Differential Expression of miRNA-223 in Coronary In-Stent Restenosis
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Subjects
2.2. Serum Preparation
2.3. Biochemical Measurements
2.4. Serum RNA Extraction
2.5. Primer Design
2.6. cDNA Synthesis and qRT-PCR
2.7. Statistical Analysis
3. Results
3.1. Baseline Characteristics of Patients
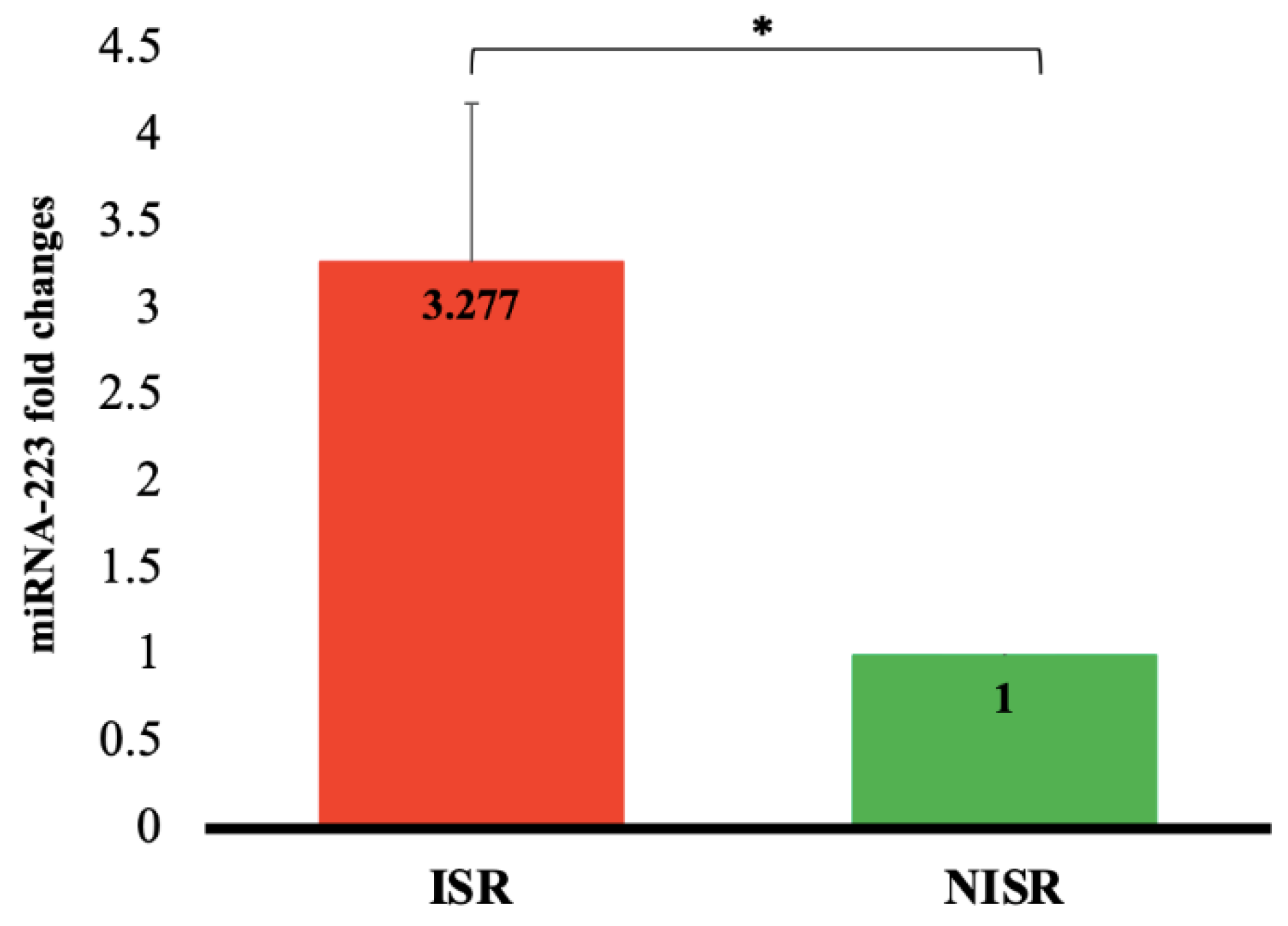
3.2. Comparison of Serum miRNA-223 Expression between Studied Groups
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- WHO. The Top 10 Causes of Death 2020. Available online: https://www.who.int/news-room/fact-sheets/detail/the-top-10-causes-of-death (accessed on 29 January 2022).
