1. Introduction
Morphea, also termed localized scleroderma (LoS), is a chronic disease associated with fibrosis of the skin and possibly underlying tissues, which has the potential to progress to significant morbidity [
1]. The incidence of morphea is estimated at 27 cases/1,000,000, with a marked female predominance [
2,
3]. There are two peaks of incidence of LoS, one between the ages of 7 and 11 and the other between the ages of 40 and 50 [
4]. The pathogenesis of LoS is still not fully known [
1]. The interaction of triggering factors with the individual susceptibility appears to have the major role in the disease development, resulting in the activation of both innate and acquired responses with immunoinflammatory and profibrotic actions involving the epidermis and dermis. Furthermore, in the light of evidence, including the high prevalence of an individual or family history of autoimmune disease and the presence of autoantibodies as well as certain human leukocyte antigen subtypes, morphea is believed to have an autoimmune nature [
5,
6].
The clinical features of LoS are heterogeneous and classified into five subtypes: limited, generalized, linear, deep and mixed [
2]. In general, morphea is characterized by a consecutive stage of an active phase characterized by inflammatory or inflammatory-sclerotic, erythematous or indurative lesions with active “lilac” ring, which appeared or enlarged in the last month, followed by an inactive postinflammatory lesions with hyperpigmentation and dermal atrophy [
4,
7]. A variety of methods is available for the treatment of LoS [
8]. For mild, superficial lesions limited to the skin, topical treatments and UV phototherapy are recommended, while for generalized, linear or deep types, systemic immunomodulatory therapies, such as glucocorticosteroids (GCS) or methotrexate (MTX), are usually introduced. In severe cases, early implementation of therapy, at the stage of inflammatory lesions, allows to avoid serious complications and disfigurement [
8].
For the assessment of disease severity, the “localized scleroderma cutaneous assessment tool” (LoSCAT) in combination with Physician’s Global Assessment (PGA) are recommended [
