Thoracic Curve Correction Ratio: An Objective Measure to Guide against Overcorrection of a Main Thoracic Curve in the Setting of a Structural Proximal Thoracic Curve
Abstract
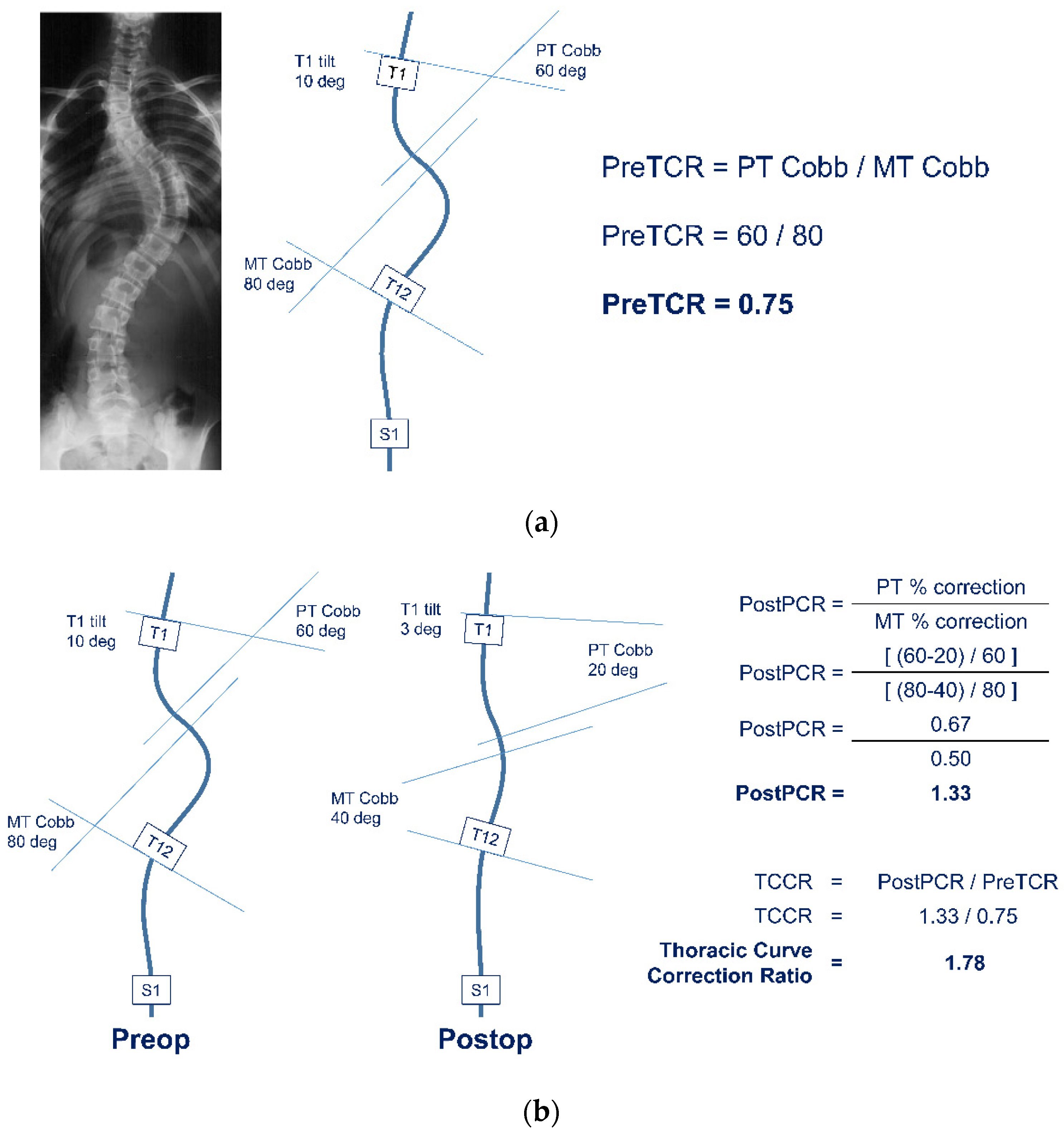
:1. Introduction
2. Materials and Methods
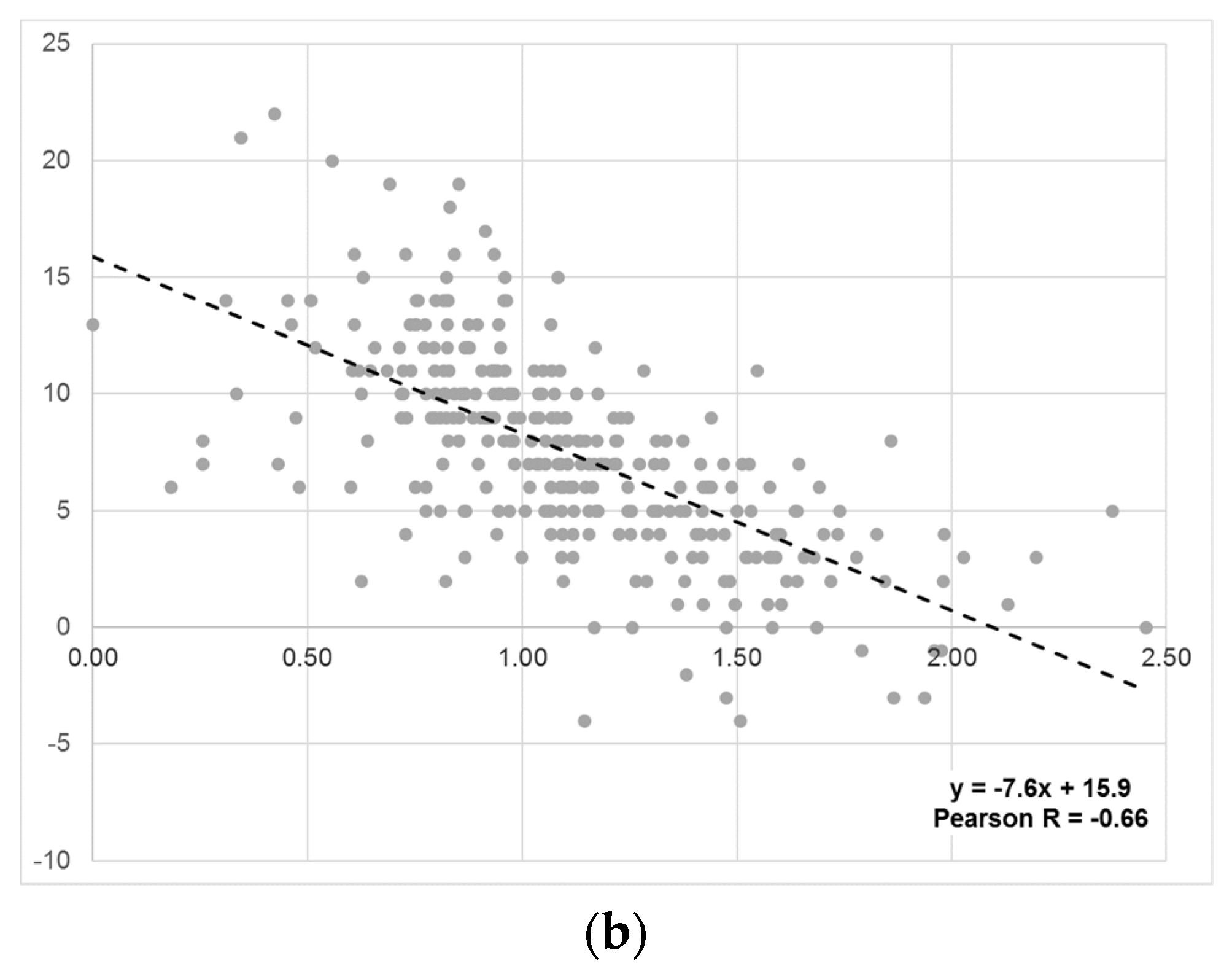
3. Results
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ponseti, I.V.; Friedman, B. Prognosis in idiopathic scoliosis. J. Bone Jt. Surg. Am. 1950, 32, 381–395. [Google Scholar] [CrossRef] [Green Version]
- Winter, R.B. The idiopathic double thoracic curve pattern. Its recognition and surgical management. Spine 1989, 14, 1287–1292. [Google Scholar] [CrossRef] [PubMed]
- Lenke, L.G.; Bridwell, K.H.; O’Brien, M.F.; Baldus, C.; Blanke, K. Recognition and treatment of the proximal thoracic curve in adolescent idiopathic scoliosis treated with Cotrel-Dubousset instrumentation. Spine 1994, 19, 1589–1597. [Google Scholar] [CrossRef] [PubMed]
- Suk, S.I.; Kim, W.J.; Lee, C.S.; Lee, S.M.; Kim, J.H.; Chung, E.R.; Lee, J.H. Indications of proximal thoracic curve fusion in thoracic adolescent idiopathic scoliosis: Recognition and treatment of double thoracic curve pattern in adolescent idiopathic scoliosis treated with segmental instrumentation. Spine 2000, 25, 2342–2349. [Google Scholar] [CrossRef] [PubMed]
- Kuklo, T.R.; Lenke, L.G.; Graham, E.J.; Won, D.S.; Sweet, F.A.; Blanke, K.M.; Bridwell, K.H. Correlation of radiographic, clinical, and patient assessment of shoulder balance following fusion versus nonfusion of the proximal thoracic curve in adolescent idiopathic scoliosis. Spine 2002, 27, 2013–2020. [Google Scholar] [CrossRef] [PubMed]
- Yagi, M.; Takemitsu, M.; Machida, M. Clavicle chest cage angle difference (CCAD): A novel predictor of postoperative shoulder imbalance in patients with adolescent idiopathic scoliosis. Spine 2013, 38, E705–E712. [Google Scholar] [CrossRef] [PubMed]
