Trans-Endothelial Migration of Memory T Cells Is Impaired in Alemtuzumab-Treated Multiple Sclerosis Patients
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Participants
2.2. PBMC Isolation from Whole Blood
2.3. Transmigration Assay
2.4. Spectral Flow Cytometry
2.5. Gating Strategy
2.6. Statistical Analysis
3. Results
3.1. CD4+ TEM and CD8+ TCM Cells from Alemtuzumab-Treated RRMS Patients Have Reduced Trans-Endothelial Migration
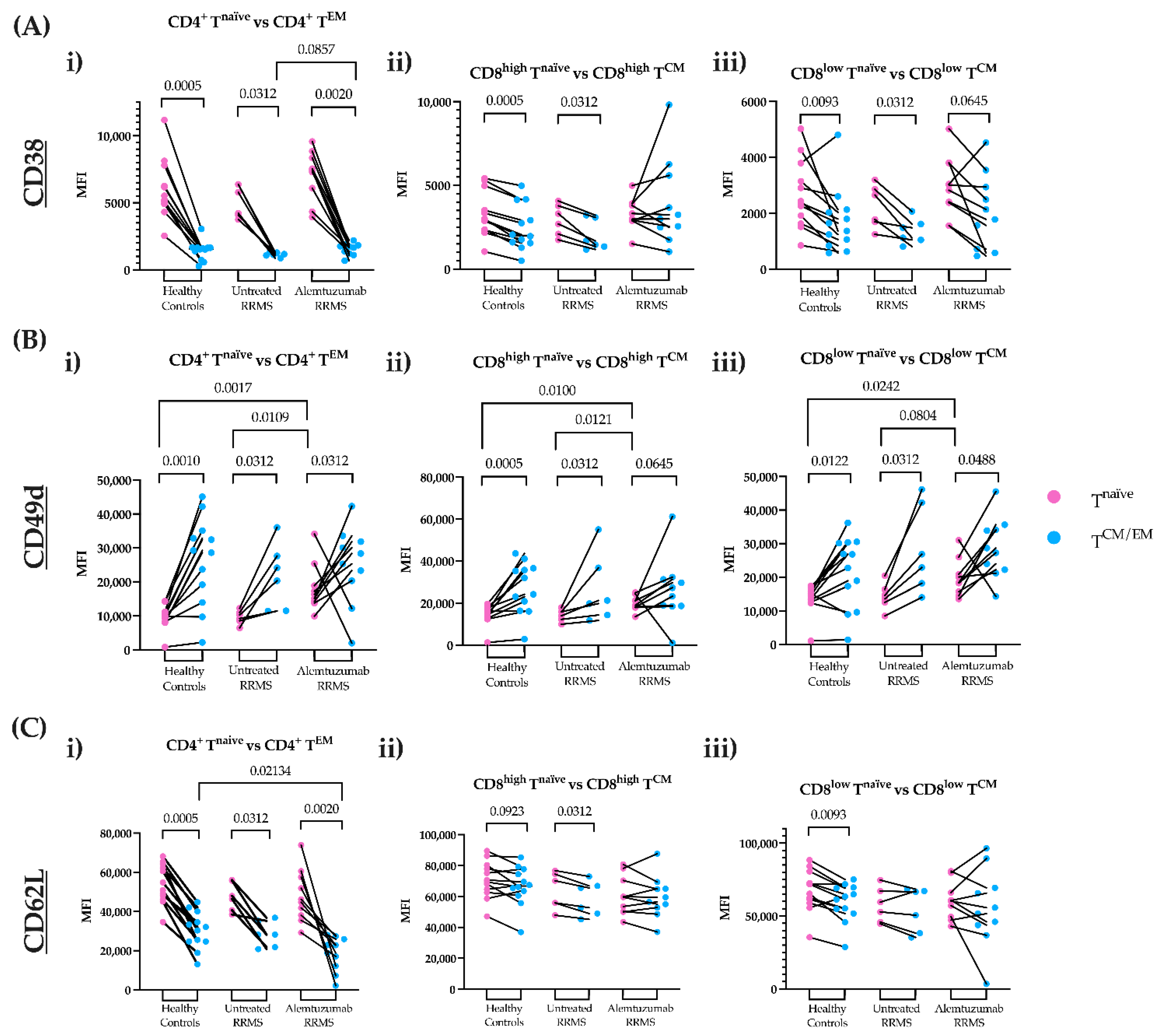
3.2. CD38 and CD62L Expression on CD4+ TEM and CD8+ TCM Cells Is Altered following Alemtuzumab
3.3. Alemtuzumab Significantly Depletes Circulating CD4+ TEM and CD8+ TCM Cell Numbers
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Gallo, P.; Centonze, D.; Marrosu, M.G. Alemtuzumab for multiple sclerosis: The new concept of immunomodulation. Mult. Scler. Demyelinating Disord. 2017, 2, 7. [Google Scholar] [CrossRef]
- Ruck, T.; Bittner, S.; Wiendl, H.; Meuth, S.G. Alemtuzumab in Multiple Sclerosis: Mechanism of Action and Beyond. Int. J. Mol. Sci. 2015, 16, 16414–16439. [Google Scholar] [CrossRef] [PubMed]
- Goverman, J. Autoimmune T cell responses in the central nervous system. Nat. Rev. Immunol. 2009, 9, 393–407. [Google Scholar] [CrossRef]
- McPherson, R.C.; Cambrook, H.E.; O’Connor, R.A.; Anderton, S.M. Induction of Passive EAE Using Myelin-Reactive CD4+ T Cells. Methods Mol. Biol. 2014, 1193, 187–198. [Google Scholar] [CrossRef]
- Prat, A.; Biernacki, K.; Lavoie, J.-F.; Poirier, J.; Duquette, P.; Antel, J. Migration of Multiple Sclerosis Lymphocytes through Brain Endothelium. Arch. Neurol. 2002, 59, 391–397. [Google Scholar] [CrossRef] [PubMed]
- Bahbouhi, B.; Berthelot, L.; Pettré, S.; Michel, L.; Wiertlewski, S.; Weksler, B.; Romero, I.-A.; Miller, F.; Couraud, P.-O.; Brouard, S.; et al. Peripheral blood CD4+ T lymphocytes from multiple sclerosis patients are characterized by higher PSGL-1 expression and transmigration capacity across a human blood-brain barrier-derived endothelial cell line. J. Leukoc. Biol. 2009, 86, 1049–1063. [Google Scholar] [CrossRef] [PubMed]