9]. LoSCAT includes the “modified localized scleroderma severity index” (mLoSSI) and the “localized scleroderma skin damage index” (LoSDI). mLoSSI incorporates features of disease activity or severity, such as the appearance of new skin lesions or enlargement of existing lesions in the past month, together with erythema and induration of the skin. LoSDI assesses tissue damage, reflected by atrophy of the skin and subcutaneous tissue, as well as pigmentary alterations [
10].
To date, the search for laboratory biomarkers for LoS has not been much of a success.
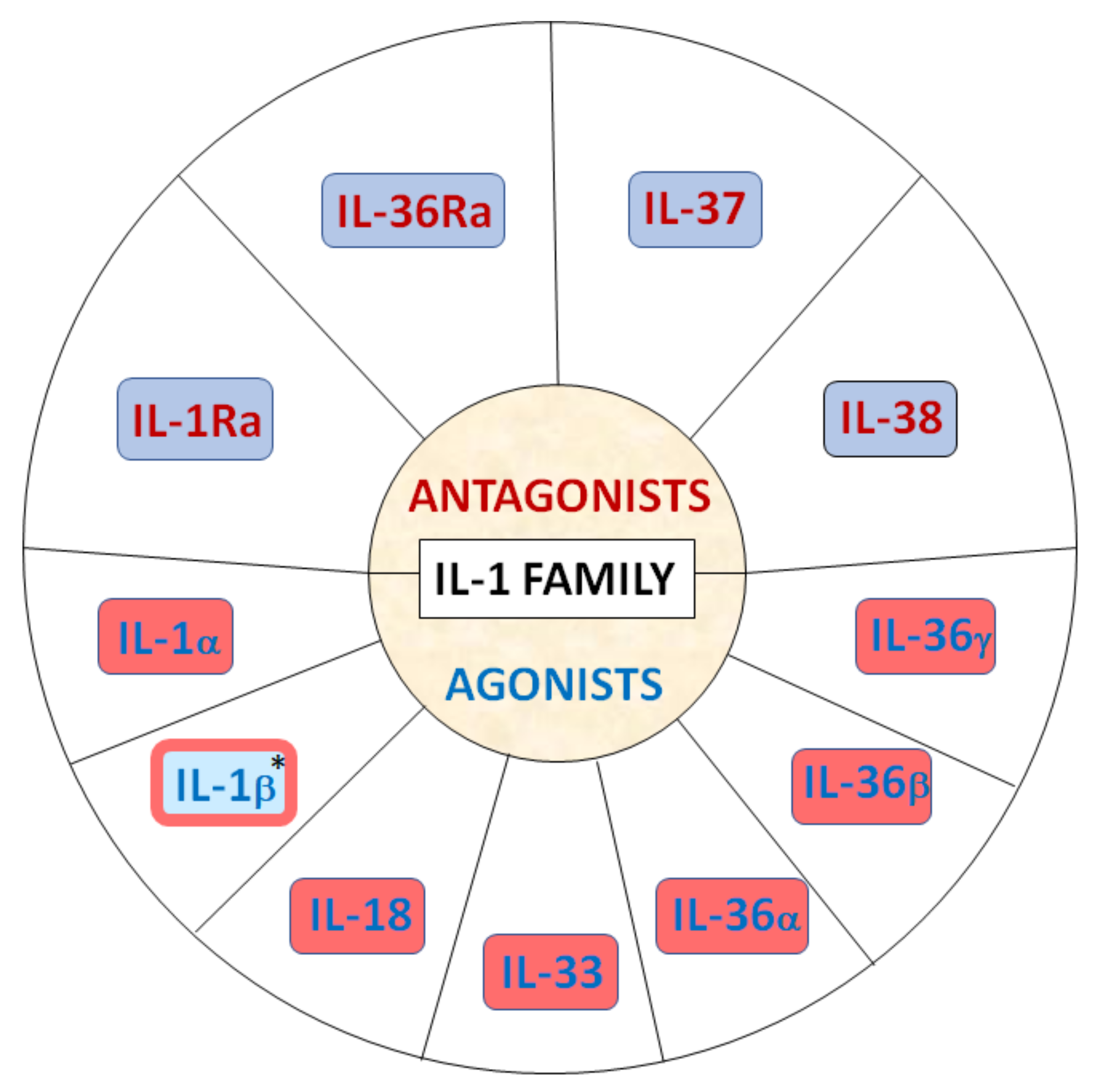
The IL-1 cytokine family comprises 11 members, including seven ligands with broad pro-inflammatory and profibrotic activities (IL-1α, IL-1β, IL-18, IL-33, IL-36α, IL-36β and IL-36γ), three receptor antagonists and one anti-inflammatory cytokine (
Figure 1) [
11,
12,
13,
14].
IL-1 is critical to the pathogenesis of a variety of human diseases and IL-1 targeted therapies have been successfully employed to treat a range of inflammatory conditions such as rheumatoid arthritis. The role of the IL-1 family in LoS has not been extensively investigated to date [
15,
16,
17,
18,
19,
20,
21,
22,
23,
24,
25,
26,
27]. Of note, involvement of the IL-1 family seems to be well established in the pathogenesis of systemic sclerosis (SSc), including development of inflammation and fibrosis in both the skin and underlying tissues, as well as internal organs [
28,
29,
30].
Thus, considering the presence of some resemblances between SSc and LoS, including the similarity of in the histological pattern of skin [
31], we aimed to evaluate the clinical relevance of selected serum levels of IL-1 family cytokines, IL-1α, IL-1β, IL-18, IL-33, IL-37 and IL-38 in a modest-sized single-center cohort of well-characterized and prospectively followed LoS patients and healthy controls, including comparison before and after the initiation of therapy with the use of the standardized disease assessment tools.
4. Discussion
To the best of our knowledge, this study is the first to investigate the extensive profile of IL-1 family in LoS as biomarkers of the disease and possible therapy-targeted measure.
