The Efficacy of Mebeverine in the Treatment of Irritable Bowel Syndrome—A Systematic Review
Abstract
:1. Introduction
2. Materials and Methods
2.1. Information Sources and Searches
2.2. Study Selection and Quality Evaluation
2.3. Data Items and Extraction
2.4. Statistical Analysis
3. Results
3.1. Overview of Included Studies
3.2. Efficacy of Mebeverine
3.2.1. Abdominal Pain and Discomfort
3.2.2. Abdominal Distension
3.2.3. Abnormal Bowel Habits and Bloating
3.2.4. Constipation and Diarrhoea
3.2.5. Stool Frequency and Consistency
3.2.6. Nausea, Anxiety and Depression
3.3. Safety Assessment
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Canavan, C.; West, J.; Card, T. The epidemiology of irritable bowel syndrome. Clin. Epidemiol. 2014, 6, 71–80. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Drossman, D.A. Functional Gastrointestinal Disorders: History, Pathophysiology, Clinical Features and Rome IV. Gastroenterology 2016, 150, 1262–1279. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lacy, B.E.; Patel, N.K. Rome Criteria and a Diagnostic Approach to Irritable Bowel Syndrome. J. Clin. Med. 2017, 6, 99. [Google Scholar] [CrossRef]
- Moayyedi, P.; Mearin, F.; Azpiroz, F.; Andresen, V.; Barbara, G.; Corsetti, M.; Emmanuel, A.; Hungin, A.P.S.; Layer, P.; Stanghellini, V.; et al. Irritable bowel syndrome diagnosis and management: A simplified algorithm for clinical practice. United Eur. Gastroenterol. J. 2017, 5, 773–788. [Google Scholar] [CrossRef] [Green Version]
- Mearin, F.; Lacy, B.E.; Chang, L.; Chey, W.D.; Lembo, A.J.; Simren, M.; Spiller, R. Bowel Disorders. Gastroenterology 2016, 150, 1393–1407. [Google Scholar] [CrossRef] [Green Version]
- Chey, W.D.; Kurlander, J.; Eswaran, S. Irritable bowel syndrome: A clinical review. JAMA 2015, 313, 949–958. [Google Scholar] [CrossRef]
- Annaházi, A.; Róka, R.; Rosztóczy, A.; Wittmann, T. Role of antispasmodics in the treatment of irritable bowel syndrome. World J. Gastroenterol. 2014, 20, 6031–6043. [Google Scholar] [CrossRef]
- De Groote, J.; Standaert, L. The effect of a new musculotropic subtance 9(Mebeverine) on irritable colon. Tijdschr. Gastroenterol. 1968, 11, 524–528. [Google Scholar]
- Darvish-Damavandi, M.; Nikfar, S.; Abdollahi, M. A systematic review of efficacy and tolerability of mebeverine in irritable bowel syndrome. World J. Gastroenterol. 2010, 16, 547–553. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; Group, P. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. J. Clin. Epidemiol. 2009, 62, 1006–1012. [Google Scholar] [CrossRef]
- Higgins, J.; Savovic, J.; Elbers, R. Chapter 8: Assessing risk of bias in a randomized trial. In Cochrane Handbook for Systematic Reviews of Interventions; Version 6.0; John Wiley & Sons: Chichester, UK, 2019. [Google Scholar]
- NICE. Quality of Case Series Form. Available online: http://www.nice.org.uk/guidance/cg3/resources/appendix-4-quality-of-case-series-form2 (accessed on 1 January 2021).
