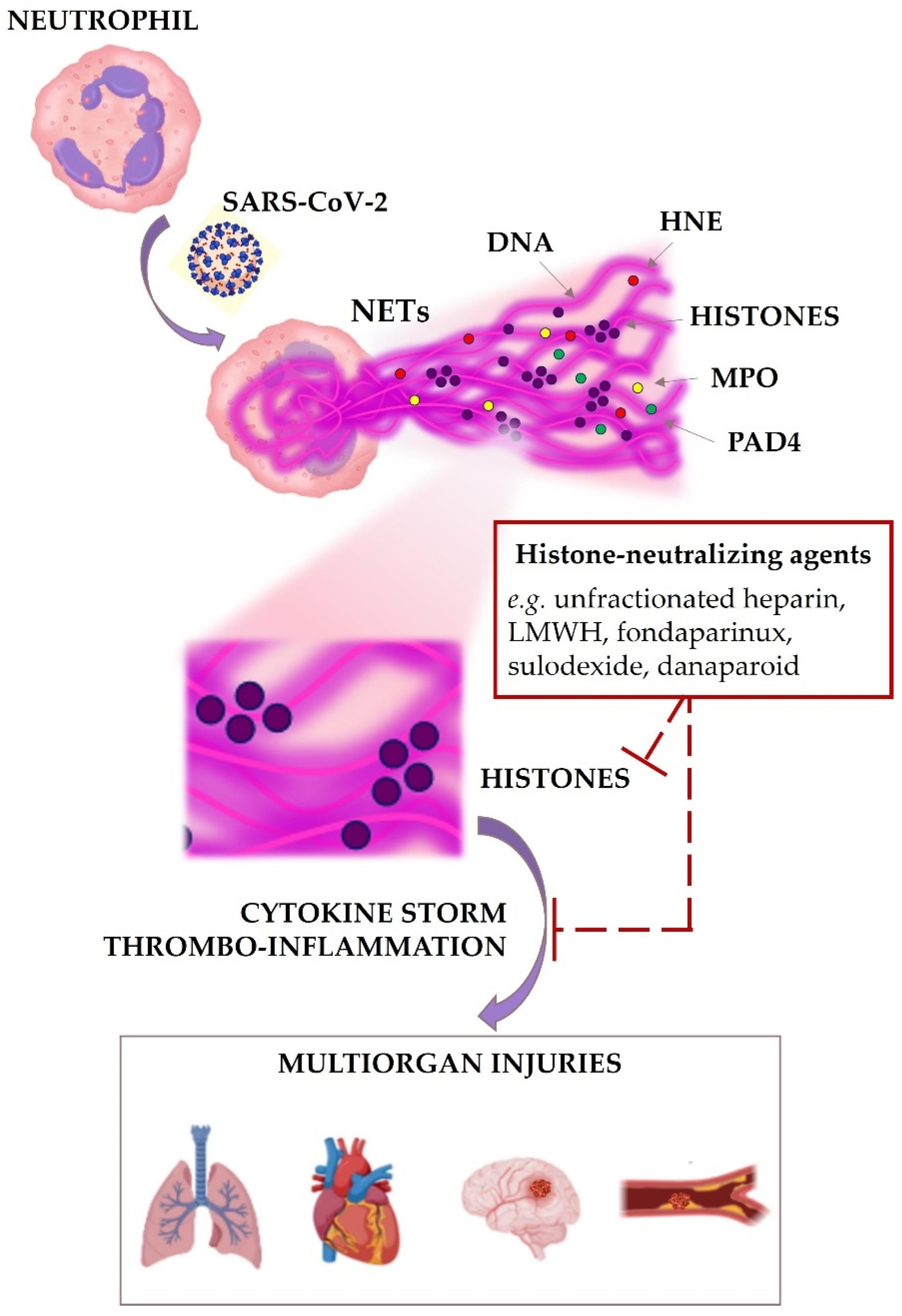
Do Circulating Histones Represent the Missing Link among COVID-19 Infection and Multiorgan Injuries, Microvascular Coagulopathy and Systemic Hyperinflammation?
