Quantifying the Effect of Monitor Wear Time and Monitor Type on the Estimate of Sedentary Time in People with COPD: Systematic Review and Meta-Analysis
Abstract
:1. Introduction
2. Methods
2.1. Study Selection
2.2. Search Strategy
2.3. Data Extraction
2.4. Statistical Analysis
3. Results
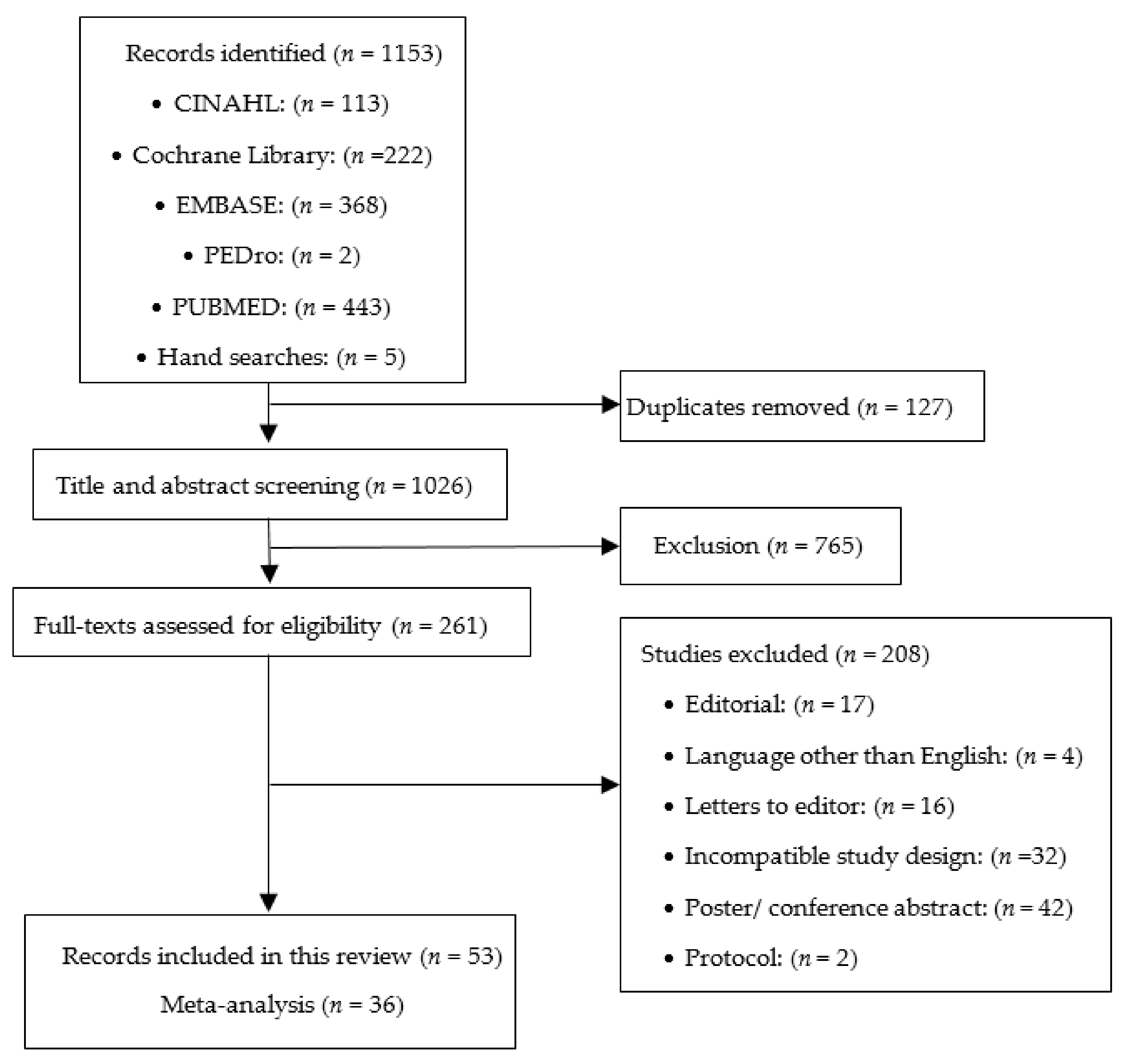
3.1. Study Selection and Grouping
3.2. Characteristics of Participants
3.3. Meta-Analysis
4. Discussion
Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Tremblay, M.S.; Aubert, S.; Barnes, J.D.; Saunders, T.J.; Carson, V.; Latima-Cheung, A.E.; Chastin, S.F.M.; Alternberg, T.M.; Chinapaw, M.J.M.; on behalf of SBRN Terminology Consensus Project Participants. Sedentary Behavior Research Network (SBRN)—Terminology Consensus Project process and outcome. Int. J. Behav. Nutr. Phys. Act. 2017, 14, 75. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dunstan, D.W.; Barr, E.L.; Healy, G.N.; Salmon, J.; Shaw, J.E.; Balkau, B.; Cameran, A.J.; Zimmet, P.Z.; Owen, N. Television viewing time and mortality: The Australian Diabetes, Obesity and Lifestyle Study (AusDiab). Circulation 2010, 121, 384–391. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chomistek, A.K.; Manson, J.E.; Stefanick, M.L.; Lu, B.; Sands-Lincoln, M.; Going, S.B.; Garcia, L.; Allison, M.A.; Sims, S.T.; Lamonte, M.J.; et al. Relationship of sedentary behavior and physical activity to incident cardiovascular disease: Results from the Women’s Health Initiative. J. Am. Coll. Cardiol. 2013, 61, 2346–2354. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tremblay, M.S.; Colley, R.C.; Saunders, T.J.; Healy, G.N.; Owen, N. Physiological and health implications of a sedentary lifestyle. Appl. Physiol. Nutr. Metab. 2010, 35, 725–740. [Google Scholar] [CrossRef]
- Furlanetto, K.C.; Donaria, L.; Schneider, L.P.; Lopes, J.R.; Ribeiro, M.; Fernandes, K.B.; Hernandes, N.A.; Pitta, F. Sedentary Behavior Is an Independent Predictor of Mortality in Subjects With COPD. Respir. Care 2017, 62, 579–587. [Google Scholar] [CrossRef]
- Lewis, L.K.; Hunt, T.; Williams, M.T.; English, C.; Olds, T.S. Sedentary Behavior in People with and without a Chronic Health Condition: How Much, What and When? AIMS Public Health 2016, 3, 503–519. [Google Scholar] [CrossRef]
- McKeough, Z.; Cheng, S.W.M.; Alison, J.; Jenkins, C.; Hamer, M.; Stamakis, E. Low leisure-based sitting time and being physically active were associated with reduced odds of death and diabetes in people with chronic obstructive pulmonary disease: A cohort study. J. Physiother. 2018, 64, 114–120. [Google Scholar] [CrossRef]
