Effects of Perioperative Oral Management in Patients with Cancer
Abstract
:1. Introduction
2. Materials and Methods
2.1. Patients
2.2. Variables
2.3. Statistical Analysis
3. Results
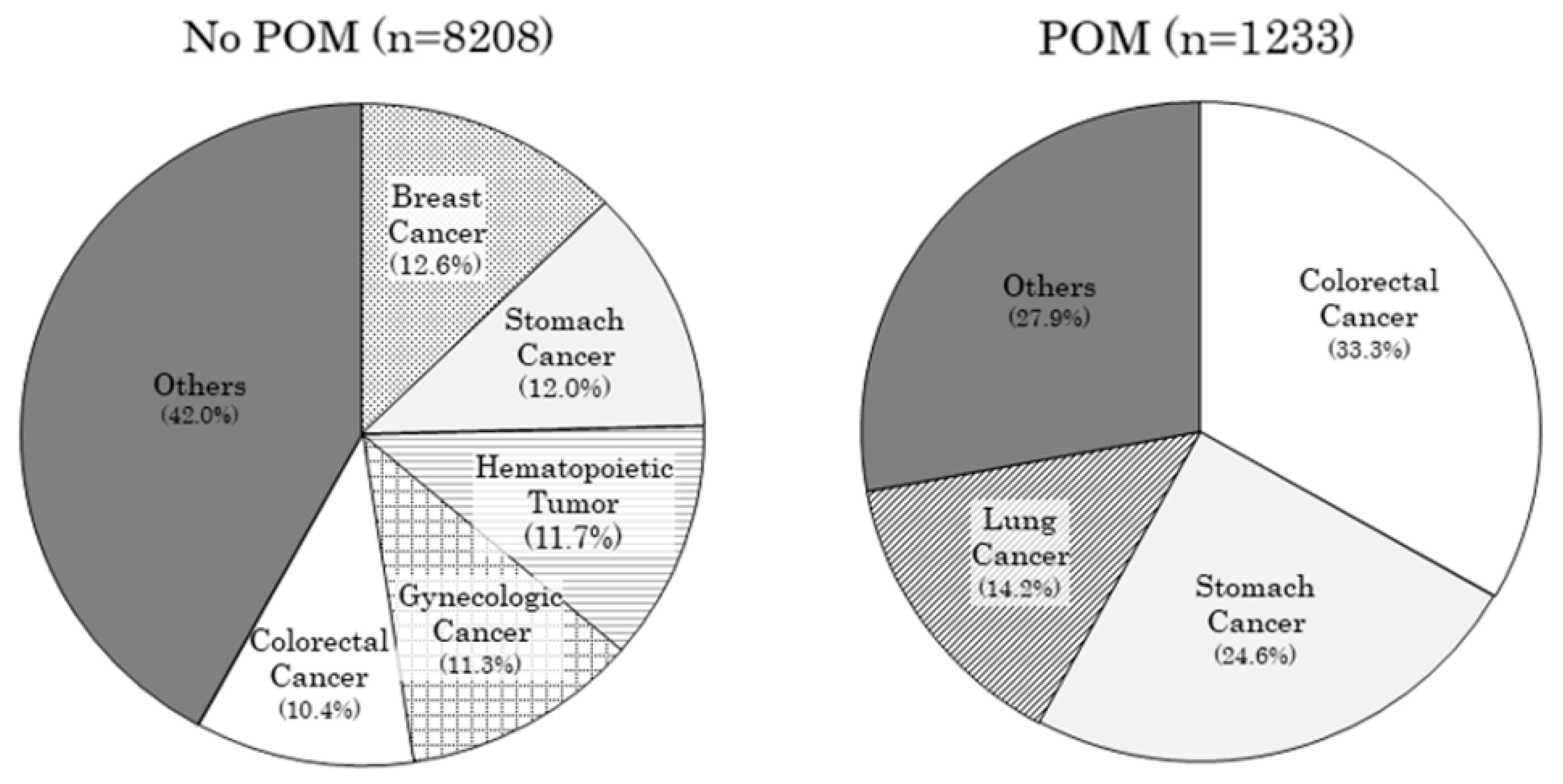
3.1. Overview of the Target
3.2. Incidence of Pneumonia by a Primary Lesion
3.3. Examination of the Effects of POM
3.4. Comparison of the Degree of Reduction in the Incidence of Pneumonia by Primary Lesion and the Proportion of Patients Who Underwent POM (PRP)
3.5. Factor Analysis of Pneumonia Occurring during Hospitalization
4. Discussion
4.1. Differences in the Incidence of Pneumonia According to the Primary Cancerous Lesion
4.2. Efficacy of POM in Preventing Pneumonia
4.3. Review of the Literature on Pneumonia Prevention Effect of POM
4.4. Effect of POM in Reducing Mortality
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Yoneyama, T.; Yoshida, M.; Matsui, T.; Sasaki, H. Oral care and pneumonia. Lancet 1999, 354, 515. [Google Scholar] [CrossRef]
- Yoshino, A.; Ebihara, T.; Ebihara, S.; Fuji, H.; Sasaki, H. Daily oral care and risk factors for pneumonia among elderly nursing home patients. JAMA 2001, 286, 2235–2236. [Google Scholar] [CrossRef] [PubMed]
- Maruoka, Y.; Michiwaki, Y.; Sekiya, H.; Kurasawa, Y.; Natsume, N. What does oral care mean to society? Biosci. Trends 2022, 16, 7–19. [Google Scholar] [CrossRef] [PubMed]
- Trinh, V.Q.; Ravi, P.; Abd-El-Barr, A.E.; Jhaveri, J.K.; Gervais, M.K.; Meyer, C.P.; Hanske, J.; Sammon, J.D.; Trinh, Q.D. Pneumonia after major cancer surgery: Temporal trends and patterns of care. Can. Respir. J. 2016, 2016, 6019416. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dimick, J.B.; Chen, S.L.; Taheri, P.A.; Henderson, W.G.; Khuri, S.F.; Campbell, D.A., Jr. Hospital costs associated with surgical complications: A report from the private-sector National Surgical Quality Improvement Program. J. Am. Coll. Surg. 2004, 199, 531–537. [Google Scholar] [CrossRef]
- Kazaure, H.S.; Martin, M.; Yoon, J.K.; Wren, S.M. Long-term results of a postoperative pneumonia prevention program for the inpatient surgical ward. JAMA Surg. 2014, 149, 914–918. [Google Scholar] [CrossRef] [Green Version]
- Teramoto, S.; Fukuchi, Y.; Sasaki, H.; Sato, K.; Sekizawa, K.; Matsuse, T. High incidence of aspiration pneumonia in community- and hospital-acquired pneumonia in hospitalized patients: A multicenter, prospective study in Japan. J. Am. Geriatr. Soc. 2008, 56, 577–579. [Google Scholar] [CrossRef]
- Labeau, S.O.; Van de Vyver, K.; Brusselaers, N.; Vogelaers, D.; Blot, S.I. Prevention of ventilator-associated pneumonia with oral antiseptics: A systematic review and meta-analysis. Lancet Infect. Dis. 2011, 11, 845–854. [Google Scholar] [CrossRef]