- Guslandi, M. Mebeverine plus saccharomyces boularii versus mebeverine alone in the treatment of irritable bowel syndrome without constipation: A retrospective analysis. Am. J. Gastroenterol. 2011, 106, S495. [Google Scholar] [CrossRef]
- Hou, X.; Chen, S.; Zhang, Y.; Sha, W.; Yu, X.; El Sawah, H.; Afifi, A.F.; El-Khayat, H.R.; Nouh, A.; Hassan, M.F.; et al. Quality of life in patients with Irritable Bowel Syndrome (IBS), assessed using the IBS-Quality of Life (IBS-QOL) measure after 4 and 8 weeks of treatment with mebeverine hydrochloride or pinaverium bromide: Results of an international prospective observational cohort study in Poland, Egypt, Mexico and China. Clin. Drug Investig. 2014, 34, 783–793. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Baume, P. Mebeverine, an effective agent in the irritable colon syndrome. Aust. N. Z. J. Med. 1972, 2, 34–36. [Google Scholar] [CrossRef]
- Everitt, H.; Moss-Morris, R.; Sibelli, A.; Tapp, L.; Coleman, N.; Yardley, L.; Smith, P.W.F.; Little, P. Management of irritable bowel syndrome in primary care: The results of an exploratory randomised controlled trial of mebeverine, methylcellulose, placebo and a self-management website. BMC Gastroenterol. 2013, 13, 68. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Connell, A.M. Physiological and clinical assessment of the effect of the musculotropic agent mebeverine on the human colon. Br. Med. J. 1965, 2, 848–851. [Google Scholar] [CrossRef] [Green Version]
- Prout, B.J. The treatment of irritable bowel syndrome. Two doses of mebeverine compared. Practitioner 1983, 227, 1607–1608. [Google Scholar]
- Kruis, W.; Weinzierl, M.; Schüssler, P.; Holl, J. Comparison of the therapeutic effect of wheat bran, mebeverine and placebo in patients with the irritable bowel syndrome. Digestion 1986, 34, 196–201. [Google Scholar] [CrossRef]
- Capurso, L.; Koch, M.; Tarquini, M.; Dezi, A.; Papi, C.; Fracasso, P. The irritable bowel syndrome. A cross-over study of octilonium bromide, mebeverine and placebo. Clin. Trials J. 1984, 21, 285–291. [Google Scholar]
- Chakraborty, D.S.; Hazra, A.; Sil, A.; Pain, S. Will controlled release mebeverine be able to surpass placebo in treatment of diarrhoea predominant irritable bowel syndrome? J. Fam. Med. Prim. Care 2019, 8, 3173–3178. [Google Scholar] [CrossRef]
- Schaffstein, W.; Panijel, M.; Luettecke, K. Comparative safety and efficacy of trimebutine versus mebeverine in the treatment of irritable bowel syndrome. A multicenter double-blind study. Curr. Res. Clin. Exp. 1990, 47, 136–145. [Google Scholar]
- Rahman, M.Z.; Ahmed, D.S.; Mahmuduzzaman, M.; Chowdhury, M.S.; Barua, R.; Ishaque, S.M. Comparative efficacy and safety of trimebutine versus mebeverine in the treatment of irritable bowel syndrome. Mymensingh Med. J. 2014, 23, 105–113. [Google Scholar] [PubMed]
- Chang, F.Y.; Lu, C.L.; Luo, J.C.; Chen, T.S.; Chen, M.J.; Chang, H.J. The evaluation of otilonium bromide treatment in Asian patients with irritable bowel syndrome. J. Neurogastroenterol. Motil. 2011, 17, 402–410. [Google Scholar] [CrossRef] [PubMed]
- Lu, C.; Chen, C.; Chang, F.; Chang, S.; Kang, L.; Lu, R.; Lee, S. Effect of a calcium channel blocker and antispasmodic in diarrhoea-predominant irritable bowel syndrome. J. Gastroenterol. Hepatol. 2000, 15, 925–930. [Google Scholar] [CrossRef] [PubMed]