- Park, S.K.; Larson, J.L. The relationship between physical activity and metabolic syndrome in people with chronic obstructive pulmonary disease. J. Cardiovasc. Nurs. 2014, 29, 499–507. [Google Scholar] [CrossRef] [Green Version]
- Holland, A.E.; Mahal, A.; Hill, C.J.; Lee, A.L.; Burge, A.T.; Cox, N.S.; Moore, R.; Nicolson, C.; O’Halloran, P.; Lahham, A. Home-based rehabilitation for COPD using minimal resources: A randomised, controlled equivalence trial. Thorax 2017, 72, 57–65. [Google Scholar] [CrossRef] [Green Version]
- Hill, K.; Ng, L.W.C.; Cecins, N.; Formico, V.R.; Cavalheri, V.; Jenkins, S.C. Effect of Using a Wheeled Walker on Physical Activity and Sedentary Time in People with Chronic Obstructive Pulmonary Disease: A Randomised Cross-Over Trial. Lung 2020, 198, 213–219. [Google Scholar] [CrossRef]
- Wootton, S.L.; Hill, K.; Alison, J.A.; Ng, L.W.C.; Jenkins, S.; Eastwood, P.R.; Hillman, D.R.; Jenkins, C.; Spencer, L.; Cecins, N. Effects of ground-based walking training on daily physical activity in people with COPD: A randomised controlled trial. Respir. Med. 2017, 132, 139–145. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pitta, F.; Troosters, T.; Spruit, M.A.; Probst, V.S.; Decramer, M.; Gosselink, R. Characteristics of physical activities in daily life in chronic obstructive pulmonary disease. Am. J. Respir. Crit. Care Med. 2005, 171, 972–977. [Google Scholar] [CrossRef] [PubMed]
- Sin, D.D.; Anthonisen, N.R.; Soriano, J.B.; Agust, A.G. Mortality in COPD: Role of comorbidities. Eur. Respir. J. 2006, 28, 1245–1257. [Google Scholar] [CrossRef] [PubMed]
- Byrom, B.; Rowe, D.A. Measuring free-living physical activity in COPD patients: Deriving methodology standards for clinical trials though a review of research studies. Contemp. Clin. Trials 2016, 47, 172–184. [Google Scholar] [CrossRef] [Green Version]
- Owen, N.; Healy, G.N.; Matthews, C.E.; Dunstan, D.W. Too much sitting: The population health science of sedentary behavior. Exerc. Sport Sci. Rev. 2010, 38, 105–113. [Google Scholar] [CrossRef]
- Grant, P.M.; Ryan, C.G.; Tigbe, W.W.; Granat, M.H. The validation of a novel activity monitor in the measurement of posture and motion during everyday activities. Br. J. Sports Med. 2006, 40, 992–997. [Google Scholar] [CrossRef] [Green Version]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef] [Green Version]
- Covidence Systematic Review Software; Computer Program; Veritas Health Innovation: Melbourne, Australia, 2020.
