Prognosis of Coronary Artery Bypass Grafting in Preschool-Aged Patients with Myocardial Ischemia Due to Giant Aneurysm of Kawasaki Disease
Abstract
:1. Introduction
2. Patients and Methods
2.1. Patients
2.2. Coronary Flow Reserve
2.3. Fractional Flow Reserve
2.4. Echocardiography
2.5. Classification of Exercise Management in Post-CABG Follow-Up
- A: Home care/hospitalization is required;
- B: Able to go to school but unable to exercise;
- C: Able to participate in “light exercise for average students of the same age”;
- D: Able to participate in “moderate exercise for average students of the same age”; and
- E: Able to participate in “vigorous exercise for average students of the same age”
2.6. Statistics
2.7. Ethics Approval
3. Results
3.1. Patient Characteristics
3.2. Evaluation of CFR, FFR and Stenosis in the Bypass Graft
3.3. LVEF, Left Ventricular Wall Motion Abnormalities
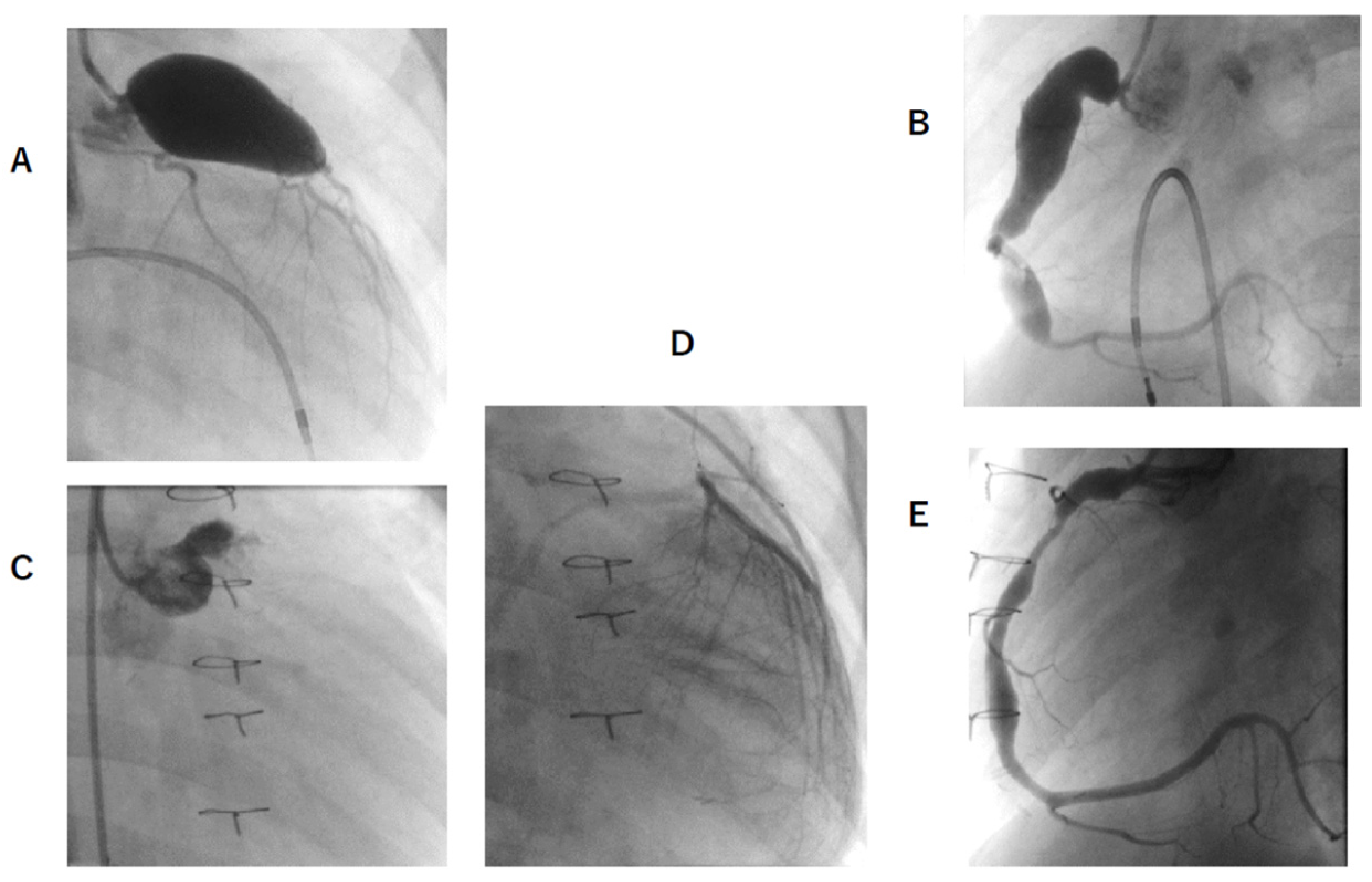
3.4. Latest CAG Findings
3.5. Post-CABG Medication and Classification of Exercise Management
4. Discussion
Study Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Fukazawa, R. Long-Term Prognosis of Kawasaki Disease: Increased Cardiovascular Risk? Curr. Opin. Pediatr. 2010, 22, 587–592. [Google Scholar] [CrossRef]
- Kitamura, S.; Kawashima, Y.; Fujita, T.; Mori, T.; Oyama, C. Aortocoronary Bypass Grafting in a Child with Coronary Artery Obstruction Due to Mucocutaneous Lymphnode Syndrome: Report of a Case. Circulation 1976, 53, 1035–1040. [Google Scholar] [CrossRef] [Green Version]
- Kitamura, S.; Kawachi, K.; Oyama, C.; Miyagi, Y.; Morita, R.; Koh, Y.; Kim, K.; Nishii, T. Severe Kawasaki Heart Disease Treated with an Internal Mammary Artery Graft in Pediatric Patients. A First Successful Report. J. Thorac. Cardiovasc. Surg. 1985, 89, 860–866. [Google Scholar] [CrossRef]
- Takeuchi, Y.; Gomi, A.; Okamura, Y.; Mori, H.; Nagashima, M. Coronary Revascularization in a Child with Kawasaki Disease: Use of Right Gastroepiploic Artery. Ann. Thorac. Surg. 1990, 50, 294–296. [Google Scholar] [CrossRef]
- Tsuda, E.; Kitamura, S.; The Cooperative Study Group of Japan. National Survey of Coronary Artery Bypass Grafting for Coronary Stenosis Caused by Kawasaki Disease in Japan. Circulation 2004, 110, II-61–II-66. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kitamura, S.; Kawachi, K.; Seki, T.; Morita, R.; Nishii, T.; Mizuguchi, K.; Fukutomi, M.; Hamada, Y.; Iioka, S. Bilateral Internal Mammary Artery Grafts for Coronary Artery Bypass Operations in Children. J. Thorac. Cardiovasc. Surg. 1990, 99, 708–715. [Google Scholar] [CrossRef]