- Bonow, R.O.; Mann, D.L.; Zipes, D.P.; Libby, P. Braunwald’s Heart Disease e-Book: A Textbook of Cardiovascular Medicine; Elsevier Health Sciences: Amsterdam, The Netherlands, 2011. [Google Scholar]
- Bavry, A.A.; Kumbhani, D.J. Indications and Techniques of Percutaneous Procedures: Coronary, Peripheral and Structural Heart Disease; Springer Science & Business Media: Heidelberg, Germany, 2012. [Google Scholar]
- Grech, E.D. Percutaneous coronary intervention. I: History and development. (ABC of interventional cardiology). Br. Med. J. 2003, 326, 1080–1083. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Taggart, D.P. Coronary-artery stents. N. Engl. J. Med. 2006, 354, 2076–2078. [Google Scholar] [PubMed]
- Cassese, S.; Xu, B.; Habara, S.; Rittger, H.; Byrne, R.A.; Waliszewski, M.; Pérez-Vizcayno, M.J.; Gao, R.; Kastrati, A.; Alfonso, F. Incidence and predictors of reCurrent restenosis after drug-coated balloon Angioplasty for Restenosis of a drUg-eluting Stent: The ICARUS Cooperation. Rev. Española Cardiol. 2018, 71, 620–627. [Google Scholar] [CrossRef]
- Juni, R.P.; Duckers, H.J.; Vanhoutte, P.M.; Virmani, R.; Moens, A.L. Oxidative Stress and Pathological Changes After Coronary Artery Interventions. J. Am. Coll. Cardiol. 2013, 61, 1471–1481. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Azevedo, L.C.; Pedro, M.A.; Souza, L.C.; de Souza, H.P.; Janiszewski, M.; da Luz, P.L.; Laurindo, F.R. Oxidative stress as a signaling mechanism of the vascular response to injury: The redox hypothesis of restenosis. Cardiovasc. Res. 2000, 47, 436–445. [Google Scholar] [CrossRef] [Green Version]
- Lee, M.S.; David, E.M.; Makkar, R.R.; Wilentz, J.R. Molecular and cellular basis of restenosis after percutaneous coronary intervention: The intertwining roles of platelets, leukocytes, and the coagulation–fibrinolysis system. J. Pathol. 2004, 203, 861–870. [Google Scholar] [CrossRef]
- Moses, J.W.; Leon, M.B.; Popma, J.J.; Fitzgerald, P.J.; Holmes, D.R.; O’Shaughnessy, C.; Caputo, R.P.; Kereiakes, D.J.; Williams, D.O.; Teirstein, P.S.; et al. Sirolimus-Eluting Stents versus Standard Stents in Patients with Stenosis in a Native Coronary Artery. N. Engl. J. Med. 2003, 349, 1315–1323. [Google Scholar] [CrossRef] [Green Version]
- Stone, G.W.; Ellis, S.G.; Cox, D.A.; Hermiller, J.; O’Shaughnessy, C.; Mann, J.T.; Turco, M.; Caputo, R.; Bergin, P.; Greenberg, J.; et al. A Polymer-Based, Paclitaxel-Eluting Stent in Patients with Coronary Artery Disease. N. Engl. J. Med. 2004, 350, 221–231. [Google Scholar] [CrossRef]
- Ghafari, S.; Hasanian, M.R.; Pourafkari, L. One-year outcome of stenting for long coronary lesions, a prospective clinical trial. J. Cardiovasc. Thorac. Res. 2011, 2, 7–12. [Google Scholar]
