Necrotizing Fasciitis of the Upper Limb: Optimizing Management to Reduce Complications
Abstract
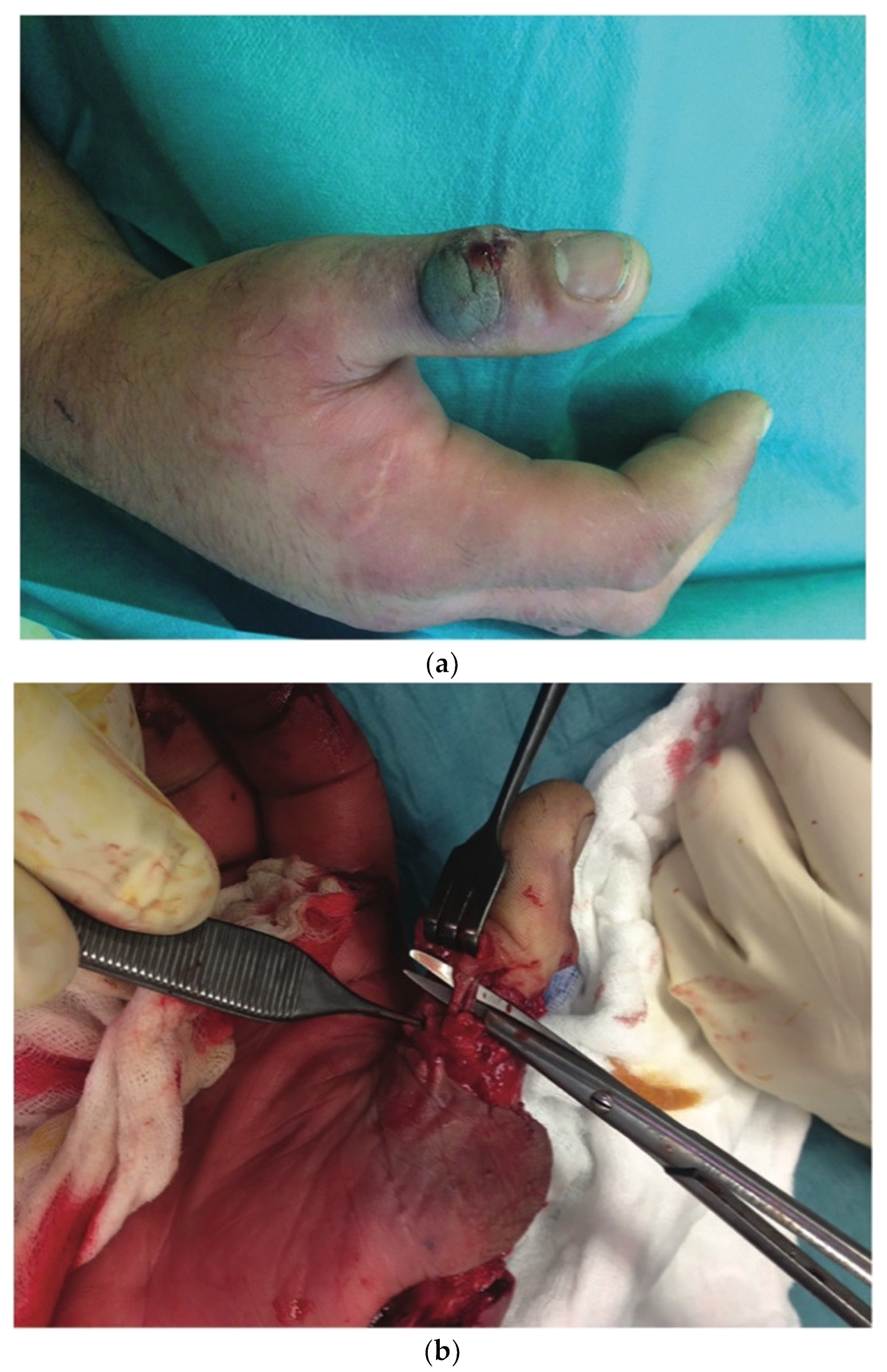
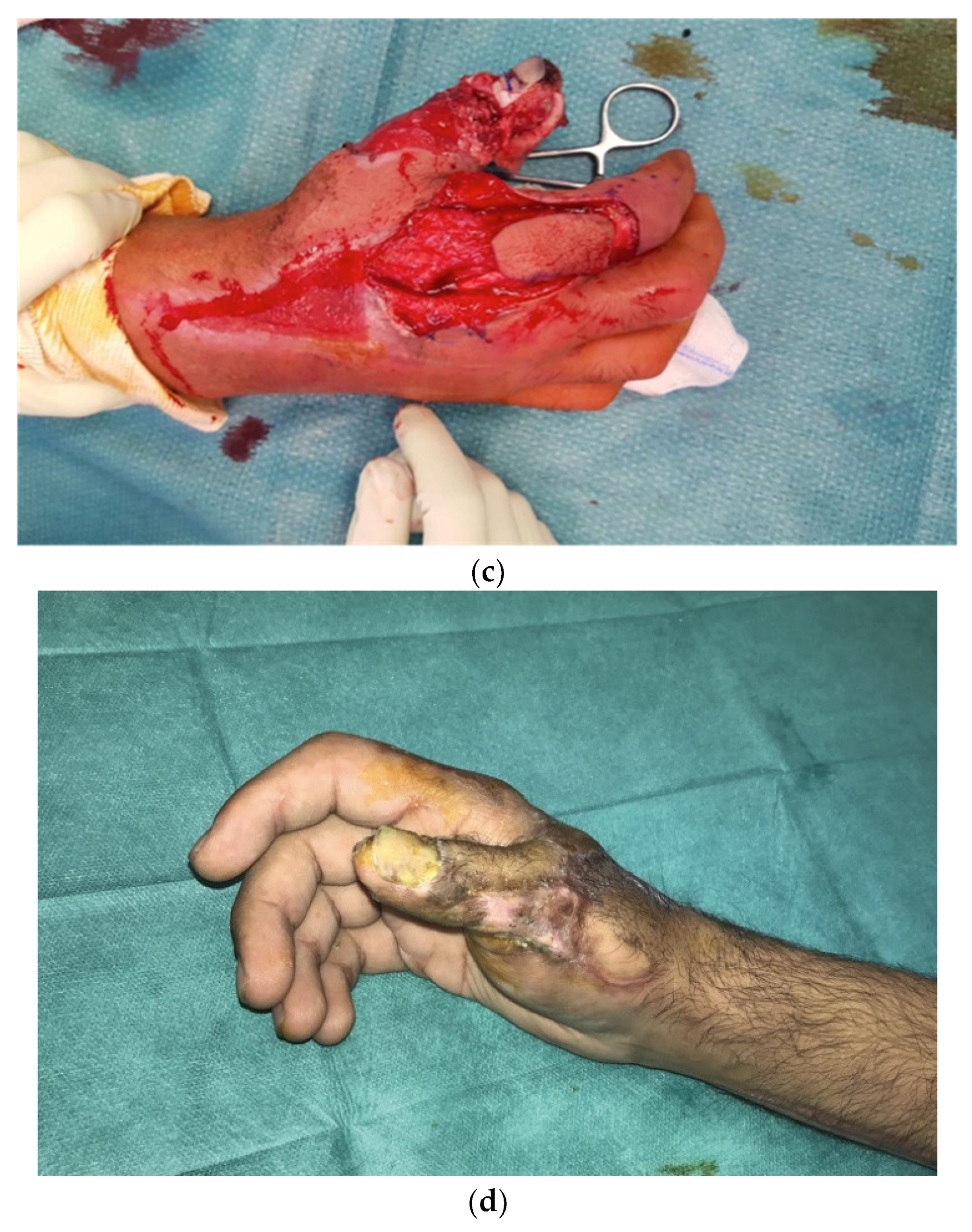
:1. Introduction
2. Materials and Methods
2.1. Standardized Management of Care of the NF Group of the Henri Mondor Institution
2.2. Surgical Protocol
3. Results
3.1. Microbiology
| NF Type I (Polymicrobial) n = 5 | One Case: MRSA and P. Aeruginosa |
|---|---|
| One case: methicillin-sensitive Staphylococcus and Enterococci | |
| Two cases: Staphylococcus aureus and Pseudomonas aeruginosa | |
| One case: M. morganii and E. faecalis | |
| NF Type II, monomicrobial n = 16 | 16 cases: GABHA |
| Muscle tissue affected (myositis) | 2 cases: GABHA NBDH-NF (2/16) |
3.2. Morbidity, Amputations and Mortality
3.3. Reconstructive Surgery
| Patients Receiving Thin Skin Grafts to Cover Loss of Soft Tissue | n = 15 (Covering Soft Tissue of the Forearm and Arm) |
|---|---|
