Learning Curve Analysis of Single-Site Robot-Assisted Hysterectomy
Abstract
:1. Introduction
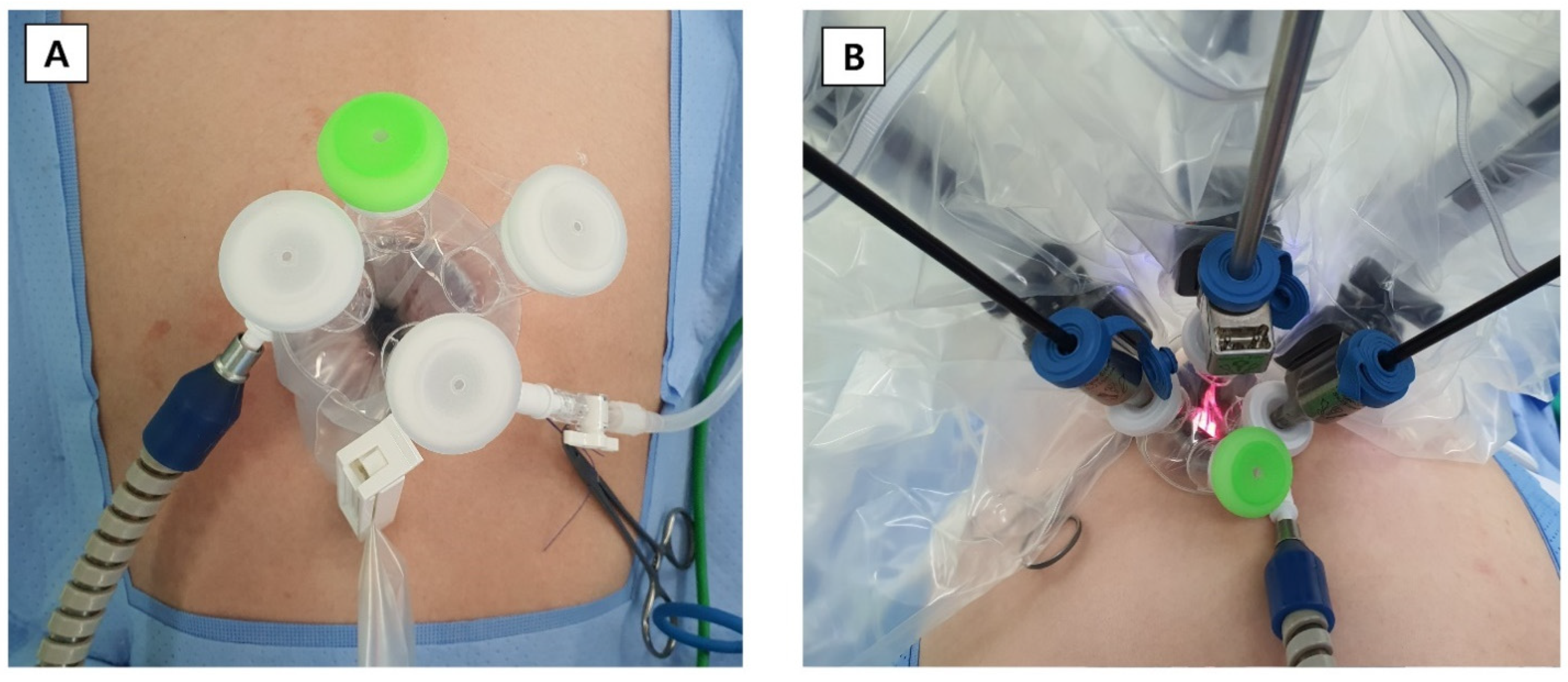
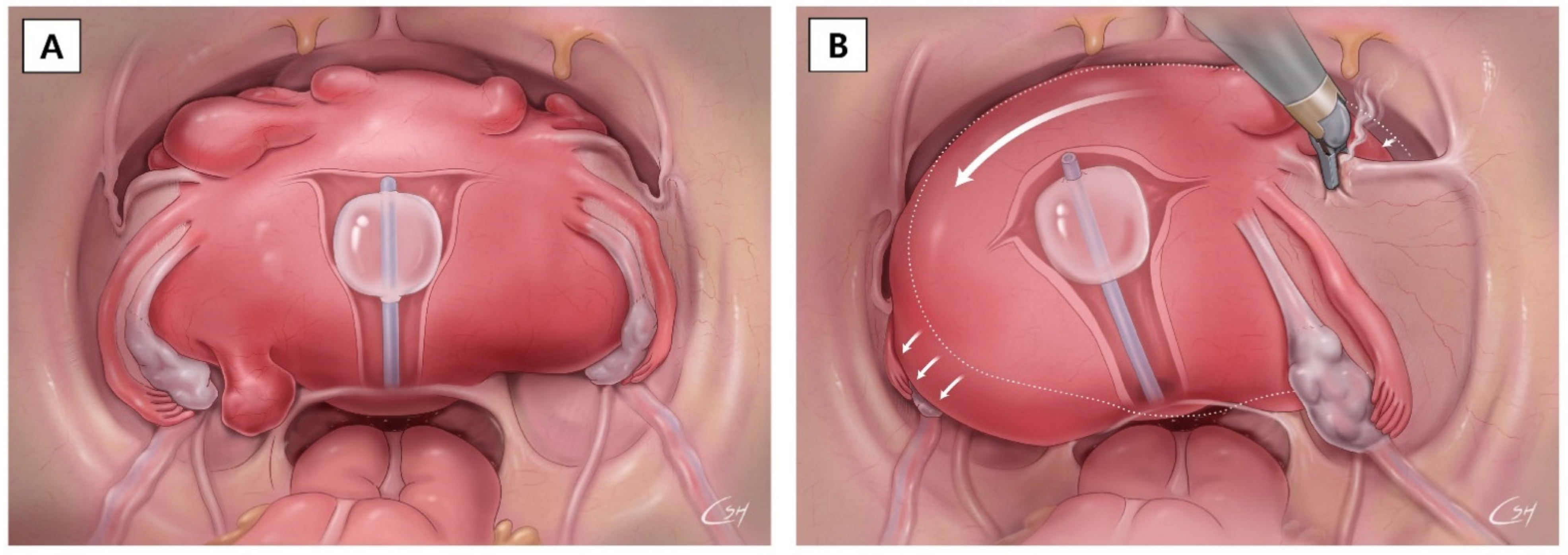
2. Materials and Methods
Statistical Analysis
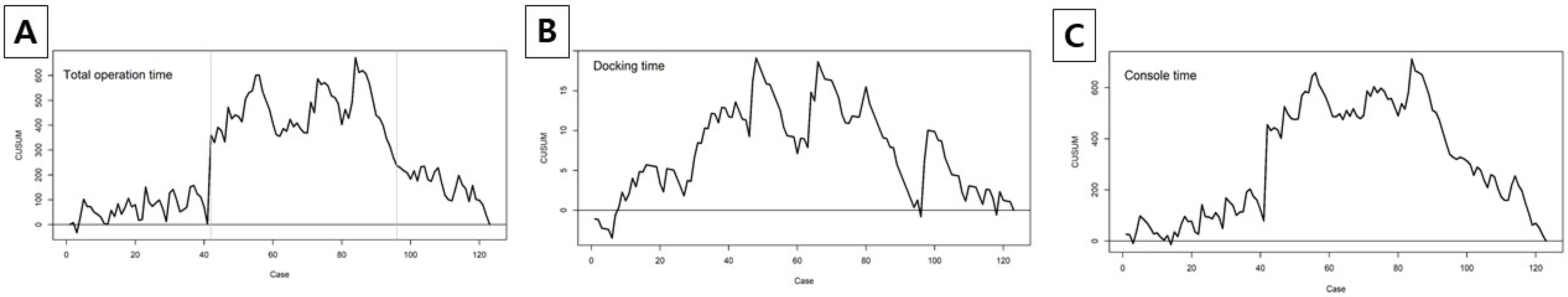
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Uppal, S.; Frumovitz, M.; Escobar, P.; Ramirez, P.T. Laparoendoscopic single-site surgery in gynecology: Review of literature and available technology. J. Minim. Invasive Gynecol. 2011, 18, 12–23. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gala, R.B.; Margulies, R.; Steinberg, A.; Murphy, M.; Lukban, J.; Jeppson, P.; Aschkenazi, S.; Olivera, C.; South, M.; Lowenstein, L.; et al. Systematic review of robotic surgery in gynecology: Robotic techniques compared with laparoscopy and laparotomy. J. Minim. Invasive Gynecol. 2014, 21, 353–361. [Google Scholar] [CrossRef]
- Bouquet de Joliniere, J.; Librino, A.; Dubuisson, J.B.; Khomsi, F.; Ben Ali, N.; Fadhlaoui, A.; Ayoubi, J.M.; Feki, A. Robotic Surgery in Gynecology. Front. Surg. 2016, 3, 26. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kim, M.; Kim, M.K.; Kim, M.L.; Jung, Y.W.; Yun, B.S.; Seong, S.J. Robotic single-site myomectomy: A single-center experience of 101 consecutive cases. Int. J. Med. Robot. + Comput. Assist. Surg. MRCAS. 2019, 15, e1959. [Google Scholar] [CrossRef] [Green Version]
- Beste, T.M.; Nelson, K.H.; Daucher, J.A. Total laparoscopic hysterectomy utilizing a robotic surgical system. JSLS J. Soc. Laparoendosc. Surg. 2005, 9, 13–15. [Google Scholar]
- Fiorentino, R.P.; Zepeda, M.A.; Goldstein, B.H.; John, C.R.; Rettenmaier, M.A. Pilot study assessing robotic laparoscopic hysterectomy and patient outcomes. J. Minim. Invasive Gynecol. 2006, 13, 60–63. [Google Scholar] [CrossRef] [PubMed]