- Jones, R.H.; Holtmann, G.; Rodrigo, L.; Ehsanullah, R.S.; Crompton, P.M.; Jacques, L.A.; Mills, J.G. Alosetron relieves pain and improves bowel function compared with mebeverine in female nonconstipated irritable bowel syndrome patients. Aliment. Pharm. 1999, 13, 1419–1427. [Google Scholar] [CrossRef]
- Sahib, A.S. Treatment of irritable bowel syndrome using a selected herbal combination of Iraqi folk medicines. J. Ethnopharmacol. 2013, 148, 1008–1012. [Google Scholar] [CrossRef] [PubMed]
- Lee, K.J.; Kim, N.Y.; Kwon, J.K.; Huh, K.C.; Lee, O.Y.; Lee, J.S.; Choi, S.C.; Sohn, C.I.; Myung, S.J.; Park, H.; et al. Efficacy of ramosetron in the treatment of male patients with irritable bowel syndrome with diarrhea: A multicenter, randomized clinical trial, compared with mebeverine. J. Neurogastroenterol. Motil. 2011, 23, 1098–1104. [Google Scholar] [CrossRef]
- Hatami, K.; Kazemi-Motlagh, A.H.; Ajdarkosh, H.; Zargaran, A.; Karimi, M.; Shamshiri, A.R.; Ghadir, M.R. Comparing the Efficacy of Cumin Sofouf With Mebeverine on Irritable Bowel Syndrome Severity and Quality of Life: A Double-blind Randomized Clinical Trial. Crescent. J. Med. Biol. Sci. 2020, 7, 186–194. [Google Scholar]
- Mokhtare, M.; Asadipanah, M.; Bahardoust, M.; Chaharmahali, A.; Sikaroudi, M.K.; Khoshdelnezamiha, M.; Davanloo, F.A.; Masoodi, M.; Bahadorizadeh, L. Efficacy of adding Luvos® Healing Earth supplementation to mebeverine in improving symptoms and quality of life of patients with diarrhea-predominant irritable bowel syndrome: A randomized clinical trial. Biomed. Res. 2018, 5, 2776–2783. [Google Scholar] [CrossRef]
- Tudor, G.J. A general practice study to compare alverine citrate with mebeverine hydrochloride in the treatment of irritable bowel syndrome. Br. J. Clin. Pract. 1986, 40, 276–278. [Google Scholar]
- Inauen, W.; Halter, F. Clinical Efficacy, Safety and Tolerance of Mebeverine Slow Release (200 mg) vs Mebeverine Tablets in Patients with Irritable Bowel Syndrome. Drug Investig. 1994, 8, 234–240. [Google Scholar] [CrossRef]
- Van Outryve, M.; Mayeur, S.; Meeus, M.A.; Rosillon, D.; Hendrickx, B.; Ceuppens, M. A double-blind crossover comparison study of the safety and efficacy of mebeverine with mebeverine sustained release in the treatment of irritable bowel syndrome. J. Clin. Pharm. 1995, 20, 277–282. [Google Scholar] [CrossRef] [PubMed]
- Gilbody, J.S.; Fletcher, C.P.; Hughes, I.W.; Kidman, S.P. Comparison of two different formulations of mebeverine hydrochloride in irritable bowel syndrome. Int. J. Clin. Pract. 2000, 54, 461–464. [Google Scholar] [PubMed]
- Everitt, H.A.; Moss-Morris, R.E.; Sibelli, A.; Tapp, L.; Coleman, N.S.; Yardley, L.; Smith, P.W.; Little, P.S. Management of irritable bowel syndrome in primary care: Feasibility randomised controlled trial of mebeverine, methylcellulose, placebo and a patient self-management cognitive behavioural therapy website. (MIBS trial). BMC Gastroenterol. 2010, 10, 136. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Everitt, H. Management of Irritable Bowel Syndrome in Primary Care (MIBS Trial). ClinicalTrials.gov, Internet. Available online: https://clinicaltrials.gov/ct2/show/NCT00934973 (accessed on 17 June 2021).
- Clinicaltrialsregister.eu Internet. Management of Irritable Bowel Syndrome in Primary Care: Feasibility Randomised Controlled Trial of Mebeverine, Methylcellulose, Placebo and a Patient Self-Management Cognitive Behavioural Therapy Website. (MIBS Trial). Available online: https://www.clinicaltrialsregister.eu/ctr-search/trial/2009-013426-16/GB (accessed on 17 June 2021).
