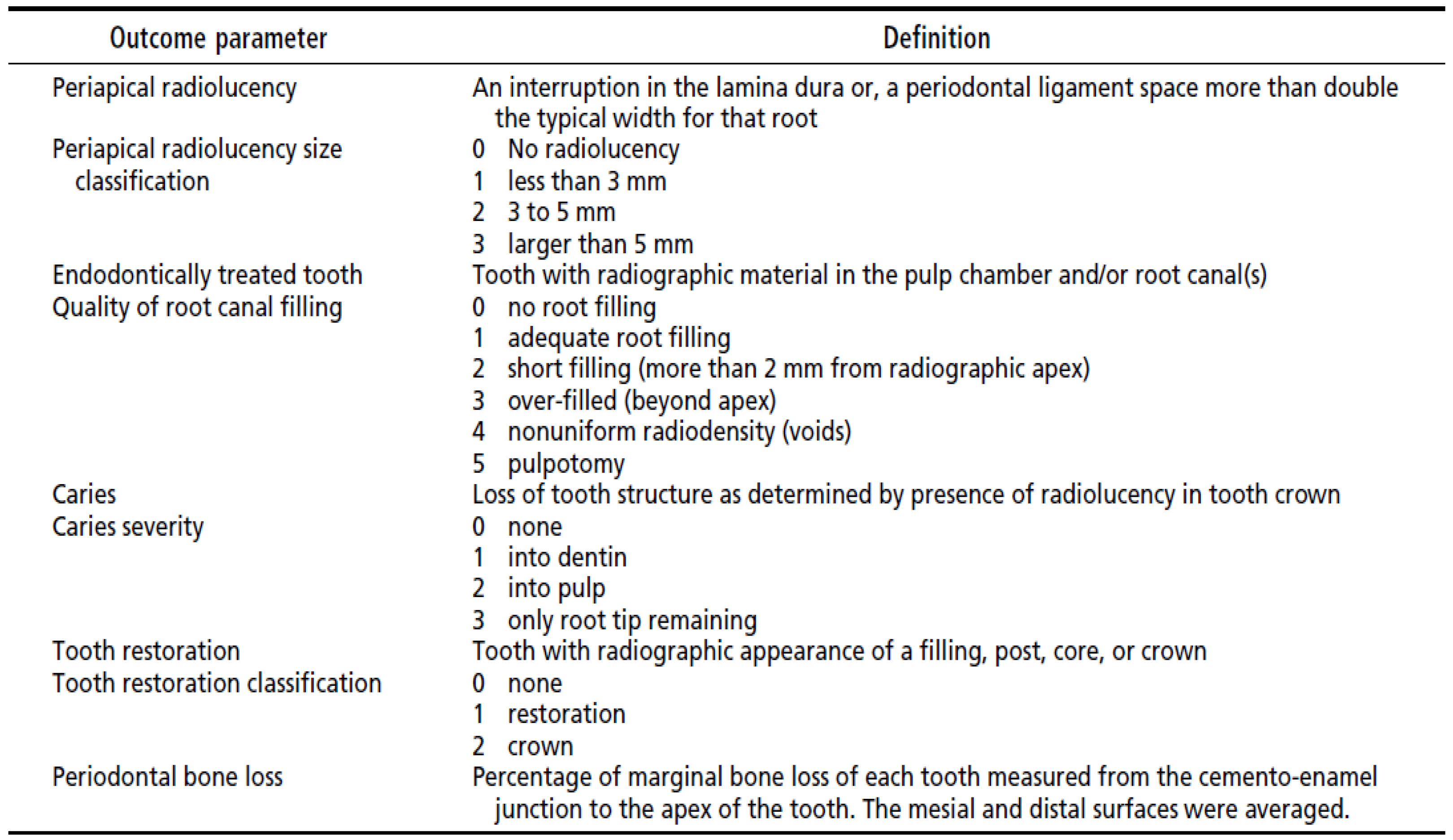
2.5. Data Collection
- number of teeth requiring endodontic treatment,
- tooth type,
- whether the tooth/teeth previously had root canal treatment,
- diagnosis based on Ingle’s classification of pulp and periapical status [24] (If a patient had multiple teeth requiring endodontic treatment, the diagnostic classification of the tooth about which the patient chiefly complained was considered),
- periapical radiolucency was based on the methods and criteria of the peri-apical index (PAI) from periapical radiographs [25]. The highest score amongst the teeth was assigned to the participant; for multirooted teeth, the highest score of any individual root was assigned.
