Utilizing Three-Dimensional Head-Lesser Trochanter Distance Could Further Reduce Leg Length Inequality in Primary Bipolar Hemiarthroplasty
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Patients Group
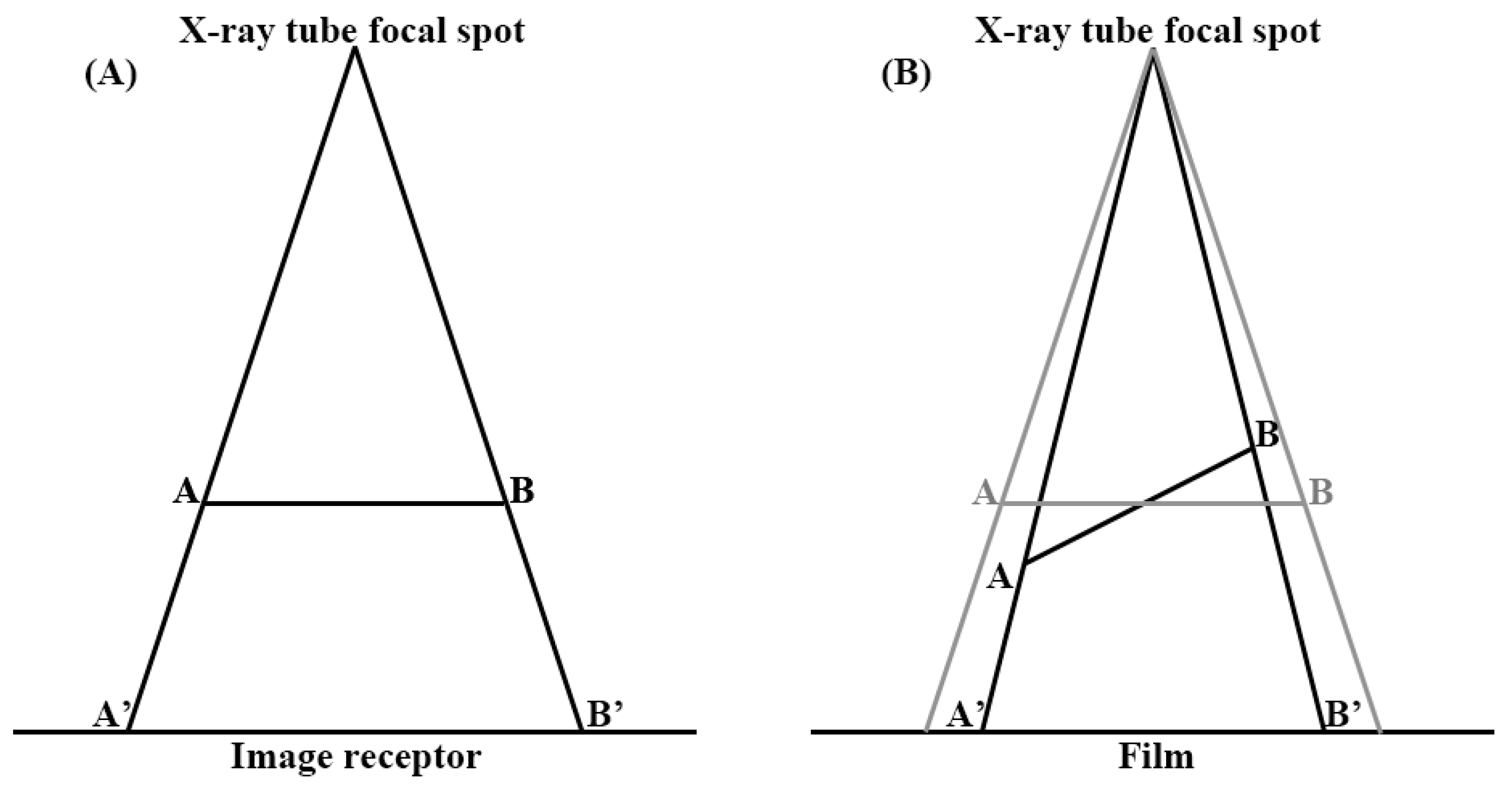
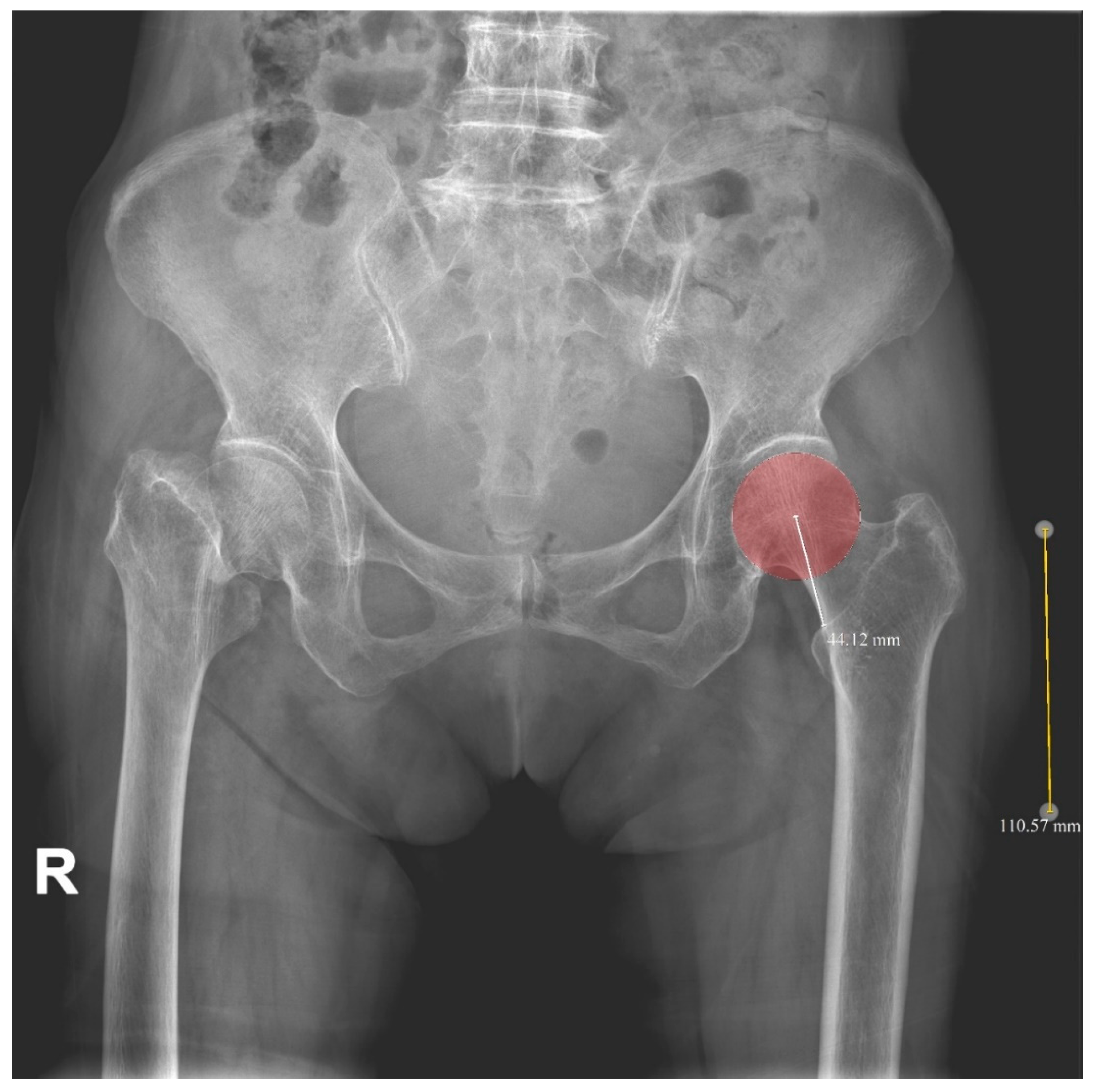
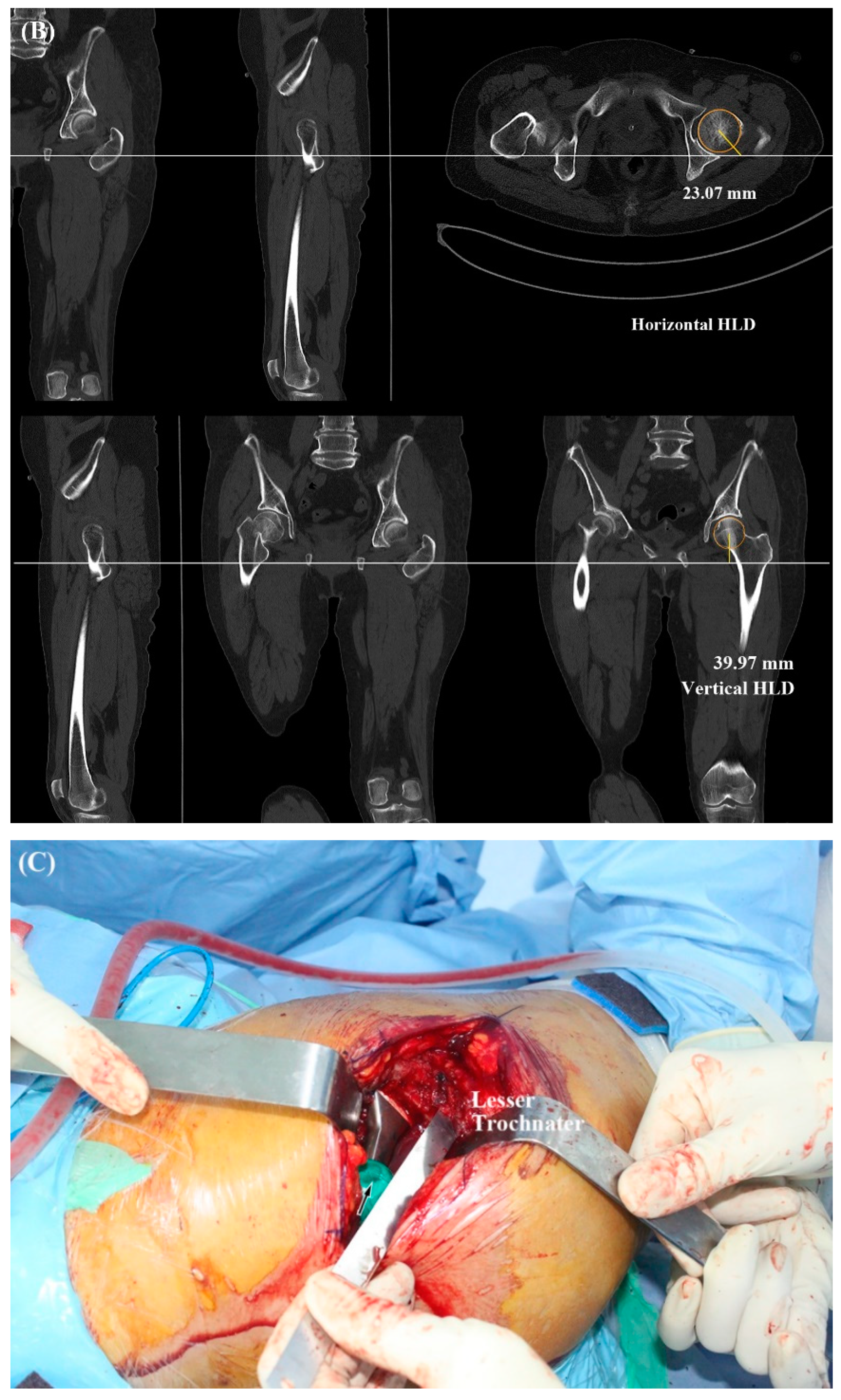
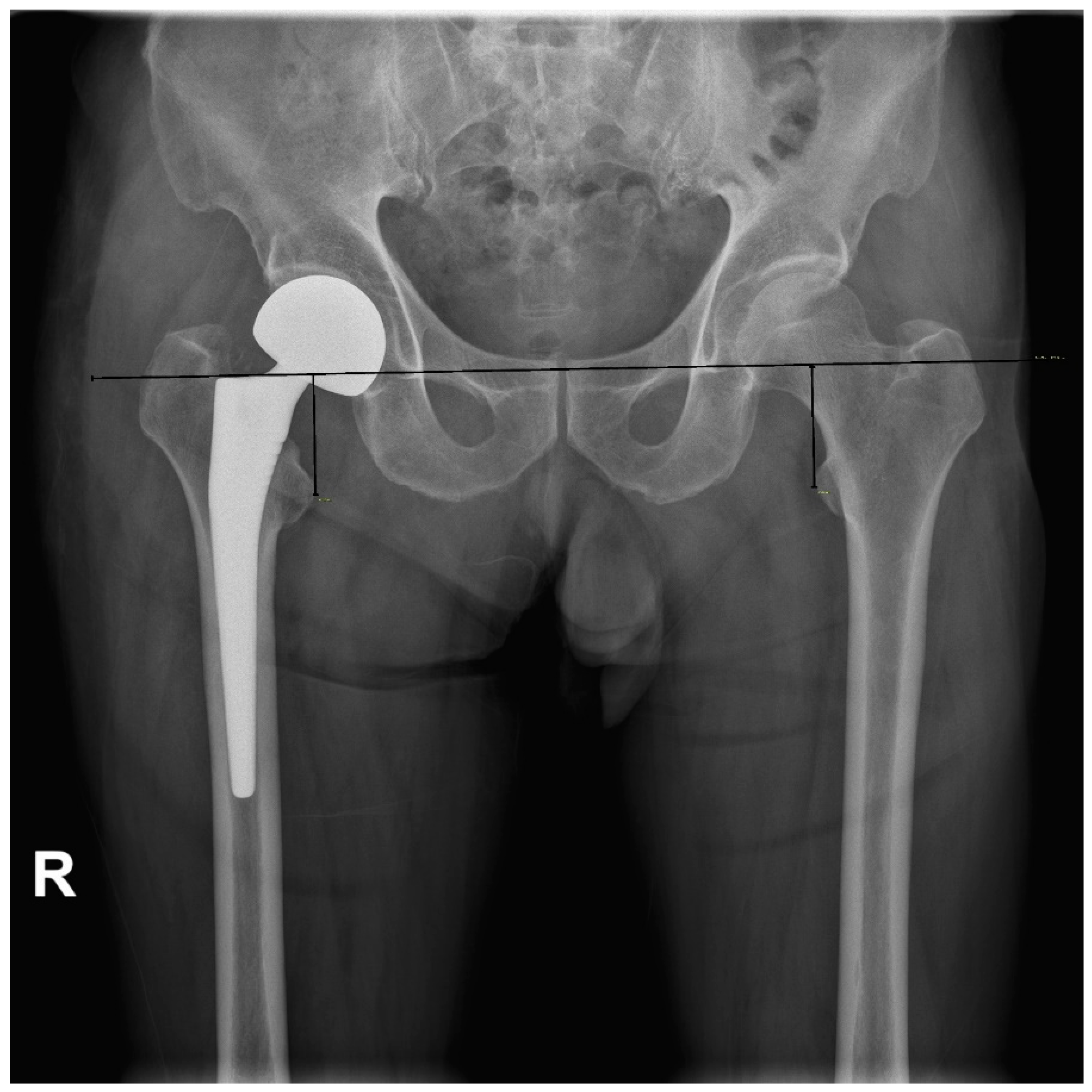
2.2. Radiologic Parameters
2.3. Operative Technique
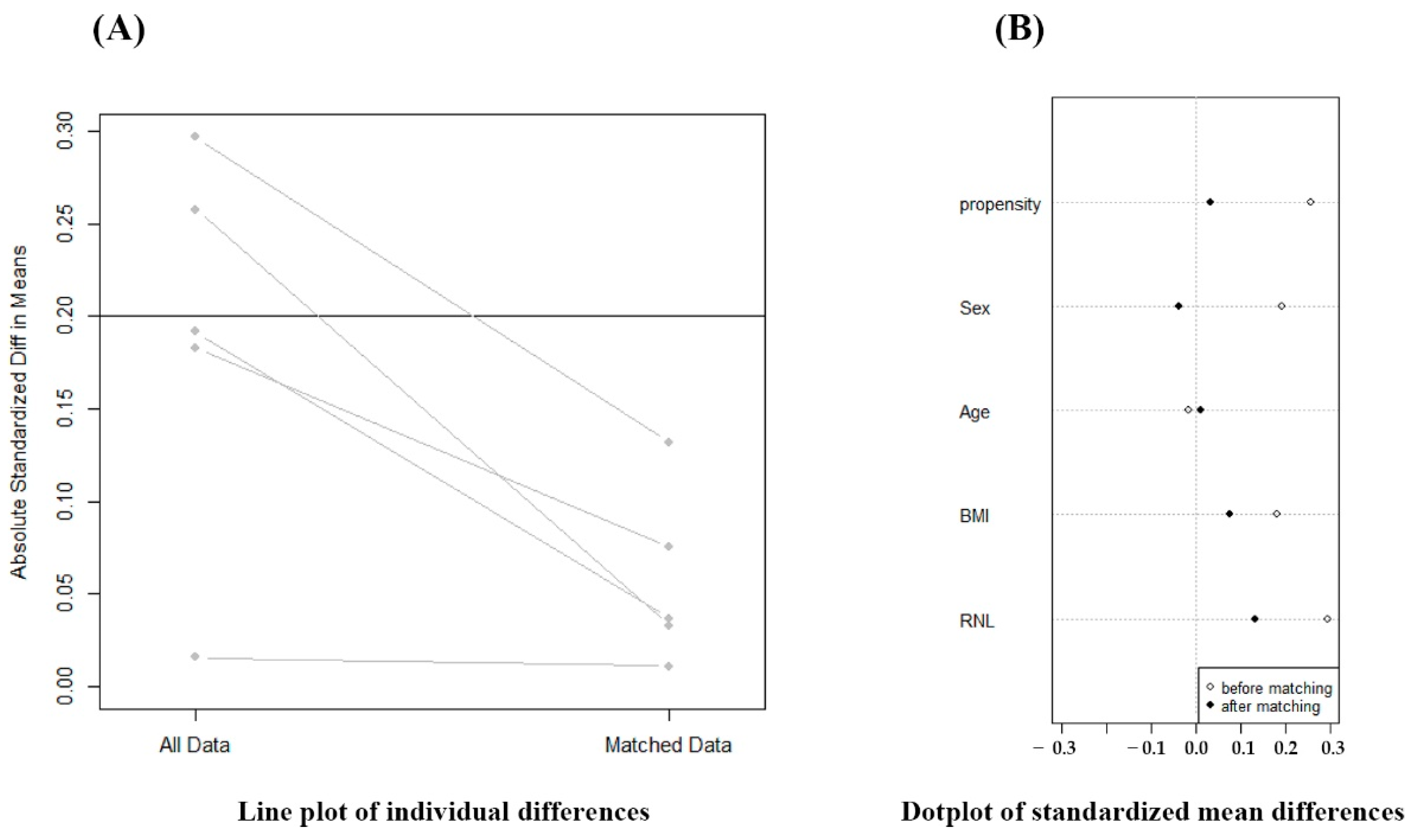
2.4. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Cooper, C.; Campion, G.; Melton, L.J., 3rd. Hip fractures in the elderly: A world-wide projection. Osteoporos. Int. 1992, 2, 285–289. [Google Scholar] [CrossRef] [PubMed]
- Gullberg, B.; Johnell, O.; Kanis, J.A. World-wide projections for hip fracture. Osteoporos. Int. 1997, 7, 407–413. [Google Scholar] [CrossRef] [PubMed]
- Cooper, C.; Cole, Z.A.; Holroyd, C.R.; Earl, S.C.; Harvey, N.C.; Dennison, E.M.; Melton, L.J.; Cummings, S.R.; Kanis, J.A.; The IOF CSA Working Group on Fracture Epidemiology. Secular trends in the incidence of hip and other osteoporotic fractures. Osteoporos. Int. 2011, 22, 1277–1288. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bhandari, M.; Swiontkowski, M. Management of Acute Hip Fracture. N. Engl. J. Med. 2017, 377, 2053–2062. [Google Scholar] [CrossRef] [PubMed]
- Hofmann, A.A.; Skrzynski, M.C. Leg-length inequality and nerve palsy in total hip arthroplasty: A lawyer awaits! Orthopedics 2000, 23, 943–944. [Google Scholar] [CrossRef]
- Mihalko, W.M.; Phillips, M.J.; Krackow, K.A. Acute sciatic and femoral neuritis following total hip arthroplasty. A case report. J. Bone Jt. Surg. Am. 2001, 83, 589–592. [Google Scholar] [CrossRef]
- Abraham, W.D.; Dimon, J.H., 3rd. Leg length discrepancy in total hip arthroplasty. Orthop. Clin. N. Am. 1992, 23, 201–209. [Google Scholar] [CrossRef]
- Gurney, B.; Mermier, C.; Robergs, R.; Gibson, A.; Rivero, D. Effects of limb-length discrepancy on gait economy and lower-extremity muscle activity in older adults. J. Bone Jt. Surg. Am. 2001, 83, 907–915. [Google Scholar] [CrossRef]