- Marchal, F.; Rauch, P.; Vandromme, J.; Laurent, I.; Lobontiu, A.; Ahcel, B.; Verhaeghe, J.L.; Meistelman, C.; Degueldre, M.; Villemot, J.P.; et al. Telerobotic-assisted laparoscopic hysterectomy for benign and oncologic pathologies: Initial clinical experience with 30 patients. Surg. Endosc. 2005, 19, 826–831. [Google Scholar] [CrossRef] [PubMed]
- Park, J.S.; Ahn, H.K.; Na, J.; Lee, H.H.; Yoon, Y.E.; Yoon, M.G.; Han, W.K. Cumulative sum analysis of the learning curve for video-assisted minilaparotomy donor nephrectomy in healthy kidney donors. Medicine 2018, 97, e0560. [Google Scholar] [CrossRef] [PubMed]
- Hopper, A.N.; Jamison, M.H.; Lewis, W.G. Learning curves in surgical practice. Postgrad. Med. J. 2007, 83, 777–779. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chiu, L.H.; Chen, C.H.; Tu, P.C.; Chang, C.W.; Yen, Y.K.; Liu, W.M. Comparison of robotic surgery and laparoscopy to perform total hysterectomy with pelvic adhesions or large uterus. J. Minim. Access Surg. 2015, 11, 87–93. [Google Scholar] [PubMed]
- Sinha, R.; Bana, R.; Sanjay, M. Comparison of Robotic and Laparoscopic Hysterectomy for the Large Uterus. SLS J. Soc. Laparoendosc. Surg. 2019, 23, 87–93. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Terzi, H.; Hasdemir, P.S.; Biler, A.; Kale, A.; Sendag, F. Evaluation of the surgical outcome and complications of total laparoscopic hysterectomy in patients with enlarged uteruses. Int. J. Surg. 2016, 36, 90–95. [Google Scholar] [CrossRef]
- Boggess, J.F.; Gehrig, P.A.; Cantrell, L.; Shafer, A.; Mendivil, A.; Rossi, E.; Hanna, R. Perioperative outcomes of robotically assisted hysterectomy for benign cases with complex pathology. Obstet. Gynecol. 2009, 114, 585–593. [Google Scholar] [CrossRef] [PubMed]