- Tsuda, E.; Kitamura, S.; Kimura, K.; Kobayashi, J.; Miyazaki, S.; Echigo, S.; Yagihara, T. Long-Term Patency of Internal Thoracic Artery Grafts for Coronary Artery Stenosis Due to Kawasaki Disease: Comparison of Early with Recent Results in Small Children. Am. Heart J. 2007, 153, 995–1000. [Google Scholar] [CrossRef] [PubMed]
- Ochi, M. Review: Surgical Treatment of Giant Coronary Aneurysms in Pediatric Patients with Kawasaki Disease. Gen. Thorac. Cardiovasc. Surg. 2018, 66, 121–129. [Google Scholar] [CrossRef] [PubMed]
- Yamauchi, H.; Ochi, M.; Fujii, M.; Hinokiyama, K.; Ohmori, H.; Sasaki, T.; Ikegami, E.; Uchikoba, Y.; Ogawa, S.; Shimizu, K. Optimal Time of Surgical Treatment for Kawasaki Coronary Artery Disease. J. Nippon. Med. Sch. 2004, 71, 279–286. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Donohue, T.J.; Kern, M.J.; Aguirre, F.V.; Bach, R.G.; Wolford, T.; Bell, C.A.; Segal, J. Assessing the Hemodynamic Significance of Coronary Artery Stenoses: Analysis of Translesional Pressure-Flow Velocity Relations in Patients. J. Am. Coll. Cardiol. 1993, 22, 449–458. [Google Scholar] [CrossRef] [Green Version]
- Ogawa, S.; Ohkubo, T.; Fukazawa, R.; Kamisago, M.; Kuramochi, Y.; Uchikoba, Y.; Ikegami, E.; Watanabe, M.; Katsube, Y. Estimation of Myocardial Hemodynamics before and after Intervention in Children with Kawasaki Disease. J. Am. Coll. Cardiol. 2004, 43, 653–661. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pijls, N.H.; van Son, J.A.; Kirkeeide, R.L.; De Bruyne, B.; Gould, K.L. Experimental Basis of Determining Maximum Coronary, Myocardial, and Collateral Blood Flow by Pressure Measurements for Assessing Functional Stenosis Severity before and after Percutaneous Transluminal Coronary Angioplasty. Circulation 1993, 87, 1354–1367. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fukazawa, R.; Kobayashi, J.; Ayusawa, M.; Hamada, H.; Miura, M.; Mitani, Y.; Tsuda, E.; Nakajima, H.; Matsuura, H.; Ikeda, K.; et al. JCS/JSCS 2020 Guideline on Diagnosis and Management of Cardiovascular Sequelae in Kawasaki Disease. Circ. J. 2020, 84, 1348–1407. [Google Scholar] [CrossRef] [PubMed]
- Murakami, T.; Tanaka, N. The Physiological Significance of Coronary Aneurysms in Kawasaki Disease. EuroIntervention 2011, 7, 944–947. [Google Scholar] [CrossRef] [PubMed]
- Suzuki, A.; Miyagawa-Tomita, S.; Nakazawa, M.; Yutani, C. Remodeling of Coronary Artery Lesions Due to Kawasaki Disease: Comparison of Arteriographic and Immunohistochemical Findings. Jpn. Heart J. 2000, 41, 245–256. [Google Scholar] [PubMed] [Green Version]
- Van de Hoef, T.P.; Siebes, M.; Spaan, J.A.; Piek, J.J. Fundamentals in Clinical Coronary Physiology: Why Coronary Flow Is More Important than Coronary Pressure. Eur. Heart J. 2015, 36, 3312–3319. [Google Scholar] [CrossRef] [PubMed]