- Edeen, J.; Sharkey, P.F.; Alexander, A.H. Clinical significance of leg-length inequality after total hip arthroplasty. Am. J. Orthop. 1995, 24, 347–351. [Google Scholar]
- Woo, R.Y.; Morrey, B.F. Dislocations after total hip arthroplasty. J. Bone Jt. Surg. Am. 1982, 64, 1295–1306. [Google Scholar] [CrossRef]
- Waibel, F.W.A.; Berndt, K.; Jentzsch, T.; Farei-Campagna, J.; Rahm, S.; Dora, C.; Zingg, P.O. Symptomatic leg length discrepancy after total hip arthroplasty is associated with new onset of lower back pain. Orthop. Traumatol. Surg. Res. 2021, 107, 102761. [Google Scholar] [CrossRef]
- Jia, J.; Zhao, Q.; Lu, P.; Fan, G.; Chen, H.; Liu, C.; Liu, J.; Chen, S.; Jin, Z. Clinical efficacy of orthopilot navigation system versus conventional manual of total hip arthroplasty: A systematic review and meta-analysis. Medicine 2019, 98, e15471. [Google Scholar] [CrossRef]
- Migliorini, F.; Cuozzo, F.; Oliva, F.; Eschweiler, J.; Hildebrand, F.; Maffulli, N. Imageless navigation for primary total hip arthroplasty: A meta-analysis study. J. Orthop. Traumatol. 2022, 23, 21. [Google Scholar] [CrossRef]
- Emara, A.K.; Samuel, L.T.; Acuna, A.J.; Kuo, A.; Khlopas, A.; Kamath, A.F. Robotic-arm assisted versus manual total hip arthroplasty: Systematic review and meta-analysis of radiographic accuracy. Int. J. Med. Robot. 2021, 17, e2332. [Google Scholar] [CrossRef]
- Kamath, A.F.; Durbhakula, S.M.; Pickering, T.; Cafferky, N.L.; Murray, T.G.; Wind, M.A., Jr.; Methot, S. Improved accuracy and fewer outliers with a novel CT-free robotic THA system in matched-pair analysis with manual THA. J. Robot. Surg. 2022, 16, 905–913. [Google Scholar] [CrossRef]
- Gonzalez Della Valle, A.; Slullitel, G.; Piccaluga, F.; Salvati, E.A. The precision and usefulness of preoperative planning for cemented and hybrid primary total hip arthroplasty. J. Arthroplast. 2005, 20, 51–58. [Google Scholar] [CrossRef]
- Matsuda, K.; Nakamura, S.; Matsushita, T. A simple method to minimize limb-length discrepancy after hip arthroplasty. Acta Orthop. 2006, 77, 375–379. [Google Scholar] [CrossRef]