- Cela, V.; Freschi, L.; Simi, G.; Ruggiero, M.; Tana, R.; Pluchino, N. Robotic single-site hysterectomy: Feasibility, learning curve and surgical outcome. Surg. Endosc. 2013, 27, 2638–2643. [Google Scholar] [CrossRef] [PubMed]
- El Hachem, L.; Momeni, M.; Friedman, K.; Moshier, E.L.; Chuang, L.T.; Gretz, H.F., 3rd. Safety, feasibility and learning curve of robotic single-site surgery in gynecology. Int. J. Med. Robot. 2016, 12, 509–516. [Google Scholar] [CrossRef] [PubMed]
- Buckley de Meritens, A.; Kim, J.; Dinkelspiel, H.; Chapman-Davis, E.; Caputo, T.; Holcomb, K.M. Feasibility and Learning Curve of Robotic Laparoendoscopic Single-Site Surgery in Gynecology. J. Minim. Invasive Gynecol. 2017, 24, 323–328. [Google Scholar] [CrossRef] [PubMed]
- Paek, J.; Kim, S.W.; Lee, S.-H.; Lee, M.; Yim, G.-W.; Nam, E.-J.; Kim, Y.-T. Learning curve and surgical outcome for single-port access total laparoscopic hysterectomy in 100 consecutive cases. Gynecol. Obstet. Investig. 2011, 72, 227–233. [Google Scholar] [CrossRef] [PubMed]
- Ahn, S.H.; Park, J.H.; Kim, H.R.; Cho, S.; Lee, M.; Seo, S.K.; Choi, Y.S.; Lee, B.S. Robotic single-site versus multi-port myomectomy: A case-control study. BMC Surg. 2021, 21, 264. [Google Scholar] [CrossRef] [PubMed]
- Woelk, J.L.; Casiano, E.R.; Weaver, A.L.; Gostout, B.S.; Trabuco, E.C.; Gebhart, J.B. The learning curve of robotic hysterectomy. Obs. Gynecol. 2013, 121, 87–95. [Google Scholar] [CrossRef] [PubMed] [Green Version]
| Total | Phase 1 | Phase 2 | Phase 3 | ||||||
|---|---|---|---|---|---|---|---|---|---|
| (n = 123) | (n = 41) | (n = 54) | (n = 28) | ||||||
| N | % | n | % | n | % | n | % | p-Value | |
| Age (yr), median (range) | 49 (30–74) | 50 (35–68) | 48.5 (34–67) | 50 (30–74) | 0.8960 * | ||||
| BMI (kg/m2), median (range) | 23.2 (18.0–34.9) | 22.9 (18.0–34.9) | 23 (18.0–32.6) | 24.4 (18.6–29.8) | 0.2640 * | ||||
| Parity | 106 | 86.2 | 34 | 82.9 | 50 | 92.6 | 22 | 78.6 | 0.1662 † |