Our findings did not reveal significant differences in baseline IL-1α, IL-1β, IL-18, IL-33, IL-37 and IL-38 levels between LoS group and HCs; however, after treatment, there were marked changes in concentrations of IL-1α and IL-33 either within LoS group as well as in comparison to HCs. Specifically, in contrast to baseline measures, after completion of therapy we obtained statistically higher values of serum IL-1α in patients with LoS than in controls, although an absolute increase in these levels within LoS group were only close to significant, probably due to a relatively small sample size. On the contrary, IL-33 concentrations significantly decreased in LoS patients under treatment and were significantly lower in post-treated LoS individuals when compared to HCs.
In addition, our results showed some important associations of IL-1 members with certain disease-targeted measures. Particularly noteworthy, we found that IL-1α levels may have a potential strong association with disease activity and severity. In post-treated LoS patients IL-1α concentrations negatively correlated with both mLoSSi and PGA-A scores. With respect to serum levels of other analyzed cytokines, no significant association was found in terms of clinical variables in the study group; however, it is worth noting the inverse correlation of baseline IL-1β levels with mLoSSI scores with borderline significance.
In light of these results, it seems that IL-1α and IL-33, as well as Il-1β, may be potential mediators and targets of interest in LoS. These IL-1 family members are acknowledged to play a role in inflammation and have been suggested to be involved in autoimmune diseases, including systemic lupus erythematosus and rheumatoid arthritis as well as systemic sclerosis (SSc) [
28,
32,
33,
34,
35]. Moreover, both IL-1α and IL-1β have been shown to directly stimulate fibroblasts proliferation and collagen synthesis and fibroblasts are induced to secrete a range of inflammatory cytokines in response to IL-1α and IL-1β [
36,
37,
38]. IL-1β has also been found to participate in the differentiation of Th17 cells that may play a crucial role in the development of tissue fibrosis [
28,
32,
39]. Of note, it was demonstrated that SSc patients with coexisting LoS-like lesions exhibited overexpression of IL-1α in the epidermis of both LoS-like and typical SSc lesions [
31]. On this background, our findings of lower IL-1α levels in LoS patients after treatment and their negative correlation with both mLoSSi and PGA-A scores as well as inverse association of IL-1β with mLoSSi seem controversial. However, there is a large body of literature also demonstrating an inhibitory effect of IL-1α and IL-1β on collagen synthesis [
40,
41]. Surprisingly, it has been shown that IL-1α increases the mRNA expression of matrix metalloproteinases (MMPs), namely, MMP-1 and MMP-3, and induces MMP-7 resulting in collagen degradation [
42]. Of note, some previous studies reported increase in MMPs in LoS after treatment and their correlation with clinical improvement [
43,
44], but direct experimental studies on MMPs and IL-1 in LoS are lacking.
Another possible explanation for increased post-treatment levels of IL-1α in line with improvement in disease activity and severity scores is the direct effect of applied therapies. However, data on the effects of systemic treatment on the levels of serum IL-1 family cytokines are scarce and unavailable for LoS; the paradoxical proinflammatory properties of MTX in the form of increased IL-1 as measured by secreted protein and level of gene expression have been demonstrating in vitro on human monocytic cell line U937, which is an effect that seems to be at odds with the generally anti-inflammatory activity of this drug [
45]. In contrast, regarding systemic GCS, there are reports of down-regulation of IL-1α [
46,
47]. However, immunosuppressive and anti-inflammatory agents such as glucocorticoids may simultaneously induce increased expression of IL-1R2 (type 2 receptor for IL-1) that acts as negative regulator of the IL-1 system, modulating IL-1α availability for the signaling receptor. Interestingly, this anti-IL-1 effect seems predominantly local [
32,
48]. Thus, in relation to our results, it may be speculated that observed post-treatment increase in IL-1α is a kind of feedback compensatory reaction to the blocking effect of IL-1R2, making IL-1α an interesting ambiguous mediator in LoS. However, future experimental studies are warranted to elucidate this phenomenon.
