Robot-Assisted versus Trans-Umbilical Multiport Laparoscopic Ureteral Reimplantation for Pediatric Benign Distal Ureteral Stricture: Mid-Term Results at a Single Center
Abstract
1. Introduction
2. Patients and Methods
2.1. Patient Selection
2.2. Data Collection
2.3. Ethical Statement
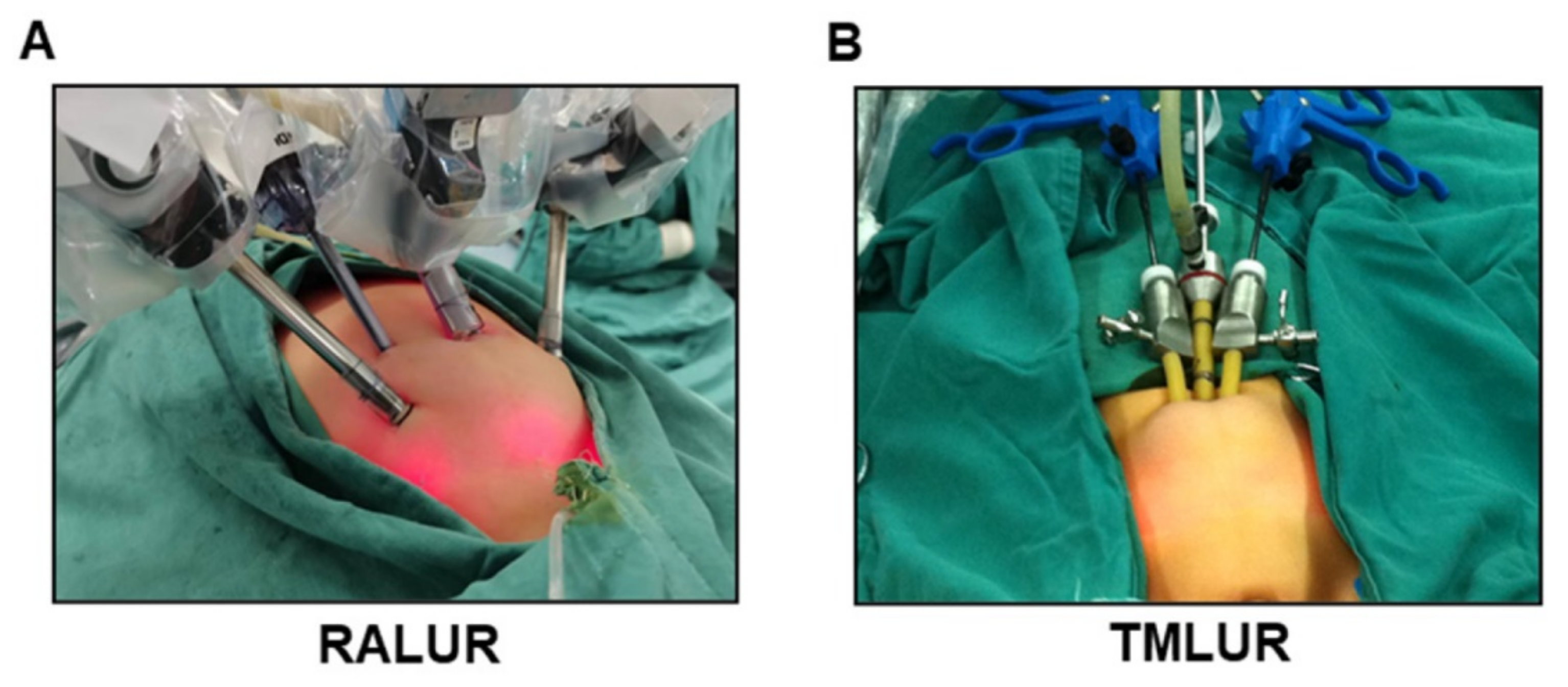
2.4. Surgical Techniques
2.5. Statistical Analysis
3. Results
3.1. Patient Demographics and Clinical Features
3.2. Comparison of Intra-Operative Characteristics in RALUR and TMLUR Groups
3.3. Comparison of Post-Operative Complications in RALUR and TMLUR Groups
3.4. Comparison of Follow-Up Data in RALUR and TMLUR Groups
4. Discussion
5. Conclusions
6. Limitations
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Kannaiyan, L.; Karl, S.; Mathai, J.; Chacko, J.; Sen, S. Congenital ureteric stenosis: A study of 17 children. Pediatr. Surg. Int. 2009, 256, 513–517. [Google Scholar] [CrossRef] [PubMed]
- Thergaonkar, R.W.; Hari, P. Current Management of Urinary Tract Infection and Vesicoureteral Reflux. Indian J. Pediatr. 2020, 878, 625–632. [Google Scholar] [CrossRef]
- Patil, N.; Javali, T. Application of the “Yang-Monti principle” in children with iatrogenic ureteral injuries. J. Pediatr. Urol. 2021, 174, 543.e1–543.e7. [Google Scholar] [CrossRef] [PubMed]
- Asghar, A.M.; Lee, R.A.; Yang, K.K.; Metro, M.; Eun, D.D. Robot-assisted distal ureteral reconstruction for benign pathology: Current state. Investig. Clin. Urol. 2020, 61 (Suppl. 1), S23–S32. [Google Scholar] [CrossRef] [PubMed]
- White, C.; Stifelman, M. Ureteral Reimplantation, Psoas Hitch, and Boari Flap. J. Endourol. 2020, 34, S25–S30. [Google Scholar] [CrossRef]
- Bowen, D.K.; Faasse, M.A.; Liu, D.B.; Gong, E.M.; Lindgren, B.W.; Johnson, E.K. Use of Pediatric Open, Laparoscopic and Robot-Assisted Laparoscopic Ureteral Reimplantation in the United States: 2000 to 2012. J. Urol. 2016, 1961, 207–212. [Google Scholar] [CrossRef]
- Winfield, H.N.; Donovan, J.F.; See, W.A.; Loening, S.A.; Williams, R.D. Urological Laparoscopic Surgery. J. Urol. 1991, 1464, 941–948. [Google Scholar] [CrossRef]
- Soulier, V.; Scalabre, A.L.; Lopez, M.; Li, C.Y.; Thach, S.; Vermersch, S.; Varlet, F.O. Laparoscopic vesico-ureteral reimplantation with Lich-Gregoir approach in children: Medium term results of 159 renal units in 117 children. World J. Urol. 2017, 3511, 1791–1798. [Google Scholar] [CrossRef]
