Health-Related Quality of Life and Mental Well-Being during the COVID-19 Pandemic in Five Countries: A One-Year Longitudinal Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Population
2.2. Data Collection Procedure and Consent
2.3. Primary Outcome Measures
2.4. Respondent Characteristics at T1
2.5. Life Events Related to Health, Work, Income, and Living Situation
2.6. Statistical Analysis
3. Results
3.1. Study Population
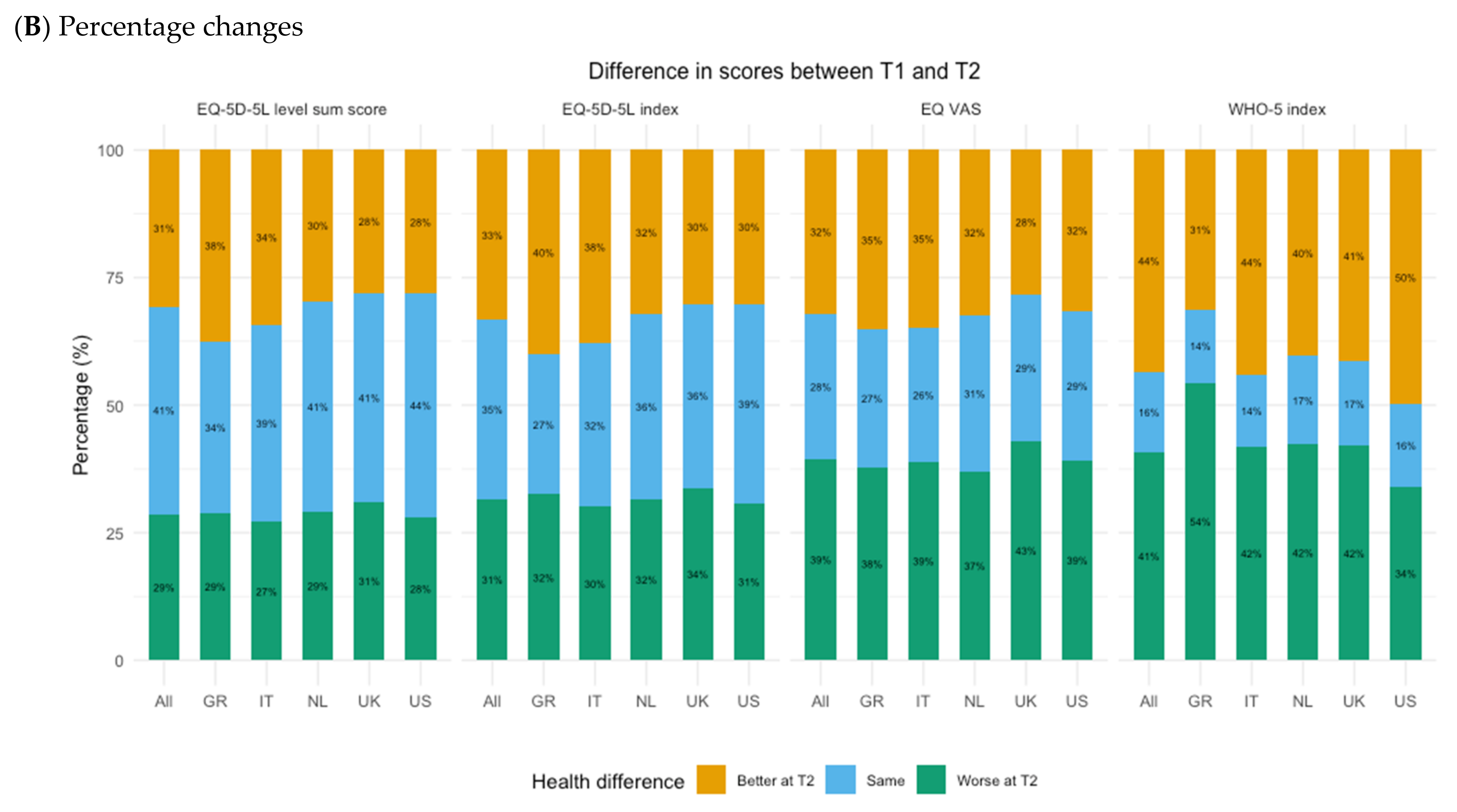
3.2. Changes in HRQoL and Mental Well-Being between T1 and T2
3.3. Determinants of Change in HRQoL and Mental Well-Being
4. Discussion
4.1. Summary of Main Findings
4.2. Interpretation
4.3. Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
| Greece | Italy | Netherlands | UK | US | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| T2 (N = 511) | T1 (N = 1022) | T2 (N = 1784) | T1 (N = 3212) | T2 (N = 1143) | T1 (N = 3296) | T2 (N = 1448) | T1 (N = 3234) | T2 (N = 1879) | T1 (N = 5919) | |
| Response rate | 50% | 56% | 35% | 45% | 32% | |||||
| Age | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | |||||
| Median (IQR) | 44 (18) | 40 (20) | 46 (21) | 43 (22) | 58(21) | 49 (29) | 54 (24) | 44 (27) | 57 (20) | 47 (27) |
| Mean (SD) | 44.1 (12.6) | 40.4 (13.2) | 47.6 (13.8) | 44.0 (14.2) | 55.0 (14.0) | 47.8 (16.6) | 52.5 (14.2) | 45.5 (15.9) | 55.2 (13.1) | 46.9 (15.8) |
| Sex | 0.083 | 0.568 | 0.310 | 0.909 | 0.019 | |||||
| Male | 264 (52%) | 480 (47%) | 858 (48%) | 1537 (48%) | 526 (46%) | 1587 (48%) | 709 (49%) | 1558 (48%) | 869 (46%) | 2613 (44%) |
| Female | 247 (48%) | 542 (53%) | 926 (52%) | 1673 (52%) | 617 (54%) | 1706 (52%) | 739 (51%) | 1672 (52%) | 1010 (54%) | 3283 (55%) |
| Education level | 0.076 | 0.468 | 0.037 | 0.002 | 0.019 | |||||
| High | 343 (67%) | 626 (61%) | 726 (41%) | 1334 (42%) | 464 (41%) | 1463 (44%) | 807 (56%) | 1976 (61%) | 1393 (74%) | 4079 (69%) |
| Middle | 153 (30%) | 357 (35%) | 786 (44%) | 1429 (44%) | 351 (31%) | 1001 (30%) | 608 (42%) | 1182 (37%) | 434 (23%) | 1510 (26%) |
| Low | 15 (3%) | 39 (4%) | 272 (15%) | 449 (14%) | 328 (29%) | 832 (25%) | 33 (2%) | 76 (2%) | 52 (3%) | 330 (6%) |
| Occupation status | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | |||||
| Employed | 324 (63%) | 551 (54%) | 1047 (59%) | 1849 (58%) | 550 (48%) | 1684 (51%) | 799 (55%) | 1934 (60%) | 1025 (55%) | 3134 (53%) |
| Student | 19 (4%) | 93 (9%) | 55 (3%) | 223 (7%) | 29 (3%) | 248 (8%) | 16 (1%) | 100 (3%) | 12 (1%) | 186 (3%) |
| Unemployed | 106 (21%) | 279 (27%) | 386 (22%) | 727 (23%) | 102 (9%) | 379 (11%) | 156 (11%) | 396 (12%) | 174 (9%) | 979 (17%) |
| Retired | 59 (12%) | 82 (8%) | 282 (16%) | 385 (12%) | 337 (29%) | 651 (20%) | 382 (26%) | 575 (18%) | 580 (31%) | 1193 (20%) |
| Unable to work | 3 (1%) | 17 (2%) | 14 (1%) | 28 (1%) | 125 (11%) | 334 (10%) | 95 (7%) | 229 (7%) | 88 (5%) | 427 (7%) |
| Chronic conditions | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | |||||
| None | 328 (64%) | 608 (59%) | 1176 (66%) | 1984 (62%) | 607 (53%) | 1641 (50%) | 888 (61%) | 1830 (57%) | 1230 (65%) | 3099 (52%) |
| One | 115 (23%) | 317 (31%) | 369 (21%) | 858 (27%) | 301 (26%) | 1026 (31%) | 319 (22%) | 883 (27%) | 414 (22%) | 1756 (30%) |
| Two or more | 68 (13%) | 97 (9%) | 239 (13%) | 370 (12%) | 235 (21%) | 629 (19%) | 241 (17%) | 521 (16%) | 235 (13%) | 1064 (18%) |
| COVID-19 status | <0.001 | <0.001 | 0.009 | <0.001 | <0.001 | |||||
| Not infected | 461 (90%) | 957 (94%) | 1565 (88%) | 2880 (90%) | 998 (87%) | 2837 (86%) | 1278 (88%) | 2747 (85%) | 1669 (89%) | 4869 (82%) |
| Likely | 28 (5%) | 63 (6%) | 115 (6%) | 316 (10%) | 77 (7%) | 420 (13%) | 112 (8%) | 446 (14%) | 113 (6%) | 873 (15%) |
| Infected | 22 (4%) | 2 (0%) | 104 (6%) | 16 (0%) | 68 (6%) | 39 (1%) | 58 (4%) | 41 (1%) | 97 (5%) | 177 (3%) |
| Living situation | 0.600 | 0.025 | <0.001 | 0.015 | <0.001 | |||||
| Living with others | 429 (84%) | 859 (84%) | 1585 (89%) | 2826 (88%) | 801 (70%) | 2371 (72%) | 1113 (77%) | 2519 (78%) | 1435 (76%) | 4345 (73%) |
| Living alone | 75 (15%) | 142 (14%) | 184 (10%) | 328 (10%) | 339 (30%) | 871 (26%) | 317 (22%) | 639 (20%) | 412 (22%) | 1328 (22%) |
| Other | 7 (1%) | 21 (2%) | 15 (1%) | 58 (2%) | 3 (0%) | 54 (2%) | 18 (1%) | 76 (2%) | 32 (2%) | 246 (4%) |
| Experience on access to healthcare | 0.533 | <0.001 | <0.001 | <0.001 | <0.001 | |||||
| Always good | 163 (32%) | 322 (32%) | 571 (32%) | 958 (30%) | 623 (54%) | 1266 (38%) | 513 (35%) | 1088 (34%) | 1007 (54%) | 2944 (50%) |
| Usually good | 208 (41%) | 382 (37%) | 709 (40%) | 1457 (45%) | 374 (33%) | 1502 (46%) | 531 (37%) | 1264 (39%) | 629 (33%) | 2027 (34%) |