- Jones, J.L.; Thompson, S.; Loh, P.; Davies, J.L.; Tuohy, O.; Curry, A.; Azzopardi, L.; Hill-Cawthorne, G.; Fahey, M.T.; Compston, A.; et al. Human autoimmunity after lymphocyte depletion is caused by homeostatic T-cell proliferation. Proc. Natl. Acad. Sci. USA 2013, 110, 20200–20205. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.; Tao, Y.; Chopra, M.; Ahn, M.; Marcus, K.L.; Choudhary, N.; Zhu, H.; Markovic-Plese, S. Differential Reconstitution of T Cell Subsets following Immunodepleting Treatment with Alemtuzumab (Anti-CD52 Monoclonal Antibody) in Patients with Relapsing–Remitting Multiple Sclerosis. J. Immunol. 2013, 191, 5867–5874. [Google Scholar] [CrossRef] [PubMed]
- Turner, M.J.; Lamorte, M.J.; Chretien, N.; Havari, E.; Roberts, B.L.; Kaplan, J.M.; Siders, W.M. Immune status following alemtuzumab treatment in human CD52 transgenic mice. J. Neuroimmunol. 2013, 261, 29–36. [Google Scholar] [CrossRef] [PubMed]
- Coles, A.J.; Arnold, D.L.; Bass, A.D.; Boster, A.L.; Compston, D.A.S.; Fernández, Ó.; Havrdová, E.K.; Nakamura, K.; Traboulsee, A.; Ziemssen, T.; et al. Efficacy and safety of alemtuzumab over 6 years: Final results of the 4-year CARE-MS extension trial. Ther. Adv. Neurol. Disord. 2021, 14, 1–17. [Google Scholar] [CrossRef] [PubMed]
- Jones, J.L.; Coles, A.J. Mode of action and clinical studies with alemtuzumab. Exp. Neurol. 2014, 262, 37–43. [Google Scholar] [CrossRef]
- Prat, A.; Al-Asmi, A.; Duquette, P.; Antel, J. Lymphocyte migration and multiple sclerosis: Relation with disease course and therapy. Ann. Neurol. 1999, 46, 253–256. [Google Scholar] [CrossRef]
- Prat, A.; Biernacki, K.; Antel, J.P. Th1 and Th2 lymphocyte migration across the human BBB is specifically regulated by interferon beta and copolymer-1. J. Autoimmun. 2005, 2, 119–124. [Google Scholar] [CrossRef]
- Uhm, J.H.; Dooley, N.P.; Stuve, O.; Francis, G.S.; Duquette, P.; Antel, J.P.; Yong, V.W. Migratory behavior of lymphocytes isolated from multiple sclerosis patients: Effects of interferon beta-1b therapy. Ann. Neurol. 1999, 46, 319–324. [Google Scholar] [CrossRef]
- Hawke, S.; Zinger, A.; Juillard, P.-G.; Holdaway, K.; Byrne, S.N.; Grau, G.E. Selective modulation of trans-endothelial migration of lymphocyte subsets in multiple sclerosis patients under fingolimod treatment. J. Neuroimmunol. 2020, 349, 577392. [Google Scholar] [CrossRef]
- Kopadze, T.; Döbert, M.; Leussink, V.I.; Dehmel, T.; Kieseier, B.C. Cladribine impedes in vitro migration of mononuclear cells: A possible implication for treating multiple sclerosis. Eur. J. Neurol. 2009, 16, 409–412. [Google Scholar] [CrossRef] [PubMed]