- Zhang, Y.O.W.; Xu, H.; Luan, Y.; Yang, J.; Lu, Y.; Hu, J.; Liu, Z.; Yu, X.; Guan, W.; Hu, Z.; et al. A Comparison of Robot-Assisted Laparoscopic Ureteral Reimplantation and Conventional Laparoscopic Ureteral Reimplantation for the Management of Benign Distal Ureteral Stricture. Urol. J. 2020, 173, 252–256. [Google Scholar]
- Yang, K.K.; Asghar, A.M.; Lee, R.A.; Strauss, D.; Kuppa, S.; Lee, Z.; Metro, M.; Eun, D.D. Robot-Assisted Laparoscopic Distal Ureteroureterostomy for Distal Benign Ureteral Strictures with Long-Term Follow-Up. J. Endourol. 2022, 362, 203–208. [Google Scholar] [CrossRef]
- Koehne, E.; Desai, S.; Lindgren, B. Robot-assisted laparoscopic diverticulectomy with ureteral reimplantation. J. Pediatr. Urol. 2020, 164, 508–509. [Google Scholar] [CrossRef]
- Dell’Oglio, P.; Palagonia, E.; Wisz, P.; Andras, I.; De Groote, R.; Poelaert, F.; Beato, S.; Goossens, M.; Schatteman, P.; D’Hondt, F.; et al. Robot-assisted Boari flap and psoas hitch ureteric reimplantation: Technique insight and outcomes of a case series with >/=1 year of follow-up. BJU Int. 2021, 1285, 625–633. [Google Scholar] [CrossRef]
- Banuelos Marco, B.; Haid, B.; Radford, A.; Knoll, T.; Sultan, S.; Spinoit, A.F.; Hiess, M.; Sforza, S.; Lammers, R.J.M.; t Hoen, L.A.; et al. Guideline Adherence of Paediatric Urolithiasis: An EAU Members’ Survey and Expert Panel Roundtable Discussion. Children 2022, 9, 504. [Google Scholar] [CrossRef]
- Kelly, P.J.; Kyngdon, F.; Ingram, I.; Deane, F.P.; Baker, A.L.; Osborne, B.A. The Client Satisfaction Questionnaire-8: Psychometric properties in a cross-sectional survey of people attending residential substance abuse treatment. Drug Alcohol Rev. 2018, 371, 79–86. [Google Scholar] [CrossRef]
- Naseri, M.K.M.; Bakhtiari, E.; Tafazoli, N.; Alamdaran, S.A.; Tafazoli, N. Diagnostic Values of Kidney Ultrasonography for Vesicoureteral Reflux (VUR) and High Grade VUR. Iran. J. Kidney Dis. 2021, 5, 328–335. [Google Scholar]
- Kirsch, A.J.; Arlen, A.M. Evolving surgical management of pediatric vesicoureteral reflux: Is open ureteral reimplantation still the ‘Gold Standard’? Int. Braz. J. Urol. 2020, 463, 314–321. [Google Scholar] [CrossRef]
- Su, J.; Wang, N.; Zhu, Q.; Yuan, L.; Zhang, Y.; Deng, Z. Initial experience of transurethal assisted laparoendoscopic single-site nephroureterectomy. Asian J. Surg. 2022. [Google Scholar] [CrossRef]