| Sometimes good | 86 (17%) | 203 (20%) | 358 (20%) | 625 (19%) | 103 (9%) | 414 (13%) | 265 (18%) | 670 (21%) | 202 (11%) | 753 (13%) |
| Usually not good | 38 (7%) | 85 (8%) | 114 (6%) | 135 (4%) | 23 (2%) | 95 (3%) | 93 (6%) | 164 (5%) | 17 (1%) | 138 (2%) |
| Never good | 16 (3%) | 30 (3%) | 32 (2%) | 37 (1%) | 20 (2%) | 19 (1%) | 46 (3%) | 48 (1%) | 24 (1%) | 57 (1%) |
| EQ-5D LSS | EQ-5D Index | EQ-VAS | WHO-5 | ||||||
|---|---|---|---|---|---|---|---|---|---|
| N | Mean | SD * | Mean | SD * | Mean | SD * | Mean | SD * | |
| Total | 6765 | 7.2 | 2.7 | 0.85 | 0.20 | 77.8 | 16.7 | 62.0 | 24.2 |
| Age groups | |||||||||
| 18–24 yrs. | 229 (3%) | 7.3 | 2.6 | 0.84 | 0.20 | 79.1 | 15.7 | 57.3 | 23.7 |
| 25–34 yrs. | 784 (12%) | 7.2 | 2.7 | 0.85 | 0.21 | 77.8 | 17.4 | 56.5 | 24.6 |
| 35–44 yrs. | 1331 (20%) | 7.1 | 2.6 | 0.86 | 0.19 | 77.8 | 16.6 | 58.6 | 24.5 |
| 45–54 yrs. | 1474 (22%) | 7.2 | 2.8 | 0.85 | 0.21 | 77.5 | 16.9 | 59.5 | 24.8 |
| 55–64 yrs. | 1516 (22%) | 7.3 | 2.8 | 0.84 | 0.22 | 77.2 | 16.9 | 63.4 | 24.0 |
| 65–75 yrs. | 1431 (21%) | 7.1 | 2.6 | 0.86 | 0.19 | 78.4 | 16.2 | 69.8 | 21.1 |
| Sex | |||||||||
| Male | 3226 (48%) | 7.0 | 2.6 | 0.86 | 0.19 | 78.1 | 16.3 | 65.9 | 23.1 |
| Female | 3539 (52%) | 7.3 | 2.8 | 0.84 | 0.21 | 77.5 | 17.0 | 58.4 | 24.6 |
| Education level | |||||||||
| High | 3733 (55%) | 7.0 | 2.5 | 0.87 | 0.19 | 79.0 | 15.8 | 62.8 | 23.6 |
| Middle | 2332 (34%) | 7.4 | 2.8 | 0.84 | 0.21 | 76.2 | 17.5 | 60.5 | 24.8 |
| Low | 700 (10%) | 7.7 | 3.1 | 0.82 | 0.23 | 76.5 | 18.1 | 62.0 | 25.2 |
| Occupation status | |||||||||
| Employed | 3622 (54%) | 6.8 | 2.2 | 0.88 | 0.16 | 79.7 | 14.7 | 62.5 | 23.5 |
| Student | 174 (3%) | 7.0 | 2.4 | 0.86 | 0.19 | 79.6 | 15.4 | 56.6 | 22.7 |
| Unemployed | 1067 (16%) | 7.4 | 2.5 | 0.84 | 0.18 | 77.0 | 16.9 | 56.4 | 24.8 |
| Retired | 1550 (23%) | 7.1 | 2.6 | 0.86 | 0.19 | 78.0 | 16.4 | 69.1 | 21.3 |
| Unable to work | 352 (5%) | 11.0 | 4.4 | 0.55 | 0.36 | 58.4 | 23.5 | 44.1 | 27.6 |
| Income level | |||||||||
| High | 1448 (21%) | 6.8 | 2.4 | 0.88 | 0.18 | 80.8 | 13.6 | 67.1 | 21.2 |
| Middle | 1879 (48%) | 7.1 | 2.5 | 0.86 | 0.19 | 78.1 | 16.0 | 62.2 | 23.4 |
| Low | 1143 (15%) | 7.9 | 3.2 | 0.80 | 0.24 | 73.0 | 20.3 | 55.1 | 27.0 |
| Unwilling to tell | 1784 (6%) | 7.0 | 2.8 | 0.86 | 0.21 | 79.6 | 16.2 | 63.4 | 24.7 |
| Unknown | - | ||||||||
| Chronic conditions | |||||||||
| No | 3888 (57%) | 6.2 | 1.7 | 0.92 | 0.12 | 83.0 | 12.8 | 66.6 | 22.1 |
| Yes | 1870 (28%) | 8.5 | 3.2 | 0.75 | 0.25 | 70.7 | 18.6 | 55.7 | 25.4 |
| Country of residence | |||||||||
| UK | 1448 (21.4%) | 7.5 | 3.2 | 0.83 | 0.25 | 75.1 | 18.9 | 59.6 | 26.2 |
| US | 1879 (27.8%) | 7.0 | 2.6 | 0.87 | 0.19 | 79.9 | 15.5 | 63.6 | 23.9 |
| Netherlands | 1143 (16.9%) | 7.3 | 2.9 | 0.84 | 0.22 | 76.6 | 17.2 | 66.9 | 22.7 |
| Italy | 1784 (26.4%) | 7.2 | 2.3 | 0.86 | 0.17 | 77.4 | 15.9 | 57.7 | 23.2 |
| Greece | 511 (7.6%) | 7.1 | 2.0 | 0.86 | 0.15 | 81.7 | 14.2 | 66.5 | 22.7 |
References
- McKee, M.; Stuckler, D. If the world fails to protect the economy, COVID-19 will damage health not just now but also in the future. Nat. Med. 2020, 26, 640–642. [Google Scholar] [CrossRef] [PubMed]
- International Monetary Fund. World Economic Outlook: The Great Lockdown; International Monetary Fund: Washington, DC, USA, 2020. [Google Scholar]
- Miller, I.F.; Becker, A.D.; Grenfell, B.T.; Metcalf, C.J.E. Disease and healthcare burden of COVID-19 in the United States. Nat. Med. 2020, 26, 1212–1217. [Google Scholar] [CrossRef] [PubMed]
- Remuzzi, A.; Remuzzi, G. COVID-19 and Italy: What next? Lancet 2020, 395, 1225–1228. [Google Scholar] [CrossRef]
- Di Renzo, L.; Gualtieri, P.; Pivari, F.; Soldati, L.; Attina, A.; Cinelli, G.; Leggeri, C.; Caparello, G.; Barrea, L.; Scerbo, F.; et al. Eating habits and lifestyle changes during COVID-19 lockdown: An Italian survey. J. Transl. Med. 2020, 18, 229. [Google Scholar] [CrossRef]
- Bentlage, E.; Ammar, A.; How, D.; Ahmed, M.; Trabelsi, K.; Chtourou, H.; Brach, M. Practical Recommendations for Maintaining Active Lifestyle during the COVID-19 Pandemic: A Systematic Literature Review. Int. J. Environ. Res. Public Health 2020, 17, 6265. [Google Scholar] [CrossRef]
- Mizrahi, B.; Shilo, S.; Rossman, H.; Kalkstein, N.; Marcus, K.; Barer, Y.; Keshet, A.; Shamir-Stein, N.; Shalev, V.; Zohar, A.E.; et al. Longitudinal symptom dynamics of COVID-19 infection. Nat. Commun. 2020, 11, 6208. [Google Scholar] [CrossRef]
- Vindegaard, N.; Benros, M.E. COVID-19 pandemic and mental health consequences: Systematic review of the current evidence. Brain Behav. Immun. 2020, 89, 531–542. (In English) [Google Scholar] [CrossRef]