2.6. Statistical Analysis
3. Results
3.1. Demographic and Clinical Profile of Cases
3.1.1. Age and Gender Distribution
3.1.2. Clinical Profile of Cases
3.2. Agreement on OPG Interpretation between Examiners
3.3. Endodontic and Periodontal Status among the Investigated Population Sample
4. Discussion
4.1. Demographic Characteristics of the Sample
4.2. Clinical Profile of the Sample
4.3. Prevalence of Periapical Radiolucency in the Investigated Sample
4.4. Quality of Endodontic Treatment in the Investigated Sample
4.5. Prevalence and Severity of Dental Caries
4.6. Prevalence of Tooth Restorations
4.7. Prevalence of Periodontal Bone Loss
5. Limitations of the Study
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Kolte, V.S.; Dolas, R.S.; Shenoi, R. Demographic Study of Prevalence of Systemic Diseases in Oral Maxillofacial Surgery Patients of Central India. J. Maxillofac. Oral. Surg. 2014, 13, 267–270. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Tavares, M.; Lindefjeld Calabi, K.A.; San Martin, L. Systemic Diseases and Oral Health. Dent. Clin. N. Am. 2014, 58, 797–814. [Google Scholar] [CrossRef] [PubMed]
- Buhlin, K.; Gustafsson, A.; Håkansson, J.; Klinge, B. Oral Health and Cardiovascular Disease in Sweden. J. Clin. Periodontol. 2002, 29, 254–259. [Google Scholar] [CrossRef] [PubMed]
- Chaudhry, S.; Jaiswal, R.; Sachdeva, S. Dental Considerations in Cardiovascular Patients: A Practical Perspective. Indian Heart J. 2016, 68, 572–575. [Google Scholar] [CrossRef]
- Joshipura, K.; Rimm, E.; Douglass, C.; Trichopoulos, D.; Ascherio, A.; Willett, W. Poor Oral Health and Coronary Heart Disease. J. Dent. Res. 1996, 75, 1631–1636. [Google Scholar] [CrossRef] [PubMed]
- Beck, J.; Garcia, R.; Heiss, G.; Vokonas, P.S.; Offenbacher, S. Periodontal Disease and Cardiovascular Disease. J. Periodontol. 1996, 67, 1123–1137. [Google Scholar] [CrossRef] [PubMed]
- Schmalz, G.; Binner, C.; Eisner, M.; Wagner, J.; Rast, J.; Kottmann, T.; Haak, R.; Lehmann, S.; Borger, M.A.; Garbade, J.; et al. Oral Health-Related Quality of Life in Patients with Heart Failure and Left Ventricular Assist Devices-Results of a Cross-Sectional Study. Clin. Oral Investig. 2021, 25, 5879–5887. [Google Scholar] [CrossRef]
- Soto-Barreras, U.; Olvera-Rubio, J.O.; Loyola-Rodriguez, J.P.; Reyes-Macias, J.F.; Martinez-Martinez, R.E.; Patiño-Marin, N.; Martinez-Castañon, G.A.; Aradillas-Garcia, C.; Little, J.W. Peripheral Arterial Disease Associated with Caries and Periodontal Disease. J. Periodontol. 2013, 84, 486–494. [Google Scholar] [CrossRef]
- Morrison, H.I.; Ellison, L.F.; Taylor, G.W. Periodontal Disease and Risk of Fatal Coronary Heart and Cerebrovascular Diseases. J. Cardiovasc. Risk 1999, 6, 7–11. [Google Scholar] [CrossRef]
- Sanz, M.; Marco del Castillo, A.; Jepsen, S.; Gonzalez-Juanatey, J.R.; D’Aiuto, F.; Bouchard, P.; Chapple, I.; Dietrich, T.; Gotsman, I.; Graziani, F.; et al. Periodontitis and Cardiovascular Diseases: Consensus Report. J. Clin. Periodontol. 2020, 47, 268–288. [Google Scholar] [CrossRef]
- Humphrey, L.L.; Fu, R.; Buckley, D.I.; Freeman, M.; Helfand, M. Periodontal Disease and Coronary Heart Disease Incidence: A Systematic Review and Meta-Analysis. J. Gen. Intern. Med. 2008, 23, 2079–2086. [Google Scholar] [CrossRef]
- Berlin-Broner, Y.; Febbraio, M.; Levin, L. Association between Apical Periodontitis and Cardiovascular Diseases: A Systematic Review of the Literature. Int. Endod. J. 2017, 50, 847–859. [Google Scholar] [CrossRef]
- Gomes, M.S.; Blattner, T.C.; Sant’Ana Filho, M.; Grecca, F.S.; Hugo, F.N.; Fouad, A.F.; Reynolds, M.A. Can Apical Periodontitis Modify Systemic Levels of Inflammatory Markers? A Systematic Review and Meta-Analysis. J. Endod. 2013, 39, 1205–1217. [Google Scholar] [CrossRef]
- Aminoshariae, A.; Kulild, J.C.; Mickel, A.; Fouad, A.F. Association between Systemic Diseases and Endodontic Outcome: A Systematic Review. J. Endod. 2017, 43, 514–519. [Google Scholar] [CrossRef]