- Naitoh, Y.; Ajiki, J.; Yamada, Y.; Fujihara, A.; Hongo, F.; Ukimura, O. Comparison of the initial operative experience of a single surgeon carrying out robot-assisted laparoscopic pyeloplasty, laparoendoscopic single-site pyeloplasty and conventional laparoscopic pyeloplasty. Int. J. Urol. 2020, 272, 186–187. [Google Scholar] [CrossRef]
- Abdel-Karim, A.M.; El Tayeb, M.M.; Yahia, E.; Elmissiry, M.; Hassouna, M.; Elsalmy, S. Evaluation of the Role of Laparoendoscopic Single-Site Surgery vs Minilaparoscopy for Treatment of Upper Urinary Tract Pathologies: Prospective Randomized Comparative Study. J. Endourol. 2017, 3112, 1237–1242. [Google Scholar] [CrossRef]
- Mei, H.; Pu, J.; Qi, T.; Qi, M.; Li, D.; Tang, S.; Zheng, L.; Tong, Q. Transumbilical multiport laparoscopic orchiopexy in children: Comparison with standard laparoscopic orchiopexy. Urology 2012, 806, 1345–1349. [Google Scholar] [CrossRef]
- Mei, H.; Qi, T.; Li, S.; Pu, J.; Cao, G.; Tang, S.; Zheng, L.; Tong, Q. Transumbilical multiport laparoscopic nephroureterectomy for congenital renal dysplasia in children: Midterm follow-up from a single institution. Front. Pediatr. 2013, 1, 46. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Mei, H.; Zhao, X.; Li, D.; Fang, E.; Wang, X.; Song, H.; Pu, J.; Zheng, L.; Tong, Q. Comparison of transumbilical multiport and standard laparoscopic pyeloplasty in children: Mid-term results at a single center. J. Pediatr. Surg. 2017, 523, 473–477. [Google Scholar] [CrossRef] [PubMed]
- Baldie, K.; Angell, J.; Ogan, K.; Hood, N.; Pattaras, J.G. Robotic management of benign mid and distal ureteral strictures and comparison with laparoscopic approaches at a single institution. Urology 2012, 803, 596–601. [Google Scholar] [CrossRef] [PubMed]
- Javali, T.; Pathade, A.; Nagaraj, H.K. Laparoscopic extravesical detrusorraphy, a minimally invasive treatment option for vesicoureteral reflux: A single centre experience. J. Pediatr. Urol. 2015, 112, 88.e1–88.e6. [Google Scholar] [CrossRef]
- Gundeti, M.S.; Boysen, W.R.; Shah, A. Robot-assisted Laparoscopic Extravesical Ureteral Reimplantation: Technique Modifications Contribute to Optimized Outcomes. Eur. Urol. 2016, 705, 818–823. [Google Scholar] [CrossRef]
- Sahadev, R.; Spencer, K.; Srinivasan, A.K.; Long, C.J.; Shukla, A.R. The Robot-Assisted Extravesical Anti-reflux Surgery: How We Overcame the Learning Curve. Front. Pediatr. 2019, 7, 93. [Google Scholar] [CrossRef]