- Madrigal, C.; Bower, E.; Simons, K.; Gillespie, S.M.; Van Orden, K.; Mills, W.L. Assessing Social Functioning During COVID-19 and Beyond: Tools and Considerations for Nursing Home Staff. J. Am. Med. Dir. Assoc. 2021, 22, 1989–1997. [Google Scholar] [CrossRef]
- McGinty, E.E.; Presskreischer, R.; Han, H.; Barry, C.L. Psychological Distress and Loneliness Reported by US Adults in 2018 and April 2020. JAMA 2020, 324, 93–94. [Google Scholar] [CrossRef]
- Deng, J.; Zhou, F.; Hou, W.; Silver, Z.; Wong, C.Y.; Chang, O.; Huang, E.; Zuo, Q.K. The prevalence of depression, anxiety, and sleep disturbances in COVID-19 patients: A meta-analysis. Ann. N. Y. Acad. Sci. 2021, 1486, 90–111. [Google Scholar] [CrossRef]
- Wostyn, P. COVID-19 and chronic fatigue syndrome: Is the worst yet to come? Med. Hypotheses 2021, 146, 110469. [Google Scholar] [CrossRef]
- Hale, T.; Webster, S.; Petherick, A.; Phillips, T.; Kira, B. Oxford COVID-19 government response tracker (OxCGRT). Last Updated 2020, 8, 30. [Google Scholar]
- Stenman, U.; Hakama, M.; Knekt, P.; Aromaa, A.; Teppo, L.; Leinonen, J.; Zhang, B.; Yang, B.; Tang, Z. Measurement and modeling of health-related quality of life. Epidem Demog Public Health 2010, 195, 130–135. [Google Scholar]
- Herrman, H.; Saxena, S.; Moodie, R. Promoting Mental Health: Concepts, Emerging Evidence, Practice: A Report of the World Health Organization, Department of Mental Health and Substance Abuse in Collaboration with the Victorian Health Promotion Foundation and the University of Melbourne; World Health Organization: Geneva, Switzerland, 2005. [Google Scholar]
- O’Dwyer, M.C.; Meixner, K.; Albiac, L.C.; El Khoury, C.; Capizzano, J.N.; Ramakrishnan, M.; Salada, C.; Furst, W.; Haro, E.; Alves, M. Health-Related Quality of Life for People With Acute and Chronic Illnesses During the COVID-19 Pandemic. J. Am. Board Fam. Med. 2021, 34, 509–521. [Google Scholar] [CrossRef]
- Epifanio, M.S.; Andrei, F.; Mancini, G.; Agostini, F.; Piombo, M.A.; Spicuzza, V.; Riolo, M.; Lavanco, G.; Trombini, E.; La Grutta, S. The Impact of COVID-19 Pandemic and Lockdown Measures on Quality of Life among Italian General Population. J. Clin. Med. 2021, 10, 289. (In English) [Google Scholar] [CrossRef]
- Ping, W.; Zheng, J.; Niu, X.; Guo, C.; Zhang, J.; Yang, H.; Shi, Y. Evaluation of health-related quality of life using EQ-5D in China during the COVID-19 pandemic. PLoS ONE 2020, 15, e0234850. [Google Scholar] [CrossRef]
- Ferreira, L.N.; Pereira, L.N.; da Fe Bras, M.; Ilchuk, K. Quality of life under the COVID-19 quarantine. Qual. Life Res. 2021, 30, 1389–1405. (In English) [Google Scholar] [CrossRef]
- Shek, D.T.L. COVID-19 and Quality of Life: Twelve Reflections. Appl. Res. Qual. Life 2021, 16, 1–11. [Google Scholar] [CrossRef]
- Didriksen, M.; Werge, T.; Nissen, J.; Schwinn, M.; Sorensen, E.; Nielsen, K.R.; Bruun, M.T.; Banasik, K.; Hansen, T.F.; Erikstrup, C.; et al. Impact of COVID-19 Pandemic on Sleep Quality, Stress Level and Health-Related Quality of Life-A Large Prospective Cohort Study on Adult Danes. Int. J. Environ. Res. Public Health 2021, 18, 7610. (In English) [Google Scholar] [CrossRef]
- Watkinson, R.E.; Sutton, M.; Turner, A.J. Ethnic inequalities in health-related quality of life among older adults in England: Secondary analysis of a national cross-sectional survey. Lancet Public Health 2021, 6, e145–e154. [Google Scholar] [CrossRef]
- Posel, D.; Oyenubi, A.; Kollamparambil, U. Job loss and mental health during the COVID-19 lockdown: Evidence from South Africa. PLoS ONE 2021, 16, e0249352. [Google Scholar] [CrossRef] [PubMed]
- Ikeda, T.; Igarashi, A.; Odani, S.; Murakami, M.; Tabuchi, T. Health-related quality of life during COVID-19 pandemic: Assessing impacts of job loss and financial support programs in Japan. Appl. Res. Qual. Life 2022, 17, 541–557. [Google Scholar] [CrossRef] [PubMed]
- Michelen, M.; Manoharan, L.; Elkheir, N.; Cheng, V.; Dagens, A.; Hastie, C.; O’Hara, M.; Suett, J.; Dahmash, D.; Bugaeva, P.; et al. Characterising long COVID: A living systematic review. BMJ Glob. Health 2021, 6, e005427. [Google Scholar] [CrossRef] [PubMed]
- Robinson, E.; Sutin, A.R.; Daly, M.; Jones, A. A systematic review and meta-analysis of longitudinal cohort studies comparing mental health before versus during the COVID-19 pandemic. medRxiv 2021. [Google Scholar] [CrossRef]
- Koenig, J.; Kohls, E.; Moessner, M.; Lustig, S.; Bauer, S.; Becker, K.; Thomasius, R.; Eschenbeck, H.; Diestelkamp, S.; Gille, V.; et al. The impact of COVID-19 related lockdown measures on self-reported psychopathology and health-related quality of life in German adolescents. Eur. Child Adolesc. Psychiatry 2021, 1–10. [Google Scholar] [CrossRef]