| Menopause | 48 | 39 | 16 | 39 | 20 | 37 | 12 | 42.9 | 0.8770 † |
| Chronic illness | 45 | 36.6 | 12 | 29.3 | 17 | 31.5 | 16 | 57.1 | 0.0359 † |
| Vaginal delivery | 73 | 59.4 | 24 | 58.5 | 32 | 59.3 | 17 | 60.7 | 0.9836 † |
| Previous cesarean section | 38 | 30.9 | 13 | 31.7 | 19 | 35.2 | 6 | 21.4 | 0.4375 † |
| Previous abdominal surgery | 47 | 38.2 | 11 | 26.8 | 19 | 35.2 | 17 | 60.7 | 0.0145 † |
| ASA classification | <0.0001 ‡ | ||||||||
| I | 74 | 60.2 | 33 | 80.5 | 37 | 68.5 | 4 | 14.3 | |
| II | 48 | 39 | 8 | 19.5 | 17 | 31.5 | 23 | 82.1 | |
| III | 1 | 0.8 | 0 | 0 | 0 | 0 | 1 | 3.6 | |
| Indication of surgery | 0.5755 ‡ | ||||||||
| Adenomyosis | 16 | 13 | 6 | 14.6 | 8 | 14.8 | 2 | 7.1 | |
| Myoma | 56 | 45.5 | 20 | 48.8 | 26 | 48.2 | 10 | 35.7 | |
| Adenomyosis and myoma | 27 | 22 | 8 | 19.5 | 12 | 22.2 | 7 | 25 | |
| Endometrial hyperplasia | 1 | 0.8 | 0 | 0 | 0 | 0 | 1 | 3.6 | |
| Malignancy | 3 | 2.4 | 0 | 0 | 1 | 1.9 | 2 | 7.1 | |
| Ovarian cyst | 20 | 16.3 | 7 | 17.1 | 7 | 13 | 6 | 21.4 | |
| Concomitant procedure | |||||||||
| Adnexectomy | 0.9466 ‡ | ||||||||
| USO | 2 | 1.6 | 1 | 2.4 | 1 | 1.9 | 0 | 0 | |
| BSO | 64 | 52 | 23 | 56.1 | 27 | 50 | 14 | 50 | |
| Ovarian cystectomy | 8 | 6.5 | 3 | 7.3 | 4 | 7.4 | 1 | 3.6 | 0.8078 ‡ |
| Peritonectomy | 2 | 1.6 | 1 | 2.4 | 1 | 1.9 | 0 | 0 | 1.0000 ‡ |
| Adhesiolysis | 61 | 49.6 | 23 | 56.1 | 28 | 51.9 | 10 | 35.7 | 0.2275 † |
| Pelvic washing cytology | 122 | 99.2 | 40 | 97.6 | 54 | 100 | 28 | 100 | 0.5610 ‡ |
| Pelvic LND | 19 | 15.5 | 6 | 14.6 | 9 | 16.7 | 4 | 14.3 | 0.9459 † |
| Para-aortic LND | 1 | 0.8 | 0 | 0 | 1 | 1.9 | 0 | 0 | 1.0000 ‡ |
| Total | Phase 1 | Phase 2 | Phase 3 | ||||||
|---|---|---|---|---|---|---|---|---|---|
| (n = 123) | (n = 41) | (n = 54) | (n = 28) | ||||||
| n | % | n | % | n | % | n | % | p-Value | |