- Dobbs, R.W.; Magnan, B.P.; Abhyankar, N.; Hemal, A.K.; Challacombe, B.; Hu, J.; Dasgupta, P.; Porpiglia, F.; Crivellaro, S. Cost effectiveness and robot-assisted urologic surgery: Does it make dollars and sense? Minerva Urol. Nefrol. 2017, 694, 313–323. [Google Scholar] [CrossRef]


| RALUR | TMLUR | p Value | |
|---|---|---|---|
| Case number | 28 | 28 | NA |
| Age (months) | 57.48 ± 30.66 | 52.62 ± 25.52 | 0.522 |
| (Range 12.0–142.0) | (Range 10.0–115.5) | ||
| Gender (F/M) | 20/8 | 18/10 | 0.567 |
| BMI | 23.22 ± 1.84 | 22.75 ± 1.50 | 0.298 |
| Laterality | 0.584 | ||
| Left | 16 (57.1%) | 18 (64.3%) | |
| Right | 12 (42.9%) | 10 (35.7%) | |
| Etiology | 0.495 | ||
| Congenital | 21 (75.0%) | 23 (82.1%) | |
| Urolithiasis | 5 (17.9%) | 3 (10.7%) | |
| Infection | 2 (7.1%) | 2 (7.1%) | |
| Length (cm) | 0.64 ± 0.15 | 0.60 ± 0.22 | 0.720 |
| Clinical presentation | 0.577 | ||
| Yes | 19 (67.9%) | 17 (60.7%) | |
| Fever | 6 | 6 | |
| Flank pain | 12 | 10 | |
| UTI | 14 | 15 | |
| No | 9 (32.1%) | 11 (39.3%) | |
| Urinalysis/urine culture | 18 (64.3%) | 19 (67.9%) | 0.778 |
| Ultrasonography | 30.10 ± 6.55 | 29.11 ± 7.44 | 0.600 |
| 99mTc-DTPA renal scan of affected side | 0.501 | ||
| HMT > 20 min | 18 (64.3%) | 17 (60.7%) | |
| HMT 15–20 min | 10 (35.7%) | 11 (39.3%) | |
| eGFR of affected side | 58.11 ± 9.77 | 59.36 ± 11.11 | 0.657 |
| SCr (μmol/L) | 43.71 ± 10.46 | 44.13 ± 9.64 | 0.478 |
| RALUR | TMLUR | p Value | |
|---|---|---|---|
| Case number | 28 | 28 | NA |
| Operative time (minutes) | 127.11 ± 13.57 | 138.39 ± 14.99 | 0.005 |
| Estimated blood loss (ml) | 18.57 ± 6.06 | 26.07 ± 9.36 | 0.001 |
| D-J placement | 28 | 28 | NA |
| Conversion to open | 0 | 0 | NA |
| Oral feeding time (hours) | 34.61 ± 6.01 | 35.82 ± 5.36 | 0.428 |
| Length of stay (days) | 6.07 ± 1.18 | 6.71 ± 1.49 | 0.079 |
| Vas pain score at postoperative day 1 | 3.50 ± 1.19 | 3.18 ± 1.06 | 0.289 |
| Parents satisfaction score | 30.07 ± 1.70 | 29.54 ± 2.13 | 0.303 |
| Catheter removal (days) | 5.14 ± 0.93 | 5.36 ± 1.06 | 0.426 |
| Postoperative Complication | |||
| Wound infection | 0 | 0 | NA |
| Hernia formation | 0 | 0 | NA |
| Urinary leakage | 0 | 1 (3.6%) | 0.313 |
| Subcutaneous emphysema | 4 (14.3%) | 2 (7.1%) | 0.388 |
| Internal organ damage | 0 | 0 | NA |
| Stent migration | 0 | 0 | NA |
| Hospitalization expenses | 43108.44 ± 2753.24 | 23265.45 ± 2673.99 | <0.001 |