- SPSS Statistics for Windows; Version 25.0; Computer Program; IBM: Armonk, NY, USA, 2017.
- Viechtbauer, W. Conducting meta-analyses in R with metafor package. J. Stat. Softw. 2010, 36, 1–48. [Google Scholar] [CrossRef] [Green Version]
- Borenstein, M.; Hedges, L.V.; Higgins, J.P.T.; Rothstein, H. Introduction to Meta-Analysis; TJ International: Cornwall, UK, 2009. [Google Scholar]
- Cheng, S.W.M.; Alison, J.A.; Stamatakis, E.; Dennis, S.; McKeough, Z.J. Patterns and Correlates of Sedentary Behaviour Accumulation and Physical Activity in People with Chronic Obstructive Pulmonary Disease: A Cross-Sectional Study. COPD J. Chronic Obstr. Pulm. Dis. 2020, 17, 156–164. [Google Scholar] [CrossRef]
- McNamara, R.J.; McKeough, Z.J.; McKenzie, D.K.; Alison, J.A. Physical comorbidities affect physical activity in chronic obstructive pulmonary disease: A prospective cohort study. Respirology 2014, 19, 866–872. [Google Scholar] [CrossRef] [Green Version]
- Breyer, M.K.; Breyer-Kohansal, R.; Funk, G.C.; Dornhofer, N.; Spruit, M.; Wouters, E.; Wouters, E.F.M.; Burghuber, O.C.; Hartl, S. Nordic walking improves daily physical activities in COPD: A randomised controlled trial. Respir. Res. 2010, 11, 112. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cani, K.C.; Matte, D.L.; Silva, I.; Gulart, A.A.; Karloh, M.; Mayer, A.F. Impact of Home Oxygen Therapy on the Level of Physical Activities in Daily Life in Subjects With COPD. Respir. Care 2019, 64, 1392–1400. [Google Scholar] [CrossRef] [PubMed]
- Gulart, A.A.; Munari, A.B.; Klein, S.R.; Santos de Silveira, L.; Mayer, A.F. The Glittre-ADL Test Cut-Off Point to Discriminate Abnormal Functional Capacity in Patients with COPD. COPD J. Chronic Obstr. Pulm. Dis. 2018, 15, 73–78. [Google Scholar] [CrossRef] [PubMed]
- Gulart, A.A.; Araujo, C.L.P.; Munari, A.B.; Santos, K.D.; Karloh, M.; Foscarini, B.G.; Dal Lago, P.; Mayer, A.F. The minimal important difference for Glittre-ADL test in patients with chronic obstructive pulmonary disease. Braz. J. Phys. Ther. 2020, 24, 54–60. [Google Scholar] [CrossRef] [PubMed]
- Gulart, A.A.; Munari, A.B.; Klein, S.R.; Venancio, R.S.; Alexandre, H.F.; Mayer, A.F. The London Chest Activity of Daily Living scale cut-off point to discriminate functional status in patients with chronic obstructive pulmonary disease. Braz. J. Phys. Ther. 2020, 24, 264–272. [Google Scholar] [CrossRef] [PubMed]
- Machado, F.V.C.; Schneider, L.P.; Fonseca, J.; Belo, L.F.; Bonomo, C.; Furlanetto, K.C.; Felcar, J.M.; Roderigues, A.; Franssen, F.M.E.; Spruit, M.A. Clinical impact of body composition phenotypes in patients with COPD: A retrospective analysis. Eur. J. Clin. Nutr. 2019, 73, 1512–1519. [Google Scholar] [CrossRef]
- Morita, A.A.; Silva, L.K.O.; Bisca, G.W.; Oliveira, J.M.; Hernandes, N.A.; Pitta, F.; Furlanetto, K.C. Heart Rate Recovery, Physical Activity Level, and Functional Status in Subjects With COPD. Respir. Care 2018, 63, 1002–1008. [Google Scholar] [CrossRef] [Green Version]
- Munari, A.B.; Gulart, A.A.; Dos Santos, K.; Venancio, R.S.; Karloh, M.; Mayer, A.F. Modified Medical Research Council Dyspnea Scale in GOLD Classification Better Reflects Physical Activities of Daily Living. Respir. Care 2018, 63, 77–85. [Google Scholar] [CrossRef]