- Räber, L.; Wohlwend, L.; Wigger, M.; Togni, M.; Wandel, S.; Wenaweser, P.; Cook, S.; Moschovitis, A.; Vogel, R.; Kalesan, B.; et al. Five-year clinical and angiographic outcomes of a randomized comparison of sirolimus-eluting and paclitaxel-eluting stents: Results of the Sirolimus-Eluting Versus Paclitaxel-Eluting Stents for Coronary Revascularization, L.A.TE trial. Circulation 2011, 123, 2819–2828. [Google Scholar] [CrossRef] [Green Version]
- Zampetaki, A.; Willeit, P.; Tilling, L.; Drozdov, I.; Prokopi, M.; Renard, J.-M.; Mayr, A.; Weger, S.; Schett, G.; Shah, A.; et al. Prospective Study on Circulating MicroRNAs and Risk of Myocardial Infarction. J. Am. Coll. Cardiol. 2012, 60, 290–299. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Devaux, Y.; Mueller, M.; Haaf, P.; Goretti, E.; Twerenbold, R.; Zangrando, J.; Vausort, M.; Reichlin, T.; Wildi, K.; Moehring, B.; et al. Diagnostic and prognostic value of circulating microRNAs in patients with acute chest pain. J. Intern. Med. 2013, 277, 260–271. [Google Scholar] [CrossRef] [Green Version]
- Devaux, Y.; Vausort, M.; McCann, G.P.; Kelly, D.; Collignon, O.; Ng, L.L.; Wagner, D.R.; Squire, I.B. A panel of 4 microRNAs facilitates the prediction of left ventricular contractility after acute myocardial infarction. PLoS ONE 2013, 8, e70644. [Google Scholar] [CrossRef]
- Creemers, E.E.; Tijsen, A.J.; Pinto, Y.M. Circulating microRNAs: Novel biomarkers and extracellular communicators in cardiovascular disease? Circ. Res. 2012, 110, 483–495. [Google Scholar] [CrossRef] [PubMed]
- Nik Mohamed Kamal, N.N.S.B.; Shahidan, W.N.S. Non-exosomal and exosomal circulatory microRNAs: Which are more valid as biomarkers? Front. Pharmacol. 2020, 10, 1500. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Smani, T.; Mayoral-Gonzalez, I.; Galeano-Otero, I.; Gallardo-Castillo, I.; Rosado, J.A.; Ordoñez, A.; Hmadcha, A. Non-coding RNAs and ischemic cardiovascular diseases. Adv. Exp. Med. Biol. 2020, 1229, 259–271. [Google Scholar] [PubMed]
- He, M.; Gong, Y.; Shi, J.; Pan, Z.; Zou, H.; Sun, D.; Tu, X.; Tan, X.; Li, J.; Li, W.; et al. Plasma MicroRNAs as Potential Noninvasive Biomarkers for In-Stent Restenosis. PLoS ONE 2014, 9, e112043. [Google Scholar] [CrossRef]
- Cheng, Y.; Liu, X.; Yang, J.; Lin, Y.; Xu, D.-Z.; Lu, Q.; Deitch, E.A.; Huo, Y.; Delphin, E.S.; Zhang, C. MicroRNA-145, a novel smooth muscle cell phenotypic marker and modulator, controls vascular neointimal lesion formation. Circ. Res. 2009, 105, 158–166. [Google Scholar] [CrossRef]
- Romaine, S.P.R.; Tomaszewski, M.; Condorelli, G.; Samani, N.J. MicroRNAs in cardiovascular disease: An introduction for clinicians. Heart 2015, 101, 921–928. [Google Scholar] [CrossRef]
- Yang, H.; Zhang, H.; Ge, S.; Ning, T.; Bai, M.; Li, J.; Li, S.; Sun, W.; Deng, T.; Zhang, L.; et al. Exosome-Derived miR-130a Activates Angiogenesis in Gastric Cancer by Targeting C-MYB in Vascular Endothelial Cells. Mol. Ther. 2018, 26, 2466–2475. [Google Scholar] [CrossRef] [Green Version]