- Manabe, O.; Naya, M.; Tamaki, N. Feasibility of PET for the Management of Coronary Artery Disease: Comparison between CFR and FFR. J. Cardiol. 2017, 70, 135–140. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Van de Hoef, T.P.; van Lavieren, M.A.; Damman, P.; Delewi, R.; Piek, M.A.; Chamuleau, S.A.; Voskuil, M.; Henriques, J.P.; Koch, K.T.; de Winter, R.J.; et al. Physiological Basis and Long-Term Clinical Outcome of Discordance between Fractional Flow Reserve and Coronary Flow Velocity Reserve in Coronary Stenoses of Intermediate Severity. Circ. Cardiovasc. Interv. 2014, 7, 301–311. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- McCrindle, B.W.; Rowley, A.H.; Newburger, J.W.; Burns, J.C.; Bolger, A.F.; Gewitz, M.; Baker, A.L.; Jackson, M.A.; Takahashi, M.; Shah, P.B.; et al. Diagnosis, Treatment, and Long-Term Management of Kawasaki Disease: A Scientific Statement for Health Professionals From the American Heart Association. Circulation 2017, 135, e927–e999. [Google Scholar] [CrossRef] [PubMed]

| Patient | Sex | Age at Onset (Months) | Age at CABG (Months) | Period from Onset to CABG (Months) | Post-Surgery Observation Period (Months) | Coronary AN (Diameter × Length) | Stenosis | Thrombus | Event | Surgical Procedure |
|---|---|---|---|---|---|---|---|---|---|---|
| A | Female | 32 | 51 | 19 | 134 | LAD: 12.0 × 28 mm RCA: 7.0 × 12 mm | No | Yes | Angina | LITA–LAD |
| B | Male | 13 | 38 | 25 | 108 | LAD: 10.0 × 20 mm | 75% LS at AN outlet | Yes | No | LITA–LAD |
| C | Male | 36 | 76 | 40 | 110 | LAD: 8.5 × 12 mm RCA: Occluded | 90% LS at AN outlet | No | No | LITA–LAD |
| D | Male | 14 | 18 | 4 | 46 | LAD: 17.5 × 40 mm LCx: 10.0 × 15 mm RCA: Occluded | No | Yes | No | LITA–LAD |
| E | Male | 54 | 59 | 5 | 37 | LAD: 15.2 × 23 mm RCA: 7.5 × 17 mm | 90% LS at AN outlet | No | No | LITA–LAD RCA down-sizing |
| F | Male | 50 | 62 | 12 | 115 | LMT: 19.0 × 39 mm RCA: 12.0 × 42 mm | No | Yes | No | LITA–LAD RCA down-sizing |
| G | Male | 56 | 65 | 9 | 42 | LMT: 16.5 × 31 mm RCA: 10.0 × 37 mm, 7.0 × 17 mm | No | Yes | AMI | LITA–LAD RCA down-sizing |
| 36 (13, 56) | 59 (18, 76) | 12 (4, 40) | 108 (37, 134) |
| Patient | CFR | FFR | Anastomotic Site Stenosis | LVEF (%) | LV Wall Motion Abnormalities | ||||
|---|---|---|---|---|---|---|---|---|---|
| Pre-CABG | Post-CABG | Pre-CABG | Post-CABG | Pre-CABG | Post-CABG | Pre-CABG | Post-CABG | ||
| A | LAD: 1.2 RCA: 2.3 | LAD: 3.0 RCA: 2.6 | LAD: 0.86 RCA: 0.88 | LAD: 0.87 RCA: 0.88 | No | 64 | 70 | Anterior septum | No |
| B | LAD: 1.9 | LAD: 2.7 | LAD: 0.56 | LAD: 0.81 | No | 62 | 60 | Anterior septum | Anterior septum |
| C | LAD: 1.6 | LAD: 3.1 | LAD: 0.59 | LAD: 0.82 | No | 68 | 75 | Septum; Apical region | No |