Abstract
:Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Bonaventura, A.; Vecchiè, A.; Abbate, A.; Montecucco, F. Neutrophil extracellular traps and cardiovascular diseases: An update. Cells 2020, 9, 231. [Google Scholar]
- Cavalier, E.; Guiot, J.; Lechner, K.; Dutsch, A.; Eccleston, M.; Herzog, M.; Bygott, T.; Schomburg, A.; Kelly, T.; Holdenrieder, S. Circulating nucleosome as potential markers to monitor COVID-19 disease progression. Front. Mol. Biosci. 2021, 8, 600881. [Google Scholar] [PubMed]
- Blanch-Ruiz, M.A.; Ortega-Luna, R.; Martina-Cuesta, M.A.; Alvarez, A. The neutrophil secretome as a crucial link between inflammation and thrombosis. Int. J. Mol. Sci. 2021, 22, 4170. [Google Scholar] [PubMed]
- Zuo, Y.; Yalavarthi, S.; Shi, H.; Gockman, K.; Zuo, M.; Madison, J.A.; Blair, C.; Weber, A.; Barnes, B.J.; Egeblad, M.; et al. Neutrophil extracellular traps in COVID-19. JCI Insight 2020, 5, e138999. [Google Scholar]
- Huckriede, J.; Anderberg, S.B.; Morales, A.; de Vries, F.; Hultström, M.; Bergqvist, A.; Ortiz-Pérez, J.T.; Sels, J.W.; Wichapong, K.; Lipcsey, M.; et al. Evolution of NETosis markers and DAMPs have prognostic value in critically ill COVID-19 patients. Sci. Rep. 2021, 11, 15701. [Google Scholar]
- Katsoularis, I.; Fonseca-Rodriguez, O.; Farrington, P.; Lindmark, K.; Fors Connolly, A.-M. Risk of acute myocardial infarction and ischaemic stroke following COVID-19 in Sweden: A self-controlled case series and matched cohort study. Lancet 2021, 398, 599–607. [Google Scholar]
- Lubrano, V.; Balza, S. Cardiovascular risk in COVID-19 infection. Am. J. Cardiovasc. Dis. 2020, 10, 284–293. [Google Scholar]
- Mafham, M.; Baigent, C. What is the association of COVID-19 with heart attacks and strokes? Lancet 2021, 398, 561–563. [Google Scholar]
- Al-Kindi, S.; Zidar, D.A. COVID-lateral damage: Cardiovascular manifestations of SARS-CoV-2 infection. Transl. Res. 2021, 41, S1931–S5244. [Google Scholar] [CrossRef]
- Spyropoulos, A.C.; Bonaca, M.P. Studying the coagulopathy of COVID-19. Lance 2022, 399, 118–119. [Google Scholar]
- Gorog, D.A.; Storey, R.F.; Gurbel, P.A.; Tantry, U.S.; Berger, J.S.; Chan, M.Y.; Duerschmied, D.; Smyth, S.S.; Parker, W.A.; Ajjan, R.A.; et al. Current and novel biomarkers of thrombotic risk in COVID-19: A consensus statement from the International COVID-19 Thrombosis Biomarkers Colloquium. Nat. Rev. Cardiol. 2022, 1–21. [Google Scholar] [CrossRef]
- Henry, B.M.; Santos de Oliveira, M.H.; Benoit, S.; Plebani, M.; Lippi, G. Hematologic, biochemical and immune biomarker abnormalities associated with severe illness and mortality in coronavirus disease 2019 (COVID-19): A meta-analysis. Clin. Chem. Lab. Med. 2020, 58, 1021–1028. [Google Scholar] [PubMed] [Green Version]
- Ng, H.; Havervall, S.; Rosell, A.; Aguilera, K.; Parv, K.; Von Meijenfeldt, F.A.; Lisman, T.; Mackman, N.; Thålin, C.; Phillipson, M. Circulating markers of neutrophil extracellular traps are of prognostic value in patients with COVID-19. Arterioscler. Thromb. Vasc. Biol. 2021, 41, 988–994. [Google Scholar] [PubMed]
- Tahir Huyut, M.; Huyut, Z.; Ilkbahar, F.; Mertoglu, C. What is the impact and efficacy of routine immunological, biochemical and hematological biomarkers as predictors of COVID-19 mortality? Int. Immunopharmacol. 2022, 105, 1085452. [Google Scholar]