- Kurasawa, Y.; Maruoka, Y.; Sekiya, H.; Negishi, A.; Mukohyama, H.; Shigematsu, S.; Sugizaki, J.; Karakida, K.; Ohashi, M.; Ueno, M.; et al. Pneumonia prevention effects of perioperative oral management in approximately 25,000 patients following cancer surgery. Clin. Exp. Dent. Res. 2020, 6, 165–173. [Google Scholar] [CrossRef]
- Okamoto, K.; Uchiyama, T.; Takemura, T.; Kume, N.; Adachi, T.; Kuroda, T.; Uchiyama, T.; Yoshihara, H. Qualitative Evaluation of the Supporting System for Diagnosis Procedure Combination Code Selection. Stud. Health Technol. Inform. 2013, 192, 1031. [Google Scholar]
- Nakamura, K. Diagnosis Procedure Combination Database Would Develop Nationwide Clinical Research in Japan. Circ. J. 2016, 80, 2289–2290. [Google Scholar] [CrossRef] [PubMed]
- Fuji, T.; Akagi, M.; Abe, Y.; Oda, E.; Matsubayashi, D.; Ota, K.; Kobayashi, M.; Matsushita, Y.; Kaburagi, J.; Ibusuki, K.; et al. Incidence of Venous Thromboembolism and Bleeding Events in Patients with Lower Extremity Orthopedic Surgery: A Retrospective Analysis of a Japanese Healthcare Database. J. Orthop. Surg. 2017, 12, 55. [Google Scholar] [CrossRef] [Green Version]
- Okamoto, K.; Uchiyama, T.; Takemura, T.; Kume, N.; Kuroda, T.; Yoshihara, H. Automatic election of Diagnosis Procedure Combination Codes Based on Partial Treatment Data Relative to the Number of Hospitalization Days. Eur. J. Biomed. Inform. 2018, 14, 45–51. [Google Scholar] [CrossRef]
- Nozoe, T.; Kimura, Y.; Ishida, M.; Saeki, H.; Korenaga, D.; Sugimachi, K. Correlation of preoperative nutritional condition with post-operative complications in surgical treatment for oesophageal carcinoma. Eur. J. Surg. Oncol. 2002, 28, 396–400. [Google Scholar] [CrossRef] [PubMed]
- Oze, I.; Charvat, H.; Matsuo, K.; Ito, H.; Tamakoshi, A.; Nagata, C.; Wada, K.; Sugawara, Y.; Sawada, N.; Yamaji, T.; et al. Revisit of an unanswered question by pooled analysis of eight cohort studies in Japan: Does cigarette smoking and alcohol drinking have interaction for the risk of esophageal cancer? Cancer Med. 2019, 8, 6414–6425. [Google Scholar] [CrossRef] [Green Version]
- Wakai, K.; Inoue, M.; Mizoue, T.; Tanaka, K.; Tsuji, I.; Nagata, C.; Tsugane, S.; Research Group for the, D.; Evaluation of Cancer Prevention Strategies in, J. Tobacco smoking and lung cancer risk: An evaluation based on a systematic review of epidemiological evidence among the Japanese population. Jpn. J. Clin. Oncol. 2006, 36, 309–324. [Google Scholar] [CrossRef] [Green Version]
- Soutome, S.; Yanamoto, S.; Funahara, M.; Hasegawa, T.; Komori, T.; Yamada, S.I.; Kurita, H.; Yamauchi, C.; Shibuya, Y.; Kojima, Y.; et al. Effect of perioperative oral care on prevention of postoperative pneumonia associated with esophageal cancer surgery: A multicenter case-control study with propensity score matching analysis. Medicine 2017, 96, e7436. [Google Scholar] [CrossRef] [Green Version]