- Lun, W.; Wu, X.; Deng, Q.; Zhi, F. MiR-218 regulates epithelial–mesenchymal transition and angiogenesis in colorectal cancer via targeting CTGF. Cancer Cell Int. 2018, 18, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Dai, R.; Liu, Y.; Zhou, Y.; Xiong, X.; Zhou, W.; Li, W.; Zhou, W.; Chen, M. Potential of circulating pro-angiogenic microRNA expressions as biomarkers for rapid angiographic stenotic progression and restenosis risks in coronary artery disease patients underwent percutaneous coronary intervention. J. Clin. Lab. Anal. 2019, 34, e23013. [Google Scholar] [CrossRef]
- Chen, L.-J.; Lim, S.H.; Yeh, Y.-T.; Lien, S.-C.; Chiu, J.-J. Roles of microRNAs in atherosclerosis and restenosis. J. Biomed. Sci. 2012, 19, 79. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mirzaei, S.; Zarrabi, A.; Hashemi, F.; Zabolian, A.; Saleki, H.; Ranjbar, A.; Saleh, S.H.S.; Bagherian, M.; Sharifzadeh, S.O.; Hushmandi, K.; et al. Regulation of Nuclear Factor-KappaB (NF-κB) signaling pathway by non-coding, RNAs in cancer: Inhibiting or promoting carcinogenesis? Cancer Lett. 2021, 509, 63–80. [Google Scholar] [CrossRef] [PubMed]
- Van der Heiden, K.; Cuhlmann, S.; Luong, L.A.; Zakkar, M.; Evans, P.C. Role of nuclear factor kappa B in cardiovascular health and disease. Clin. Sci. 2010, 118, 593–605. [Google Scholar] [CrossRef]
- Qin, S.; Zhang, C. MicroRNAs in vascular disease. J. Cardiovasc. Pharmacol. 2011, 57, 8. [Google Scholar] [CrossRef] [Green Version]
- Ren, J.; Zhang, J.; Xu, N.; Han, G.; Geng, Q.; Song, J.; Li, S.; Zhao, J.; Chen, H. Signature of Circulating MicroRNAs as Potential Biomarkers in Vulnerable Coronary Artery Disease. PLoS ONE 2013, 8, e80738. [Google Scholar] [CrossRef] [Green Version]
- Baldán, Á.; de Aguiar Vallim, T.Q. miRNAs and high-density lipoprotein metabolism. Biochim. Biophys. Acta Mol. Cell Biol. Lipids 2016, 1861, 2053–2061. [Google Scholar] [CrossRef] [Green Version]
- Fichtlscherer, S.; De Rosa, S.; Fox, H.; Schwietz, T.; Fischer, A.; Liebetrau, C.; Weber, M.; Hamm, C.W.; Röxe, T.; Müller-Ardogan, M.; et al. Circulating MicroRNAs in Patients with Coronary Artery Disease. Circ. Res. 2010, 107, 677–684. [Google Scholar] [CrossRef] [Green Version]
- Dávalos, A.; Fernández-Hernando, C. From evolution to revolution: miRNAs as pharmacological targets for modulating cholesterol efflux and reverse cholesterol transport. Pharmacol. Res. 2013, 75, 60–72. [Google Scholar] [CrossRef] [Green Version]