- Calvet, J.; Berenguer-Llergo, A.; Gay, M.; Massanella, M.; Domingo, P.; Llop, M.; Sánchez-Jiménez, E.; Arévalo, M.; Carrillo, J.; Albiñana, N.; et al. Biomarker candidates for progression and clinical management of COVID-19 associated pneumonia at time of admission. Sci. Rep. 2022, 12, 640. [Google Scholar]
- Ackermann, M.; Anders, H.J.; Bilyy, R.; Bowlin, G.L.; Daniel, C.; De Lorenzo, R.; Egeblad, M.; Henneck, T.; Hidalgo, A.; Hoffmann, M.; et al. Patients with COVID-19: In the dark-NETs of neutrophils. Cell Death Differ. 2021, 28, 3125–3139. [Google Scholar]
- Mutua, V.; Gershwin, L.J. A review of neutrophil extracellular traps (NETs) in disease: Potential anti-NETs therapeutics. Clin. Rev. Allergy Immunol. 2021, 61, 194–211. [Google Scholar]
- Kumar, S.; Payal, N.; Kumar Srivastava, V.; Kaushik, S.; Saxena, J.; Jyoti, A. Neutrophil extracellular traps and organ dysfunction in sepsis. Clin. Chim. Acta 2021, 523, 152–162. [Google Scholar]
- Wolach, O.; Martinod, K. Casting NET on cancer: The multiple roles for neutrophil extracellular traps in cancer. Curr. Opin. Hematol. 2022, 29, 53–62. [Google Scholar]
- Perez-Olivares, L.; Soehnlein, O. Contemporary lifestyle and neutrophil extracellular traps: An emerging link in atherosclerosis disease. Cells 2021, 10, 1985. [Google Scholar]
- Scieszka, D.; Lin, Y.-H.; Li, W.; Choudhury, S.; Yu, Y.; Freire, M. NETome: The molecular characterization of neutrophil extracellular traps (NETs). Cold Spring Harb. 2020. [Google Scholar] [CrossRef]
- Murao, A.; Aziz, M.; Wang, H.; Brenner, M.; Wang, P. Release mechanisms of major DAMPs. Apoptosis 2021, 26, 152–162. [Google Scholar] [PubMed]
- Moiana, M.; Aranda, F.; de Larranaga, G. A focus on the roles of histones in health and diseases. Clin. Biochem. 2021, 94, 12–19. [Google Scholar] [PubMed]
- Blasco, A.; Coronado, M.J.; Hernández-Terciado, F.; Martín, P.; Royuela, A.; Ramil, E.; García, D.; Goicolea, J.; Del Trigo, M.; Ortega, J.; et al. Assessment of neutrophil extracellular traps in coronavirus thrombus of a case series of patients with COVID-19 and myocardial infarction. JAMA Cardiol. 2020, 6, 469–474. [Google Scholar]
- Shah, M.; He, Z.; Rauf, A.; Beikoghli Kalkhoran, S.; Heiestad, C.M.; Stensløkken, K.O.; Parish, C.R.; Soehnlein, O.; Arjun, S.; Davidson, S.M.; et al. Extracellular histones are target in myocardial ischaemia-reperfusion injury. Cardiovasc. Res. 2021, 118, cvab139. [Google Scholar] [CrossRef]
- Li, Y.; Liu, Z.; Shi, X.; Tong, H.; Su, L. Prognostic value of plasma exosomal levels of histone H3 protein in patients with heat stroke. Exp. Ther. Med. 2021, 22, 922. [Google Scholar]
- Hofbauer, T.M.; Ondracek, A.S.; Mangold, A.; Scherz, T.; Nechvile, J.; Seidl, V.; Brostjan, C.; Lang, I.M. Neutrophil extracellular traps induce MCP-1 at the culprit site in ST-segment elevation myocardial infarction. Front. Cell Dev. Biol. 2020, 8, 564169. [Google Scholar]
- Hally, K.E.; Parker, O.M.; Brunton-O’Sullivan, M.M.; Harding, S.A.; Larsen, P.D. Linking neutrophil extracellular traps and platelet activation: A composite biomarker score for predicting outcomes after acute myocardial infarction. Thromb. Haemost. 2021, 121, 1637–1649. [Google Scholar]
- Shaw, R.J.; Abrams, S.T.; Austin, J.; Taylor, J.M.; Lane, S.; Dutt, T.; Downey, C.; Du, M.; Turtle, L.; Baillie, J.K.; et al. Circulating histones play a central role in COVID-19-associated coagulopathy and mortality. Haematologica 2021, 106, 2493–2498. [Google Scholar]