- Lim, Y.W.; Chang, Y.J.; Kwon, S.Y.; Kim, Y.S. A simple method using a PACS to minimize leg length discrepancy in primary THA: A method to minimize leg length discrepancy. J. Arthroplast. 2013, 28, 1791–1795. [Google Scholar] [CrossRef]
- Kim, S.C.; Lim, Y.W.; Kwon, S.Y.; Lee, J.K.; Park, I.K.; Kim, Y.S. Comparative Analysis of Radiographic Hip Joint Geometry Using Measurement Tools on Picture Archiving and Communication System: A Prospective Study of 100 Pelvic Radiographs of Koreans. J. Arthroplast. 2016, 31, 2597–2602. [Google Scholar] [CrossRef]
- Asnis, S.E.; Heller, Y.Y. Total Hip Arthroplasty Templating: A Simple Method to Correct for Radiograph Magnification. Orthopedics 2019, 42, e322–e325. [Google Scholar] [CrossRef]
- Polishchuk, D.L.; Patrick, D.A., Jr.; Gvozdyev, B.V.; Lee, J.H.; Geller, J.A.; Macaulay, W. Predicting femoral head diameter and lesser trochanter to center of femoral head distance: A novel method of templating hip hemiarthroplasty. J. Arthroplast. 2013, 28, 1603–1607. [Google Scholar] [CrossRef] [PubMed]
- Siebenrock, K.A.; Kalbermatten, D.F.; Ganz, R. Effect of pelvic tilt on acetabular retroversion: A study of pelves from cadavers. Clin. Orthop. Relat. Res. 2003, 407, 241–248. [Google Scholar] [CrossRef] [PubMed]
- Ranawat, C.S.; Rao, R.R.; Rodriguez, J.A.; Bhende, H.S. Correction of limb-length inequality during total hip arthroplasty. J. Arthroplast. 2001, 16, 715–720. [Google Scholar] [CrossRef] [PubMed]
- Callary, S.A.; Campbell, D.G.; Mercer, G.E.; Nilsson, K.G.; Field, J.R. The 6-year migration characteristics of a hydroxyapatite-coated femoral stem: A radiostereometric analysis study. J. Arthroplast. 2012, 27, 1344–1348.e1. [Google Scholar] [CrossRef]
- Knutson, G.A. Anatomic and functional leg-length inequality: A review and recommendation for clinical decision-making. Part I, anatomic leg-length inequality: Prevalence, magnitude, effects and clinical significance. Chiropr. Osteopat. 2005, 13, 11. [Google Scholar] [CrossRef] [Green Version]