- Soutome, S.; Yanamoto, S.; Funahara, M.; Hasegawa, T.; Komori, T.; Oho, T.; Umeda, M. Preventive Effect on Post-Operative Pneumonia of Oral Health Care among Patients Who Undergo Esophageal Resection: A Multi-Center Retrospective Study. Surg. Infect. 2016, 17, 479–484. [Google Scholar] [CrossRef]
- Ishikawa, S.; Yamamori, I.; Takamori, S.; Kitabatake, K.; Edamatsu, K.; Sugano, A.; Oizumi, H.; Kato, H.; Suzuki, J.; Sato, K.; et al. Evaluation of effects of perioperative oral care intervention on hospitalization stay and postoperative infection in patients undergoing lung cancer intervention. Support Care Cancer 2021, 29, 135–143. [Google Scholar] [CrossRef]
- Ishimaru, M.; Matsui, H.; Ono, S.; Hagiwara, Y.; Morita, K.; Yasunaga, H. Preoperative oral care and effect on postoperative complications after major cancer surgery. Br. J. Surg. 2018, 105, 1688–1696. [Google Scholar] [CrossRef]
- Sekiya, H.; Kurasawa, Y.; Kaneko, K.; Takahashi, K.I.; Maruoka, Y.; Michiwaki, Y.; Takeda, Y.; Ochiai, R. Preventive effects of sustainable and developmental perioperative oral management using the "oral triage" system on postoperative pneumonia after cancer surgery. Int. J. Environ. Res. Public Health 2021, 18, 6296. [Google Scholar] [CrossRef] [PubMed]
- Miki, Y.; Makuuchi, R.; Tokunaga, M.; Tanizawa, Y.; Bando, E.; Kawamura, T.; Terashima, M. Risk factors for postoperative pneumonia after gastrectomy for gastric cancer. Surg. Today 2016, 46, 552–556. [Google Scholar] [CrossRef] [PubMed]
- Kiuchi, J.; Komatsu, S.; Ichikawa, D.; Kosuga, T.; Okamoto, K.; Konishi, H.; Shiozaki, A.; Fujiwara, H.; Yasuda, T.; Otsuji, E. Putative risk factors for postoperative pneumonia which affects poor prognosis in patients with gastric cancer. Int. J. Clin. Oncol. 2016, 21, 920–926. [Google Scholar]
- Allen, M.S.; Darling, G.E.; Pechet, T.T.; Mitchell, J.D.; Herndon, J.E., 2nd; Landreneau, R.J.; Inculet, R.I.; Jones, D.R.; Meyers, B.F.; Harpole, D.H.; et al. Morbidity and mortality of major pulmonary resections in patients with early-stage lung cancer: Initial results of the randomized, prospective ACOSOG Z0030 trial. Ann. Thorac. Surg. 2006, 81, 1013–1019. [Google Scholar] [CrossRef]
- Shiono, S.; Yoshida, J.; Nishimura, M.; Hagiwara, M.; Hishida, T.; Nitadori, J.; Nagai, K. Risk factors of postoperative respiratory infections in lung cancer surgery. J. Thorac. Oncol. 2007, 2, 34–38. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kochi, M.; Hinoi, T.; Niitsu, H.; Ohdan, H.; Konishi, F.; Kinugasa, Y.; Kobatake, T.; Ito, M.; Inomata, M.; Yatsuoka, T.; et al. Risk factors for postoperative pneumonia in elderly patients with colorectal cancer: A sub-analysis of a large, multicenter, case-control study in Japan. Surg. Today 2018, 48, 756–764. [Google Scholar] [CrossRef] [PubMed]