- Pitta, F.; Breyer, M.K.; Hernandes, N.A.; Teixeira, D.; Sant’Anna, T.J.; Fontana, A.D.; Probst, V.S.; Brunetto, A.F.; Spruit, M.A.; Wouters, E.F. Comparison of daily physical activity between COPD patients from Central Europe and South America. Respir. Med. 2009, 103, 421–426. [Google Scholar] [CrossRef] [Green Version]
- Pitta, F.; Troosters, T.; Spruit, M.A.; Decramer, M.; Gosselink, R. Activity monitoring for assessment of physical activities in daily life in patients with chronic obstructive pulmonary disease. Arch. Phys. Med. Rehabil. 2005, 86, 1979–1985. [Google Scholar] [CrossRef] [Green Version]
- Probst, V.S.; Kovelis, D.; Hernandes, N.A.; Camillo, C.A.; Cavalheri, V.; Pitta, F. Effects of 2 exercise training programs on physical activity in daily life in patients with COPD. Respir. Care 2011, 56, 1799–1807. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schneider, L.P.; Furlanetto, K.C.; Rodrigues, A.; Lopes, J.R.; Hernandes, N.A.; Pitta, F. Sedentary Behaviour and Physical Inactivity in Patients with Chronic Obstructive Pulmonary Disease: Two Sides of the Same Coin? COPD J. Chronic Obstr. Pulm. Dis. 2018, 15, 432–438. [Google Scholar] [CrossRef] [PubMed]
- Schneider, L.P.; Furlanetto, K.C.; Hernandes, N.A.; Pitta, F. Does wearing time of motion sensor interfere with the choice of physical activity in daily life outcomes of COPD patients? Fisioter. Pesqui. 2018, 25, 43–48. [Google Scholar] [CrossRef] [Green Version]
- Karloh, M.; Araujo, C.L.; Gulart, A.A.; Reis, C.M.; Steidle, L.J.; Mayer, A.F. The Glittre-ADL test reflects functional performance measured by physical activities of daily living in patients with chronic obstructive pulmonary disease. Braz. J. Phys. Ther. 2016, 20, 223–230. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bernard, P.; Hains-Monfette, G.; Atoui, S.; Moullec, G. Daily Objective Physical Activity and Sedentary Time in Adults with COPD Using Spirometry Data from Canadian Measures Health Survey. Can. Respir. J. 2018, 2018, 9107435. [Google Scholar] [CrossRef]
- Geidl, W.; Carl, J.; Cassar, S.; Lehbert, N.; Mino, E.; Wittmann, M.; Wagner, R.; Schulz, K.; Pfeifer, K. Physical Activity and Sedentary Behaviour Patterns in 326 Persons with COPD before Starting a Pulmonary Rehabilitation: A Cluster Analysis. J. Clin. Med. 2019, 8, 1346. [Google Scholar] [CrossRef] [Green Version]
- Vasilopoulou, M.; Papaioannou, A.I.; Kaltsakas, G.; Louvaris, A.; Chynkiamis, N.; Stavroula, S.; Kortianou, E.; Genimata, S.A.; Palamidas, A.; Kostikas, K. Home-based maintenance tele-rehabilitation reduces the risk for acute exacerbations of COPD, hospitalisations and emergency department visits. Eur. Respir. J. 2017, 49, 1602129. [Google Scholar] [CrossRef]
- Kawagoshi, A.; Kiyokawa, N.; Sugawara, K.; Takahashi, H.; Sakata, S.; Miura, S.; Sawamura, S.; Satake, M.; Shioya, T. Quantitative assessment of walking time and postural change in patients with COPD using a new triaxial accelerometer system. Int. J. Chronic Obstr. Pulm. Dis. 2013, 8, 397–404. [Google Scholar] [CrossRef] [Green Version]
- Park, S.K.; Richardson, C.R.; Holleman, R.G.; Larson, J.L. Physical activity in people with COPD, using the National Health and Nutrition Evaluation Survey dataset (2003–2006). Heart Lung 2013, 42, 235–240. [Google Scholar] [CrossRef] [Green Version]
