Prevention of Abdominal Bulging Using Onlay Dermal Autografts from Discarded Zone IV TRAM Flap Tissue
Abstract
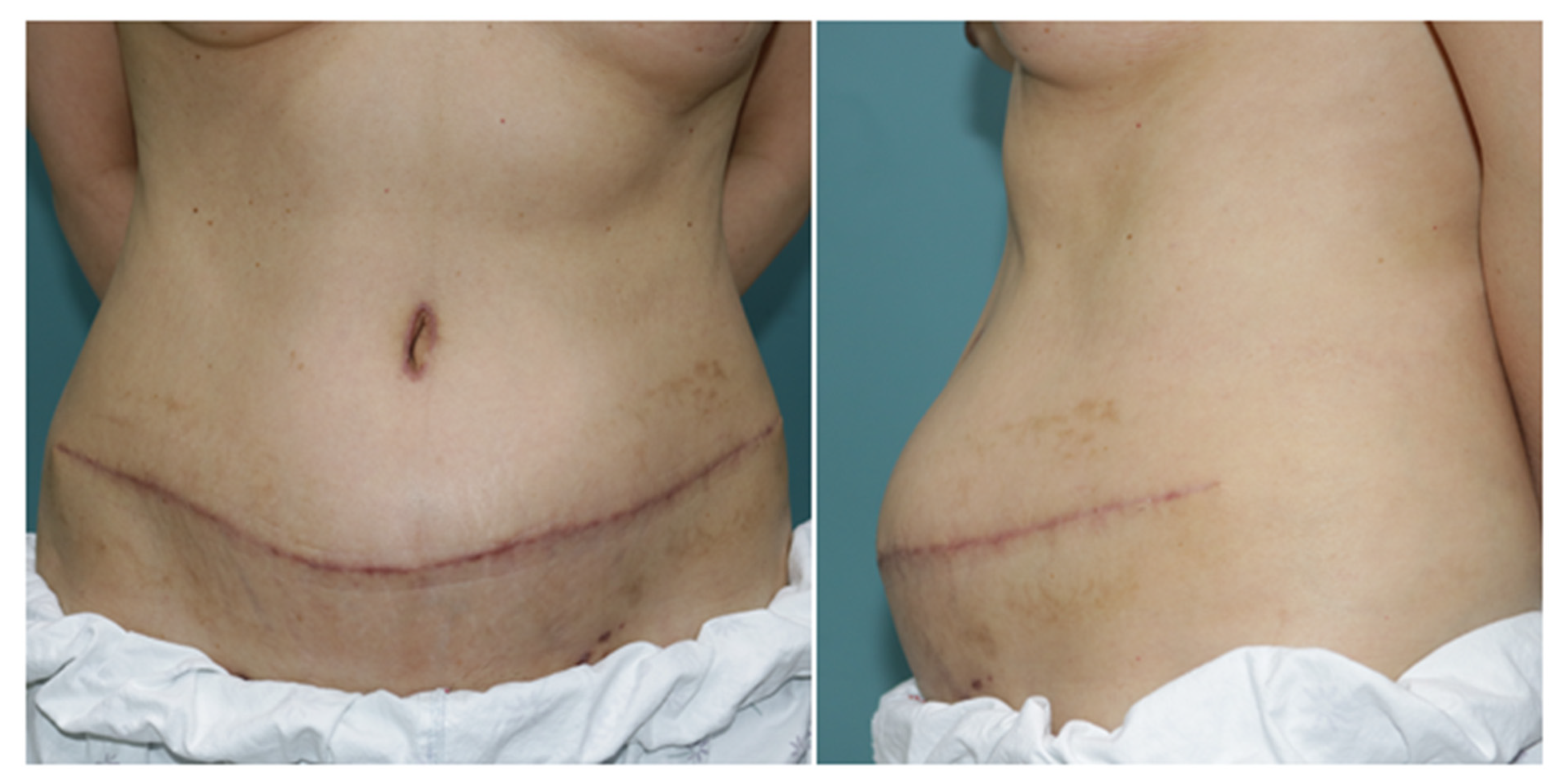
:1. Introduction
2. Materials and Methods
2.1. Patients and Clinical Data Collection
2.2. Surgical Technique
2.3. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Nahabedian, M.Y.; Patel, K. Autologous flap breast reconstruction: Surgical algorithm and patient selection. J. Surg. Oncol. 2016, 113, 865–874. [Google Scholar] [CrossRef] [PubMed]
- Scheflan, M.; Hartrampf, C.R.; Black, P.W. Breast reconstruction with a transverse abdominal island flap. Plast. Reconstr. Surg. 1982, 69, 908–909. [Google Scholar] [PubMed]
- Holmström, H. The free abdominoplasty flap and its use in breast reconstruction. An experimental study and clinical case report. Scand J. Plast. Reconstr. Surg. 1979, 13, 423–427. [Google Scholar] [CrossRef]
- Gandolfo, E.A. Breast reconstruction with a lower abdominal myocutaneous flap. Br. J. Plast. Surg. 1982, 35, 452–457. [Google Scholar] [CrossRef]
- Wan, D.C.; Tseng, C.Y.; Anderson-Dam, J.; Dalio, A.L.; Crisera, C.A.; Festekjian, J.H. Inclusion of mesh in donor-site repair of free TRAM and muscle-sparing free TRAM flaps yields rates of abdominal complications comparable to those of DIEP flap reconstruction. Plast. Reconstr. Surg. 2010, 126, 367–374. [Google Scholar] [CrossRef] [PubMed]
- Veiga, D.F.; Neto, M.S.; Garcia, E.B.; Filho, J.V.; Juliano, Y.; Ferreira, L.M.; Rocha, J.L. Evaluations of the aesthetic results and patient satisfaction with the late pedicled TRAM flap breast reconstruction. Ann. Plast. Surg. 2002, 48, 515–520. [Google Scholar] [CrossRef]
- Ascherman, J.A.; Seruya, M.; Bartsich, S.A. Abdominal wall morbidity following unilateral and bilateral breast reconstruction with pedicled TRAM flaps: An outcomes analysis of 117 consecutive patients. Plast. Reconstr. Surg. 2008, 121, 1–8. [Google Scholar] [CrossRef]
- Suominen, S.; Asko-Seljavaara, S.; von Smitten, K.; Ahovuo, J.; Sainio, P.; Alaranta, H. Sequelae in the abdominal wall after pedicled or free TRAM flap surgery. Ann. Plast. Surg. 1996, 36, 629–636. [Google Scholar] [CrossRef]
- Edsander-Nord, A.; Jurell, G.; Wickman, M. Donor-site morbidity after pedicled or free TRAM flap surgery: A prospective and objective study. Plast. Reconstr. Surg. 1998, 102, 1508–1516. [Google Scholar] [CrossRef]
- Reece, G.P.; Kroll, S.S. Abdominal wall complications. Prevention and treatment. Clin. Plast. Surg. 1998, 25, 235–249. [Google Scholar] [CrossRef]