- Sardella, A.; Lenzo, V.; Bonanno, G.A.; Basile, G.; Quattropani, M.C. Expressive Flexibility and Dispositional Optimism Contribute to the Elderly’s Resilience and Health-Related Quality of Life during the COVID-19 Pandemic. Int. J. Environ. Res. Public Health 2021, 18, 1698. [Google Scholar] [CrossRef]
- Ravens-Sieberer, U.; Kaman, A.; Erhart, M.; Otto, C.; Devine, J.; Löffler, C.; Hurrelmann, K.; Bullinger, M.; Barkmann, C.; Siegel, N.A. Quality of life and mental health in children and adolescents during the first year of the COVID-19 pandemic: Results of a two-wave nationwide population-based study. Eur. Child Adolesc. Psychiatry 2021, 1–14. [Google Scholar] [CrossRef]
- Do Nascimento, R.J.; Barbosa Filho, V.C.; Rech, C.R.; Brasil, R.B.; Junior, R.C.; Streit, I.A.; de Souza Bezerra, E. Changes in Health-Related Quality of Life and Physical Activity Among Older Adults in the First-Wave COVID-19 Outbreak: A Longitudinal Analysis. J. Aging Phys. Act. 2021, 30, 389–396. [Google Scholar] [CrossRef]
- Long, D.; Haagsma, J.A.; Janssen, M.F.; Yfantopoulos, J.N.; Lubetkin, E.I.; Bonsel, G.J. Health-related quality of life and mental well-being of healthy and diseased persons in 8 countries: Does stringency of government response against early COVID-19 matter? SSM Popul. Health 2021, 15, 100913. (In English) [Google Scholar] [CrossRef]
- Devlin, N.J.; Brooks, R. EQ-5D and the EuroQol Group: Past, Present and Future. Appl. Health Econ. Health Policy 2017, 15, 127–137. [Google Scholar] [CrossRef]
- Oppe, M.; Devlin, N.J.; Szende, A. EQ-5D Value Sets: Inventory, Comparative Review and User Guide; Springer: Berlin/Heidelberg, Germany, 2007. [Google Scholar]
- Pickard, A.S.; Law, E.H.; Jiang, R.; Pullenayegum, E.; Shaw, J.W.; Xie, F.; Oppe, M.; Boye, K.S.; Chapman, R.H.; Gong, C.L.; et al. United States Valuation of EQ-5D-5L Health States Using an International Protocol. Value Health 2019, 22, 931–941. [Google Scholar] [CrossRef] [PubMed]
- Topp, C.W.; Ostergaard, S.D.; Sondergaard, S.; Bech, P. The WHO-5 Well-Being Index: A systematic review of the literature. Psychother. Psychosom. 2015, 84, 167–176. [Google Scholar] [CrossRef] [PubMed]
- Brooks, R. EuroQol: The current state of play. Health Policy 1996, 37, 53–72. (In English) [Google Scholar] [CrossRef]
- Rogers, A.M.; Lauren, B.N.; Baidal, J.A.W.; Ozanne, E.M.; Hur, C. Persistent effects of the COVID-19 pandemic on diet, exercise, risk for food insecurity, and quality of life: A longitudinal study among US adults. Appetite 2021, 167, 105639. [Google Scholar] [CrossRef] [PubMed]
- Pieh, C.; Budimir, S.; Humer, E.; Probst, T. Comparing Mental Health During the COVID-19 Lockdown and 6 Months After the Lockdown in Austria: A Longitudinal Study. Front. Psychiatry 2021, 12, 197. [Google Scholar] [CrossRef]
- Colucci, E.; Nadeau, S.; Higgins, J.; Kehayia, E.; Poldma, T.; Saj, A.; de Guise, E. COVID-19 lockdowns’ effects on the quality of life, perceived health and well-being of healthy elderly individuals: A longitudinal comparison of pre-lockdown and lockdown states of well-being. Arch. Gerontol. Geriatr. 2022, 99, 104606. [Google Scholar] [CrossRef]
- Bolbocean, C.; Rhidenour, K.B.; McCormack, M.; Suter, B.; Holder, J.L. Resilience, and positive parenting in parents of children with syndromic autism and intellectual disability. Evidence from the impact of the COVID-19 pandemic on family’s quality of life and parent-child relationships. Autism Res. 2022. (In English) [Google Scholar] [CrossRef]
- Lee, Y.; Lui, L.M.; Chen-Li, D.; Liao, Y.; Mansur, R.B.; Brietzke, E.; Rosenblat, J.D.; Ho, R.; Rodrigues, N.B.; Lipsitz, O. Government response moderates the mental health impact of COVID-19: A systematic review and meta-analysis of depression outcomes across countries. J. Affect. Disord. 2021, 290, 364–377. [Google Scholar] [CrossRef]
- Schneider, C.R.; Dryhurst, S.; Kerr, J.; Freeman, A.L.; Recchia, G.; Spiegelhalter, D.; van der Linden, S. COVID-19 risk perception: A longitudinal analysis of its predictors and associations with health protective behaviours in the United Kingdom. J. Risk Res. 2021, 24, 294–313. [Google Scholar] [CrossRef]
- Koltai, J.; Raifman, J.; Bor, J.; McKee, M.; Stuckler, D. COVID-19 Vaccination and Mental Health: A Difference-In-Difference Analysis of the Understanding America Study. Am. J. Prev. Med. 2022, 62, 679–687. (In English) [Google Scholar] [CrossRef]