- Mesquita, R.; Meijer, K.; Pitta, F.; Azcuna, H.; Goetz, Y.M.J.; Essers, J.M.N.; Wouters, E.F.M.; Spruit, M.A. Changes in physical activity and sedentary behaviour following pulmonary rehabilitation in patients with COPD. Respir. Med. 2017, 126, 122–129. [Google Scholar] [CrossRef] [Green Version]
- Mesquita, R.; Nakken, N.; Janssen, D.J.A.; van den Bogaart, E.H.; Delbressine, J.M.L.; Essers, J.M.N.; Meijer, K.; van Vliet, M.; de Vries, G.J.; Muris, J.W. Activity Levels and Exercise Motivation in Patients With COPD and Their Resident Loved Ones. Chest 2017, 151, 1028–1038. [Google Scholar] [CrossRef] [PubMed]
- Cruz, J.; Brooks, D.; Marques, A. Impact of feedback on physical activity levels of individuals with chronic obstructive pulmonary disease during pulmonary rehabilitation: A feasibility study. Chron. Respir. Dis. 2014, 11, 191–198. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cruz, J.; Brooks, D.; Marques, A. Walk2Bactive: A randomised controlled trial of a physical activity-focused behavioural intervention beyond pulmonary rehabilitation in chronic obstructive pulmonary disease. Chron. Respir. Dis. 2016, 13, 57–66. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Alyami, M.M.; Jenkins, S.C.; Hill, K. Walking-based activity and sedentary behavior in Saudi males with chronic obstructive pulmonary disease. Saudi Med. J. 2018, 39, 506–513. [Google Scholar] [CrossRef] [PubMed]
- Eliason, G.; Zakrisson, A.B.; Piehl-Aulin, K.; Hurtig-Wennlof, A. Physical activity patterns in patients in different stages of chronic obstructive pulmonary disease. COPD J. Chronic Obstr. Pulm. Dis. 2011, 8, 369–374. [Google Scholar] [CrossRef]
- Orme, M.W.; Steiner, M.C.; Morgan, M.D.; Kingsnorth, A.P.; Esliger, D.W.; Singh, S.J.; Sherar, L.B. 24-hour accelerometry in COPD: Exploring physical activity, sedentary behavior, sleep and clinical characteristics. Int. J. Chronic Obstr. Pulm. Dis. 2019, 14, 419–430. [Google Scholar] [CrossRef] [Green Version]
- Larson, J.L.; Covey, M.K.; Kapella, M.C.; Alex, C.G.; McAuley, E. Self-efficacy enhancing intervention increases light physical activity in people with chronic obstructive pulmonary disease. Int. J. Chronic Obstr. Pulm. Dis. 2014, 9, 1081–1090. [Google Scholar] [CrossRef] [Green Version]
- Loprinzi, P.D.; Kane, C.; Sigler, S.; Brown, K.; Walker, J.K. Free-living physical activity characteristics, activity-related air trapping and breathlessness, and utilization of transtheoretical constructs in COPD: A pilot study. Physiol. Behav. 2015, 152, 79–84. [Google Scholar] [CrossRef]
- Higgins, J.P.T.; Thompson, S.G.; Deeks, J.J.; Altman, D.G. Measuring inconsistency in meta-analysis. BMJ 2003, 237, 557–560. [Google Scholar] [CrossRef] [Green Version]
- Bowler, R.; Allinder, M.; Jacobson, S.; Miller, B.; Tal-Singer, R.; Locantore, N. Real-world use of rescue inhaler sensors, electronic symptom questionnaires and physical activity monitors in COPD. BMJ Open Respir Res. 2019, 6, e000350. [Google Scholar] [CrossRef] [Green Version]
- Demeyer, H.; Louvaris, Z.; Frei, A.; Rabinovich, R.A.; de Jong, C.; Gimeno-Santas, E.; Loeckx, M.; Buttery, S.C.; Rubio, N.; Van der Molen, T.; et al. Physical activity is increased by a 12-week semiautomated telecoaching programme in patients with COPD: A multicentre randomised controlled trial. Thorax 2017, 72, 415–423. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Demeyer, H.; Mohan, D.; Burtin, C.; Vaes, A.; Heasley, M.; Bowler, R.; Casaburi, R.; Cooper, C.B.; Corriol-Rohou, S.; Frei, A.; et al. Objectively Measured Physical Activity in Patients with COPD: Recommendations from an International Task Force on Physical Activity. Chronic Obstr. Pulm. Dis. J. COPD Found. 2021, 8, 528. [Google Scholar] [CrossRef] [PubMed]