| D | LAD: 1.0 | LAD: 2.4 | LAD: 0.85 | No | 64 | 63 | Anterior septum; Apical region | No | |
| E | LAD: 1.6 RCA: 1.3 | LAD: 2.7 RCA: 3.4 | LAD: 0.65 RCA: 0.95 | LAD: 0.94 RCA: 0.85 | No | 70 | 74 | Anterior septum; Apical region | No |
| F | LAD: 1.3 RCA: 1.2 | LAD: 2.5 RCA: 2.5 | LAD: 0.94 RCA: 0.93 | LAD: 0.96 RCA: 0.85 | No | 69 | 72 | Anterior-lateral wall; Septum | No |
| G | LAD: 1.3 RCA: 1.3 | LAD: 2.1 RCA: 2.6 | LAD: 0.84 RCA: 0.94 | No | AMI occurred one day after CAG | 46 | Anterior septum; Apical region | Diffuse decrease in wall motion | |
| Mean | LAD: 1.41 ± 0.30 RCA: 1.53 ± 0.52 | LAD: 2.64 ± 0.35 * RCA: 2.78 ± 0.42 ** | LAD: 0.7 ± 0.16 RCA: 0.9 ± 0.03 | LAD: 0.86 ± 0.05 † RCA: 0.88 ± 0.04 †† | 66.1 ± 3.3 | 65.7 ± 10.3 | |||
| Patient | Latest CAG Findings | Current Medications | Symptoms | Exercise Limitation |
|---|---|---|---|---|
| A | LITA–LAD patency good LAD AN occluded RCA AN: 6.0 × 12 mm | Aspirin | No | E |
| B | LITA–LAD patency good LAD AN outlet 75% LS | Aspirin, Candesartan | No | E |
| C | LITA–LAD patency good LAD AN occluded RCA segmental stenosis | Aspirin, Candesartan | No | E |
| D | LITA–LAD patency good LAD AN occluded LCx AN regressed RCA segmental stenosis | Aspirin, Candesartan | No | E |
| E | LITA–LAD patency good LAD AN occluded RCA AN: 6.2 × 15 mm | Aspirin, Candesartan | No | E |
| F | LITA–LAD patency good LAD AN occluded LCx arise from AN RCA AN: 8.8 × 12 mm | Warfarin, Aspirin, | No | E (Restricted from contact sports) |
| G | LITA–LAD patency good LMT AN occluded LCx segmental stenosis RCA AN 5.4 × 12, 4.2 × 11, and 5.2 × 11 mm | Aspirin, Enalapril, Carvedilol | No | D |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Watanabe, M.; Fukazawa, R.; Kamisago, M.; Ohkubo, T.; Abe, M.; Ochi, M.; Nitta, T.; Ishii, Y.; Ogawa, S.; Itoh, Y. Prognosis of Coronary Artery Bypass Grafting in Preschool-Aged Patients with Myocardial Ischemia Due to Giant Aneurysm of Kawasaki Disease. J. Clin. Med. 2022, 11, 1421. https://doi.org/10.3390/jcm11051421
Watanabe M, Fukazawa R, Kamisago M, Ohkubo T, Abe M, Ochi M, Nitta T, Ishii Y, Ogawa S, Itoh Y. Prognosis of Coronary Artery Bypass Grafting in Preschool-Aged Patients with Myocardial Ischemia Due to Giant Aneurysm of Kawasaki Disease. Journal of Clinical Medicine. 2022; 11(5):1421. https://doi.org/10.3390/jcm11051421
Chicago/Turabian StyleWatanabe, Makoto, Ryuji Fukazawa, Mitsuhiro Kamisago, Takashi Ohkubo, Masanori Abe, Masami Ochi, Takashi Nitta, Yohsuke Ishii, Shunichi Ogawa, and Yasuhiko Itoh. 2022. "Prognosis of Coronary Artery Bypass Grafting in Preschool-Aged Patients with Myocardial Ischemia Due to Giant Aneurysm of Kawasaki Disease" Journal of Clinical Medicine 11, no. 5: 1421. https://doi.org/10.3390/jcm11051421






