Robotic-Assisted versus Laparoscopic Proctectomy with Ileal Pouch-Anal Anastomosis for Ulcerative Colitis: An Analysis of Clinical and Financial Outcomes from a Tertiary Referral Center
Abstract
:1. Introduction
2. Materials and Methods
2.1. Patient Cohort
- Age ≥ 18 years;
- Medically refractory ulcerative colitis;
- Elective surgery performed between 1 January 2016, and 31 September 2021;
- Previous laparoscopic colectomy with rectal stump closure and creation of an end ileostomy as a first step according to a three-step procedure.
- Age ≤ 18 years;
- Proven carcinoma or dysplasia;
- Crohn’s disease, indeterminate colitis, or familial adenomatous polyposis;
- Non-elective surgery.
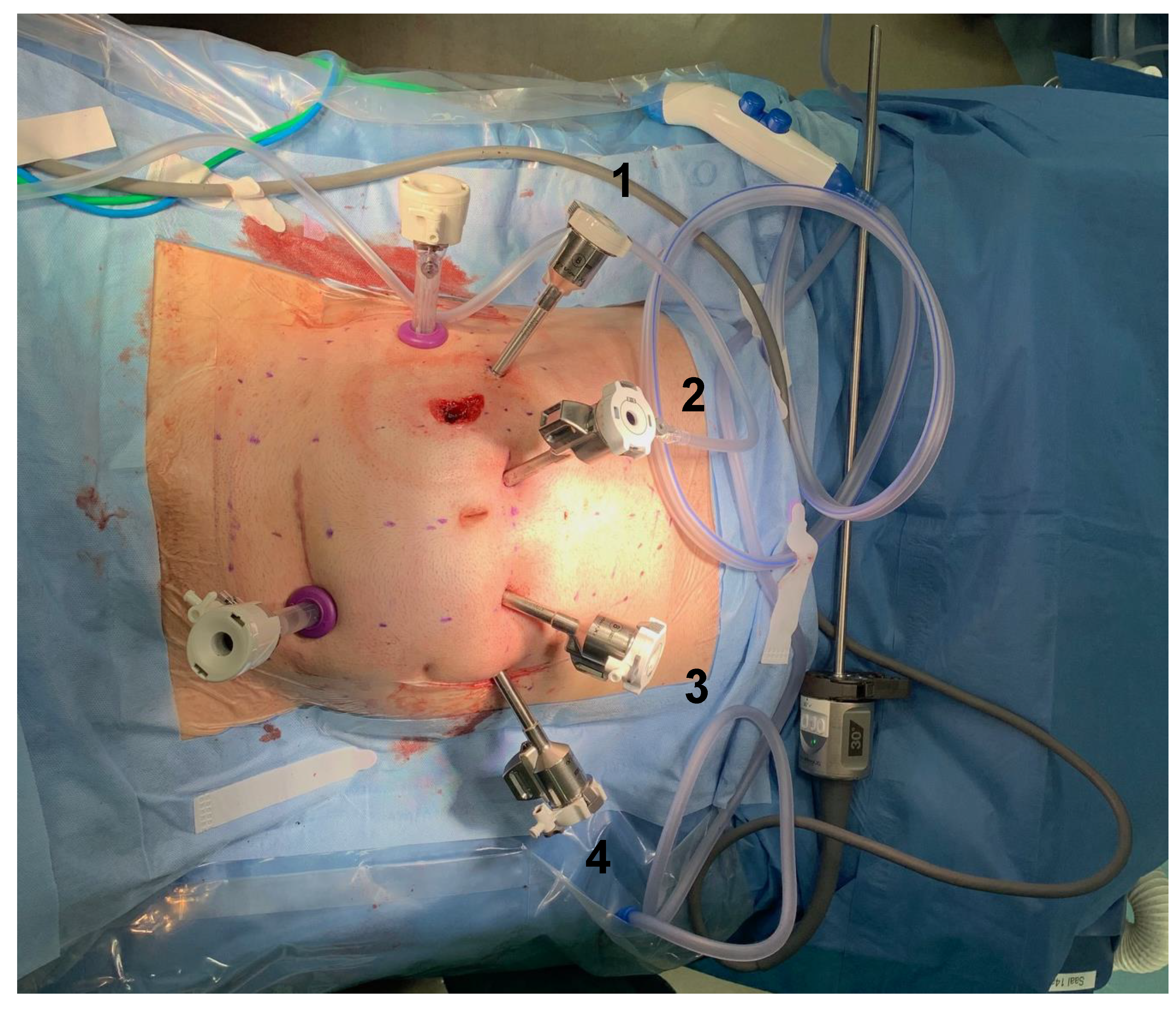
2.2. Surgical Interventions
2.3. Outcome Measures
2.4. Statistical Analysis
3. Results
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Frolkis, A.D.; Dykeman, J.; Negrón, M.E.; Debruyn, J.; Jette, N.; Fiest, K.M.; Frolkis, T.; Barkema, H.; Rioux, K.P.; Panaccione, R.; et al. Risk of Surgery for Inflammatory Bowel Diseases Has Decreased Over Time: A Systematic Review and Meta-analysis of Population-Based Studies. Gastroenterology 2013, 145, 996–1006. [Google Scholar] [CrossRef] [PubMed]
- Bhangu, A.; Singh, P.; Lundy, J.; Bowley, D.M. Systemic Review and Meta-analysis of Randomized Clinical Trials Comparing Primary vs Delayed Primary Skin Closure in Contaminated and Dirty Abdominal Incisions. JAMA Surg. 2013, 148, 779–786. [Google Scholar] [CrossRef] [Green Version]
- Miller, A.T.; Berian, J.R.; Rubin, M.; Hurst, R.D.; Fichera, A.; Umanskiy, K. Robotic-Assisted Proctectomy for Inflammatory Bowel Disease: A Case-Matched Comparison of Laparoscopic and Robotic Technique. J. Gastrointest. Surg. 2012, 16, 587–594. [Google Scholar] [CrossRef] [PubMed]
- Ali, U.A.; Keus, F.; Heikens, J.T.; A Bemelman, W.; Berdah, S.V.; Gooszen, H.G.; Van Laarhoven, C.J. Open versus laparoscopic (assisted) ileo pouch anal anastomosis for ulcerative colitis and familial adenomatous polyposis. Cochrane Database Syst. Rev. 2009, CD006267. [Google Scholar] [CrossRef] [Green Version]
- Schwenk, W.; Haase, O.; Neudecker, J.J.; Müller, J.M. Short term benefits for laparoscopic colorectal resection. Cochrane Database Syst. Rev. 2005, 2008, CD003145. [Google Scholar] [CrossRef] [PubMed]
- The Collaborative LAFA Study Group; Bartels, S.A.L.; Vlug, M.S.; Hollmann, M.W.; Dijkgraaf, M.G.W.; Ubbink, D.T.; Cense, H.A.; van Wagensveld, B.A.; Engel, A.F.; Gerhards, M.F.; et al. Small bowel obstruction, incisional hernia and survival after laparoscopic and open colonic resection (LAFA study). Br. J. Surg. 2014, 101, 1153–1159. [Google Scholar] [CrossRef] [PubMed]