- Horie, T.; Baba, O.; Kuwabara, Y.; Chujo, Y.; Watanabe, S.; Kinoshita, M.; Horiguchi, M.; Nakamura, T.; Chonabayashi, K.; Hishizawa, M.; et al. MicroRNA-33 deficiency reduces the progression of atherosclerotic plaque in ApoE-/- mice. J. Am. Heart Assoc. 2012, 1, e003376. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mandolini, C.; Santovito, D.; Marcantonio, P.; Buttitta, F.; Bucci, M.; Ucchino, S.; Mezzetti, A.; Cipollone, F. Identification of microRNAs 758 and 33b as potential modulators of, ABCA1 expression in human atherosclerotic plaques. Nutr. Metab. Cardiovasc. Dis. 2015, 25, 202–209. [Google Scholar] [CrossRef] [PubMed]
- Madrigal-Matute, J.; Rotllan, N.; Aranda, J.F.; Fernández-Hernando, C. MicroRNAs and Atherosclerosis. Curr. Atheroscler. Rep. 2013, 15, 322. [Google Scholar] [CrossRef] [PubMed]
- Linton, M.F.; Yancey, P.G.; Davies, S.S.; Jerome, W.G.; Linton, E.F.; Song, W.L.; Doran, A.C.; Vickers, K.C. The Role of Lipids and Lipoproteins in Atherosclerosis. In Endotext; NCBI: Bethesda, MA, USA, 2019. [Google Scholar]
- Rayner, K.; Moore, K.J. MicroRNA Control of High-Density Lipoprotein Metabolism and Function. Circ. Res. 2014, 114, 183–192. [Google Scholar] [CrossRef] [Green Version]
- Maheronnaghsh, M.; Niktab, I.; Enayati, S.; Amoli, M.; Hosseini, S.; Tavakkoly-Bazzaz, J. Differentially expressed miR-152, a potential biomarker for in-stent restenosis (ISR) in peripheral blood mononuclear cells (PBMCs) of coronary artery disease (CAD) patients. Nutr. Metab. Cardiovasc. Dis. 2020, 31, 1137–1147. [Google Scholar] [CrossRef]
- Yuan, Y.; Liu, X.; Hao, S.; He, Q.; Shen, Z. Plasma levels of miR-143 and miR-145 are associated with coronary in-stent restenosis within 1 year of follow-up after drug-eluting stent implantation. Ann. Transl. Med. 2020, 8, 756. [Google Scholar] [CrossRef]
- Farina, F.M.; Hall, I.F.; Serio, S.; Zani, S.; Climent, M.; Salvarani, N.; Carullo, P.; Civilini, E.; Condorelli, G.; Elia, L.; et al. miR-128-3p Is a Novel Regulator of Vascular Smooth Muscle Cell Phenotypic Switch and Vascular Diseases. Circ. Res. 2020, 126, e120–e135. [Google Scholar] [CrossRef]
- Zhang, Y.; Chen, X. miR-18a-5p Promotes Proliferation and Migration of Vascular Smooth Muscle Cells by Activating the AKT/Extracellular Regulated Protein Kinases (ERK) Signaling Pathway. Med Sci. Monit. 2020, 26, e924625. [Google Scholar] [CrossRef]
- Zhang, H.; Zhang, Q.; Liu, Y.; Xue, T. miR-146a and miR-146b predict increased restenosis and rapid angiographic stenotic progression risk in coronary heart disease patients who underwent percutaneous coronary intervention. Ir. J. Med. Sci. 2020, 189, 467–474. [Google Scholar] [CrossRef]
- Wang, M.; Zhang, W.; Zhang, L.; Wang, L.; Li, J.; Shu, C.; Li, X. Roles of MicroRNAs in Peripheral Artery In-Stent Restenosis after Endovascular Treatment. BioMed Res. Int. 2021, 2021, 9935671. [Google Scholar] [CrossRef]
- Pan, C.-H.; Chien, S.-C.; Chen, C.-J.; Shih, C.-M.; Hsieh, M.-H.; Huang, C.-Y.; Bi, W.-F.; Chan, C.-S.; Kao, Y.-T.; Hsiao, C.-Y.; et al. Circulating level of microRNA-142-5p is a potential biomarker for predicting in-stent restenosis: A case–control study. BMC Cardiovasc. Disord. 2021, 21, 7. [Google Scholar] [CrossRef] [PubMed]