- Sjogren, P.; Wardh, I.; Zimmerman, M.; Almstahl, A.; Wikstrom, M. Oral care and mortality in older adults with pneumonia in hospitals or nursing homes: Systematic review and meta-Analysis. J. Am. Geriatr. Soc. 2016, 64, 2109–2115. [Google Scholar] [CrossRef]
- Nobuhara, H.; Yanamoto, S.; Funahara, M.; Matsugu, Y.; Hayashida, S.; Soutome, S.; Kawakita, A.; Ikeda, S.; Itamoto, T.; Umeda, M. Effect of perioperative oral management on the prevention of surgical site infection after colorectal cancer surgery: A multicenter retrospective analysis of 698 patients via analysis of covariance using propensity score. Medicine 2018, 97, e12545. [Google Scholar] [CrossRef]


| No POM | POM | ||||
|---|---|---|---|---|---|
| (n = 8208) | (n = 1233) | p-Value | |||
| Age (year), mean ± SD | 65.0 | 14.2 | 66.9 | 11.5 | <0.001 |
| Sex (male), n (%) | 4153 | 50.6 | 728 | 59.0 | <0.001 |
| Incidence of Pneumonia (%) | Mortality (%) | |||||||
|---|---|---|---|---|---|---|---|---|
| Primary Lesion | No POM | POM | Difference No POM and POM | p-Value | No POM | POM | Difference No POM and POM | p-Value |
| Esophageal cancer | 5.2 | 5.0 | −0.2 | NS | 4.1 | 0 | −4.1 | NS |
| Hematopoietic tumor | 4.8 | 4.8 | 0 | NS | 15.1 | 21.4 | 6.3 | NS |
| Musculoskeletal cancer | 4.1 | 0 | −4.1 | NS | 12.2 | 0 | −12.2 | NS |
| Lung cancer | 3.7 | 1.1 | −2.6 | NS | 4.3 | 0.6 | −3.7 | 0.018 |
| Head and neck cancer | 3.7 | 2.7 | −1.0 | NS | 1.3 | 1.4 | 0.1 | NS |
| Unknown primary | 3.2 | 100 | 96.8 | NS | 12.9 | 0 | −12.9 | NS |
| Brain tumor | 2.0 | 0 | −2.0 | NS | 4.6 | 0 | −4.6 | NS |
| Colorectal cancer | 1.4 | 1.5 | 0.1 | NS | 2.0 | 2.0 | 0.0 | NS |
| Stomach cancer | 1.3 | 1.0 | −0.3 | NS | 3.9 | 2.6 | −1.3 | NS |
| Liver and gallbladder cancer | 0.7 | 1.6 | 0.9 | NS | 5.1 | 1.6 | −3.5 | NS |
| Thyroid gland cancer | 0.6 | 0 | −0.6 | NS | 1.3 | 0 | −1.3 | NS |
| Pancreas cancer | 0.4 | 0 | −0.4 | NS | 8.7 | 0 | −8.7 | 0.019 |
| Breast cancer | 0 | 0 | 0 | 1.0 | 0 | −1.0 | ||
| Gynecologic cancer | 0 | 0 | 0 | 2.4 | 0 | −2.4 | ||
| Prostate cancer | 0 | 0 | 0 | 1.9 | 0 | −1.9 | ||
| Kidney cancer | 0 | 0 | 0 | 3.2 | 0 | −3.2 | ||
| Small intestine cancer | 0 | 0 | 0 | 5.1 | 0 | −5.1 | ||
| Mediastinal cancer | 0 | 0 | 0 | 0 | 0 | 0 | ||
| Skin cancer | 0 | 0 | 0 | 0 | ||||
| Malignant eye tumor | 0 | 0 | ||||||
| Male genital cancer | 0 | 10.0 | ||||||
| Malignant cardiac tumor | 0 | 25.0 | ||||||
| Primary Lesion | No POM (n) | POM (n) | PRP (%) |
|---|---|---|---|
| Colorectal cancer | 857 | 410 | 32.4 |
| Stomach cancer | 982 | 303 | 23.6 |