- Khalighinejad, N.; Aminoshariae, M.R.; Aminoshariae, A.; Kulild, J.C.; Mickel, A.; Fouad, A.F. Association between Systemic Diseases and Apical Periodontitis. J. Endod. 2016, 42, 1427–1434. [Google Scholar] [CrossRef]
- Georgiou, A.C.; Crielaard, W.; Armenis, I.; de Vries, R.; van der Waal, S.V. Apical Periodontitis Is Associated with Elevated Concentrations of Inflammatory Mediators in Peripheral Blood: A Systematic Review and Meta-Analysis. J. Endod. 2019, 45, 1279–1295.e3. [Google Scholar] [CrossRef]
- Aminoshariae, A.; Kulild, J.; Fouad, A.F. The Impact of Cardiovascular Disease and Endodontic Outcome: A Systematic Review of Longitudinal Studies. Clin. Oral Investig. 2020, 24, 3813–3819. [Google Scholar] [CrossRef]
- Jakovljevic, A.; Duncan, H.F.; Nagendrababu, V.; Jacimovic, J.; Milasin, J.; Dummer, P.M.H. Association between Cardiovascular Diseases and Apical Periodontitis: An Umbrella Review. Int. Endod. J. 2020, 53, 1374–1386. [Google Scholar] [CrossRef]
- Koletsi, D.; Iliadi, A.; Tzanetakis, G.N.; Vavuranakis, M.; Eliades, T. Cardiovascular Disease and Chronic Endodontic Infection. Is There an Association? A Systematic Review and Meta-Analysis. Int. J. Environ. Res. Public Health 2021, 18, 9111. [Google Scholar] [CrossRef]
- Aloutaibi, Y.A.; Alkarim, A.S.; Qumri, E.M.; Almansour, L.A.; Alghamdi, F.T. Chronic Endodontic Infections and Cardiovascular Diseases: Does the Evidence Support an Independent Association. Cureus 2021, 13, e19864. [Google Scholar] [CrossRef]
- Cintra, L.T.A.; Gomes, M.S.; da Silva, C.C.; Faria, F.D.; Benetti, F.; Cosme-Silva, L.; Samuel, R.O.; Pinheiro, T.N.; Estrela, C.; González, A.C.; et al. Evolution of Endodontic Medicine: A Critical Narrative Review of the Interrelationship between Endodontics and Systemic Pathological Conditions. Odontology 2021, 109, 741–769. [Google Scholar] [CrossRef]
- Faul, F.; Erdfelder, E.; Lang, A.-G.; Buchner, A. G*Power 3: A Flexible Statistical Power Analysis Program for the Social, Behavioral, and Biomedical Sciences. Behav. Res. Methods 2007, 39, 175–191. [Google Scholar] [CrossRef]
- Ascvd Risk Factor Estimate—Yahoo India Search Results. Available online: https://tools.acc.org (accessed on 19 April 2022).
- Ingle, J.I.; Bakland, L.K.; Baumgartner, J.C. Ingle’s Endodontics 6, 6th ed.; Decker, B.C., Ed.; McGraw-Hill Education: Hamilton, ON, Canada, 2008; ISBN 978-1-60795-068-4. [Google Scholar]
- Ørstavik, D.; Kerekes, K.; Eriksen, H.M. The Periapical Index: A Scoring System for Radiographic Assessment of Apical Periodontitis. Dent. Traumatol. 1986, 2, 20–34. [Google Scholar] [CrossRef]
- Chen, C.-Y.; Hasselgren, G.; Serman, N.; Elkind, M.S.V.; Desvarieux, M.; Engebretson, S.P. Prevalence and Quality of Endodontic Treatment in the Northern Manhattan Elderly. J. Endod. 2007, 33, 230–234. [Google Scholar] [CrossRef]
- Ahlqwist, M.; Halling, A.; Hollender, L. Rotational Panoramic Radiography in Epidemiological Studies of Dental Health. Comparison between Panoramic Radiographs and Intraoral Full Mouth Surveys. Swed. Dent. J. 1986, 10, 73–84. [Google Scholar]
- Eriksen, H.M.; Bjertness, E. Prevalence of Apical Periodontitis and Results of Endodontic Treatment in Middle-Aged Adults in Norway. Endod. Dent. Traumatol. 1991, 7, 1–4. [Google Scholar] [CrossRef]
- Alkis, H.T.; Kustarci, A. Radiographic Assessment of the Relationship between Root Canal Treatment Quality, Coronal Restoration Quality, and Periapical Status. Niger. J. Clin. Pract. 2019, 22, 1126. [Google Scholar] [CrossRef]
- Choi, J.-W. Assessment of Panoramic Radiography as a National Oral Examination Tool: Review of the Literature. Imaging Sci. Dent. 2011, 41, 1–6. [Google Scholar] [CrossRef]
- Eckerbom, M.; Andersson, J.E.; Magnusson, T. Interobserver Variation in Radiographic Examination of Endodontic Variables. Endod. Dent. Traumatol. 1986, 2, 243–246. [Google Scholar] [CrossRef]
- Locht, S.; Poulsen, S. Intra-Observer Variability in the Assessment of Panoramic Radiographs of Children Aged 9–10 Years. Dentomaxillofac. Radiol. 1980, 9, 28–31. [Google Scholar] [CrossRef]