- Blondeel, N.; Vanderstraeten, G.G.; Monstrey, S.J.; Van Landuyt, K.; Tonnard, P.; Lysens, R.; Boeckx, W.D.; Matton, G. The donor site morbidity of free DIEP flaps and free TRAM flaps for breast reconstruction. Br. J. Plast. Surg. 1997, 50, 322–330. [Google Scholar] [CrossRef]
- Kroll, S.S. Midline fascial preservation in double-pedicle TRAM flap breast reconstruction. Ann. Plast. Surg. 1989, 23, 104–111. [Google Scholar] [CrossRef] [PubMed]
- Nohira, K.; Shintomi, Y.; Hosokawa, M.; Yajima, K.; Sasaki, S.; Yamamoto, Y.; Sugihara, T. TRAM flap breast reconstruction using a fascia-sparing technique. Nihon Geka Gakkai Zasshi 1999, 100, 547–550. [Google Scholar] [PubMed]
- Erni, D.; Harder, Y.D. The dissection of the rectus abdominis myocutaneous flap with complete preservation of the anterior rectus sheath. Br. J. Plast. Surg. 2003, 56, 395–400. [Google Scholar] [CrossRef]
- Hein, K.D.; Morris, D.J.; Goldwyn, R.M.; Kolker, A. Dermal autografts for fascial repair after TRAM flap harvest. Plast. Reconstr. Surg. 1998, 102, 2287–2292. [Google Scholar] [CrossRef]
- Scheflan, M. Rectus abdominis myocutaneous flaps. Plast. Reconstr. Surg. 1983, 72, 737–739. [Google Scholar] [CrossRef]
- Brunbjerg, M.E.; Jensen, T.B.; Christiansen, P.; Overgaard, J.; Engberg Damsgaard, T. Reinforcement of the abdominal wall with acellular dermal matrix or synthetic mesh after breast reconstruction with the pedicled transverse rectus abdominis musculocutaneous flap. A prospective double-blind randomized study. J. Plast. Surg. Hand. Surg. 2021, 55, 202–209. [Google Scholar] [CrossRef]
- Bunkis, J.; Walton, R.L.; Mathes, S.J.; Krizek, T.J.; Vasconez, L.O. Experience with the transverse lower rectus abdominis operation for breast reconstruction. Plast. Reconstr. Surg. 1983, 72, 819–829. [Google Scholar] [CrossRef]
- Kheradmand, A.A.; Novin, N.R.; Omranipour, R. The use of dermal autograft for fascial repair of TRAM flap donor sites. Acta Med. Iran. 2010, 48, 111–116. [Google Scholar]
- Chun, Y.S.; Sinha, I.; Turko, A.; Yueh, J.H.; Lipsitz, S.; Pribaz, J.J.; Lee, B.T. Comparison of morbidity, functional outcome, and satisfaction following bilateral TRAM versus bilateral DIEP flap breast reconstruction. Plast. Reconstr. Surg. 2010, 126, 1133–1141. [Google Scholar] [CrossRef]
- Serletti, J.M. Breast reconstruction with the TRAM flap: Pedicled and free. J. Surg. Oncol. 2006, 94, 532–537. [Google Scholar] [CrossRef] [PubMed]
- Selber, J.C. The robotic DIEP flap. Plast. Reconstr. Surg. 2020, 145, 340–343. [Google Scholar] [CrossRef] [PubMed]