- Smyrnis, P.N.; Sekouris, N.; Papadopoulos, G. Surgical assessment of the proximal thoracic curve in adolescent idiopathic scoliosis. Eur. Spine J. 2009, 18, 522–530. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lenke, L.G.; Betz, R.R.; Harms, J.; Bridwell, K.H.; Clements, D.H.; Lowe, T.G.; Blanke, K. Adolescent idiopathic scoliosis: A new classification to determine extent of spinal arthrodesis. J. Bone Jt. Surg. Am. 2001, 83, 1169–1181. [Google Scholar] [CrossRef]
- Qiu, X.S.; Ma, W.W.; Li, W.G.; Wang, B.; Yu, Y.; Zhu, Z.Z.; Qian, B.P.; Zhu, F.; Sun, X.; Ng, B.K.; et al. Discrepancy between radiographic shoulder balance and cosmetic shoulder balance in adolescent idiopathic scoliosis patients with double thoracic curve. Eur. Spine J. 2009, 18, 45–51. [Google Scholar] [CrossRef] [Green Version]
- Ilharreborde, B.; Even, J.; Lefevre, Y.; Fitoussi, F.; Presedo, A.; Souchet, P.; Penneçot, G.F.; Mazda, K. How to determine the upper level of instrumentation in Lenke types 1 and 2 adolescent idiopathic scoliosis: A prospective study of 132 patients. J. Pediatr. Orthop. 2008, 28, 733–739. [Google Scholar] [CrossRef] [PubMed]
- Amir, D.; Yaszay, B.; Bartley, C.E.; Bastrom, T.P.; Newton, P.O. Does Leveling the Upper Thoracic Spine Have Any Impact on Postoperative Clinical Shoulder Balance in Lenke 1 and 2 Patients? Spine 2016, 41, 1122–1127. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chang, D.G.; Kim, J.H.; Kim, S.S.; Lim, D.J.; Ha, K.Y.; Suk, S.I. How to Improve Shoulder Balance in the Surgical Correction of Double Thoracic Adolescent Idiopathic Scoliosis. Spine 2014, 39, E1359–E1367. [Google Scholar] [CrossRef] [PubMed]