- Garber, C.E.; Blissmer, B.; Deschenes, M.R.; Franklin, B.A.; Lamonte, M.J.; Lee, I.M.; Nieman, D.C.; Swain, D.P.; American College of Sports Medicine. American College of Sports Medicine position stand. Quantity and quality of exercise for developing and maintaining cardiorespiratory, musculoskeletal, and neuromotor fitness in apparently healthy adults: Guidance for prescribing exercise. Med. Sci. Sports Exerc. 2011, 43, 1334–1359. [Google Scholar] [CrossRef] [PubMed]
- Pate, R.R.; Pratt, M.; Blair, S.N.; Haskell, W.L.; Macera, C.A.; Bouchard, C.; Buchner, D.; Ettinger, W.; Heath, G.W.; King, A.C.; et al. American College of Sports Medicine. JAMA 1995, 273, 402–407. [Google Scholar] [CrossRef]
- Chau, J.Y.; Grunseit, A.; Midthjell, K.; Holmen, T.L.; Bauman, A.E.; van der Ploeg, H.P. Cross-sectional associations of total sitting and leisure screen time with cardiometabolic risk in adults. Results from the HUNT Study, Norway. J. Sci. Med. Sport 2014, 17, 78–84. [Google Scholar] [CrossRef]
- Peddle-McIntyre, C.J.; Cavalheri, V.; Boyle, T.; McVeigh, J.A.; Jeffery, E.; Lynch, B.M.; Vallance, J.K. A Review of Accelerometer-based Activity Monitoring in Cancer Survivorship Research. Med. Sci. Sports Exerc. 2018, 50, 1790–1801. [Google Scholar] [CrossRef]
- O’Brien, C.M.; Duda, J.L.; Kitas, G.D.; Veldhuijzen van Zanten, J.S.C.; Metsios, G.S.; Fenton, S.A.M. Measurement of sedentary time and physical activity in rheumatoid arthritis: An ActiGraph and activPAL validation study. Rheumatol. Int. 2020, 40, 1509–1518. [Google Scholar] [CrossRef]
- Reid, N.; Daly, R.M.; Winkler, E.A.; Gardiner, P.A.; Eakin, E.G.; Owen, N.; Dunstan, D.W.; Healy, G. Associations of Monitor-Assessed Activity with Performance-Based Physical Function. PLoS ONE 2016, 11, e0153398. [Google Scholar] [CrossRef]
- Grant, P.M.; Dall, P.M.; Mitchell, S.L.; Granat, M.H. Activity-monitor accuracy in measuring step number and cadence in community-dwelling older adults. J. Aging Phys. Act. 2008, 16, 201–214. [Google Scholar] [CrossRef] [Green Version]
- Kozey-Keadle, S.; Libertine, A.; Lyden, K.; Staudenmayer, J.; Freedson, P.S. Validation of wearable monitors for assessing sedentary behavior. Med. Sci Sports Exerc. 2011, 43, 1561–1567. [Google Scholar] [CrossRef] [Green Version]
- Coll, F.; Cavalheri, V.; Gucciardi, D.F.; Wulff, S.; Hill, K. In people with COPD, there is limited Evidence that Exercise Training Reduced Sedentary Time, and Behaviour Change Techniques are Poorly Reported: Systematic Review and Meta-analysis. Phys. Ther. 2021, 101, pzab097. [Google Scholar] [CrossRef] [PubMed]

| Study (Publication Year) | Total Sample Size | Age, Year | Males, N (Y%) | FEV1, % Predicted | Device | Time over which Participants were Instructed to Wear the Device | Minimum Daily wear Time to be Included in Analyses | Minimum Number of Days Data Needed to be Available to be Included in Analyses | Days Used in Data Analyses |
|---|---|---|---|---|---|---|---|---|---|