- Sanchez, P.; Everett, B.; Salamonson, Y.; Redfern, J.; Ajwani, S.; Bhole, S.; Bishop, J.; Lintern, K.; Nolan, S.; Rajaratnam, R.; et al. The Oral Health Status, Behaviours and Knowledge of Patients with Cardiovascular Disease in Sydney Australia: A Cross-Sectional Survey. BMC Oral Health 2019, 19, 12. [Google Scholar] [CrossRef] [PubMed]
- Maas, A.H.E.M.; Appelman, Y.E.A. Gender Differences in Coronary Heart Disease. Neth. Heart J. 2010, 18, 598–602. [Google Scholar] [CrossRef]
- Weidner, G. Why Do Men Get More Heart Disease than Women? An International Perspective. J. Am. Coll. Health 2000, 48, 291–294. [Google Scholar] [CrossRef]
- Han, S.-J.; Son, Y.-J.; Kim, B.-H. Association between Diabetes Mellitus and Oral Health Status in Patients with Cardiovascular Diseases: A Nationwide Population-Based Study. Int. J. Environ. Res. Public Health 2021, 18, 4889. [Google Scholar] [CrossRef]
- Aoyama, N.; Suzuki, J.-I.; Kobayashi, N.; Hanatani, T.; Ashigaki, N.; Yoshida, A.; Shiheido, Y.; Sato, H.; Izumi, Y.; Isobe, M. Increased Oral Porphyromonas Gingivalis Prevalence in Cardiovascular Patients with Uncontrolled Diabetes Mellitus. Int. Heart J. 2018, 59, 802–807. [Google Scholar] [CrossRef] [PubMed]
- Mei, F.; Xie, M.; Huang, X.; Long, Y.; Lu, X.; Wang, X.; Chen, L. Porphyromonas gingivalis and Its Systemic Impact: Current Status. Pathogens 2020, 9, 944. [Google Scholar] [CrossRef]
- Segura-Egea, J.J.; Jimenez-Moreno, E.; Calvo-Monroy, C.; Ríos-Santos, J.V.; Velasco-Ortega, E.; Sánchez-Domínguez, B.; Castellanos-Cosano, L.; Llamas-Carreras, J.M. Hypertension and Dental Periapical Condition. J. Endod. 2010, 36, 1800–1804. [Google Scholar] [CrossRef] [PubMed]
- Katz, J.; Rotstein, I. Prevalence of Periapical Abscesses in Patients with Hypertension: A Cross-Sectional Study of a Large Hospital Population. J. Endod. 2021, 47, 1070–1074. [Google Scholar] [CrossRef]
- Kim, J.; Kim, H.J.; Jeon, J.; Song, T.-J. Association between Oral Health and Cardiovascular Outcomes in Patients with Hypertension: A Nationwide Cohort Study. J. Hypertens. 2022, 40, 374–381. [Google Scholar] [CrossRef]
- Kumar, P.; Mastan, K.; Chowdhary, R.; Shanmugam, K. Oral Manifestations in Hypertensive Patients: A Clinical Study. J. Oral Maxillofac. Pathol. 2012, 16, 215–221. [Google Scholar] [CrossRef] [PubMed]
- Golpasand Hagh, L.; Zakavi, F.; Hajizadeh, F.; Saleki, M. The Association Between Hyperlipidemia and Periodontal Infection. Iran. Red Crescent Med. J. 2014, 16, e6577. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Hedayatnia, M.; Asadi, Z.; Zare-Feyzabadi, R.; Yaghooti-Khorasani, M.; Ghazizadeh, H.; Ghaffarian-Zirak, R.; Nosrati-Tirkani, A.; Mohammadi-Bajgiran, M.; Rohban, M.; Sadabadi, F.; et al. Dyslipidemia and Cardiovascular Disease Risk among the MASHAD Study Population. Lipids Health Dis. 2020, 19, 42. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.K.; Hwang, S.Y. Oral Health in Adults with Coronary Artery Disease and Its Risk Factors: A Comparative Study Using the Korea National Health and Nutrition Examination Survey Data. BMC Cardiovasc. Disord. 2021, 21, 71. [Google Scholar] [CrossRef] [PubMed]
- Miller, M. Dyslipidemia and Cardiovascular Risk: The Importance of Early Prevention. QJM 2009, 102, 657–667. [Google Scholar] [CrossRef]
- Keto, J.; Ventola, H.; Jokelainen, J.; Linden, K.; Keinänen-Kiukaanniemi, S.; Timonen, M.; Ylisaukko-oja, T.; Auvinen, J. Cardiovascular Disease Risk Factors in Relation to Smoking Behaviour and History: A Population-Based Cohort Study. Open Heart 2016, 3, e000358. [Google Scholar] [CrossRef]
- Joshipura, K.; Pitiphat, W.; Hung, H.; Willett, W.; Colditz, G.; Douglass, C. Pulpal Inflammation and Incidence of Coronary Heart Disease. J. Endod. 2006, 32, 99–103. [Google Scholar] [CrossRef]
- Colgate. Effects Of Smoking on Teeth. Available online: https://www.colgate.com/en-us/oral-health/threats-to-dental-health/effects-of-smoking-on-teeth (accessed on 5 April 2022).