- Hammarsten, O.; Ljungqvist, P.; Redfors, B.; Wernbom, M.; Widing, H.; Lindahl, B.; Salahuddin, S.; Sammantar, R.; Jha, S.; Ravn-Fisher, A.; et al. The ratio of cardiac troponin T to troponin I may indicate non-necrotic troponin release among COVID-19 patients. Clin. Chim. Acta 2022, 527, 33–37. [Google Scholar]
- Silk, E.; Zhao, H.; Weng, H.; Ma, D. The role of extracellular histone in organ injury. Cell Death Dis. 2017, 8, e2812. [Google Scholar] [PubMed] [Green Version]
- Siddiq, M.M.; Chan, A.T.; Miorin, L.; Yadaw, A.S.; Beaumont, K.G.; Kehrer, T.; Cupic, A.; White, K.M.; Tolentino, R.E.; Hu, B.; et al. Functional effects of cardiomyocyte injury in COVID-19. J. Virol. 2022, 96, e0106321. [Google Scholar] [PubMed]
- Kim, C.; Aronow, W.S. COVID-19, cardiovascular diseases and cardiac troponins. Future Cardiol. 2022, 18, 135–142. [Google Scholar] [PubMed]
- Bouchard, B.A.; Colovos, C.; Lawson, M.A.; Osborn, Z.T.; Sackheim, A.M.; Mould, K.J.; Janssen, W.J.; Cohen, M.J.; Majumdar, D.; Freeman, K. Increased histone-DNA complexes and endothelial-dependent thrombin generation in severe COVID-19. Vascul. Pharmacol. 2021, 142, 106950. [Google Scholar] [PubMed]
- Huckriede, J.; Vries, F.D.; Hultström, M.; Wichapong, K.; Reutelingsperger, C.; Lipcsey, M.; Garcia de Frutos, P.; Frithiof, R.; Nicolaes, G.A. Histone H3 cleavage in severe COVID-19 ICU patients. Front. Cell. Infect. Microbiol. 2021, 11, 694186. [Google Scholar]
- Santocki, M.; Kolaczkowska, E. On neutrophil extracellular trap (NET) removal: What we know thus far and why so little. Cells 2020, 9, 2079. [Google Scholar]
- Bikdeli, B.; Madhavan, M.V.; Gupta, A.; Jimenez, D.; Burton, J.R.; Der Nigoghossian, C.; Chuich, T.; Nouri, S.N.; Dreyfus, I.; Driggin, E.; et al. Pharmacological agents targeting thromboinflammation in COVID-19: Review and implications for future research. Thromb. Haemost. 2020, 120, 1004–1024. [Google Scholar]
- Lippi, G.; Henry, B.M.; Favaloro, E.J. The benefits of heparin use in COVID-19: Pleiotropic antiviral activity beyond anticoagulant and anti-Inflammatory. Semin. Thromb. Hemost. 2022. [Google Scholar] [CrossRef]
- Buijsers, B.; Yanginlar, C.; Maciej-Hulme, M.L.; de Mast, Q.; van der Vlag, J. Beneficial non-anticoagulant mechanisms underlying heparin treatment of COVID-19 patients. EBioMedicine 2020, 59, 102969. [Google Scholar]
- Schulman, S.; Harenberg, J. Anticoagulant treatment of COVID-19 as early as possible- Sulodexide and perspective. Thromb. Haemost. 2021, 121, 849–853. [Google Scholar]
- Iba, T.; Hashiguchi, N.; Nagaoka, I.; Tabe, Y.; Kadota, K.; Sato, K. Heparins attenuated histone-mediate cytotoxicity in vitro and improved the survival in a rat model of histone-induced organ dysfunction. Intensive Care Med. Exp. 2015, 3, 36. [Google Scholar] [PubMed] [Green Version]
- Ginsburg, I.; Fibach, E. Polycations and polyanions in SARS-CoV-2 infection. Med. Hypotheses 2021, 146, 110470. [Google Scholar] [PubMed]
- Gozzo, L.; Viale, P.; Longo, L.; Vitale, D.C.; Drago, F. The potential role of heparin in patients with COVID-19: Beyond the anticoagulant effect. A review. Front. Pharmacol. 2020, 11, 1307. [Google Scholar] [PubMed]
- Jamil, Z.; Khan, A.A.; Khgalid, S.; Asghar, M.; Muhammad, K.; Waheed, Y. Beneficial effects of anticoagulants on the clinical outcomes of COVID-19 patients. Antibiotics 2021, 10, 1394. [Google Scholar]
- Shi, H.; Gandhi, A.A.; Smith, S.A.; Wang, Q.; Chiang, D.; Yalavarthi, S.; Ali, R.A.; Liu, C.; Sule, G.; Tsou, P.S.; et al. Endothelium-protective, histone-neutralizing properties of polyanionic agent defibrotide. JCI Insight 2021, 6, e149149. [Google Scholar]