- Gutierrez-Carretero, E.; Mayoral-González, I.; Morón, F.J.; Fernández-Quero, M.; Domínguez-Rodríguez, A.; Ordóñez, A.; Smani, T. miR-30b-5p Downregulation as a Predictive Biomarker of Coronary In-Stent Restenosis. Biomedicines 2021, 9, 354. [Google Scholar] [CrossRef] [PubMed]
- Vickers, K.C.; Palmisano, B.T.; Shoucri, B.M.; Shamburek, R.D.; Remaley, A.T. MicroRNAs are transported in plasma and delivered to recipient cells by high-density lipoproteins. Nat. Cell Biol. 2011, 13, 423–433. [Google Scholar] [CrossRef] [Green Version]
- M’Baya-Moutoula, E.; Marchand, A.; Six, I.; Bahrar, N.; Celic, T.; Mougenot, N.; Maitrias, P.; Massy, Z.A.; Lompreh, A.-M.; Metzinger, L.; et al. Inhibition of miR-223 Expression Using a Sponge Strategy Decreases Restenosis in Rat Injured Carotids. Curr. Vasc. Pharmacol. 2020, 18, 507–516. [Google Scholar] [CrossRef]
- Torres, L.F.C.; Zhu, W.; Öhrling, G.; Larsson, R.; Patel, M.; Wiese, C.B.; Larsson, R.; Patel, M.; Wiese, C.B.; Rye, K.-Y.; et al. High-density lipoproteins induce miR-223–3p biogenesis and export from myeloid cells: Role of scavenger receptor, BI-mediated lipid transfer. Atherosclerosis 2019, 286, 20–29. [Google Scholar] [CrossRef] [PubMed]
- Vickers, K.C.; Landstreet, S.R.; Levin, M.; Shoucri, B.M.; Toth, C.L.; Taylor, R.C.; Palmisano, B.T.; Tabet, F.; Cui, H.L.; Rye, K.-A.; et al. MicroRNA-223 coordinates cholesterol homeostasis. Proc. Natl. Acad. Sci. USA 2014, 111, 14518–14523. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rayner, K.J.; Suárez, Y.; Dávalos, A.; Parathath, S.; Fitzgerald, M.L.; Tamehiro, N.; Fisher, E.A.; Moore, K.J.; Fernández-Hernando, C. MiR-33 contributes to the regulation of cholesterol homeostasis. Science 2010, 328, 1570–1573. [Google Scholar] [CrossRef] [Green Version]
- Canfran-Duque, A.; Ramírez, C.M.; Goedeke, L.; Lin, C.-S.; Fernandez-Hernando, C. microRNAs and, H.D.L life cycle. Cardiovasc. Res. 2014, 103, 414–422. [Google Scholar] [CrossRef] [Green Version]
- Wang, L.; Jia, X.-J.; Jiang, H.-J.; Du, Y.; Yang, F.; Si, S.-Y.; Hong, B. MicroRNAs 185, 96, and 223 Repress Selective High-Density Lipoprotein Cholesterol Uptake through Posttranscriptional Inhibition. Mol. Cell. Biol. 2013, 33, 1956–1964. [Google Scholar] [CrossRef] [Green Version]
| miRNAs | Sequences | Product Length (bp) | Length (bp) | |
|---|---|---|---|---|
| miRNA-223 | RT stem loop | 5′-GTCGTATGCAGAGCAGGGTCCGAGGTATTCGCACTGCATACGACTGGGGT-3′ | 50 | 69 |
| Forward | 5′-CGCTGTCAGTTTGTCAAAT-3′ | 19 | ||
| Reverse | 5′-GAGCAGGGTCCGAGGT-3′ | 16 | ||
| Probe | 5′-FAM-CCCCAGTCGTATGCAGTGC-BHQ-1-3′ | 19 | ||
| U6 snRNA | RT stem loop | 5′-GTCGTATGCAGAGCAGGGTCCGAGGTATTCGCACTGCATACGACAAAATATGG-3′ | 53 | 82 |
| Forward | 5′-AAGGATGACACGCAAATTC-3′ | 19 | ||