- Wu, J.; Peters, B.A.; Dominianni, C.; Zhang, Y.; Pei, Z.; Yang, L.; Ma, Y.; Purdue, M.P.; Jacobs, E.J.; Gapstur, S.M.; et al. Cigarette Smoking and the Oral Microbiome in a Large Study of American Adults. ISME J. 2016, 10, 2435–2446. [Google Scholar] [CrossRef]
- EBSCOhost 24523838. Smoking and Oral Health Status. Available online: https://web.p.ebscohost.com/abstract?direct=true&profile=ehost&scope=site&authtype=crawler&jrnl=07098936&AN=24523838&h=sO2OdCJ3DINl10QKv6lEnMycRuBQCEW95M%2bHT0EQN%2bPcaSC%2bZBdHCc%2bM9lCZnXtEsuLosqFzMdMABwFfXOEsmA%3d%3d&crl=c&resultNs=AdminWebAuth&resultLocal=ErrCrlNotAuth&crlhashurl=login.aspx%3fdirect%3dtrue%26profile%3dehost%26scope%3dsite%26authtype%3dcrawler%26jrnl%3d07098936%26AN%3d24523838 (accessed on 17 April 2022).
- Telivuo, M.; Kallio, P.; Berg, M.-A.; Korhonen, H.J.; Murtomaa, H. Smoking and Oral Health: A Population Survey in Finland. J. Public Health Dent. 1995, 55, 133–138. [Google Scholar] [CrossRef]
- CDC. Tobacco Free Smoking, Gum Disease, and Tooth Loss. Available online: https://www.cdc.gov/tobacco/campaign/tips/diseases/periodontal-gum-disease.html (accessed on 17 April 2022).
- Komar, K.; Glavina, A.; Boras, V.V.; Verzak, Ž.; Brailo, V. Impact of Smoking on Oral Health: Knowledge and Attitudes of Croatian Dentists and Dental Students. Acta Stomatol. Croat. 2018, 52, 148–155. [Google Scholar] [CrossRef]
- Balto, H.A.; Alabdulaaly, L.; Bahammam, S.; Al-Ekrish, A.A. Comparative Analysis of Prevalence of Apical Periodontitis in Smokers and Non-Smokers Using Cone-Beam Computed Tomography. Saudi Dent. J. 2019, 31, 52–57. [Google Scholar] [CrossRef]
- Lofthag-Hansen, S.; Huumonen, S.; Gröndahl, K.; Gröndahl, H.-G. Limited Cone-Beam CT and Intraoral Radiography for the Diagnosis of Periapical Pathology. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2007, 103, 114–119. [Google Scholar] [CrossRef]
- Colić, M.; Gazivoda, D.; Vucević, D.; Vasilijić, S.; Rudolf, R.; Lukić, A. Proinflammatory and Immunoregulatory Mechanisms in Periapical Lesions. Mol. Immunol. 2009, 47, 101–113. [Google Scholar] [CrossRef]
- Martinho, F.C.; Chiesa, W.M.M.; Leite, F.R.M.; Cirelli, J.A.; Gomes, B.P.F.A. Correlation between Clinical/Radiographic Features and Inflammatory Cytokine Networks Produced by Macrophages Stimulated with Endodontic Content. J. Endod. 2012, 38, 740–745. [Google Scholar] [CrossRef]
- Virtanen, E.; Nurmi, T.; Söder, P.-Ö.; Airila-Månsson, S.; Söder, B.; Meurman, J.H. Apical Periodontitis Associates with Cardiovascular Diseases: A Cross-Sectional Study from Sweden. BMC Oral Health 2017, 17, 107. [Google Scholar] [CrossRef] [PubMed]
- Lin, P.-Y.; Chien, K.-L.; Chang, H.-J.; Chi, L.-Y. Unfinished Root Canal Treatments and the Risk of Cardiovascular Disease. J. Endod. 2015, 41, 1991–1996. [Google Scholar] [CrossRef] [PubMed]
- Gomes, B.; Lilley, J.; Drucker, D. Clinical Significance of Dental Root Canal Microflora. J. Dent. 1996, 24, 47–55. [Google Scholar] [CrossRef]
- Márton, I.; Kiss, C.; Balla, G.; Szabó, T.; Karmazsin, L. Acute Phase Proteins in Patients with Chronic Periapical Granuloma before and after Surgical Treatment. Oral Microbiol. Immunol. 1988, 3, 95–96. [Google Scholar] [CrossRef] [PubMed]