- Havari, E.; Turner, M.J.; Dodge, J.C.; Treleaven, C.; Shihabuddin, L.S.; Roberts, B.L.; Kaplan, J.M.; Siders, W.M. Anti-murine CD52 antibody treatment does not adversely affect the migratory ability of immune cells. J. Neuroimmunol. 2014, 275, 62–63. [Google Scholar] [CrossRef]
- Knudsen, M.H.; Lindberg, U.; Frederiksen, J.L.; Vestergaard, M.B.; Simonsen, H.J.; Varatharaj, A.; Galea, I.; Blinkenberg, M.; Sellebjerg, F.; Larsson, H.B.W.; et al. Blood-brain barrier permeability changes in the first year after alemtuzumab treatment predict 2-year outcomes in relapsing-remitting multiple sclerosis. Mult. Scler. Relat. Disord. 2022, 63, 103891. [Google Scholar] [CrossRef] [PubMed]
- Rolla, S.; Maglione, A.; De Mercanti, S.F.; Clerico, M. The Meaning of Immune Reconstitution after Alemtuzumab Therapy in Multiple Sclerosis. Cells 2020, 9, 1396. [Google Scholar] [CrossRef] [PubMed]
- Berard, M.; Tough, D.F. Qualitative differences between naive and memory T cells. Immunology 2002, 106, 127–138. [Google Scholar] [CrossRef] [PubMed]
- Thompson, A.J.; Banwell, B.L.; Barkhof, F.; Carroll, W.M.; Coetzee, T.; Comi, G.; Correale, J.; Fazekas, F.; Filippi, M.; Freedman, M.S.; et al. Diagnosis of multiple sclerosis: 2017 revisions of the McDonald criteria. Lancet Neurol. 2018, 17, 162–173. [Google Scholar] [CrossRef]
- Izad, M.; Harirchian, M.H.; Amiri, H.; Najafi, F.; Ghaflati, Z.; Salehi, Z. Low and high CD8 positive T cells in multiple sclerosis patients. Iran. J. Allergy Asthma Immunol. 2013, 12, 276–280. [Google Scholar] [PubMed]
- Chiarini, M.; Capra, R.; Serana, F.; Bertoli, D.; Sottini, A.; Giustini, V.; Scarpazza, C.; Rovaris, M.; Clerici, V.T.; Ferraro, D.; et al. Simultaneous quantification of natural and inducible regulatory T-cell subsets during interferon-β therapy of multiple sclerosis patients. J. Transl. Med. 2020, 18, 169. [Google Scholar] [CrossRef] [PubMed]
- Schenkel, J.M.; Fraser, K.A.; Casey, K.A.; Beura, L.K.; Pauken, K.E.; Vezys, V.; Masopust, D. IL-15-Independent Maintenance of Tissue-Resident and Boosted Effector Memory CD8 T Cells. J. Immunol. 2016, 196, 3920–3926. [Google Scholar] [CrossRef]
- Clénet, M.-L.; Gagnon, F.; Moratalla, A.C.; Viel, E.C.; Arbour, N. Peripheral human CD4+CD8+ T lymphocytes exhibit a memory phenotype and enhanced responses to IL-2, IL-7 and IL-15. Sci. Rep. 2017, 7, 11612. [Google Scholar] [CrossRef]