- Ahn, H.C.; Seo, H.J.; Chang, S.; Chang, L.S.; Park, S.O. Technique for the prevention of hernia after pedicled transverse rectus abdominis musculocutaneous flap for breast reconstruction. J. Plast. Reconstr. Aesthet. Surg. 2022, 75, 439–488. [Google Scholar] [CrossRef] [PubMed]
- Bharti, G.; Groves, L.; Sanger, C.; Thompson, J.; David, L.; Marks, M. Minimizing donor-site morbidity following bilateral pedicled TRAM breast reconstruction with the double mesh fold over technique. Ann. Plast. Surg. 2013, 70, 484–487. [Google Scholar] [CrossRef] [PubMed]
- Rietjens, M.; De Lorenzi, F.; Andrea, M.; Petit, J.Y.; Chirappapha, P.; Hamza, A.; Martella, S.; Barbieri, B.; Gottardi, A.; Giuseppe, L. Technique for minimizing donor-site morbidity after pedicled TRAM-flap breast reconstruction: Outcomes by a single surgeon's experience. Plast. Reconstr. Surg. Glob. Open 2015, 3, e476. [Google Scholar] [CrossRef]
- Kim, Y.S.; Lee, W.S.; Park, B.Y.; Choi, M.; Lee, J.H.; Bae, Y.K.; Kim, I.K. Abnormal ultrasonographic findings of acellular dermal matrix in implant-based breast reconstruction: Correlations with histopathology. J. Clin. Med. 2022, 11, 1057. [Google Scholar] [CrossRef]
- Kim, I.K.; Park, S.O.; Chang, H.; Jin, U.S. Inhibition mechanism of acellular dermal matrix on capsule formation in expander-implant breast reconstruction after postmastectomy radiotherapy. Ann. Surg. Oncol. 2018, 25, 2279–2287. [Google Scholar] [CrossRef]
- Uihlein, A., Jr. Use of the cutis graft in plastic operations. Arch. Surg. 1939, 38, 118–130. [Google Scholar] [CrossRef]
- Loewe, O. Ueber hautimplantation an stelle der freien faszienplastik. Muenchener Medizinische Wochenschrift 1913, 24, 1320–1321. [Google Scholar]
- Zienowicz, R.J.; May, J.W., Jr. Hernia prevention and aesthetic contouring of the abdomen following TRAM flap breast reconstruction by the use of polypropylene mesh. Plast. Reconstr. Surg. 1995, 96, 1346–1350. [Google Scholar] [CrossRef]
- Mizgala, C.L.; Hartrampf, C.R., Jr.; Bennett, G.K. Assessment of the abdominal wall after pedicled TRAM flap surgery: 5- to 7-year follow-up of 150 consecutive patients. Plast. Reconstr. Surg. 1994, 93, 988–1002. [Google Scholar] [CrossRef] [PubMed]
- Lejour, M.; Dome, M. Abdominal wall function after rectus abdominis transfer. Plast. Reconstr. Surg. 1991, 87, 1054–1068. [Google Scholar] [CrossRef] [PubMed]