- Sielatycki, J.A.; Cerpa, M.; Beauchamp, E.C.; Shimizu, T.; Wei, C.; Pongmanee, S.; Wang, H.; Xue, R.; Zhou, R.; Liu, X.; et al. The Amount of Relative Curve Correction Is More Important Than Upper Instrumented Vertebra Selection for Ensuring Postoperative Shoulder Balance in Lenke Type 1 and Type 2 Adolescent Idiopathic Scoliosis. Spine 2019, 44, E1031–E1037. [Google Scholar] [CrossRef] [PubMed]
- Lee, C.S.; Park, S.; Lee, D.H.; Hwang, C.J.; Cho, J.H.; Park, J.W.; Park, K.B. Is the Combination of Convex Compression for the Proximal Thoracic Curve and Concave Distraction for the Main Thoracic Curve Using Separate-rod Derotation Effective for Correcting Shoulder Balance and Thoracic Kyphosis? Clin. Orthop. Relat. Res. 2021, 479, 1347–1356. [Google Scholar] [CrossRef] [PubMed]
- Koller, H.; Meier, O.; McClung, A.; Hitzl, W.; Mayer, M.; Sucato, D. Parameters leading to a successful radiographic outcome following surgical treatment for Lenke 2 curves. Eur. Spine J. 2015, 24, 1490–1501. [Google Scholar] [CrossRef] [PubMed]
- Namikawa, T.; Matsumura, A.; Kato, M.; Hayashi, K.; Nakamura, H. Radiological assessment of shoulder balance following posterior spinal fusion for thoracic adolescent idiopathic scoliosis. Scoliosis 2015, 10 (Suppl. S2), S18. [Google Scholar] [CrossRef] [PubMed]
- Yang, S.; Feuchtbaum, E.; Werner, B.C.; Cho, W.; Reddi, V.; Arlet, V. Does anterior shoulder balance in adolescent idiopathic scoliosis correlate with posterior shoulder balance clinically and radiographically? Eur. Spine J. 2012, 21, 1978–1983. [Google Scholar] [CrossRef] [PubMed] [Green Version]


| Variable | n | (%) | |||
|---|---|---|---|---|---|
| Gender | |||||
| Male | 98 | (32) | |||
| Female | 207 | (68) | |||
| Curve Type | |||||
| Lenke 2A | 213 | (70) | |||
| Lenke 2B | 57 | (19) | |||
| Lenke 2C | 35 | (11) | |||
| n | Mean | ± | SD | (Range) | |
| Age (years) | 305 | 14.5 | ± | 2.2 | (10.1–21.5) |
| Body Mass Index | 260 | 22.0 | ± | 4.1 | (13.1–41.8) |