- Barkhordar, R.A.; Hayashi, C.; Hussain, M.Z. Detection of Interleukin-6 in Human Dental Pulp and Periapical Lesions. Endod. Dent. Traumatol. 1999, 15, 26–27. [Google Scholar] [CrossRef]
- Cotti, E.; Dessì, C.; Piras, A.; Flore, G.; Deidda, M.; Madeddu, C.; Zedda, A.; Longu, G.; Mercuro, G. Association of Endodontic Infection with Detection of an Initial Lesion to the Cardiovascular System. J. Endod. 2011, 37, 1624–1629. [Google Scholar] [CrossRef]
- Stennett, M.; Tsakos, G. The Impact of the COVID-19 Pandemic on Oral Health Inequalities and Access to Oral Healthcare in England. Br. Dent. J. 2022, 232, 109–114. [Google Scholar] [CrossRef] [PubMed]
- Glodny, B.; Nasseri, P.; Crismani, A.; Schoenherr, E.; Luger, A.K.; Bertl, K.; Petersen, J. The Occurrence of Dental Caries Is Associated with Atherosclerosis. Clinics 2013, 68, 946–953. [Google Scholar] [CrossRef]
- Suematsu, Y.; Miura, S.; Zhang, B.; Uehara, Y.; Ogawa, M.; Yonemoto, N.; Nonogi, H.; Nagao, K.; Kimura, T.; Saku, K. Association between Dental Caries and Out-of-Hospital Cardiac Arrests of Cardiac Origin in Japan. J. Cardiol. 2016, 67, 384–391. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Holm-Pedersen, P.; Avlund, K.; Morse, D.E.; Stoltze, K.; Katz, R.V.; Viitanen, M.; Winblad, B. Dental Caries, Periodontal Disease, and Cardiac Arrhythmias in Community-Dwelling Older Persons Aged 80 and Older: Is There a Link? J. Am. Geriatr. Soc. 2005, 53, 430–437. [Google Scholar] [CrossRef]
- Kelishadi, R.; Mortazavi, S.; Hossein, T.R.; Poursafa, P. Association of Cardiometabolic Risk Factors and Dental Caries in a Population-Based Sample of Youths. Diabetol. Metab. Syndr. 2010, 2, 22. [Google Scholar] [CrossRef]
- Sabharwal, A.; Stellrecht, E.; Scannapieco, F.A. Associations between Dental Caries and Systemic Diseases: A Scoping Review. BMC Oral Health 2021, 21, 472. [Google Scholar] [CrossRef] [PubMed]
- Ehnevid, H.; Jansson, L.; Lindskog, S.; Blomlöf, L. Periodontal Healing in Teeth with Periapical Lesions. A Clinical Retrospective Study. J. Clin. Periodontol. 1993, 20, 254–258. [Google Scholar] [CrossRef]
- Jansson, L.; Ehnevid, H.; Lindskog, S.; Blomlöf, L. The Influence of Endodontic Infection on Progression of Marginal Bone Loss in Periodontitis. J. Clin. Periodontol. 1995, 22, 729–734. [Google Scholar] [CrossRef]
- Helmi, M.; Goodson, J.M.; Hasturk, H.; Natto, Z.S. Annual Alveolar Bone Loss in Subjects with Cardiovascular Disease Adjusting for Associated Systemic Diseases and Risk Factors: A Retrospective Study. BMC Oral Health 2020, 20, 28. [Google Scholar] [CrossRef] [PubMed]
- Starkhammar Johansson, C.; Ravald, N.; Richter, A.; Pagonis, C. Periodontal Conditions in Patients with Coronary Heart Disease: A Case-Control Study. J. Clin. Periodontol. 2012, 35, 199–205. [Google Scholar] [CrossRef] [PubMed]
- Makkar, H.; Reynolds, M.A.; Wadhawan, A.; Dagdag, A.; Merchant, A.T.; Postolache, T.T. Periodontal, Metabolic, and Cardiovascular Disease: Exploring the Role of Inflammation and Mental Health. Pteridines 2018, 29, 124–163. [Google Scholar] [CrossRef]