| Studies which used a monitor with a thigh inclinometer and a 12 h protocol | |||||||||
| Breyer (2010) [24] | 60 | 60 ± 9 | 27 (45) | 46 ± 18 | DAM | 3 days | 12 h | 3 days | Weekend days were excluded |
| Cani (2019) [25] | 59 | O2: 68 ± 8 C: 67 ± 8 | O2: 21 (79) C: Not recorded | O2: 25 ± 7 C: 24 ± 9 | DAM | 2 days | 12 h | 2 days | All days included |
| Kawagoshi (2013) [41] | 26 | 77 ± 6 | 26 (100) | 53 ± 26 | A-MES | 7 days | 12 h | 2 days | All days included |
| Munari (2018) [31] | 115 | 66 ± 8 | 75(68) | 35 ± 16 | DAM | Not reported | 12 h | 2 days | All days included |
| Pitta (2005) [12] | 50 | 64 ±7 | 36 (72) | 43 ± 18 | DAM | 2 days | 12 h | 2 days | All days included |
| Pitta (2005) [33] | 13 | 61 ±8 | 10 (77) | 33 ± 10 | DAM | 1 day | 12 h | 1 day | All days included |
| Pitta (2009) [32] | 80 | A: 63 ± 7 B: 66 ± 8 | A: 21 (53) B: 18 (45) | A: 48 ± 17 B: 46 ± 17 | DAM | 2 days | 12 h | 2 days | All days included |
| Probst (2011) [34] | 40 | Ix: 65 ± 10 C: 67 ± 7 | 21 (52) | Ix: 39 ± 14 C: 40 ± 13 | DAM + SWA | 2 days | 12 h | 2 days | Weekend days were excluded |
| Studies that used a monitor without a thigh inclinometer and a 12 h protocol | |||||||||
| Furlanetto (2017) [6] | 101 | 66 (62–72) median (IQR) | 58 (57) | 41(30–50) | SWA + Dynaport | 2 days | 12 h | 2 days | Weekend days were excluded |
| Gulart (2018) [26] | 59 | 65 ± 9 | 45 (76) | 35 ± 13 | Dynaport minimod | 2 days | 12 h | 2 days | All days included |
| Gulart (2020) [27] | 53 | 64 ± 9 | 37 (70) | 38 ± 14 | Dynaport minimod | 2 days | 12 h | 2 days | All days included |
| Gulart (2020) [28] | 61 | 65 ± 9 | 47 (77) | 35 ± 13 | Dynaport minimod | 2 days | 12 h | 2 days | All days included |
| Karloh (2016) [37] | 38 | 65 ± 7 | 22 (58) | 41 ± 15 | Dynaport minimod | 2 days | 12 h | 2 days | All days included |
| Machado (2019) [29] | 270 | G1: 67 ± 8 G2: 67 ± 8 G3: 68 ± 9 C: 67 ± 7 | G1:25 (74) G2:35 (63) G3:59 (80) C: 33 (31) | G1: 47 ± 16 G2: 43 ± 16 G3: 42 ± 16 C: 50 ± 14 | SWA | 2 days | ≥10 h | 2 weekdays | Weekend days were excluded |
| Morita (2018) [30] | 145 | 65 (60–73) median (IQR) | 67 (46) | 45 ± 15 | Dynaport move-monitor | 2 days | 12 h | 2 days | All days included |
| Schneider (2018) [35] | 137 | 66 ± 8 | 75 (56) | 46 (31–54) IQR | SWA | 2 days | ≥10 h | 2 weekdays | All days included |
| Studies that used a monitor without a thigh inclinometer and a waking hours protocol | |||||||||
| Alyami (2018) [47] | 34 | 62 ± 5 | 34(100) | 46 ± 16 | SAM | 8 days | ≥10 h | ≥5 days | All days included |
| Bernard (2018) [38] | 941 | 57 ± 15 | 519(55) | 85 ± 28 | Actical | 7 days | ≥8 h | ≥4 days | All days included |
| Cruz (2014) [45] | 16 | 66 ± 11 | 11(69) | 70 ± 23 | Actigraph | 7 days | ≥8 h | ≥5 days | All days included |
| Cruz (2016) [46] | 32 | 67 ± 8 | 27(84) | 67 ± 20 | Actigraph | 4 weekdays | ≥8 h | 4 days | Weekend days were excluded |
| Eliason (2011) [48] | 44 | Mild COPD: 64 ± 6 Moderate COPD: 64 ± 8 Severe COPD: 63 ± 8 | 16(36) | Not recorded | Actigraph | 7 days | ≥8 h | ≥3 days | All days included |
| Geidl (2019) [39] | 326 | 58 ± 6 | 174 (68) | 54 ± 18 | Actigraph | 7 days | ≥10 h | ≥5 days | All days included |
| Larson (2014) [50] | 49 | Ix: 71 ± 8 Ix: 72 ± 9 C: 71 ± 8 | 41(84) | Ix: 61 ± 20 Ix: 54 ± 17 C: 56 ± 17 | Actigraph | 7 days | ≥10 h | ≥3 days | All days included |