- Garrote Sanchez, D.; Gomez Parra, N.; Ozden, C.; Rijkers, B. Which Jobs Are Most Vulnerable to COVID-19? What an Analysis of the European Union Reveals. In Research and Policy Brief; No. 34; World Bank: Washington, DC, USA, 2020. [Google Scholar]
- Chen, C.W.S.; Lee, S.; Dong, M.C.; Taniguchi, M. What factors drive the satisfaction of citizens with governments’ responses to COVID-19? Int. J. Infect. Dis. 2021, 102, 327–331. (In English) [Google Scholar] [CrossRef]
- Sibley, C.G.; Greaves, L.M.; Satherley, N.; Wilson, M.S.; Overall, N.C.; Lee, C.H.J.; Milojev, P.; Bulbulia, J.; Osborne, D.; Milfont, T.L.; et al. Effects of the COVID-19 Pandemic and Nationwide Lockdown on Trust, Attitudes Toward Government, and Well-Being. Am. Psychol. 2020, 75, 618–630. (In English) [Google Scholar] [CrossRef]
- Catucci, A.; Scognamiglio, U.; Rossi, L. Lifestyle Changes Related to Eating Habits, Physical Activity, and Weight Status During COVID-19 Quarantine in Italy and Some European Countries. Front. Nutr. 2021, 8, 718877. (In English) [Google Scholar] [CrossRef]
- Suzuki, Y.; Maeda, N.; Hirado, D.; Shirakawa, T.; Urabe, Y. Physical Activity Changes and Its Risk Factors among Community-Dwelling Japanese Older Adults during the COVID-19 Epidemic: Associations with Subjective Well-Being and Health-Related Quality of Life. Int. J. Environ. Res. Public Health 2020, 17, 6591. (In English) [Google Scholar] [CrossRef]
- Pujolar, G.; Oliver-Angles, A.; Vargas, I.; Vazquez, M.L. Changes in Access to Health Services during the COVID-19 Pandemic: A Scoping Review. Int. J. Environ. Res. Public Health 2022, 19, 1749. (In English) [Google Scholar] [CrossRef]
- Topriceanu, C.C.; Wong, A.; Moon, J.C.; Hughes, A.D.; Bann, D.; Chaturvedi, N.; Patalay, P.; Conti, G.; Captur, G. Evaluating access to health and care services during lockdown by the COVID-19 survey in five UK national longitudinal studies. BMJ Open 2021, 11, e045813. (In English) [Google Scholar] [CrossRef]
- Fink, G.; Tediosi, F.; Felder, S. Burden of COVID-19 restrictions: National, regional and global estimates. EClinicalMedicine 2022, 45, 101305. [Google Scholar] [CrossRef]
- Pedersen, M.T.; Andersen, T.O.; Clotworthy, A.; Jensen, A.K.; Strandberg-Larsen, K.; Rod, N.H.; Varga, T.V. Time trends in mental health indicators during the initial 16 months of the COVID-19 pandemic in Denmark. BMC Psychiatry 2022, 22, 25. [Google Scholar] [CrossRef]
- Daly, M.; Robinson, E. Psychological distress and adaptation to the COVID-19 crisis in the United States. J. Psychiatr. Res. 2021, 136, 603–609. [Google Scholar] [CrossRef]
- Kraaij, V.; De Wilde, E. Negative life events and depressive symptoms in the elderly: A life span perspective. Aging Ment. Health 2001, 5, 84–91. [Google Scholar] [CrossRef]
- Frijters, P.; Johnston, D.W.; Shields, M.A. Life satisfaction dynamics with quarterly life event data. Scand. J. Econ. 2011, 113, 190–211. [Google Scholar] [CrossRef]
- Luhmann, M.; Hofmann, W.; Eid, M.; Lucas, R.E. Subjective well-being and adaptation to life events: A meta-analysis. J. Personal. Soc. Psychol. 2012, 102, 592. [Google Scholar] [CrossRef]
- Brown, J.D.; McGill, K.L. The cost of good fortune: When positive life events produce negative health consequences. J. Personal. Soc. Psychol. 1989, 57, 1103. [Google Scholar] [CrossRef]
- Shimizu, M.; Pelham, B.W. The unconscious cost of good fortune: Implicit and explicit self-esteem, positive life events, and health. Health Psychol. 2004, 23, 101. [Google Scholar] [CrossRef]
- Ahmed, F.; Ahmed, N.; Pissarides, C.; Stiglitz, J. Why inequality could spread COVID-19. Lancet Public Health 2020, 5, e240. (In English) [Google Scholar] [CrossRef]
- Spronk, I.; Haagsma, J.A.; Lubetkin, E.I.; Polinder, S.; Janssen, M.F.; Bonsel, G.J. Health Inequality Analysis in Europe: Exploring the Potential of the EQ-5D as Outcome. Front. Public Health 2021, 9, 744405. (In English) [Google Scholar] [CrossRef]
- Agborsangaya, C.B.; Lau, D.; Lahtinen, M.; Cooke, T.; Johnson, J.A. Health-related quality of life and healthcare utilization in multimorbidity: Results of a cross-sectional survey. Qual. Life Res. 2013, 22, 791–799. (In English) [Google Scholar] [CrossRef]
- De Rosa, S.; Spaccarotella, C.; Basso, C.; Calabrò, M.P.; Curcio, A.; Filardi, P.P.; Mancone, M.; Mercuro, G.; Muscoli, S.; Nodari, S. Reduction of hospitalizations for myocardial infarction in Italy in the COVID-19 era. Eur. Heart J. 2020, 41, 2083–2088. [Google Scholar] [CrossRef]
- Stroud, I.; Gutman, L.M. Longitudinal changes in the mental health of UK young male and female adults during the COVID-19 pandemic. Psychiatry Res. 2021, 303, 114074. (In English) [Google Scholar] [CrossRef]