- Krishnan, S.P.; Carrington, R.W.; Mohiyaddin, S.; Garlick, N. Common misconceptions of normal hip joint relations on pelvic radiographs. J. Arthroplast. 2006, 21, 409–412. [Google Scholar] [CrossRef]
- Debbi, E.M.; Rajaee, S.S.; Mayeda, B.F.; Penenberg, B.L. Determining and Achieving Target Limb Length and Offset in Total Hip Arthroplasty Using Intraoperative Digital Radiography. J. Arthroplast. 2020, 35, 779–785. [Google Scholar] [CrossRef] [Green Version]
- Takao, M.; Nishii, T.; Sakai, T.; Sugano, N. Postoperative Limb-Offset Discrepancy Notably Affects Soft-Tissue Tension in Total Hip Arthroplasty. J. Bone Jt. Surg. Am. 2016, 98, 1548–1554. [Google Scholar] [CrossRef]
- Renkawitz, T.; Weber, T.; Dullien, S.; Woerner, M.; Dendorfer, S.; Grifka, J.; Weber, M. Leg length and offset differences above 5mm after total hip arthroplasty are associated with altered gait kinematics. Gait Posture 2016, 49, 196–201. [Google Scholar] [CrossRef]
- Innmann, M.M.; Maier, M.W.; Streit, M.R.; Grammatopoulos, G.; Bruckner, T.; Gotterbarm, T.; Merle, C. Additive Influence of Hip Offset and Leg Length Reconstruction on Postoperative Improvement in Clinical Outcome After Total Hip Arthroplasty. J. Arthroplast. 2018, 33, 156–161. [Google Scholar] [CrossRef]
- McGee, H.M.; Scott, J.H. A simple method of obtaining equal leg length in total hip arthroplasty. Clin. Orthop. Relat. Res. 1985, 194, 269–270. [Google Scholar] [CrossRef]
- Woolson, S.T. Leg length equalization during total hip replacement. Orthopedics 1990, 13, 17–21. [Google Scholar] [CrossRef]
- Jasty, M.; Webster, W.; Harris, W. Management of limb length inequality during total hip replacement. Clin. Orthop. Relat. Res. 1996, 333, 165–171. [Google Scholar] [CrossRef]
- Bose, W.J. Accurate limb-length equalization during total hip arthroplasty. Orthopedics 2000, 23, 433–436. [Google Scholar]
- Shiramizu, K.; Naito, M.; Shitama, T.; Nakamura, Y.; Shitama, H. L-shaped caliper for limb length measurement during total hip arthroplasty. J. Bone Jt. Surg. Br. 2004, 86, 966–969. [Google Scholar] [CrossRef]