- Kössler-Ebs, J.B.; Grummich, K.; Jensen, K.; Hüttner, F.J.; Müller-Stich, B.; Seiler, C.M.; Knebel, P.; Büchler, M.W.; Diener, M.K. Incisional Hernia Rates After Laparoscopic or Open Abdominal Surgery—A Systematic Review and Meta-Analysis. World J. Surg. 2016, 40, 2319–2330. [Google Scholar] [CrossRef] [PubMed]
- Mark-Christensen, A.; Pachler, F.R.; Nørager, C.B.; Jepsen, P.; Laurberg, S.; Tøttrup, A. Short-term Outcome of Robot-assisted and Open IPAA: An Observational Single-center Study. Dis. Colon Rectum 2016, 59, 201–207. [Google Scholar] [CrossRef]
- Roviello, F.; Piagnerelli, R.; Ferrara, F.; Scheiterle, M.; De Franco, L.; Marrelli, D. Robotic single docking total colectomy for ulcerative colitis: First experience with a novel technique. Int. J. Surg. 2015, 21, 63–67. [Google Scholar] [CrossRef]
- Kim, M.J.; Park, S.C.; Park, J.W.; Chang, H.J.; Kim, D.Y.; Nam, B.-H.; Sohn, D.K.; Oh, J.H. Robot-assisted versus Laparoscopic Surgery for Rectal Cancer: A Phase II Open Label Prospective Randomized Controlled Trial. Ann. Surg. 2018, 267, 243–251. [Google Scholar] [CrossRef]
- Trinh, B.B.; Jackson, N.R.; Hauch, A.T.; Hu, T.; Kandil, E. Robotic Versus Laparoscopic Colorectal Surgery. JSLS J. Soc. Laparoendosc. Surg. 2014, 18, e2014.00187. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Flynn, J.; Larach, J.T.; Kong, J.C.H.; Warrier, S.K.; Heriot, A. Robotic versus laparoscopic ileal pouch-anal anastomosis (IPAA): A systematic review and meta-analysis. Int. J. Color. Dis. 2021, 36, 1345–1356. [Google Scholar] [CrossRef] [PubMed]
- Hota, S.; Parascandola, S.; Amdur, R.; Obias, V. Evaluation of Minimally Invasive Surgical Therapies for Ulcerative Colitis. Am. Surg. 2020, 86, 782–786. [Google Scholar] [CrossRef] [PubMed]
- de Buck van Overstraeten, A.; Mark-Christensen, A.; Wasmann, K.A.; Bastiaenen, V.P.; Buskens, C.J.; Wolthuis, A.M.; Vanbrabant, K.; D’Hoore, A.; Bemelman, W.A.; Tottrup, A.; et al. Transanal Versus Transabdominal Minimally Invasive (Completion) Proctectomy with Ileal Pouch-anal Anastomosis in Ulcerative Colitis: A Comparative Study. Ann. Surg. 2017, 266, 878–883. [Google Scholar] [CrossRef] [PubMed]
- Larson, D.W.; Cima, R.R.; Dozois, E.J.; Davies, M.; Piotrowicz, K.; Barnes, S.A.; Wolff, B.; Pemberton, J. Safety, feasibility, and short-term outcomes of laparoscopic ileal-pouch-anal anastomosis: A single institutional case-matched experience. Ann. Surg. 2006, 243, 667–670; discussion 662–670. [Google Scholar] [CrossRef]