IL-33 is structurally related to IL-1β and is known to have a crucial role in immune and inflammatory reactions. Recent articles have also described IL-33 as a cytokine with emerging pro-fibrotic potential depending on targets such as IL-13, TGF-β, IFN-γ and TLR/NF-κB signaling pathways [
35]. Subcutaneous injection of IL-33 in mice resulted in the development of cutaneous fibrosis, similar to that observed in patients SSc, including dermal mast cells and skin-infiltrating neutrophils through the suppression of Th1-mediated contact hypersensitivity responses [
35]. Additionally, IL-33 may function as an alarmin that alerts the immune system after endothelial or epithelial cell damage during infection, physical stress, or trauma and skin trauma as well as endothelial cell damage have been proposed as crucial events in the development of LoS lesions [
49,
50,
51]. Moreover, MTX treatment has been shown to decline skin and blood IL-33 levels in psoriatic patients [
52].
Thus, with respect to these observations, our finding of significant decrease in serum IL-33 concentrations in LoS patients under treatment may highlight IL-33 as the possible pathogenic mediator in LoS as well as a candidate for future targeted therapies. However, since we did not found correlations with measures of disease activity or severity, further research on larger cohort is required to clarify this contradiction.
Currently, no comparable clinical studies are available for LoS. Thus, the results are difficult to discuss. However, some essential data may be obtained from research of other diseases that may be applicable to LoS, particularly SSc that shares common inflammatory and immunologic pathways.
However, the expression levels of IL-1β and IL-1α were found significantly up-regulated in the lesional skin tissue in SSc [
31,
53], the serum levels of IL-1α and IL-1β are somewhat controversial. Similarl to our findings in LoS, Lin et al. [
54], in line with some other studies, did not observe a significant difference in serum concentrations of IL-1α and IL-1β between SSc and HCs, although some authors have reported their elevated serum levels in SSc patients [
55,
56,
57,
58,
59]. With respect to clinical variables, observations for SSc are also puzzling. In contrast to our results in LoS cohort, serum IL-1β, but not IL-1α, was positively correlated with the severity of skin involvement in SSc measured by modified Rodnan skin score (mRSS), suggesting a potential role of this cytokine in SSc fibrotic complications, but serum levels of both IL-1α and IL-1β positively correlated with carbon monoxide transfer coefficient and patients with high serum IL-1β had higher DLCO, suggesting a reduced risk of lung fibrosis and PAH [
54].
Recently, an increasing number of studies have shown the potential role of IL-33 in SSc [
28,
35]. In contrast to our findings in LoS patients, serum IL-33 levels were reported to be elevated in patients with SSc compared with healthy controls and correlated with the extent of skin sclerosis as well as with the severity of pulmonary fibrosis [
60]. In one recent study of IL-1α, IL-1β, IL-18 and IL-33 in a relatively modest-sized Chinese SSc cohort, only serum IL-1β and IL-33 were found to be higher in SSc in multivariable analysis; however, no clinical associations with any of these cytokines were found [
59].
In conclusion, our observations may highlight the potential relevance of certain IL-1 family members, namely, IL-1α, IL-1β and, in particular, IL-33, as interesting pathogenic mediators in LoS as well as the feasibility of their use in clinical applications. However, the puzzling results obtained for IL-1α and IL-1β emphasize the need for future experimental and clinical research to clarify their role in LoS.
We are aware of several limitations in our study, including a relatively small sample size and the restriction to a single-center population, which are likely to limit the statistical power. Moreover, due to small number of patients with inactive phase of LoS lesions at baseline, their selection as separate group for statistical analysis and comparisons was unavailable. Therefore, replication in multi-center studies with a greater number of enrolled individuals will be beneficial.