- Lee, K.J.; Poong-Lyul, R. A Randomized, Open Labeled, Multicenter Clinical Trial on the Effectiveness and Safety of the 5-HT3-Receptor Antagonist Ramosetron in Male Patients with Irritable Bowel Syndrome With Diarrhea: Comparison With Mebeverine. Gastroenterology 2011, 140, S-06. [Google Scholar] [CrossRef]
- Moayyedi, P.; Andrews, C.N.; MacQueen, G.; Korownyk, C.; Marsiglio, M.; Graff, L.; Kvern, B.; Lazarescu, A.; Liu, L.; Paterson, W.G.; et al. Canadian Association of Gastroenterology Clinical Practice Guideline for the Management of Irritable Bowel Syndrome (IBS). J. Can. Assoc. Gastroenterol. 2019, 2, 6–29. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pietrzak, A.; Skrzydło-Radomańska, B.; Mulak, A.; Lipiński, M.; Małecka-Panas, E.; Regula, J.; Rydzewska, G. Guidelines on the management of irritable bowel syndrome: In memory of Professor Witold Bartnik. Prz. Gastroenterol. 2018, 13, 259–288. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jailwala, J.; Imperiale, T.F.; Kroenke, K. Pharmacologic treatment of the irritable bowel syndrome: A systematic review of randomized, controlled trials. Ann. Intern. Med. 2000, 133, 136–147. [Google Scholar] [CrossRef] [PubMed]
- Poynard, T.; Regimbeau, C.; Benhamou, Y. Meta-analysis of smooth muscle relaxants in the treatment of irritable bowel syndrome. Aliment. Pharm. 2001, 15, 355–361. [Google Scholar] [CrossRef] [Green Version]
- Gralnek, I.M.; Hays, R.D.; Kilbourne, A.; Naliboff, B.; Mayer, E.A. The impact of irritable bowel syndrome on health-related quality of life. Gastroenterology 2000, 119, 654–660. [Google Scholar] [CrossRef]
- Poynard, T.; Naveau, S.; Mory, B.; Chaput, J.C. Meta-analysis of smooth muscle relaxants in the treatment of irritable bowel syndrome. Aliment. Pharm. 1994, 8, 499–510. [Google Scholar] [CrossRef]
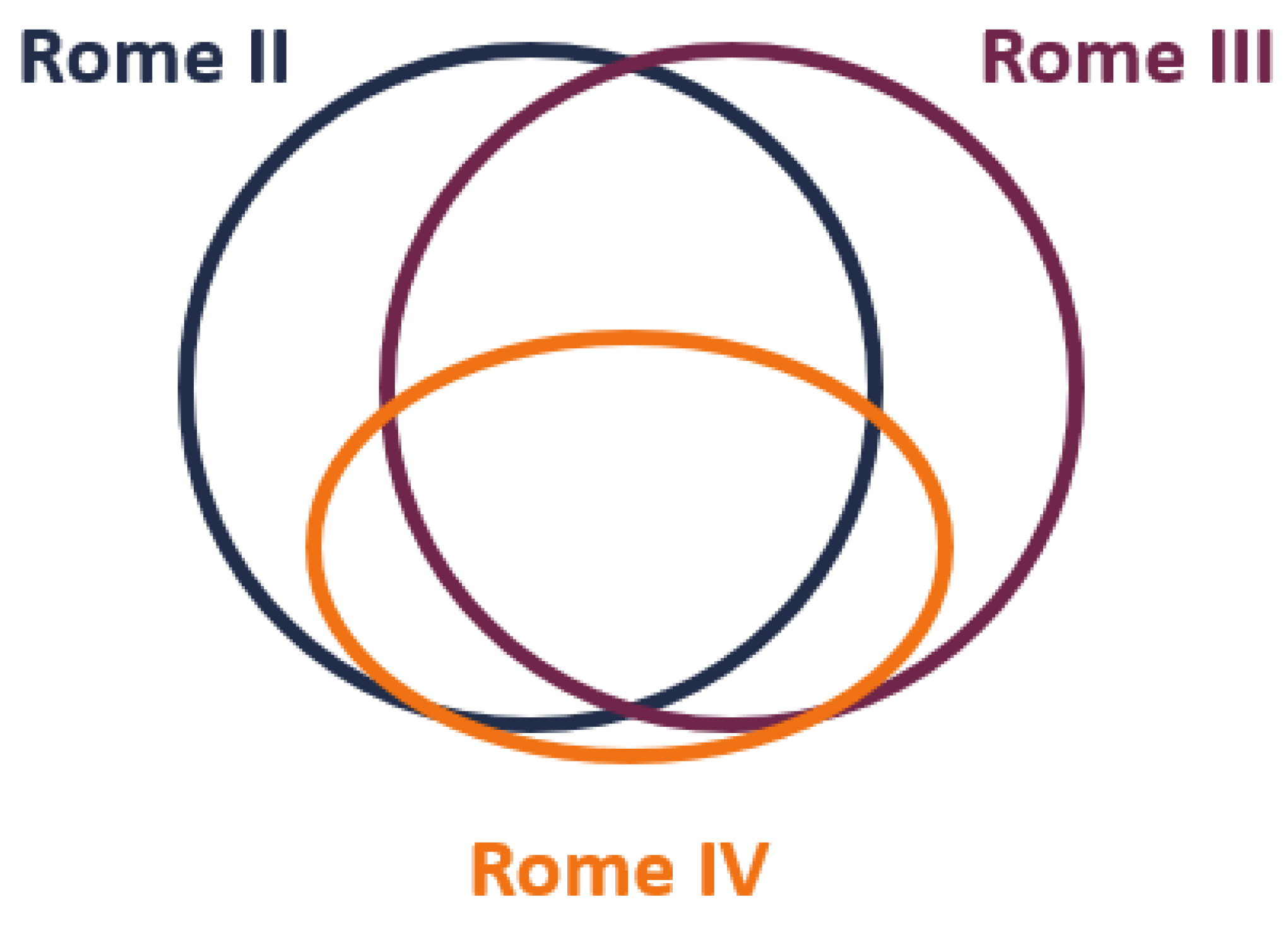
- Vork, L.; Weerts, Z.Z.; Mujagic, Z.; Kruimel, J.W.; Hesselink, M.A.M.; Muris, J.; Keszthelyi, D.; Jonkers, D.M.A.E.; Masclee, A.A.M. Rome III vs Rome IV criteria for irritable bowel syndrome: A comparison of clinical characteristics in a large cohort study. J. Neurogastroenterol. Motil. 2018, 30, e13189. [Google Scholar] [CrossRef] [PubMed]
- Ghoshal, U.C.; Abraham, P.; Bhatia, S.J.; Misra, S.P.; Choudhuri, G.; Biswas, K.D.; Chakravartty, K.; Dadhich, S.; Goswami, B.D.; Jayanthi, V.; et al. Comparison of Manning, Rome I, II, and III, and Asian diagnostic criteria: Report of the Multicentric Indian Irritable Bowel Syndrome (MIIBS) study. Indian J. Gastroenterol. 2013, 32, 369–375. [Google Scholar] [CrossRef] [PubMed]