- De Mercanti, S.; Rolla, S.; Cucci, A.; Bardina, V.; Cocco, E.; Vladic, A.; Soldo-Butkovic, S.; Habek, M.; Adamec, I.; Horakova, D.; et al. Alemtuzumab long-term immunologic effect. Am. Acad. Neurol. 2016, 3, 194. [Google Scholar] [CrossRef]
- Smeltz, R.B. Profound enhancement of the IL-12/IL-18 pathway of IFN-gamma secretion in human CD8+ memory T cell subsets via IL-15. J. Immunol. 2007, 178, 4786–4792. [Google Scholar] [CrossRef]
- Sallusto, F.; Lenig, D.; Forster, R.; Lipp, M.; Lanzavecchia, A. Two subsets of memory T lymphocytes with distinct homing potentials and effector functions. Nature 1999, 401, 708–712. [Google Scholar] [CrossRef]
- Grage-Griebenow, E.; Flad, H.; Ernst, M. Heterogeneity of human peripheral blood monocyte subsets. J. Leukoc. Biol. 2001, 69, 11–20. [Google Scholar] [CrossRef]
- Tenca, C.; Merlo, A.; Zarcone, D.; Saverino, D.; Bruno, S.; De Santanna, A.; Ramarli, D.; Fabbi, M.; Pesce, C.; Deaglio, S.; et al. Death of T cell precursors in the human thymus: A role for CD38. Int. Immunol. 2003, 15, 1105–1116. [Google Scholar] [CrossRef]
- Sandoval-Montes, C.; Santos-Argumedo, L. CD38 is expressed selectively during the activation of a subset of mature T cells with reduced proliferation but improved potential to produce cytokines. J. Leukoc. Biol. 2004, 77, 513–521. [Google Scholar] [CrossRef] [PubMed]
- Piedra-Quintero, Z.L.; Wilson, Z.; Nava, P.; Guerau-De-Arellano, M. CD38: An Immunomodulatory Molecule in Inflammation and Autoimmunity. Front. Immunol. 2020, 11, 597959. [Google Scholar] [CrossRef] [PubMed]
- Bahri, R.; Bollinger, A.; Bollinger, T.; Orinska, Z.; Bulfone-Paus, S. Ectonucleotidase CD38 Demarcates Regulatory, Memory-Like CD8+ T Cells with IFN-γ-Mediated Suppressor Activities. PLoS ONE 2012, 7, e45234. [Google Scholar] [CrossRef] [PubMed]
- Centonze, D.; Muzio, L.; Rossi, S.; Cavasinni, F.; De Chiara, V.; Bergami, A.; Musella, A.; D’Amelio, M.; Cavallucci, V.; Martorana, A.; et al. Inflammation Triggers Synaptic Alteration and Degeneration in Experimental Autoimmune Encephalomyelitis. J. Neurosci. 2009, 29, 3442–3452. [Google Scholar] [CrossRef] [PubMed]
- Piccio, L.; Rossi, B.; Scarpini, E.; Laudanna, C.; Giagulli, C.; Issekutz, A.C.; Vestweber, D.; Butcher, E.C.; Constantin, G. Molecular mechanisms involved in lymphocyte recruitment in inflamed brain microvessels: Critical roles for P-selectin glycoprotein ligand-1 and heterotrimeric G-linked receptors. J. Immunol. 2002, 168, 1940–1949. [Google Scholar] [CrossRef]