- Ecker, T.M.; Tannast, M.; Murphy, S.B. Computed tomography-based surgical navigation for hip arthroplasty. Clin. Orthop. Relat. Res. 2007, 465, 100–105. [Google Scholar] [CrossRef]
- Mainard, D. Navigated and nonnavigated total hip arthroplasty: Results of two consecutive series using a cementless straight hip stem. Orthopedics 2008, 31, 321–322. [Google Scholar]
- Brown, M.L.; Reed, J.D.; Drinkwater, C.J. Imageless computer-assisted versus conventional total hip arthroplasty: One surgeon’s initial experience. J. Arthroplast. 2014, 29, 1015–1020. [Google Scholar] [CrossRef]
- Ogawa, K.; Kabata, T.; Maeda, T.; Kajino, Y.; Tsuchiya, H. Accurate leg length measurement in total hip arthroplasty: A comparison of computer navigation and a simple manual measurement device. Clin. Orthop. Surg. 2014, 6, 153–158. [Google Scholar] [CrossRef] [Green Version]
- Tsai, T.Y.; Dimitriou, D.; Li, J.S.; Kwon, Y.M. Does haptic robot-assisted total hip arthroplasty better restore native acetabular and femoral anatomy? Int. J. Med. Robot 2016, 12, 288–295. [Google Scholar] [CrossRef]
- Bingham, J.S.; Spangehl, M.J.; Hines, J.T.; Taunton, M.J.; Schwartz, A.J. Does Intraoperative Fluoroscopy Improve Limb-Length Discrepancy and Acetabular Component Positioning During Direct Anterior Total Hip Arthroplasty? J. Arthroplast. 2018, 33, 2927–2931. [Google Scholar] [CrossRef] [PubMed]
- Wang, G.; Guo, A.; Yu, F.; Yang, B.; Yu, H.; Diao, N.; Ma, L.; Qiang, H.; Zhao, E. A simple method to minimize leg length discrepancy in hip hemiarthroplasty. Clin. Interv. Aging 2019, 14, 1601–1605. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Clement, N.D.; Gaston, P.; Bell, A.; Simpson, P.; Macpherson, G.; Hamilton, D.F.; Patton, J.T. Robotic arm-assisted versus manual total hip arthroplasty. Bone Jt. Res. 2021, 10, 22–30. [Google Scholar] [CrossRef] [PubMed]
- Herrero, C.; Lavery, J.A.; Anoushiravani, A.A.; Davidovitch, R.I. Real-Time Fluoroscopic Navigation Improves Acetabular Component Positioning During Direct Anterior Approach Total Hip Arthroplasty. Bull. Hosp. Jt. Dis. 2021, 79, 78–83. [Google Scholar]