| Uterine mass size (cm), median (range) | 6.8 (0–26) | 5 (0.5–13.5) | 7.5 (0–22) | 9.75 (6–26) | <0.0001 * | ||||
| Operation time (min), median (range) | 131 (59–502) | 140 (73–274) | 130.5 (59–502) | 129 (83–208) | 0.6943 * | ||||
| Docking time (min), median (range) | 3 (1–10) | 3 (1–6) | 2 (1–10) | 3 (1–10) | 0.0242 * | ||||
| Console time (min), median (range) | 76 (29–465) | 77 (41–208) | 77 (29–465) | 74 (40–147) | 0.4023 * | ||||
| Adnexal surgery | 66 | 53.7 | 24 | 58.5 | 28 | 51.9 | 14 | 50 | 0.7357 † |
| EBL (mL) | 10 (5–500) | 20 (5–160) | 10 (5–480) | 5 (5–500) | 0.0007 * | ||||
| Uterus weight (g) | 180 (44–1230) | 200.5 (50–730) | 180 (44–1230) | 159 (45–580) | 0.2371 * | ||||
| NA = 8 | NA = 5 | NA = 3 | |||||||
| Postoperative hospital stay (days), median (range) | 4 (3–10) | 4 (3–6) | 4 (3–10) | 4 (3–7) | 0.7595 * | ||||
| Conversion | |||||||||
| Open laparotomy | 1 | 0.8 | 0 | 0 | 0 | 0 | 1 | 3.6 | 0.2276 ‡ |
| Drain insertion | 9 | 7.3 | 7 | 17.1 | 1 | 1.9 | 1 | 3.6 | 0.0187 ‡ |
| Readmission | 5 | 4.1 | 1 | 2.4 | 3 | 5.6 | 1 | 3.6 | 0.8479 ‡ |
| Complications | |||||||||
| Immediate complication | |||||||||
| Abdominal pain | 3 | 2.4 | 0 | 0 | 3 | 5.6 | 0 | 0 | 0.3225 ‡ |
| Postoperative pain (NRS) | |||||||||
| Use of additional pain killer: NSAIDs, Opioids | 90 | 73.2 | 33 | 80.5 | 39 | 72.2 | 18 | 64.3 | 0.3216 † |
| PCA use on operation day | 11 | 8.9 | 8 | 19.5 | 3 | 5.6 | 0 | 0 | 0.0119 ‡ |
| PCA use after 24 h | 5 | 4.1 | 4 | 9.8 | 1 | 1.9 | 0 | 0 | 0.1188 ‡ |
| Pain killer not used | 28 | 22.8 | 4 | 9.8 | 14 | 25.9 | 10 | 35.7 | 0.0314 † |
| Delayed postoperative complication | 0.0296 ‡ | ||||||||
| Umbilical incisional hernias | 3 | 2.4 | 0 | 0 | 3 | 5.6 | 0 | 0 | |
| Vaginal cuff dehiscence | 2 | 1.6 | 0 | 0 | 0 | 0 | 2 | 7.1 | |
| Univariable | Multivariable (p < 0.05) | ||||||