- Sperber, A.D.; Shvartzman, P.; Friger, M.; Fich, A. A comparative reappraisal of the Rome II and Rome III diagnostic criteria: Are we getting closer to the ‘true’ prevalence of irritable bowel syndrome? Eur J. Gastroenterol. Hepatol. 2007, 19, 441–447. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Park, D.W.; Lee, O.Y.; Shim, S.G.; Jun, D.W.; Lee, K.N.; Kim, H.Y.; Lee, H.L.; Yoon, B.C.; Choi, H.S. The Differences in Prevalence and Sociodemographic Characteristics of Irritable Bowel Syndrome According to Rome II and Rome III. J. Neurogastroenterol. Motil. 2010, 16, 186–193. [Google Scholar] [CrossRef] [Green Version]
- Bai, T.; Xia, J.; Jiang, Y.; Cao, H.; Zhao, Y.; Zhang, L.; Wang, H.; Song, J.; Hou, X. Comparison of the Rome IV and Rome III criteria for IBS diagnosis: A cross-sectional survey. J. Gastroenterol. Hepatol. 2017, 32, 1018–1025. [Google Scholar] [CrossRef]
- Palsson, O.S.; Whitehead, W.; Törnblom, H.; Sperber, A.D.; Simren, M. Prevalence of Rome IV Functional Bowel Disorders Among Adults in the United States, Canada, and the United Kingdom. Gastroenterology 2020, 158, 1262–1273. [Google Scholar] [CrossRef]
- Patcharatrakul, T.; Thanapirom, K.; Gonlachanvit, S. Application of Rome III vs. Rome IV Diagnostic Criteria for Irritable Bowel Syndrome (IBS) in Clinical Practice: Is the Newer the Better? Gastroenterology 2017, 140, S717. [Google Scholar] [CrossRef]
- Pitz, N.; Cheang, M.; Bernstein, C. Defining the predictors of the placebo response in irritable bowel syndrome. Clin. Gastrol. Hepatol. 2005, 3, 237–247. [Google Scholar] [CrossRef]

| PICOS | Inclusion Criteria | Exclusion Criteria |
|---|---|---|
| Population | Patients with a diagnosis of IBS | Functional gastrointestinal disorders other than IBS |
| Intervention | Mebeverine, regardless of the dose and duration of treatment | Mebeverine in combination with another drug, cognitive therapy or diet |
| Comparators | No restrictions | x |
| Outcomes | Severity or frequency of bowel symptoms: abdominal pain or discomfort, abdominal distension, abnormal bowel habits, bloating, constipation, diarrhoea and other | x |
| Study (methodology) | Studies (experimental or observational) including ≥10 patients | Case studies, secondary studies (systematic reviews, reviews) |