- Arana, E.; Harwood, N.E.; Batista, F.D. Regulation of integrin activation through the B-cell receptor. J. Cell Sci. 2008, 121, 2279–2286. [Google Scholar] [CrossRef]
- Defer, G.; Mariotte, D.; Derache, N.; Toutirais, O.; Legros, H.; Cauquelin, B.; Le Mauff, B. CD49d expression as a promising biomarker to monitor natalizumab efficacy. J. Neurol. Sci. 2012, 314, 138–142. [Google Scholar] [CrossRef]
- Galkina, E.; Tanousis, K.; Preece, G.; Tolaini, M.; Kioussis, D.; Florey, O.; Haskard, D.O.; Tedder, T.F.; Ager, A. L-Selectin Shedding Does Not Regulate Constitutive T Cell Trafficking but Controls the Migration Pathways of Antigen-activated T Lymphocytes. J. Exp. Med. 2003, 198, 1323–1335. [Google Scholar] [CrossRef]
- Yang, S.; Liu, F.; Wang, Q.J.; Rosenberg, S.A.; Morgan, R.A. The shedding of CD62L (L-Selectin) regulates the acquisition of lytic activity in human tumor reactive T lymphocytes. PLoS ONE 2011, 6, e22560. [Google Scholar] [CrossRef]
- Freedman, M.S.; Kaplan, J.M.; Markovic-Plese, S. Insights into the Mechanisms of the Therapeutic Efficacy of Alemtuzumab in Multiple Sclerosis. J. Clin. Cell. Immunol. 2013, 4, 1000152. [Google Scholar] [CrossRef]
- Baker, D.; Herrod, S.S.; Alvarez-Gonzaález, C.; Giovannoni, G.; Schmierer, K. Interpreting Lymphocyte Reconstitution Data from the Pivotal Phase 3 Trials of Alemtuzumab. JAMA Neurol. 2017, 74, 961–969. [Google Scholar] [CrossRef] [PubMed]
- Eugenin, E.A.; Berman, J.W. Chemokine-dependent mechanisms of leukocyte trafficking across a model of the blood-brain barrier. Methods 2003, 29, 351–361. [Google Scholar] [CrossRef]
- Schulte-Mecklenbeck, A.; Bhatia, U.; Schneider-Hohendorf, T.; Schwab, N.; Wiendl, H.; Gross, C.C. Analysis of Lymphocyte Extravasation Using an In Vitro Model of the Human Blood-brain Barrier. J. Vis. Exp. 2017, 122, 55390. [Google Scholar] [CrossRef]
- Engelhardt, B.; Ransohoff, R.M. The ins and outs of T-lymphocyte trafficking to the CNS: Anatomical sites and molecular mechanisms. Trends Immunol. 2005, 26, 485–495. [Google Scholar] [CrossRef] [PubMed]


| MS ID | Sex (62.5% F) | Age * (Median = 42.6) | Disease Duration (Years) * | Months Since First Dose | Previous Treatment | Months Since Last Treatment Prior to Alemtuzumab | Active MS ** | |
|---|---|---|---|---|---|---|---|---|
| Prior | Post | |||||||
| MS01 | F | 36 | 9.3 | - | 21 | Azathioprine & intravenous immunoglobulin | 1 | Yes |