| Park (2013) [42] | 224 | 70 ± 9 | 114(51) | Actigraph | 7 days | ≥10 h | ≥4 days | All days included | |
| Vasilopoulou (2018) [40] | 147 | Ix: 67 ± 10 Ix: 67 ± 7 C: 64 ± 8 | Ix: 44(94) Ix: 38(76) C: 37(74) | Ix: 50 ± 22 Ix: 52 ± 17 C: 52 ± 21 | Actigraph | Not recorded | ≥8 h | ≥4 days | All days included |
| Studies that used a monitor with a thigh inclinometer and 24 h sleep removed protocol | |||||||||
| Cheng (2020) [22] | 69 | 74 ± 9 | 33 (48) | 55 ± 15 | ActivPAL | 7 days | ≥10 h | ≥4 days | All days included |
| Hill (2020) [11] | 11 | 72 ± 9 | 5 (45) | 28 ± 26 | ActivPAL | 5 to 7 days | ≥10 h | ≥3 days | All days included |
| Mesquita (2017) [43] | 90 | 67 ± 8 | 54 (60) | 47 ± 9 | MOX and CAM | ≥7 days | ≥10 h | 5 days | All days included |
| Mesquita (2017) [44] | 125 | 67 ± 4 | 69 (55) | 50 ± 9 | MOX | ≥7 days | ≥10 h | 5 days | All days included |
| Studies that used a monitor without a thigh inclinometer and a 24 h sleep removed protocol | |||||||||
| Holland (2017) [9] | 160 | Ix: 69 ± 13 Ix: 69 ± 10 | Ix: 48 (60) Ix: 51 (64) | 52 ± 19 49 ± 19 | SWA | 7 days | ≥10 h | ≥4 days | Yes 1 w/e day included |
| Lewis (2016) [6] | 24 | 75 ± 8 | 18(75) | 54 ± 23 | SWA + Actigraph | 7 days | ≥12 h | 6 days | All days included |
| Loprinzi (2015) [51] | 10 | 70 ± 10 | 4(40) | 68 ± 48 | Actigraph | 7 days | ≥10 h | 4 days | All days included |
| McNamara (2014) [23] | 50 | COPD + PC: 73 ± 11 COPD: 70 ± 8 | COPD + PC: 11 (44) COPD: 12 (48) | 51 ± 17 54 ± 11 | SWA | 9 days | >85% wear time | 3 days | All days included |
| Orme (2019) [49] | 109 | 66 ± 7 | 67 (61) | 76 ± 18 | Actigraph | 7 days | ≥10 h | ≥4 days | All days included |
| Schneider (2018) [36] | 45 | 66 ± 8 | 25 (55) | 46 ± 20 | SWA | 7 days | 24 h (3 groups: 8 h; 12 h; period awake) | 7 days | All days included |
| Wootton (2017) [10] | 101 | Ix: 69 ± 8 C: 68 ± 9 | Ix: 38(61) C: 24(62) | Ix: 42 ± 15 C: 43 ± 15 | SWA | 7 days | ≥12 h | ≥3 days primary analysis ≥4 days secondary analysis | No (primary analysis); 1 w/e day included (secondary analysis) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Coll, F.; Cavalheri, V.; Gucciardi, D.F.; Wulff, S.; Hill, K. Quantifying the Effect of Monitor Wear Time and Monitor Type on the Estimate of Sedentary Time in People with COPD: Systematic Review and Meta-Analysis. J. Clin. Med. 2022, 11, 1980. https://doi.org/10.3390/jcm11071980
Coll F, Cavalheri V, Gucciardi DF, Wulff S, Hill K. Quantifying the Effect of Monitor Wear Time and Monitor Type on the Estimate of Sedentary Time in People with COPD: Systematic Review and Meta-Analysis. Journal of Clinical Medicine. 2022; 11(7):1980. https://doi.org/10.3390/jcm11071980
Chicago/Turabian StyleColl, Fiona, Vinicius Cavalheri, Daniel F. Gucciardi, Sheldon Wulff, and Kylie Hill. 2022. "Quantifying the Effect of Monitor Wear Time and Monitor Type on the Estimate of Sedentary Time in People with COPD: Systematic Review and Meta-Analysis" Journal of Clinical Medicine 11, no. 7: 1980. https://doi.org/10.3390/jcm11071980
APA StyleColl, F., Cavalheri, V., Gucciardi, D. F., Wulff, S., & Hill, K. (2022). Quantifying the Effect of Monitor Wear Time and Monitor Type on the Estimate of Sedentary Time in People with COPD: Systematic Review and Meta-Analysis. Journal of Clinical Medicine, 11(7), 1980. https://doi.org/10.3390/jcm11071980