- Chen, X.; Xing, S.; Zhu, Z.; Wang, H.; Yu, Z.; Bai, X.; Li, X. Accuracy of the Horizontal Calibrator in Correcting Leg Length and Restoring Femoral Offset in Total Hip Arthroplasty. Front. Surg. 2022, 9, 845364. [Google Scholar] [CrossRef]
- Stewart, N.J.; Stewart, J.L.; Brisbin, A. A Comparison of Component Positioning between Fluoroscopy-Assisted and Robotic-Assisted Total Hip Arthroplasty. J. Arthroplast. 2022, 37, 1602–1605.e3. [Google Scholar] [CrossRef]
- Konyves, A.; Bannister, G.C. The importance of leg length discrepancy after total hip arthroplasty. J. Bone Jt. Surg. Br. 2005, 87, 155–157. [Google Scholar] [CrossRef] [Green Version]
- Mahmood, S.S.; Mukka, S.S.; Crnalic, S.; Wretenberg, P.; Sayed-Noor, A.S. Association between changes in global femoral offset after total hip arthroplasty and function, quality of life, and abductor muscle strength. A prospective cohort study of 222 patients. Acta Orthop. 2016, 87, 36–41. [Google Scholar] [CrossRef]
- Vigdorchik, J.M.; Sharma, A.K.; Elbuluk, A.M.; Carroll, K.M.; Mayman, D.J.; Lieberman, J.R. High Offset Stems Are Protective of Dislocation in High-Risk Total Hip Arthroplasty. J. Arthroplast. 2021, 36, 210–216. [Google Scholar] [CrossRef]
- Lecerf, G.; Fessy, M.H.; Philippot, R.; Massin, P.; Giraud, F.; Flecher, X.; Girard, J.; Mertl, P.; Marchetti, E.; Stindel, E. Femoral offset: Anatomical concept, definition, assessment, implications for preoperative templating and hip arthroplasty. Orthop. Traumatol. Surg. Res. 2009, 95, 210–219. [Google Scholar] [CrossRef]


| Variable | Plane X-ray HLD Group | 3-D CT HLD Group | p Value |
|---|---|---|---|
| Number of patients (hips) | 64 | 64 | |
| Side (right/left) | 33/31 | 36/28 | 0.595 |
| Male/female | 14/50 | 15/49 | 0.833 |
| Age | 79.3 ± 8.7 | 79.3 ± 8.4 | 0.951 |
| Body mass index (BMI) | 21.9 ± 3.2 | 22.2 ± 3.4 | 0.633 |
| Relative neck length (RNL) | −0.3 ± 0.7 | −0.2 ± 0.6 | 0.494 |
| Follow-up period | 19.5 (12–61) | 14.2 (12–24) | 0.001 |