| MS02 | F | 40.2 | 6.9 | - | 11 | Dimethyl fumarate | 3 | Yes |
| MS03 | F | 38.9 | 5.9 | - | 12 | Fingolimod | 2 | Yes |
| MS04 | M | 55.2 | 3.1 | - | 19 | Fingolimod | 3 | |
| MS05 | M | 46.4 | 8.8 | - | 8 | Fingolimod | 2 | Yes |
| MS06 | M | 43.1 | 23.3 | - | 19 | Natalizumab | 1 | Yes |
| MS07 | M | 57.5 | 19.1 | - | 54 | Interferon beta & natalizumab | 3 | Yes |
| MS08 | F | 44.9 | 5.8 | - | 50 | Dimethyl fumarate | 2 | Yes |
| MS09 | F | 37.7 | 10.1 | - | 54 | Fingolimod & natalizumab | 3 | Yes |
| MS10 | F | 42.1 | 12.1 | - | 37 | Interferon beta, fingolimod & natalizumab | 2 | Yes |
| MS11 | F | 52 | 0.1 | ✓ | - | Mavenclad | - | Yes |
| MS12 | F | 28.3 | 0.3 | ✓ | - | None | - | Yes |
| MS13 | F | 37.9 | 6.3 | ✓ | - | None | - | Yes |
| MS14 | M | 29.6 | 0.1 | ✓ | - | None | - | Yes |
| MS15 | F | 61.7 | 24 | ✓ | - | None | - | Yes |
| MS16 | M | 47 | 0.1 | ✓ | - | None | - | Benign MS |
| Healthy Control ID | Sex (66% F) | Age * (Median = 38) | ||||||
| HC01 | F | 24 | ||||||
| HC02 | M | 26 | ||||||
| HC03 | M | 22 | ||||||
| HC04 | F | 35 | ||||||
| HC05 | F | 30 | ||||||
| HC06 | F | 41 | ||||||
| HC07 | M | 43 | ||||||
| HC08 | F | 56 | ||||||
| HC09 | F | 28 | ||||||
| HC10 | F | 42 | ||||||
| HC11 | M | 43 | ||||||
| HC12 | F | 41 | ||||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nguyen, K.; Juillard, P.; Hawke, S.; Grau, G.E.; Marsh-Wakefield, F. Trans-Endothelial Migration of Memory T Cells Is Impaired in Alemtuzumab-Treated Multiple Sclerosis Patients. J. Clin. Med. 2022, 11, 6266. https://doi.org/10.3390/jcm11216266
Nguyen K, Juillard P, Hawke S, Grau GE, Marsh-Wakefield F. Trans-Endothelial Migration of Memory T Cells Is Impaired in Alemtuzumab-Treated Multiple Sclerosis Patients. Journal of Clinical Medicine. 2022; 11(21):6266. https://doi.org/10.3390/jcm11216266
Chicago/Turabian StyleNguyen, Kristy, Pierre Juillard, Simon Hawke, Georges E. Grau, and Felix Marsh-Wakefield. 2022. "Trans-Endothelial Migration of Memory T Cells Is Impaired in Alemtuzumab-Treated Multiple Sclerosis Patients" Journal of Clinical Medicine 11, no. 21: 6266. https://doi.org/10.3390/jcm11216266
APA StyleNguyen, K., Juillard, P., Hawke, S., Grau, G. E., & Marsh-Wakefield, F. (2022). Trans-Endothelial Migration of Memory T Cells Is Impaired in Alemtuzumab-Treated Multiple Sclerosis Patients. Journal of Clinical Medicine, 11(21), 6266. https://doi.org/10.3390/jcm11216266