- Dindo, D.; Demartines, N.; Clavien, P.-A. Classification of Surgical Complications: A new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann. Surg. 2004, 240, 205–213. [Google Scholar] [CrossRef] [PubMed]
- Berríos-Torres, S.I.; Umscheid, C.A.; Bratzler, D.W.; Leas, B.; Stone, E.C.; Kelz, R.R.; Reinke, C.E.; Morgan, S.; Solomkin, J.S.; Mazuski, J.E.; et al. Centers for Disease Control and Prevention Guideline for the Prevention of Surgical Site Infection, 2017. JAMA Surg. 2017, 152, 784–791. [Google Scholar] [CrossRef]
- Lungen, M.; Dredge, B.; Rose, A.; Roebuck, C.; Plamper, E.; Lauterbach, K.; Working, G. Using diagnosis-related groups. The situation in the United Kingdom National Health Service and in Germany. Eur. J. Health Econ. 2004, 5, 287–289. [Google Scholar] [CrossRef]
- Strobel, R.M.; Leonhardt, M.; Förster, F.; Neumann, K.; Lobbes, L.A.; Seifarth, C.; Lee, L.D.; Schineis, C.H.W.; Kamphues, C.; Weixler, B.; et al. The impact of surgical site infection—A cost analysis. Langenbeck’s Arch. Surg. 2022, 407, 819–828. [Google Scholar] [CrossRef]
- Jayne, D.; Pigazzi, A.; Marshall, H.; Croft, J.; Corrigan, N.; Copeland, J.; Quirke, P.; West, N.; Rautio, T.; Thomassen, N.; et al. Effect of Robotic-Assisted vs Conventional Laparoscopic Surgery on Risk of Conversion to Open Laparotomy among Patients Undergoing Resection for Rectal Cancer: The ROLARR Randomized Clinical Trial. JAMA 2017, 318, 1569–1580. [Google Scholar] [CrossRef]
- Lightner, A.L.; Grass, F.; McKenna, N.P.; Tilman, M.; Alsughayer, A.; Kelley, S.R.; Behm, K.; Merchea, A.; Larson, D.W. Short-term postoperative outcomes following robotic versus laparoscopic ileal pouch-anal anastomosis are equivalent. Tech. Coloproctol. 2019, 23, 259–266. [Google Scholar] [CrossRef] [PubMed]
- Rencuzogullari, A.; Gorgun, E.; Costedio, M.; Aytac, E.; Kessler, H.; Abbas, M.A.; Remzi, F.H. Case-matched Comparison of Robotic Versus Laparoscopic Proctectomy for Inflammatory Bowel Disease. Surg. Laparosc. Endosc. Percutaneous Tech. 2016, 26, e37–e40. [Google Scholar] [CrossRef] [PubMed]
- Mushtaq, H.H.; Shah, S.K.; Agarwal, A.K. The Current Role of Robotics in Colorectal Surgery. Curr. Gastroenterol. Rep. 2019, 21, 11. [Google Scholar] [CrossRef] [PubMed]
- Cheng, C.L.; Rezac, C. The role of robotics in colorectal surgery. BMJ 2018, 360, j5304. [Google Scholar] [CrossRef]
- Farinha, R.; Puliatti, S.; Mazzone, E.; Amato, M.; Rosiello, G.; Yadav, S.Y.; De Groote, R.; Piazza, P.; Bravi, C.A.; Koukourikis, P.; et al. Potential Contenders for the Leadership in Robotic Surgery. J. Endourol. 2022, 36, 317–326. [Google Scholar] [CrossRef]