- Daly, M.; Sutin, A.R.; Robinson, E. Longitudinal changes in mental health and the COVID-19 pandemic: Evidence from the UK Household Longitudinal Study. Psychol. Med. 2020, 1–10. (In English) [Google Scholar] [CrossRef]
- Buizza, C.; Bazzoli, L.; Ghilardi, A. Changes in College Students Mental Health and Lifestyle During the COVID-19 Pandemic: A Systematic Review of Longitudinal Studies. Adolesc. Res. Rev. 2022, 7, 537–550. (In English) [Google Scholar] [CrossRef] [PubMed]
- Pierce, M.; McManus, S.; Hope, H.; Hotopf, M.; Ford, T.; Hatch, S.L.; John, A.; Kontopantelis, E.; Webb, R.T.; Wessely, S.; et al. Mental health responses to the COVID-19 pandemic: A latent class trajectory analysis using longitudinal UK data. Lancet Psychiatry 2021, 8, 610–619. (In English) [Google Scholar] [CrossRef]
- Ahrens, K.F.; Neumann, R.J.; Kollmann, B.; Brokelmann, J.; von Werthern, N.M.; Malyshau, A.; Weichert, D.; Lutz, B.; Fiebach, C.J.; Wessa, M.; et al. Impact of COVID-19 lockdown on mental health in Germany: Longitudinal observation of different mental health trajectories and protective factors. Transl. Psychiatry 2021, 11, 392. (In English) [Google Scholar] [CrossRef] [PubMed]
- Choi, I.; Kim, J.H.; Kim, N.; Choi, E.; Choi, J.; Suk, H.W.; Na, J.Y. How COVID-19 affected mental well-being: An 11-week trajectories of daily well-being of Koreans amidst COVID-19 by age, gender and region. PLoS ONE 2021, 16, e0250252. (In English) [Google Scholar] [CrossRef] [PubMed]
- Vistisen, H.T.; Sonderskov, K.M.; Dinesen, P.T.; Ostergaard, S.D. Psychological well-being and symptoms of depression and anxiety across age groups during the second wave of the COVID-19 pandemic in Denmark. Acta Neuropsychiatr. 2021, 33, 331–334. (In English) [Google Scholar] [CrossRef]
- Pieh, C.; Probst, T.; Budimir, S.; Humer, E. Diminished well-being persists beyond the end of the COVID-19 lockdown. Gen. Hosp. Psychiatry 2021, 70, 137–138. (In English) [Google Scholar] [CrossRef]
- Swan, D.A.; Bracis, C.; Janes, H.; Moore, M.; Matrajt, L.; Reeves, D.B.; Burns, E.; Donnell, D.; Cohen, M.S.; Schiffer, J.T. COVID-19 vaccines that reduce symptoms but do not block infection need higher coverage and faster rollout to achieve population impact. Sci. Rep. 2021, 11, 15531. [Google Scholar] [CrossRef]
- Chen, S.; Aruldass, A.R.; Cardinal, R.N. Mental health outcomes after SARS-CoV-2 vaccination in the United States: A national cross-sectional study. J. Affect. Disord. 2022, 298, 396–399. [Google Scholar] [CrossRef]
- Bryson, W.J. Long-term health-related quality of life concerns related to the COVID-19 pandemic: A call to action. Qual. Life Res. 2021, 30, 643–645. [Google Scholar] [CrossRef]
- Halioua, B.; Zetlaoui, J.; Astruc, A.; Lévy-Heidmann, T.; Testa, D.; Bombezin, A.; Radoszycki, L. PMU85 IMPACT of the COVID-19 pandemic on patients affected by chronic diseases in Europe. Value Health 2020, 23, S617. [Google Scholar] [CrossRef]
- Arndt, C.; Davies, R.; Gabriel, S.; Harris, L.; Makrelov, K.; Robinson, S.; Levy, S.; Simbanegavi, W.; van Seventer, D.; Anderson, L. COVID-19 lockdowns, income distribution, and food security: An analysis for South Africa. Glob. Food Secur. 2020, 26, 100410. [Google Scholar] [CrossRef]
- CDC Prevention. Indicators of Anxiety or Depression Based on Reported Frequency of Symptoms during the Last 7 Days. Available online: https://www.cdc.gov/nchs/covid19/pulse/mental-health.htm (accessed on 9 November 2021).

| Greece | Italy | Netherlands | UK | US | Total | |
|---|---|---|---|---|---|---|
| Number of respondents at T2 | 511 | 1784 | 1143 | 1448 | 1879 | 6765 |
| Response rate (T2/T1) | 50% | 56% | 35% | 45% | 32% | 35% |
| Baseline characteristics (T1) | ||||||
| Age | ||||||
| Median (IQR) | 43.3 (12.5) | 46.8 (13.7) | 54.1 (13.9) | 51.5 (14.2) | 54.3 (13.0) | 50.8 (14.1) |
| Mean (SD) | 43 (18) | 45 (21) | 57 (21) | 53 (24) | 56 (20) | 51 (23) |
| Age groups | ||||||
| 18–24 yrs. | 43 (8%) | 74 (4%) | 40 (3%) | 47 (3%) | 25 (1%) | 229 (3%) |
| 25–34 yrs. | 91 (18%) | 296 (17%) | 84 (7%) | 171 (12%) | 142 (8%) | 784 (12%) |
| 35–44 yrs. | 135 (26%) | 464 (26%) | 172 (15%) | 273 (19%) | 287 (15%) | 1331 (20%) |
| 45–54 yrs. | 128 (25%) | 413 (23%) | 227 (20%) | 281 (19%) | 425 (23%) | 1474 (22%) |
| 55–64 yrs. | 88 (17%) | 291 (16%) | 295 (26%) | 344 (24%) | 498 (27%) | 1516 (22%) |
| 65–75 yrs. | 26 (5%) | 246 (14%) | 325 (28%) | 332 (23%) | 502 (27%) | 1431 (21%) |
| Sex | ||||||
| Male | 263 (51%) | 859 (48%) | 526 (46%) | 709 (49%) | 869 (46%) | 3226 (48%) |
| Female | 248 (49%) | 925 (52%) | 617 (54%) | 739 (51%) | 1010 (54%) | 3539 (52%) |
| Education level | ||||||
| High | 343 (67%) | 726 (41%) | 464 (41%) | 807 (56%) | 1393 (74%) | 3733 (55%) |