| Reverse | 5′-GAGCAGGGTCCGAGGT-3′ | 16 | ||
| Probe | 5′-FAM-CGTTCCATATTTTGTCGTATGCAGT-BHQ-1-3′ | 25 |
| Variables | ISR (n = 21) | NISR (n = 26) | p-Value | |
|---|---|---|---|---|
| Sex % | Male | 52.4 | 50.0 | 0.871 |
| Female | 47.6 | 50.0 | ||
| Age (y) | 59.5 ± 2.6 | 60.4 ± 2.1 | 0.785 | |
| Height (cm) | 161.5 ± 2.6 | 162.8 ± 2.0 | 0.678 | |
| Weight (kg) | 69.9 ± 2.8 | 73.2 ± 3.5 | 0.492 | |
| BMI (kg/m2) | 27.0 ± 0.9 | 27.5 ± 1.0 | 0.757 | |
| Smoker % | 5.9 | 23.1 | 0.215 | |
| Dyslipidemia % | 71.4 | 46.2 | 0.081 | |
| DM % | 61.9 | 46.2 | 0.282 | |
| HTN % | 71.4 | 65.4 | 0.659 | |
| Drugs consumption % | Statin | 100.0 | 88.0 | 0.239 |
| Aspirin | 90.5 | 84.0 | 0.257 | |
| Clopidogrel | 68.4 | 92.0 | 0.095 | |
| Insulin | 19.0 | 19.2 | 0.987 | |
| Oral diabetic drugs | 38.1 | 19.2 | 0.151 | |
| SBP (mmHg) | 125.7 ± 3.6 | 121.8 ± 2.9 | 0.400 | |
| DBP (mmHg) | 78.1 ± 2.4 | 74.8 ± 1.6 | 0.241 | |
| Stent type % | Bare metal | 50.0 50.0 | 11.1 88.9 | 0.015 * |
| Drug-eluting | ||||
| Stent number % | 1 | 66.7 | 65.4 | 0.927 |
| >1 | 33.3 | 34.6 | ||
| Duration of stent implantation (month) | 32.8 ± 5.9 | 22.4 ± 5.4 | 0.200 | |
| EF (%) | 46.2 ± 2.9 | 45.2 ± 2.5 | 0.806 | |
| Variables | ISR (n = 21) | NISR (n = 26) | p-Value |
|---|---|---|---|
| FBS (mg/dL) | 155.6 ± 16.9 | 138.9 ± 15.7 | 0.473 |
| TC (mg/dL) | 145.6 ± 7.9 | 124.4 ± 8.7 | 0.084 |
| TG (mg/dL) | 144.8 ± 21.2 | 97.3 ± 11.8 | 0.059 |
| HDL-C (mg/dL) | 36.6 ± 1.6 | 34.1 ± 2.2 | 0.395 |
| LDL-C (mg/dL) | 81.7 ± 6.7 | 70.8 ± 6.4 | 0.252 |
| hs-CRP (mg/L) | 3.9 ± 0.8 | 4.6 ± 0.8 | 0.509 |
| Variables | Unadjusted | Adjusted | ||||
|---|---|---|---|---|---|---|
| Model I | Model II | |||||
| OR (95% CI) | p-Value | OR (95% CI) | p-Value | OR (95% CI) | p-Value | |
| miRNA-223 expression (FC) | 3.077 (0.846–11.187) | 0.088 | 1.885 (0.610–5.825) | 0.271 | 17.818 (1.115–284.623) | 0.042 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ganjali, S.; Aghaee-Bakhtiari, S.H.; Reiner, Ž.; Sahebkar, A. Differential Expression of miRNA-223 in Coronary In-Stent Restenosis. J. Clin. Med. 2022, 11, 849. https://doi.org/10.3390/jcm11030849
Ganjali S, Aghaee-Bakhtiari SH, Reiner Ž, Sahebkar A. Differential Expression of miRNA-223 in Coronary In-Stent Restenosis. Journal of Clinical Medicine. 2022; 11(3):849. https://doi.org/10.3390/jcm11030849
Chicago/Turabian StyleGanjali, Shiva, Seyed Hamid Aghaee-Bakhtiari, Željko Reiner, and Amirhossein Sahebkar. 2022. "Differential Expression of miRNA-223 in Coronary In-Stent Restenosis" Journal of Clinical Medicine 11, no. 3: 849. https://doi.org/10.3390/jcm11030849
APA StyleGanjali, S., Aghaee-Bakhtiari, S. H., Reiner, Ž., & Sahebkar, A. (2022). Differential Expression of miRNA-223 in Coronary In-Stent Restenosis. Journal of Clinical Medicine, 11(3), 849. https://doi.org/10.3390/jcm11030849