- Kassebaum, N.J.; Bernabé, E.; Dahiya, M.; Bhandari, B.; Murray, C.J.L.; Marcenes, W. Global Burden of Severe Periodontitis in 1990–2010: A Systematic Review and Meta-Regression. J. Dent. Res. 2014, 93, 1045–1053. [Google Scholar] [CrossRef] [PubMed]
- Linden, G.J.; Lyons, A.; Scannapieco, F.A. Periodontal Systemic Associations: Review of the Evidence. J. Periodontol. 2013, 84, S8–S19. [Google Scholar] [CrossRef] [PubMed]
- Sharma, M.; Jindal, R.; Siddiqui, M.A.; Wangnoo, S.K. Diabetes and Periodontitis: A Medical Perspective. J. Int. Clin. Dent. Res. Organ. 2016, 8, 3. [Google Scholar] [CrossRef]
- Ling, M.R.; Chapple, I.L.C.; Matthews, J.B. Neutrophil Superoxide Release and Plasma C-Reactive Protein Levels Pre- and Post-Periodontal Therapy. J. Clin. Periodontol. 2016, 43, 652–658. [Google Scholar] [CrossRef]

| Inclusion Criteria | Exclusion Criteria |
|---|---|
| Patients who visited OPD of Institute of Dental Sciences and Department of Cardiology, IMS and SUM Hospital, | Patients with severe medical conditions and who were hospitalized |
| Patients between 40–80 years of age. | Patients with physical disabilities (mobility, visual, or hearing impairments) |
| Patients with primary dental experience or who required dental intervention | Any communication difficulties were noted on the patient’s record |
| Pregnant patients |
| Age Group | Group 1 (Control) | Group 2 (CVR) | Group 3 (CVD) | Total | χ2, p | ||||
|---|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | n | % | ||
| ≤50 | 62 | 60.8 | 52 | 23.4 | 21 | 25 | 135 | 33.1 | χ2 = 56.927 p = 0.000 |
| 51-60 | 27 | 26.5 | 70 | 31.5 | 29 | 34.5 | 126 | 30.9 | |
| 61-70 | 11 | 10.8 | 79 | 35.6 | 22 | 26.2 | 112 | 27.5 | |
| >70 | 2 | 2 | 21 | 9.5 | 12 | 14.3 | 35 | 8.6 | |
| Gender | |||||||||
| Male | 50 | 49 | 148 | 66.7 | 52 | 61.9 | 250 | 61.3 | χ2 = 9.190 p = 0.010 |
| Female | 52 | 51 | 74 | 33.3 | 32 | 38.1 | 158 | 38.7 | |
| Total | 102 | 100 | 222 | 100 | 84 | 100 | 408 | 100 | |
| DM | Group 1 (Control) | Group 2 (CVR) | Group 3 (CVD) | Total | χ2, p | ||||
|---|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | n | % | ||
| No | 102 | 100 | 94 | 42.3 | 49 | 58.3 | 245 | 60 | χ2 = 96.977 p = 0.000 |
| Yes | 0 | 0 | 128 | 57.7 | 35 | 41.7 | 163 | 40 | |
| χ2, p-value for association of DM with Gr. 2 and 3: χ2 = 6.260, p = 0.012 | |||||||||
| HTN | |||||||||
| No | 102 | 100 | 94 | 42.3 | 26 | 31 | 222 | 54.4 | χ2 = 117.133 p = 0.000 |
| Yes | 0 | 0 | 128 | 57.7 | 58 | 69 | 186 | 45.6 | |
| χ2, p-value for association of HTN with Gr. 2 and 3: χ2 = 3.317, p = 0.069 | |||||||||
| Dyslipidemia | |||||||||
| No | 102 | 100 | 217 | 97.7 | 45 | 53.6 | 364 | 89.2 | χ2 = 140.050 p = 0.000 |
| Yes | 0 | 0 | 5 | 2.3 | 39 | 46.4 | 44 | 10.8 | |
| χ2, p-value for association of dyslipidemia with Gr. 2 and 3: χ2 = 96.600, p = 0.000 | |||||||||
| Smoking | |||||||||
| No | 102 | 100 | 191 | 86 | 76 | 90.5 | 369 | 90.4 | χ2 = 15.764 p = 0.000 |
| Yes | 0 | 0 | 31 | 14 | 8 | 9.5 | 39 | 9.6 | |
| χ2, p-value for association of smoking with Gr. 2 and 3: χ2 = 1.080, p = 0.299 | |||||||||
| Total | 102 | 100 | 222 | 100 | 84 | 100 | 408 | 100 | |