| Variable | Robotic-Assisted Proctectomy with IPAA (n = 29) | Laparoscopic Proctectomy with IPAA (n = 38) | p Value |
|---|---|---|---|
| Age, Mean ± SD, years | 39 ± 15 | 37 ± 12 | 0.704 |
| ASA classification, No. (%) | 0.454 | ||
| 1, Normal healthy patient | 3 (10.3) | 5 (13.2) | |
| 2, Patient with mild systemic disease | 21 (72.4) | 30 (78.9) | |
| 3, Patient with severe systemic disease | 5 (17.2) | 3 (7.9) | |
| Sex, No. (%) | 0.624 | ||
| Female | 16 (55.2) | 18 (47.4) | |
| Male | 13 (44.8) | 20 (52.6) | |
| BMI a, Mean ± SD, kg/m2 | 24.0 ± 4.0 | 23.7 ± 4.6 | 0.699 |
| Previous abdominal surgeries, No. (%) | 0.028 * | ||
| 1 | 15 (51.7) | 30 (78.9) | |
| 2–3 | 14 (48.3) | 8 (21.1) | |
| Current smoking, No. (%) | 2 (6.9) | 0 (0.0) | 0.184 |
| Diabetes, No. (%) | 1 (3.4) | 1 (2.6) | 1.000 |
| Anemia, No. (%) | 0 (0.0) | 2 (5.3) | 0.502 |
| Preoperative steroid use, No. (%) | 1 (3.4) | 2 (5.3) | 1.000 |
| Preoperative immunomodulatory use, No. (%) | 0 (0.0) | 2 (5.3) | 0.502 |
| Complications | Robotic-Assisted Proctectomy with IPAA (n = 29) | Laparoscopic Proctectomy with IPAA (n = 38) | p Value |
|---|---|---|---|
| Surgical complications, No. (%) | |||
| Surgical site infection | 2 (6.9) | 2 (5.3) | 1.000 |
| Postoperative ileus | 2 (6.9) | 5 (13.2) | 0.459 |
| Anastomotic leakage | 3 (10.3) | 4 (10.5) | 1.000 |
| Hemorrhage | 1 (3.4) | 3 (7.9) | 0.628 |
| Medical complications, No. (%) | |||
| Urinary tract infection | 7 (24.1) | 1 (2.6) | 0.010 * |
| Pulmonary artery embolism | 1 (3.4) | 0 (0.0) | 0.433 |
| Pneumonia | 1 (3.4) | 0 (0.0) | 0.433 |
| Clavien-Dindo classification, No. (%) | 0.502 | ||
| Total complications, grade 1–5 | 15 (51.7) | 16 (42.1) | 0.468 |
| Severe complications only, grade 3b–5 | 5 (17.2) | 4 (10.5) | 0.485 |
| Return to operating room, No. (%) | 5 (17.2) | 3 (7.9) | 0.278 |
| Dependent Variable | Variable | OR | 95% CI | p Value | |
|---|---|---|---|---|---|
| Lower | Upper | ||||
| Urinary tract infection | Rob. vs. Lap. | 0.097 | 0.010 | 0.922 | 0.042 * |
| ASA 2–3 vs. ASA 1 | 7.896 | 1.203 | 51.817 | 0.031 * | |
| Parameter | Robotic-Assisted Proctectomy with IPAA (n = 29) | Laparoscopic Proctectomy with IPAA (n = 38) | p Value |
|---|---|---|---|
| Operative time, Mean ± SD, min | 346 ± 65 | 281 ± 66 | <0.0001 * |
| Anastomotic technique, No (%) | 1.000 | ||
| Stapled ileal pouch-anal anastomosis | 27 (93.1) | 36 (94.7) | |
| Hand-sewn ileal pouch-anal anastomosis | 2 (6.9) | 2 (5.3) | |