- Erdmann-Sager, J.; Wilkins, E.G.; Pusic, A.L.; Qi, J.; Hamill, J.B.; Kim, H.M.; Guldbrandsen, G.E.; Chun, Y.S. Complications and patient-reported outcomes after abdominally based breast reconstruction: Results of the mastectomy reconstruction outcomes consortium study. Plast. Reconstr. Surg. 2018, 141, 271–281. [Google Scholar] [CrossRef] [PubMed]
- Mennie, J.C.; Mohanna, P.N.; O'Donoghue, J.M.; Rainsbury, R.; Cromwell, D.A. Donor-site hernia repair in abdominal flap breast reconstruction: A population-based cohort study of 7929 patients. Plast. Reconstr. Surg. 2015, 136, 1–9. [Google Scholar] [CrossRef]


| Primary Closure (%) | Dermal Autograft (%) | p | |
|---|---|---|---|
| No. | 41 | 38 | |
| Mean age ± SD | 48.5 ± 7.4 | 47.9 ± 7.5 | 0.759 |
| BMI ± SD | 23.2 ± 3.0 | 25 ± 3.3 | 0.011 † |
| Follow-up period ± SD | 1.24 ± 0.62 | 1.04 ± 0.37 | 0.084 |
| Smokers | 3 (7.3) | 2 (5.3) | 1.000 |
| Anticoagulant use | 1 (2.4) | 1 (2.6) | 1.000 |
| History of abdominal surgery | 4 (9.8) | 3 (7.9) | 1.000 |
| Chemotherapy | 10 (24.4) | 12 (31.6) | 0.616 |
| Radiotherapy | 5 (12.2) | 4 (10.5) | 1.000 |
| Comorbidity | |||
| Diabetes mellitus | 3 (7.3) | 5 (13.2) | 0.471 |
| Hypertension | 3 (7.3) | 7 (18.4) | 0.183 |
| Dyslipidemia | 2 (4.9) | 5 (13.2) | 0.252 |
| Primary Closure (%) | Dermal Autograft (%) | p | |
|---|---|---|---|
| Time of reconstruction | 0.133 | ||
| Immediate | 27 (65.9) | 31 (81.6) | |
| Delayed | 14 (34.1) | 7 (18.4) | |
| Type of reconstruction | <0.05 † | ||
| Free TRAM | 26 (63.4) | 3 (7.9) | |
| Pedicled TRAM | 15 (36.6) | 35 (92.1) |
| Primary Closure (%) | Dermal Autograft (%) | p | |
|---|---|---|---|
| Donor Morbidity | |||
| Bulging | 8 (19.5) | 1 (2.6) | 0.030 † |
| Hernia | 0 (0.0) | 0 (0.0) | N/A |
| Fat necrosis | 1 (2.4) | 0 (0.0) | 1.000 |
| Seroma | 0 (0.0) | 0 (0.0) | N/A |
| Umbilicus necrosis | 1 (2.4) | 0 (0.0) | 1.000 |
| Wound dehiscence | 0 (0.0) | 0 (0.0) | N/A |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, W.S.; Park, S.O.; Kim, I.-K. Prevention of Abdominal Bulging Using Onlay Dermal Autografts from Discarded Zone IV TRAM Flap Tissue. J. Clin. Med. 2022, 11, 1929. https://doi.org/10.3390/jcm11071929
Lee WS, Park SO, Kim I-K. Prevention of Abdominal Bulging Using Onlay Dermal Autografts from Discarded Zone IV TRAM Flap Tissue. Journal of Clinical Medicine. 2022; 11(7):1929. https://doi.org/10.3390/jcm11071929
Chicago/Turabian StyleLee, Won Seob, Seong Oh Park, and Il-Kug Kim. 2022. "Prevention of Abdominal Bulging Using Onlay Dermal Autografts from Discarded Zone IV TRAM Flap Tissue" Journal of Clinical Medicine 11, no. 7: 1929. https://doi.org/10.3390/jcm11071929