| Study Name | Population | Diagnostic Criteria | Mebeverine Arm | Evaluated Symptoms | ||
|---|---|---|---|---|---|---|
| N | Dose | Treatment Period | ||||
| Lu 2000 [25] | IBS-D: 100% | Manning criteria | 46 | 100 mg 3 times daily | 2 weeks | Abdominal pain, bloating, stool frequency, stool consistency, incomplete evacuation, stool with mucus |
| Van Outryve 1995 [33] | IBS NOS: 100% | Kruis criteria | 60 | 135 mg, 2 tablets 3 times daily or sustained release 200 mg, 2 tablets twice daily (crossing-over) | 6 weeks | Abdominal pain, bloating, flatulence, constipation |
| Schaffstein 1990 [22] | IBS-C100% a | Kruis criteria | 99 | 135 mg 3 times daily | 4 weeks | Abdominal pain |
| Jones 1999 [26] | IBS-D: 71%, IBS-C: 5%, IBS-M: 24% | Rome I | 304 | 135 mg 3 times daily | 12 weeks | Pain and discomfort, urgency, stool frequency, stool consistency |
| Gilbody 2000 [34] | IBS NOS: 100% | Rome I | 184 | 135 mg 3 times daily or 200 mg twice daily | 8 weeks | Abdominal pain |
| Chang 2011 [24] | IBS-D: 72%, IBS-C: 21%, IBS-M: 7% | Rome II | 58 | 100 mg 3 times daily | 8 weeks | Bloating, flatulence, stool frequency |
| Rahman 2014 [23] | IBS-D: 67%, IBS-C: 33% b | Rome II | 70 | 135 mg twice daily | 6 weeks | Abdominal pain, flatulence, stool frequency, stool consistency |
| Sahib 2013 [27] | IBS NOS: 100% | Rome III | 20 | 135 mg 3 times daily | 8 weeks | Pain, abdominal distension, urgency, stool frequency, stool consistency, incomplete evacuation, the passing of mucus |
| MIBS trial 2013 [16,35,36,37] | IBS-D: 30%, IBS-C: 11%, IBS-M: 57% | Rome III | 43 | 135 mg 3 times daily | 6 weeks | IBS-SSS (severity of abdominal pain, duration of abdominal pain, abdominal distension/tightness, bowel habit, quality of life), anxiety, depression |
| Lee 2011 [28,38] | IBS-D: 100% | Rome III | 168 | 135 mg 3 times daily | 4 weeks | Abdominal pain/discomfort, abnormal bowel habits, urgency, stool frequency, stool consistency |
| Guslandi 2011 [13] | IBS-D: 100% c | Rome III | 28 | 200 mg twice daily | 6 weeks | Abdominal discomfort, bloating, diarrhoea |
| Hou 2014 [14] | IBS-D: 33%, IBS-C: 33%, IBS-M: 33% | Rome III | 464 | 135 mg 3 times daily or 200 mg twice daily or prolonged-release 200 mg twice daily | 8 weeks | Abdominal pain/discomfort, quality of life |
| Chakraborty 2019 [21] | IBS -D: 100% | Rome IV | 20 | 200 mg twice daily controlled release | 8 weeks | Abdominal pain, stool frequency, quality of life |