| Conversion to open surgery, No. (%) | 0.379 | ||
| Yes | 1 (3.4) | 4 (10.5) | |
| No | 28 (96.6) | 34 (89.5) | |
| Intraoperative adverse event, No (%) | |||
| None | 25 (86.2) | 31 (81.6) | 0.745 |
| Damage to organ structures | 1 (3.4) | 2 (5.3) | 0.858 |
| Positive air leak test | 1 (3.4) | 4 (10.5) | 0.379 |
| Serosal tear | 3 (10.3) | 3 (7.9) | 1.000 |
| Length of stay (days), Median (IQR) | 9.0 (4.0) | 8.5 (7.0) | 0.877 |
| Dependent Variable | Variable | Regression Coefficient | 95% CI | Standardized Coefficient | p Value | |
|---|---|---|---|---|---|---|
| Lower | Upper | |||||
| Operative time | Rob. vs. Lap. | −55.953 | −83.018 | −28.888 | −0.384 | <0.0001 * |
| Anastomotic technique | −68.393 | −125.114 | −11.673 | −0.224 | 0.019 * | |
| BMI | 6.491 | 3.367 | 9.616 | 0.385 | <0.0001 * | |
| Category | Robotic-Assisted Proctectomy with IPAA (n = 29) | Laparoscopic Proctectomy with IPAA (n = 38) | p Value |
|---|---|---|---|
| Total inpatient costs | 0.118 | ||
| Median | 15.051 EUR (16.275 USD) | 13.243 EUR (14.320 USD) | |
| IQR | 5.821 EUR (6.294 USD) | 7.122 EUR (7.701 USD) | |
| Q25 | 13.547 EUR (14.649 USD) | 10.907 EUR (11.794 USD) | |
| Q75 | 19.368 EUR (20.943 USD) | 18.030 EUR (19.496 USD) | |
| Total inpatient revenues | 0.256 | ||
| Median | 15.524 EUR (16.766 USD) | 15.524 EUR (16.766 USD) | |
| IQR | 1.544 EUR (1.668 USD) | 2.129 EUR (2.299 USD) | |
| Q25 | 14.402 EUR (15.554 USD) | 14.810 EUR (15.995 USD) | |
| Q75 | 15.946 EUR (17.222 USD) | 16.939 EUR (18.294 USD) | |
| Total inpatient profits | 0.001 * | ||
| Median | 110 EUR (119 USD) | 2.853 EUR (3.081 USD) | |
| IQR | 4.971 EUR (5.369 USD) | 5.386 EUR (5.817 USD) | |
| Q25 | −3.691 EUR (−3.986 USD) | 526 EUR (568 USD) | |
| Q75 | 1.280 EUR (1.382 USD) | 5.911 EUR (6.384 USD) | |
| Surgery costs | <0.0001 * | ||
| Median | 10.377 EUR (11.221 USD) | 6.689 EUR (7.233 USD) | |
| IQR | 4.727 EUR (5.111 USD) | 3.170 EUR (3.427 USD) | |
| Q25 | 9.121 EUR (9.862 USD) | 5.281 EUR (5.710 USD) | |
| Q75 | 13.849 EUR (14.975 USD) | 8.452 EUR (9.139 USD) | |
| Surgery revenues | 0.604 | ||
| Median | 6.970 EUR (7.528 USD) | 6.671 EUR (7.205 USD) | |
| IQR | 1.065 EUR (1.150 USD) | 511 EUR (552 USD) | |
| Q25 | 6.276 EUR (6.778 USD) | 6.459 EUR (6.976 USD) | |
| Q75 | 7.341 EUR (7.928 USD) | 6.970 EUR (7.528 USD) | |
| Surgery profits | <0.0001 * | ||
| Median | −4.134 EUR (−4.465 USD) | −78 EUR (−84 USD) | |
| IQR | 4.097 EUR (4.425 USD) | 2.666 EUR (2.879 USD) | |
| Q25 | −6.786 EUR (−7.329 USD) | −1.482 EUR (−1.601 USD) | |
| Q75 | −2.689 EUR (−2.904 USD) | 1.183 EUR (1.278 USD) | |