| Preop PT Cobb | 305 | 38.9 | ± | 8.6 | (25.0–86.0) |
| Preop MT Cobb | 305 | 59.1 | ± | 11.5 | (36.0–108.0) |
| Follow-up (years) | 305 | 2.3 | ± | 0.4 | (1.9–4.4) |
| Final PT Cobb | 305 | 21.0 | ± | 7.4 | (2.0–55.0) |
| % PT Correction | 305 | 46 | ± | 16 | (0–94) |
| Final MT Cobb | 305 | 21.2 | ± | 7.8 | (3.0–49.0) |
| % MT Correction | 305 | 64 | ± | 13 | (12–95) |
| Variable | n | Correlation with TCCR | |
|---|---|---|---|
| Pearson R | p value | ||
| Change in SRS-24 Self Image | 234 | 0.11 | 0.08 |
| Change in SRS-24 Function | 233 | 0.08 | 0.20 |
| SRS-24 Satisfaction | 234 | 0.07 | 0.25 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Landrum, M.R.; Milby, A.H.; Yaszay, B.; Parent, S.; Nelson, S.E.; Pahys, J.M.; Samdani, A.F.; Capraro, A.C.; Flynn, J.M.; Cahill, P.J.; et al. Thoracic Curve Correction Ratio: An Objective Measure to Guide against Overcorrection of a Main Thoracic Curve in the Setting of a Structural Proximal Thoracic Curve. J. Clin. Med. 2022, 11, 1545. https://doi.org/10.3390/jcm11061545
Landrum MR, Milby AH, Yaszay B, Parent S, Nelson SE, Pahys JM, Samdani AF, Capraro AC, Flynn JM, Cahill PJ, et al. Thoracic Curve Correction Ratio: An Objective Measure to Guide against Overcorrection of a Main Thoracic Curve in the Setting of a Structural Proximal Thoracic Curve. Journal of Clinical Medicine. 2022; 11(6):1545. https://doi.org/10.3390/jcm11061545
Chicago/Turabian StyleLandrum, Matthew R., Andrew H. Milby, Burt Yaszay, Stefan Parent, Susan E. Nelson, Joshua M. Pahys, Amer F. Samdani, Anthony C. Capraro, John M. Flynn, Patrick J. Cahill, and et al. 2022. "Thoracic Curve Correction Ratio: An Objective Measure to Guide against Overcorrection of a Main Thoracic Curve in the Setting of a Structural Proximal Thoracic Curve" Journal of Clinical Medicine 11, no. 6: 1545. https://doi.org/10.3390/jcm11061545