| Prosthesis | Corail 64 | Corail 64 | 1.000 |
| 2-D HLD | 43.4 ± 4.5 | 43.1 ± 3.9 | 0.710 |
| 3-D HLD | - | 45.9 ± 3.6 | N/A |
| Prosthesis | |||
| Corail 8 | 0 | 2 | |
| Corail 9 | 2 | 1 | |
| Corail 10 | 3 | 5 | |
| Corail 11 | 8 | 10 | |
| Corail 12 | 17 | 13 | |
| Corail 13 | 17 | 17 | |
| Corail 14 | 8 | 11 | |
| Corail 15 | 7 | 4 | |
| Corail 16 | 2 | 1 | 0.327 |
| Neck length | |||
| Short neck | 48 | 49 | |
| Standard neck | 13 | 9 | |
| Long neck | 3 | 6 | |
| Extra-long neck | 0 | 0 | 0.767 |
| Canal flare index (CFI) | 3.12 ± 0.57 | 2.95 ± 0.56 | 0.085 |
| Cortical index ratio (CI) | 0.48 ± 0.07 | 0.47 ± 0.07 | 0.229 |
| Dorr type A | 5 | 3 | |
| Dorr type B | 25 | 24 | |
| Dorr type C | 34 | 37 | 0.724 |
| Parameter | Plane X-ray HLD Group | 3-D CT HLD Group | p Value |
|---|---|---|---|
| Mean LLD | 1.6 ± 1.2 | 1.1 ± 1.2 | 0.024 |
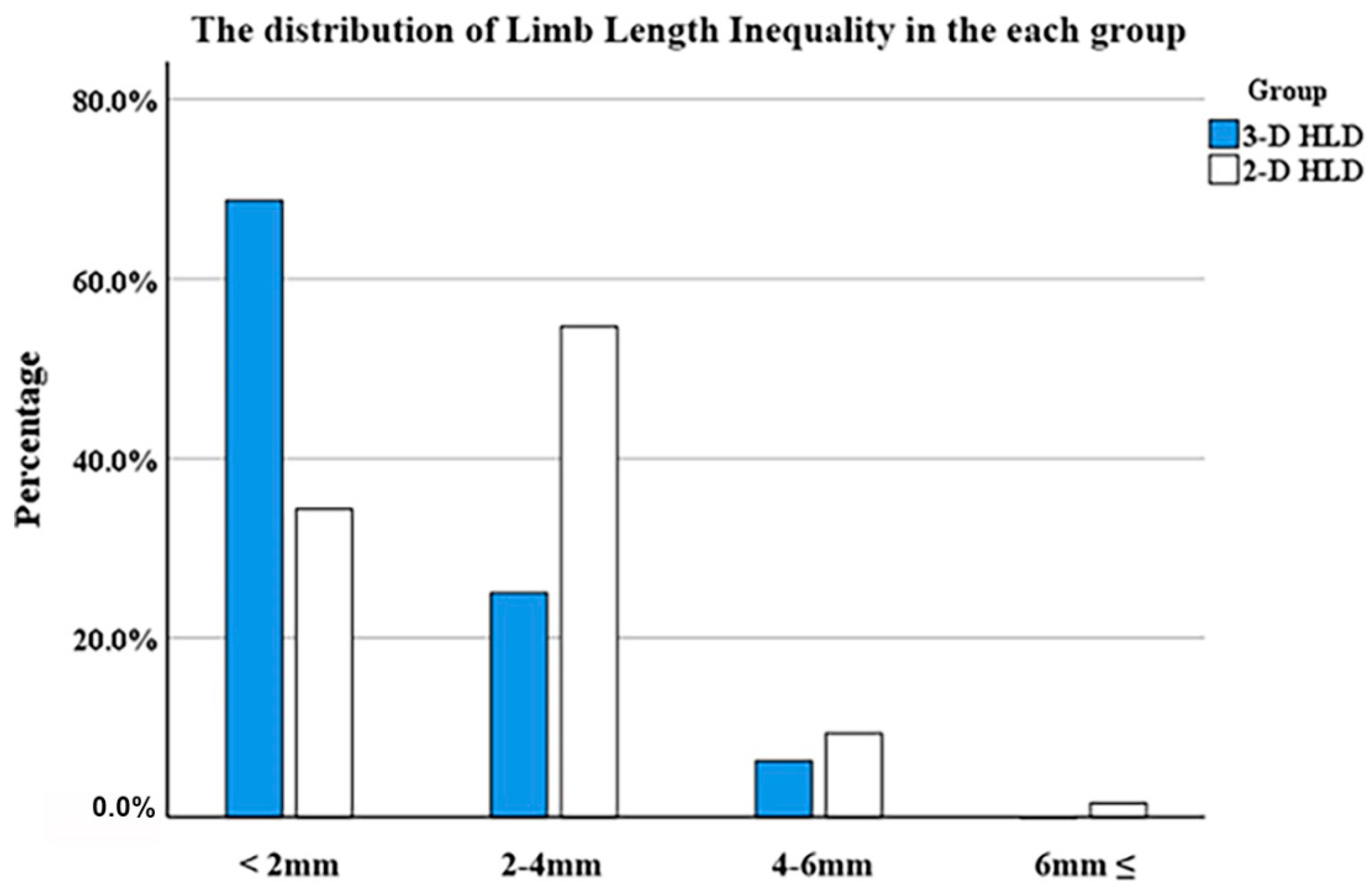
| <2 mm | 22 (34.4%) | 44 (68.8%) | |
| 2–4 mm | 37 (57.8%) | 16 (25.0%) | |
| 4–6 mm | 4 (6.3%) | 4 (6.3%) | |
| ≥6 mm | 1 (1.6%) | 0 (0.0%) | 0.001 |
| Harris hip score | 86.9 (65–93) | 86.2 (63–98) | 0.507 |
| Study | Mean LLD (mm) | Methods |
|---|---|---|
| McGee and Scott (1985) [31] | No results presented | A Steinmann pin was driven in 2 cm superior to the acetabulum and bent into a “u” shape; a mark was made at the point where the free end of the “u” contacted the greater trochanter |
| Woolson (1990) [32] | 2.8 | Comparing the dimensions of the resected bone with the dimensions replaced by the prosthesis |
| Jasty et al. (1996) [33] | 5.4 | Use of mechanical jigs and measuring calipers |
| Bose (2000) [34] | 3.4 | Use of measuring calipers (the Acculength hip gauge device) |
| Ranawat et al. (2001) [23] | 7.4 | A vertical Steinmann pin at the infracotyloid groove of the acetabulum |
| Shiramizu et al. (2004) [35] | 2.1 | Use of measuring L-shaped caliper |
| Gonzalez et al. (2005) [16] | 1.71 | Measuring between the proximal edge of the lesser trochanter and the center of rotation of the femoral head (HLD) |