|---|---|---|---|---|---|---|---|
| Beta | SE | p-Value | Beta | SE | p-Value | ||
| Age (yr) | −1.10 | 0.66 | 0.1012 | ||||
| BMI (kg/m2) | 2.44 | 1.48 | 0.1015 | ||||
| Uterus weight (g) | Missing = 8 | 0.19 | 0.02 | <0.0001 | 0.18 | 0.02 | <0.0001 |
| Parity | No | 1(ref) | 1(ref) | ||||
| Yes | −51.19 | 14.74 | 0.0007 | −36.49 | 12.42 | 0.0040 | |
| Menopause | No | 1(ref) | |||||
| Yes | −16.03 | 10.84 | 0.1416 | ||||
| Chronic illness | No | 1(ref) | |||||
| Yes | −11.75 | 11.02 | 0.2883 | ||||
| Vaginal delivery | No | 1(ref) | |||||
| Yes | −6.26 | 10.84 | 0.5646 | ||||
| Previous cesarean section | No | 1(ref) | |||||
| Yes | −15.87 | 11.45 | 0.1683 | ||||
| Previous abdominal surgery | No | 1(ref) | |||||
| Yes | −22.57 | 10.78 | 0.0385 | ||||
| ASA classification | I | 1(ref) | |||||
| II, III | −9.95 | 10.86 | 0.3614 | ||||
| Adnexectomy | None | 1(ref) | |||||
| USO, BSO | −15.47 | 10.60 | 0.1471 | ||||
| Ovarian cystectomy | No | 1(ref) | |||||
| Yes | 19.05 | 21.56 | 0.3788 | ||||
| Other (Peritonectomy, Adhesiolysis, | No | 1(ref) | |||||
| Pelvic LND, Para-aortic LND) | Yes | 19.63 | 10.62 | 0.0671 | |||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, Y.J.; Lee, D.-E.; Bae, J.; Ha, H.I.; Lim, M.C. Learning Curve Analysis of Single-Site Robot-Assisted Hysterectomy. J. Clin. Med. 2022, 11, 1378. https://doi.org/10.3390/jcm11051378
Lee YJ, Lee D-E, Bae J, Ha HI, Lim MC. Learning Curve Analysis of Single-Site Robot-Assisted Hysterectomy. Journal of Clinical Medicine. 2022; 11(5):1378. https://doi.org/10.3390/jcm11051378
Chicago/Turabian StyleLee, Yeon Jee, Dong-Eun Lee, Jaekyung Bae, Hyeong In Ha, and Myong Cheol Lim. 2022. "Learning Curve Analysis of Single-Site Robot-Assisted Hysterectomy" Journal of Clinical Medicine 11, no. 5: 1378. https://doi.org/10.3390/jcm11051378