| Middle | 153 (30%) | 786 (44%) | 351 (31%) | 608 (42%) | 434 (23%) | 2332 (34%) |
| Low | 15 (3%) | 272 (15%) | 328 (29%) | 33 (2%) | 52 (3%) | 700 (10%) |
| Occupation status | ||||||
| Employed | 289 (57%) | 1008 (57%) | 552 (48%) | 797 (55%) | 976 (52%) | 3622 (54%) |
| Student | 31 (6%) | 77 (4%) | 34 (3%) | 17 (1%) | 15 (1%) | 174 (3%) |
| Unemployed | 134 (26%) | 415 (23%) | 124 (11%) | 160 (11%) | 234 (12%) | 1067 (16%) |
| Retired | 52 (10%) | 269 (15%) | 305 (27%) | 365 (25%) | 559 (30%) | 1550 (23%) |
| Unable to work | 5 (1%) | 15 (1%) | 128 (11%) | 109 (8%) | 95 (5%) | 352 (5%) |
| Income level | ||||||
| High | 177 (35%) | 227 (13%) | 215 (19%) | 327 (23%) | 490 (26%) | 1448 (21%) |
| Middle | 162 (32%) | 998 (56%) | 513 (45%) | 616 (43%) | 986 (52%) | 1879 (48%) |
| Low | 121 (24%) | 369 (21%) | 182 (16%) | 383 (26%) | 290 (15%) | 1143 (15%) |
| Unwilling to tell | 27 (5%) | 190 (11%) | 233 (20%) | 122 (8%) | 113 (6%) | 1784 (6%) |
| Unknown | 12 (3%) | - | - | - | - | - |
| Number of chronic conditions | ||||||
| 0 | 304 (59%) | 1128 (63%) | 545 (48%) | 830 (57%) | 1081 (58%) | 3888 (57%) |
| 1 | 153 (30%) | 461 (26%) | 369 (32%) | 379 (26%) | 508 (27%) | 1870 (28%) |
| 2 | 36 (7%) | 118 (7%) | 139 (12%) | 152 (10%) | 181 (10%) | 626 (9%) |
| 3 | 11 (2%) | 41 (2%) | 54 (5%) | 57 (4%) | 67 (4%) | 230 (3%) |
| 4 or more | 7 (1%) | 36 (2%) | 36 (3%) | 30 (2%) | 42 (2%) | 151 (2%) |
| COVID-19 status at T1 | ||||||
| Not infected | 507 (99%) | 1756 (98%) | 1115 (98%) | 1421 (98%) | 1823 (97%) | 6662 (98%) |
| Infected | 4 (1%) | 28 (2%) | 28 (2%) | 157 (2%) | 56 (3%) | 143 (2%) |
| Living situation | ||||||
| Not living alone | 437 (86%) | 1615 (91%) | 810 (71%) | 1143 (79%) | 1472 (78%) | 5477 (81%) |
| Living alone | 74 (14%) | 169 (9%) | 333 (29%) | 305 (21%) | 407 (22%) | 1288 (19%) |
| Change between T1 (April–May 2020) and T2 (May–June 2021) | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Characteristic | N | tEQ-5D Level Sum Score | tEQ-5D Index | EQ VAS | WHO-5 Index | ||||
| Coefficient | p-Value | Coefficient | p-Value | Coefficient | p-Value | Coefficient | p-Value | ||
| Age group | |||||||||
| Intercept | 0.1 | 0.894 | 0.5 | 0.637 | -1.5 | 0.126 | 0.2 | 0.883 | |
| 18–24 (ref) | 229 | ||||||||
| 25–34 | 783 | -0.1 | 0.913 | −0.4 | 0.736 | 0.5 | 0.612 | 1.1 | 0.455 |
| 35–44 | 1329 | 0.0 | 0.991 | −0.5 | 0.638 | −0.2 | 0.838 | −1.0 | 0.466 |
| 45–54 | 1469 | 0.1 | 0.929 | 0.0 | 0.965 | 0.0 | 0.974 | 0.6 | 0.684 |
| 55–64 | 1514 | −0.1 | 0.857 | −0.5 | 0.650 | 0.3 | 0.802 | 0.6 | 0.694 |
| 65–75 | 1429 | −0.4 | 0.536 | −1.0 | 0.358 | −0.2 | 0.882 | 0.4 | 0.779 |
| Sex | |||||||||
| Intercept | −0.1 | 0.736 | −0.1 | 0.690 | −1.1 | <0.001 | 0.2 | 0.604 | |
| Male (ref) | 3220 | ||||||||
| Female | 3533 | 0.1 | 0.825 | 0.2 | 0.585 | −0.6 | 0.065 | 0.5 | 0.286 |
| Education level | |||||||||
| Intercept | −0.1 | 0.552 | −0.1 | 0.605 | −1.5 | <0.001 | 1.0 | 0.002 | |
| High (ref) | 3724 | ||||||||
| Middle | 2329 | 0.1 | 0.611 | 0.3 | 0.495 | 0.4 | 0.254 | −1.0 | 0.056 |
| Low | 700 | 0.2 | 0.643 | 0.3 | 0.609 | −0.3 | 0.563 | −2.0 | 0.014 |
| Occupation status | |||||||||
| Intercept | 0.1 | 0.591 | 0.2 | 0.475 | −1.3 | <0.001 | 0.6 | 0.057 | |
| Employed (ref) | 3614 | ||||||||
| Student | 174 | −0.3 | 0.679 | −0.6 | 0.608 | 0.5 | 0.633 | −0.8 | 0.618 |
| Unemployed | 1066 | −0.2 | 0.490 | −0.4 | 0.416 | −0.3 | 0.489 | −0.6 | 0.423 |
| Retired | 1547 | −0.4 | 0.143 | −0.7 | 0.120 | −0.3 | 0.538 | −0.3 | 0.599 |
| Unable to work | 352 | 0.5 | 0.345 | 1.2 | 0.132 | −0.1 | 0.941 | 0.0 | 0.976 |
| Income | |||||||||
| Intercept | 0.4 | 0.091 | 0.5 | 0.180 | −1.0 | 0.010 | 0.6 | 0.224 | |
| High (ref) | 1436 | ||||||||
| Middle | 3275 | −0.4 | 0.194 | −0.4 | 0.380 | −0.4 | 0.364 | 0.2 | 0.711 |
| Low | 1345 | −1.3 | <0.001 | −1.6 | 0.004 | −1.2 | 0.030 | −1.1 | 0.153 |
| Chronic disease status | |||||||||
| Intercept | −0.3 | 0.038 | −0.5 | 0.034 | −1.6 | <0.001 | 0.2 | 0.560 | |
| No chronic disease (ref) | 3881 | ||||||||
| With chronic disease | 2872 | 0.7 | 0.004 | 1.2 | 0.001 | 0.5 | 0.150 | 0.6 | 0.201 |
| COVID-19 status | |||||||||
| Intercept | −0.1 | 0.427 | −0.1 | 0.462 | −1.4 | <0.001 | 0.3 | 0.168 | |
| Not infected at T1 (ref) | 6610 | ||||||||
| Infected at T1 | 143 | 3.1 | <0.001 | 6.2 | <0.001 | 0.3 | 0.829 | 5.4 | 0.001 |
| Living situation | |||||||||
| Intercept | −0.6 | 0.023 | −1.0 | 0.016 | −1.9 | <0.001 | −0.3 | 0.602 | |
| Not living alone (ref) | 5469 | ||||||||
| Living alone | 1284 | −0.7 | 0.016 | −1.2 | 0.007 | −0.6 | 0.197 | −0.9 | 0.138 |
| Country | |||||||||