| Surgical ward costs | 0.430 | ||
| Median | 4.202 EUR (4.543 USD) | 3.585 EUR (3.876 USD) | |
| IQR | 1.966 EUR (2.125 USD) | 3.598 EUR (3.890 USD) | |
| Q25 | 3.603 EUR (3.896 USD) | 2.858 EUR (3.090 USD) | |
| Q75 | 5.570 EUR (6.023 USD) | 6.456 EUR (6.981 USD) | |
| Surgical ward revenues | 0.305 | ||
| Median | 7.085 EUR (7.652 USD) | 7.085 EUR (7.652 USD) | |
| IQR | 1.126 EUR (1.216 USD) | 770 EUR (832 USD) | |
| Q25 | 6.116 EUR (6.605 USD) | 6.469 EUR (6.987 USD) | |
| Q75 | 7.242 EUR (7.821 USD) | 7.239 EUR (7.818 USD) | |
| Surgical ward profits | 0.957 | ||
| Median | 2.467 EUR (2.664 USD) | 2.506 EUR (2.706 USD) | |
| IQR | 1.945 EUR (2.101 USD) | 2.718 EUR (2.935 USD) | |
| Q25 | 1.400 EUR (1.512 USD) | 782 EUR (845 USD) | |
| Q75 | 3.345 EUR (3.613 USD) | 3.500 EUR (3.780 USD) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gebhardt, J.M.; Werner, N.; Stroux, A.; Förster, F.; Pozios, I.; Seifarth, C.; Schineis, C.; Kamphues, C.; Weixler, B.; Beyer, K.; et al. Robotic-Assisted versus Laparoscopic Proctectomy with Ileal Pouch-Anal Anastomosis for Ulcerative Colitis: An Analysis of Clinical and Financial Outcomes from a Tertiary Referral Center. J. Clin. Med. 2022, 11, 6561. https://doi.org/10.3390/jcm11216561
Gebhardt JM, Werner N, Stroux A, Förster F, Pozios I, Seifarth C, Schineis C, Kamphues C, Weixler B, Beyer K, et al. Robotic-Assisted versus Laparoscopic Proctectomy with Ileal Pouch-Anal Anastomosis for Ulcerative Colitis: An Analysis of Clinical and Financial Outcomes from a Tertiary Referral Center. Journal of Clinical Medicine. 2022; 11(21):6561. https://doi.org/10.3390/jcm11216561
Chicago/Turabian StyleGebhardt, Jasper Max, Neno Werner, Andrea Stroux, Frank Förster, Ioannis Pozios, Claudia Seifarth, Christian Schineis, Carsten Kamphues, Benjamin Weixler, Katharina Beyer, and et al. 2022. "Robotic-Assisted versus Laparoscopic Proctectomy with Ileal Pouch-Anal Anastomosis for Ulcerative Colitis: An Analysis of Clinical and Financial Outcomes from a Tertiary Referral Center" Journal of Clinical Medicine 11, no. 21: 6561. https://doi.org/10.3390/jcm11216561
APA StyleGebhardt, J. M., Werner, N., Stroux, A., Förster, F., Pozios, I., Seifarth, C., Schineis, C., Kamphues, C., Weixler, B., Beyer, K., & Lauscher, J. C. (2022). Robotic-Assisted versus Laparoscopic Proctectomy with Ileal Pouch-Anal Anastomosis for Ulcerative Colitis: An Analysis of Clinical and Financial Outcomes from a Tertiary Referral Center. Journal of Clinical Medicine, 11(21), 6561. https://doi.org/10.3390/jcm11216561