| Matsuda (2006) [17] | 2.0 | Measuring the actual HLD preoperatively and reproducing it in the operative field with a modular neck system |
| Ecker et al. (2007) [36] | 1.3 | Computed tomography-based navigation |
| Mainard (2008) [37] | 4.4 | Imageless navigation |
| Lim et al. (2013) [18] | 1.5 | Measuring head to lesser trochanter length using PACS and reproducing it in the operative field with a modular neck system |
| Brown et al. (2014) [38] | 5.2 | Imageless navigation |
| Ogawa et al. (2014) [39] | 2.9 | Measuring with PCA limb lengthening gauge |
| Tsai et al. (2016) [40] | 0.7 | Robot-assisted technology |
| Bingham et al. (2018) [41] | 1.1 | Fluoroscopic guidance |
| Wang et al. (2019) [42] | 4.4 | Measuring ratio of contralateral femoral head and the distance of HLD using PACS |
| Clement et al. (2021) [43] | 2.3 | Robot-assisted technology |
| Herrero et al. (2021) [44] | 1.02 | Fluoroscopy-based navigation |
| Chen et al. (2022) [45] | 2.5 | Use of measuring horizontal calibrator |
| Stewart et al. (2022) [46] | 3.79 | Fluoroscopic guidance |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Oh, S.; Kim, Y.-S.; Kwon, S.-Y.; Lim, Y.-W.; Park, H.; Park, J.; Song, J.-H. Utilizing Three-Dimensional Head-Lesser Trochanter Distance Could Further Reduce Leg Length Inequality in Primary Bipolar Hemiarthroplasty. J. Clin. Med. 2022, 11, 6303. https://doi.org/10.3390/jcm11216303
Oh S, Kim Y-S, Kwon S-Y, Lim Y-W, Park H, Park J, Song J-H. Utilizing Three-Dimensional Head-Lesser Trochanter Distance Could Further Reduce Leg Length Inequality in Primary Bipolar Hemiarthroplasty. Journal of Clinical Medicine. 2022; 11(21):6303. https://doi.org/10.3390/jcm11216303
Chicago/Turabian StyleOh, Seungbae, Yong-Sik Kim, Soon-Yong Kwon, Young-Wook Lim, Hyunwoo Park, Jongwoo Park, and Joo-Hyoun Song. 2022. "Utilizing Three-Dimensional Head-Lesser Trochanter Distance Could Further Reduce Leg Length Inequality in Primary Bipolar Hemiarthroplasty" Journal of Clinical Medicine 11, no. 21: 6303. https://doi.org/10.3390/jcm11216303