| Intercept | 0.8 | 0.078 | 1.0 | 0.114 | −0.2 | 0.735 | −5.3 | <0.001 | |
| Greece(ref) | 499 | ||||||||
| Italy | 1784 | −0.3 | 0.532 | −0.5 | 0.491 | −0.7 | 0.371 | 5.7 | <0.001 |
| Netherlands | 1143 | −0.8 | 0.153 | −0.8 | 0.307 | −0.8 | 0.329 | 4.6 | <0.001 |
| UK | 1448 | −1.3 | 0.010 | −1.7 | 0.027 | −2.3 | 0.002 | 4.6 | <0.001 |
| US | 1879 | −1.1 | 0.022 | −1.5 | 0.048 | −1.4 | 0.052 | 9.1 | <0.001 |
| Change between T1 (April–May 2020) and T2 (May–June 2021) | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Characteristic | N | tEQ-5D Level Sum Score | tEQ-5D Index | EQ VAS | WHO-5 Index | ||||
| Coeff. | p-Value | Coeff. | p-Value | Coeff. | p-Value | Coeff. | p-Value | ||
| Intercept | 1.0 | 0.055 | 1.0 | 0.150 | -0.2 | 0.735 | -5.4 | <0.001 | |
| Income | |||||||||
| High (ref) | 1436 | ||||||||
| Middle | 3275 | −0.5 | 0.154 | −0.3 | 0.358 | ||||
| Low | 1345 | −1.4 | <0.001 | −1.7 | 0.002 | ||||
| Chronic disease status | |||||||||
| No chronic disease (ref) | 3881 | ||||||||
| With chronic disease | 2872 | 0.8 | 0.001 | 1.2 | <0.001 | ||||
| COVID-19 status | |||||||||
| Not infected at T1 (ref) | 6610 | ||||||||
| Infected at T1 | 143 | 3.0 | <0.001 | 6.1 | <0.001 | 4.7 | 0.004 | ||
| Country | |||||||||
| Greece (ref) | 499 | ||||||||
| Italy | 1784 | −0.2 | 0.623 | −0.5 | 0.527 | −0.7 | 0.371 | 5.6 | <0.001 |
| Netherlands | 1143 | −0.9 | 0.077 | −1.1 | 0.149 | −0.8 | 0.329 | 4.5 | <0.001 |
| UK | 1448 | −1.3 | 0.012 | −1.7 | 0.026 | −2.3 | 0.002 | 4.5 | <0.001 |
| US | 1879 | −1.3 | 0.011 | −1.7 | 0.023 | −1.4 | 0.052 | 8.9 | <0.001 |
| F-value | 5.9 | <0.001 | 5.9 | <0.001 | 4.0 | 0.002 | 22.9 | <0.001 | |
| R-square | 0.008 | 0.009 | 0.002 | 0.017 | |||||
| Mean Change in Scores between T1 and T2 | |||||
|---|---|---|---|---|---|
| Life Event | n | tEQ-5D-5L Level Sum Score | tEQ-5D-5L Index | EQ VAS | WHO-5 |
| Number of chronic disease(s) | |||||
| Decreased | 1202 | 1.90 | 2.86 | 0.09 | 3.57 |
| Same | 4672 | −0.003 | 0.02 | −1.20 | 0.59 |
| Increased | 891 | −2.81 | −4.03 | −4.53 | −4.53 |
| COVID-19 status | |||||
| No (past) COVID-19 infection at T1 and T2 | 6442 | 0.04 | 0.07 | −1.33 | 0.52 |
| (past) COVID-19 infection at T1 | 27 | 0.74 | 1.26 | −4.44 | −4.74 |
| (past) COVID-19 infection between T1 and T2 | 296 | −1.69 | −1.93 | −2.86 | −0.72 |
| Vaccination status | |||||
| Received vaccine at T2 | 3945 | −0.17 | −0.22 | −1.58 | 1.36 |
| Not received vaccine at T2 | 2820 | 0.16 | 0.28 | −1.17 | −0.83 |
| Change in work status * | |||||
| Gained job | 218 | 1.35 | 1.91 | −0.21 | 2.44 |
| Kept job | 3361 | 0.30 | 0.42 | −1.08 | 0.70 |
| Lost job | 116 | −1.77 | −1.12 | −4.59 | −3.10 |
| Remained unemployed | 422 | −0.37 | −0.71 | −0.98 | −0.59 |
| Change in income in past year (T1-T2) | |||||
| Improved | 782 | −0.25 | −0.41 | −2.02 | 1.70 |
| Remained the same | 4564 | 0.16 | 0.27 | −0.95 | 1.39 |
| Worsened | 1322 | −0.60 | −0.77 | −2.61 | −3.44 |
| Don’t know | 97 | 0.31 | 0.39 | −1.55 | −1.40 |
| Living situation | |||||
| Living with others at T1 and T2 | 5314 | 0.14 | 0.27 | −1.30 | 0.68 |
| Living alone at T1 and T2 | 1164 | −0.52 | −0.81 | −1.69 | −0.10 |
| Living alone at T1 and with others at T2 | 124 | −1.41 | −2.28 | −3.17 | −1.81 |
| Living with others at T1 and alone at T2 | 163 | −1.17 | −1.58 | −1.53 | −1.74 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Long, D.; Bonsel, G.J.; Lubetkin, E.I.; Yfantopoulos, J.N.; Janssen, M.F.; Haagsma, J.A. Health-Related Quality of Life and Mental Well-Being during the COVID-19 Pandemic in Five Countries: A One-Year Longitudinal Study. J. Clin. Med. 2022, 11, 6467. https://doi.org/10.3390/jcm11216467
Long D, Bonsel GJ, Lubetkin EI, Yfantopoulos JN, Janssen MF, Haagsma JA. Health-Related Quality of Life and Mental Well-Being during the COVID-19 Pandemic in Five Countries: A One-Year Longitudinal Study. Journal of Clinical Medicine. 2022; 11(21):6467. https://doi.org/10.3390/jcm11216467
Chicago/Turabian StyleLong, Di, Gouke J. Bonsel, Erica I. Lubetkin, John N. Yfantopoulos, Mathieu F. Janssen, and Juanita A. Haagsma. 2022. "Health-Related Quality of Life and Mental Well-Being during the COVID-19 Pandemic in Five Countries: A One-Year Longitudinal Study" Journal of Clinical Medicine 11, no. 21: 6467. https://doi.org/10.3390/jcm11216467
APA StyleLong, D., Bonsel, G. J., Lubetkin, E. I., Yfantopoulos, J. N., Janssen, M. F., & Haagsma, J. A. (2022). Health-Related Quality of Life and Mental Well-Being during the COVID-19 Pandemic in Five Countries: A One-Year Longitudinal Study. Journal of Clinical Medicine, 11(21), 6467. https://doi.org/10.3390/jcm11216467