| RALUR | TMLUR | p Value | |
|---|---|---|---|
| Case number | 28 | 28 | NA |
| Follow up in months | 18.29 ± 4.77 | 24.64 ± 4.65 | <0.001 |
| Symptom remissions | 18 (100%) | 14 (82.4%) | 0.075 |
| Urinalysis/urine culture | 2 (7.1%) * | 5 (17.9%) # | 0.225 |
| Ultrasonography | 13.77 ± 5.17 * | 14.33 ± 5.81 # | 0.704 |
| 99mTc-DTPA renal scan of affected side | 0.690 | ||
| HMT > 20 min | 0 * | 1 (3.6%) # | |
| HMT 15–20 min | 3 (10.7%) * | 1 (3.6%) # | |
| HMT < 15 min | 25 (89.3%) * | 26 (92.8%) # | |
| eGFR of affected side at 12 months postoperatively | 86.05 ± 10.99 * | 85.80 ± 12.32 # | 0.936 |
| SCr (μmol/L) | 44.09 ± 11.26 | 46.05 ± 10.88 | 0.307 |
| Anastomotic stenosis | 1 (3.6%) | 3 (10.7%) | 0.299 |
| VUR | 0.167 | ||
| GradeⅠ | 2 (7.2%) | 0 | |
| GradeⅡ | 1 (3.6%) | 2 (7.2%) | |
| Reoperation | 0 | 1 (3.6%) | 0.313 |
| Success rate | 28 (100.0%) | 27 (96.4%) | 0.313 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Guo, Y.; Cheng, Y.; Li, D.; Mei, H.; Jin, H.; Chen, G.; Hu, A.; Li, Q.; Du, X.; Zheng, L.; et al. Robot-Assisted versus Trans-Umbilical Multiport Laparoscopic Ureteral Reimplantation for Pediatric Benign Distal Ureteral Stricture: Mid-Term Results at a Single Center. J. Clin. Med. 2022, 11, 6229. https://doi.org/10.3390/jcm11216229
Guo Y, Cheng Y, Li D, Mei H, Jin H, Chen G, Hu A, Li Q, Du X, Zheng L, et al. Robot-Assisted versus Trans-Umbilical Multiport Laparoscopic Ureteral Reimplantation for Pediatric Benign Distal Ureteral Stricture: Mid-Term Results at a Single Center. Journal of Clinical Medicine. 2022; 11(21):6229. https://doi.org/10.3390/jcm11216229
Chicago/Turabian StyleGuo, Yanhua, Yang Cheng, Dan Li, Hong Mei, Huan Jin, Guo Chen, Anpei Hu, Qilan Li, Xinyi Du, Liduan Zheng, and et al. 2022. "Robot-Assisted versus Trans-Umbilical Multiport Laparoscopic Ureteral Reimplantation for Pediatric Benign Distal Ureteral Stricture: Mid-Term Results at a Single Center" Journal of Clinical Medicine 11, no. 21: 6229. https://doi.org/10.3390/jcm11216229
APA StyleGuo, Y., Cheng, Y., Li, D., Mei, H., Jin, H., Chen, G., Hu, A., Li, Q., Du, X., Zheng, L., & Tong, Q. (2022). Robot-Assisted versus Trans-Umbilical Multiport Laparoscopic Ureteral Reimplantation for Pediatric Benign Distal Ureteral Stricture: Mid-Term Results at a Single Center. Journal of Clinical Medicine, 11(21), 6229. https://doi.org/10.3390/jcm11216229