| Hatami 2020 [29] | IBS-D: 22.5%, IBS-C: 12.5%, IBS-M: 65% | Rome IV | 40 | 200 mg twice daily sustain release | 4 weeks | Abdominal pain, flatulence, quality of life |
| Mokhtare 2018 [30] | IBS-D: 100% | Rome IV | 36 | 135 mg twice daily | 4 weeks | Abdominal pain, bloating, diarrhoea, stool frequency |
| Connell 1965 [17] | IBS NOS: 100% | NR | 20 | 100 mg 4 times daily | 12 weeks | Abdominal cramps, disturbance of bowel habit |
| Baume 1972 [15] | IBS NOS: 100% | Truelove and Reynell diagnostic criteria for IBS | 59 | 50 mg, 2 tablets twice daily | 2 weeks | Pain, abnormal bowel habits |
| Prout 1983 [18] | IBS NOS: 100% | NR | 41 | 405 mg or 810 mg (crossing-over) | 8 weeks | Abdominal pain, abdominal distension, pain on moving bowels, wind, nausea, anxiety |
| Kruis 1986 [19] | IBS-D: 18%, IBS-C: 36%, IBS-M: 46% d | Own criteria | 40 | 100 mg 4 times daily | 16 weeks | Abdominal pain, irregular bowel habits, flatulence |
| Inauen 1994 [32] | IBS NOS: 100% | NR | 48 | 135 mg 3 times daily or slow-release 200 mg twice daily | 3 weeks | Abdominal pain, abdominal distension, constipation |
| Tudor 1986 [31] | IBS NOS: 100% | NR | 37 | 135 mg | 4 weeks | Abdominal pain, bowel habits |
| Capurso 1984 [20] | IBS NOS: 100% | NR | 60 | 135 mg 3 times daily | 2 weeks | Pain, flatulence, constipation or diarrhoea |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Daniluk, J.; Malecka-Wojciesko, E.; Skrzydlo-Radomanska, B.; Rydzewska, G. The Efficacy of Mebeverine in the Treatment of Irritable Bowel Syndrome—A Systematic Review. J. Clin. Med. 2022, 11, 1044. https://doi.org/10.3390/jcm11041044
Daniluk J, Malecka-Wojciesko E, Skrzydlo-Radomanska B, Rydzewska G. The Efficacy of Mebeverine in the Treatment of Irritable Bowel Syndrome—A Systematic Review. Journal of Clinical Medicine. 2022; 11(4):1044. https://doi.org/10.3390/jcm11041044
Chicago/Turabian StyleDaniluk, Jaroslaw, Ewa Malecka-Wojciesko, Barbara Skrzydlo-Radomanska, and Grazyna Rydzewska. 2022. "The Efficacy of Mebeverine in the Treatment of Irritable Bowel Syndrome—A Systematic Review" Journal of Clinical Medicine 11, no. 4: 1044. https://doi.org/10.3390/jcm11041044
APA StyleDaniluk, J., Malecka-Wojciesko, E., Skrzydlo-Radomanska, B., & Rydzewska, G. (2022). The Efficacy of Mebeverine in the Treatment of Irritable Bowel Syndrome—A Systematic Review. Journal of Clinical Medicine, 11(4), 1044. https://doi.org/10.3390/jcm11041044