| ASCVD Risk Factor | n | % |
|---|---|---|
| Low-risk (<5%) | 42 | 18.9 |
| Borderline risk (5% to 7.4%) | 23 | 10.4 |
| Intermediate risk (7.5% to 19.9%) | 86 | 38.7 |
| High risk (≥20%) | 71 | 32 |
| Total | 222 | 100 |
| Group 1 (Control) | Group 2 (CVR) | Group 3 (CVD) | Total | χ2, p | |||||
|---|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | n | % | ||
| Periapical radiolucency | |||||||||
| No radiolucency | 73 | 71.6 | 119 | 53.6 | 49 | 58.3 | 241 | 59.1 | χ2 = 9.353 p = 0.009 |
| Radiolucency | 29 | 28.4 | 103 | 46.4 | 35 | 41.7 | 167 | 40.9 | |
| χ2, p-value for Gr. 2 and 3: χ2 = 0.009, p = 0.922 | |||||||||
| Endodontically treated tooth | |||||||||
| No root canal filling | 84 | 82.4 | 152 | 68.5 | 58 | 69 | 294 | 72.1 | χ2 = 7.168 p= 0.028 |
| Root canal filling | 18 | 17.6 | 70 | 31.5 | 26 | 31 | 114 | 27.9 | |
| χ2, p-value for Gr. 2 and 3: χ2 = 0.009, p = 0.922 | |||||||||
| Caries severity | |||||||||
| None | 32 | 31.4 | 53 | 23.9 | 23 | 27.4 | 108 | 26.5 | χ2 = 2.064 p= 0.356 |
| Severity | 70 | 68.6 | 169 | 76.1 | 61 | 72.6 | 300 | 73.5 | |
| χ2, p-value for Gr. 2 and 3: χ2 = 0.402, p = 0.526 | |||||||||
| Tooth restoration | |||||||||
| None | 75 | 73.5 | 138 | 62.2 | 50 | 59.5 | 263 | 64.5 | χ2 = 5.067 p = 0.079 |
| Restoration | 27 | 26.5 | 84 | 37.8 | 34 | 40.5 | 145 | 35.5 | |
| χ2, p-value for Gr. 2 and 3: χ2 = 0.179, p = 0.672 | |||||||||
| Periodontal bone loss | |||||||||
| No loss | 68 | 66.7 | 64 | 28.8 | 29 | 34.5 | 161 | 39.5 | χ2 = 42.964 p = 0.000 |
| Loss | 34 | 33.3 | 158 | 71.2 | 55 | 65.5 | 247 | 60.5 | |
| χ2, p-value for Gr. 2 and 3: χ2 = 0.934, p = 0.334 | |||||||||
| Total | 102 | 100 | 222 | 100 | 84 | 100 | 408 | 100 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Dash, G.; Mishra, L.; Singh, N.R.; Behera, R.; Misra, S.R.; Kumar, M.; Sokolowski, K.; Agarwal, K.; Behera, S.K.; Mishra, S.; et al. Prevalence and Quality of Endodontic Treatment in Patients with Cardiovascular Disease and Associated Risk Factors. J. Clin. Med. 2022, 11, 6046. https://doi.org/10.3390/jcm11206046
Dash G, Mishra L, Singh NR, Behera R, Misra SR, Kumar M, Sokolowski K, Agarwal K, Behera SK, Mishra S, et al. Prevalence and Quality of Endodontic Treatment in Patients with Cardiovascular Disease and Associated Risk Factors. Journal of Clinical Medicine. 2022; 11(20):6046. https://doi.org/10.3390/jcm11206046
Chicago/Turabian StyleDash, Gathani, Lora Mishra, Naomi Ranjan Singh, Rini Behera, Satya Ranjan Misra, Manoj Kumar, Krzysztof Sokolowski, Kunal Agarwal, Suresh Kumar Behera, Sunil Mishra, and et al. 2022. "Prevalence and Quality of Endodontic Treatment in Patients with Cardiovascular Disease and Associated Risk Factors" Journal of Clinical Medicine 11, no. 20: 6046. https://doi.org/10.3390/jcm11206046
APA StyleDash, G., Mishra, L., Singh, N. R., Behera, R., Misra, S. R., Kumar, M., Sokolowski, K., Agarwal, K., Behera, S. K., Mishra, S., & Lapinska, B. (2022). Prevalence and Quality of Endodontic Treatment in Patients with Cardiovascular Disease and Associated Risk Factors. Journal of Clinical Medicine, 11(20), 6046. https://doi.org/10.3390/jcm11206046