- Al-Kuraishy, H.M.; Al-Gareeb, A.I.; Akeel Al-Hussaniy, H.A.; Hadi Al-Harcan, N.A.; Alexiou, A.; El-Saber Batiha, G. Neutrophil extracellular traps (NETs) and COVID-19: A new frontier for therapeutic modality. Int. Immunopharmacol. 2022, 104, 108516. [Google Scholar]
- Daviet, F.; Guervilly, C.; Baldesi, O.; Bernard-Guervilly, F.; Pilarczyk, E.; Genin, A.; Lefebvre, L.; Forel, J.M.; Papazian, L.; Camoin-Jau, L. Heparin-induced thrombocytopenia in severe COVID-19. Circulation 2020, 142, 1875–1877. [Google Scholar]
- Magnani, H.N. Rationale for the role of heparin and related GAG antithrombotic in COVID-19 infection. Clin. Appl. Thromb. Hemost. 2021, 27, 1–26. [Google Scholar]
- Hogwood, H.; Pitchford, S.; Muloy, B.; Page, C.; Gray, E. Heparin and non-anticoagulant heparin attenuate histone-induced inflammatory responses in whole blood. PLoS ONE 2020, 15, e0233644. [Google Scholar]
- Francischetti, I.M.; Toomer, K.; Zhang, Y.; Jani, J.; Siddiqui, Z.; Brotman, D.J.; Hooper, J.E.; Kickler, T.S. Upregulation of pulmonary tissue factor, loss of thrombomodulin and immunothrombosis in SARS-CoV-2 infection. EclinicalMedicine 2021, 39, 101069. [Google Scholar]
- Gleeson, E.M.; Rehill, A.M.; Fox, O.W.; Ainle, F.N.; McDonnell, C.J.; Rushe, H.J.; McCluskey, S.; O’Donnell, J.S.; Preston, R.J. Apolipoprotein A-I enhances activated protein C cytoprotective activity. Blood Adv. 2020, 4, 2404–2408. [Google Scholar] [PubMed]
- Li, Y.; Wan, D.; Luo, X.; Song, T.; Wang, Y.; Yu, Q.; Jiang, L.; Liao, R.; Zhao, W.; Su, B. Circulating histones in sepsis: Potential outcome predictors and therapeutic targets. Front. Immunol. 2021, 12, 650184. [Google Scholar] [PubMed]
- Sheng Lim, M.; Mcrae, S. COVID-19 and immunothrombosis: Pathophysiology and therapeutic implications. Crit. Rev. Oncol. Hematol. 2021, 168, 103529. [Google Scholar]
- Elliott, W.; Guda, M.R.; Asuthkar, S.; Teluguakula, N.; Prasad, D.V.; Tsung, A.J.; Velpula, K.K. PAD inhibitors as potential treatment for SARS-CoV-2 immunothrombosis. Biomedicines 2021, 9, 1867. [Google Scholar] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ligi, D.; Maniscalco, R.; Plebani, M.; Lippi, G.; Mannello, F. Do Circulating Histones Represent the Missing Link among COVID-19 Infection and Multiorgan Injuries, Microvascular Coagulopathy and Systemic Hyperinflammation? J. Clin. Med. 2022, 11, 1800. https://doi.org/10.3390/jcm11071800
Ligi D, Maniscalco R, Plebani M, Lippi G, Mannello F. Do Circulating Histones Represent the Missing Link among COVID-19 Infection and Multiorgan Injuries, Microvascular Coagulopathy and Systemic Hyperinflammation? Journal of Clinical Medicine. 2022; 11(7):1800. https://doi.org/10.3390/jcm11071800
Chicago/Turabian StyleLigi, Daniela, Rosanna Maniscalco, Mario Plebani, Giuseppe Lippi, and Ferdinando Mannello. 2022. "Do Circulating Histones Represent the Missing Link among COVID-19 Infection and Multiorgan Injuries, Microvascular Coagulopathy and Systemic Hyperinflammation?" Journal of Clinical Medicine 11, no. 7: 1800. https://doi.org/10.3390/jcm11071800
APA StyleLigi, D., Maniscalco, R., Plebani, M., Lippi, G., & Mannello, F. (2022). Do Circulating Histones Represent the Missing Link among COVID-19 Infection and Multiorgan Injuries, Microvascular Coagulopathy and Systemic Hyperinflammation? Journal of Clinical Medicine, 11(7), 1800. https://doi.org/10.3390/jcm11071800