| Head and neck cancer | 299 | 73 | 19.6 |
| Lung cancer | 749 | 175 | 18.9 |
| Pancreas cancer | 253 | 48 | 15.9 |
| Thyroid gland cancer | 160 | 25 | 13.5 |
| Kidney cancer | 279 | 32 | 11.5 |
| Esophageal cancer | 194 | 20 | 9.3 |
| Liver and gallbladder cancer | 693 | 62 | 8.2 |
| Hematopoietic tumor | 958 | 42 | 4.2 |
| Breast cancer | 1033 | 14 | 1.3 |
| Small intestine cancer | 59 | 7 | 10.6 |
| Mediastinal cancer | 54 | 6 | 10.0 |
| Prostate cancer | 376 | 6 | 1.6 |
| Musculoskeletal cancer | 74 | 1 | 1.4 |
| Brain tumor | 153 | 2 | 1.3 |
| Gynecologic cancer | 930 | 6 | 0.6 |
| Malignant eye tumor | 20 | 0 | 0 |
| Male genital cancer | 10 | 0 | 0 |
| Malignant cardiac tumor | 4 | 0 | 0 |
| Skin cancer | 40 | 0 | 0 |
| Other | 31 | 1 | 3.1 |
| n | Odds Ratio | 95% CI | p-Value | ||
|---|---|---|---|---|---|
| Female | 4560 | standard | |||
| Male | 4881 | 2.52 | 1.67 | 3.80 | p < 0.001 |
| Age <50 years | 1328 | standard | |||
| 50–59 | 1321 | 1.83 | 0.57 | 5.89 | NS |
| 60–69 | 2694 | 3.53 | 1.25 | 9.94 | 0.017 |
| 70–79 | 2853 | 3.65 | 1.30 | 10.22 | 0.014 |
| 80 or older | 1245 | 5.69 | 1.99 | 16.26 | 0.001 |
| No POM | 8208 | standard | |||
| POM | 1233 | 0.87 | 0.52 | 1.47 | NS |
| Others | 4149 | standard | |||
| Brain tumor | 155 | 9.33 | 2.52 | 34.55 | p < 0.001 |
| Colorectal cancer | 1267 | 4.43 | 2.01 | 9.74 | p < 0.001 |
| Esophageal cancer | 214 | 13.11 | 5.44 | 31.62 | p < 0.001 |
| Hematopoietic tumor | 1000 | 15.80 | 7.94 | 31.44 | p < 0.001 |
| Head and neck cancer | 372 | 9.76 | 4.19 | 22.69 | p < 0.001 |
| Lung cancer | 924 | 10.32 | 4.99 | 21.33 | p < 0.001 |
| Musculoskeletal cancer | 75 | 14.82 | 3.96 | 55.48 | p < 0.001 |
| Stomach cancer | 1285 | 3.34 | 1.50 | 7.46 | 0.003 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kurasawa, Y.; Iida, A.; Narimatsu, K.; Sekiya, H.; Maruoka, Y.; Michiwaki, Y. Effects of Perioperative Oral Management in Patients with Cancer. J. Clin. Med. 2022, 11, 6576. https://doi.org/10.3390/jcm11216576
Kurasawa Y, Iida A, Narimatsu K, Sekiya H, Maruoka Y, Michiwaki Y. Effects of Perioperative Oral Management in Patients with Cancer. Journal of Clinical Medicine. 2022; 11(21):6576. https://doi.org/10.3390/jcm11216576
Chicago/Turabian StyleKurasawa, Yasuhiro, Akihiko Iida, Kaya Narimatsu, Hideki Sekiya, Yutaka Maruoka, and Yukihiro Michiwaki. 2022. "Effects of Perioperative Oral Management in Patients with Cancer" Journal of Clinical Medicine 11, no. 21: 6576. https://doi.org/10.3390/jcm11216576
APA StyleKurasawa, Y., Iida, A., Narimatsu, K., Sekiya, H., Maruoka, Y., & Michiwaki, Y. (2022). Effects of Perioperative Oral Management in Patients with Cancer. Journal of Clinical Medicine, 11(21), 6576. https://doi.org/10.3390/jcm11216576