| Patients receiving a full thickness skin graft to cover loss of soft tissue | n = 2 (2 patients from among the previous 15 cases), a full thickness skin graft was used to cover the back of the hand and the dorsal side of the thumb and second finger respectively. |
| Flaps | n = 1 kite-shaped flap to cover loss of soft tissue of the dorsal side of thumb |
| Healing by secondary intention | n = 3 mean delay for healing 98 days |
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Goh, T.; Goh, L.G.; Ang, C.H.; Wong, C.H. Early diagnosis of necrotizing fasciitis. J. Br. Surg. 2014, 101, e119–e125. [Google Scholar] [CrossRef] [PubMed]
- Endorf, F.W.; Supple, K.G.; Gamelli, R.L. The evolving characteristics and care of necrotizing soft-tissue infections. Burns 2005, 31, 269–273. [Google Scholar] [CrossRef] [PubMed]
- Ryssel, H.; Germann, G.; Kloeters, O.; Radu, C.A.; Reichenberger, M.; Gazyakan, E. Necrotizing fasciitis of the extremities: 34 cases at a single centre over the past 5 years. Arch. Orthop. Trauma. Surg. 2010, 130, 1515–1522. [Google Scholar] [CrossRef] [PubMed]
- Su, Y.-C.; Chen, H.-W.; Hong, Y.-C.; Chen, C.-T.; Hsiao, C.-T.; Chen, I.-C. Laboratory risk indicator for necrotizing fasciitis score and the outcomes. ANZ J. Surg. 2008, 78, 968–972. [Google Scholar] [CrossRef] [Green Version]
- Anaya, D.A.; McMahon, K.; Nathens, A.B.; Sullivan, S.R.; Foy, H.; Bulger, E. Predictors of mortality and limb loss in necrotizing soft tissue infections. Arch. Surg. 2005, 140, 151–157. [Google Scholar] [CrossRef] [Green Version]
- Hsiao, C.-T.; Weng, H.-H.; Yuan, Y.-D.; Chen, C.-T.; Chen, I.-C. Predictors of mortality in patients with necrotizing fasciitis. Am. J. Emerg. Med. 2008, 26, 170–175. [Google Scholar] [CrossRef]
- Chelsom, J.; Halstensen, A.; Haga, T.; Høiby, E.A. Necrotising fasciitis due to group A streptococci in western Norway: Incidence and clinical features. Lancet 1994, 344, 1111–1115. [Google Scholar] [CrossRef]
- Golger, A.; Ching, S.; Goldsmith, C.H.; Pennie, R.A.; Bain, J.R. Mortality in patients with necrotizing fasciitis. Plast. Reconstr. Surg. 2007, 119, 1803–1807. [Google Scholar] [CrossRef]
- Wong, C.-H.; Chang, H.-C.; Pasupathy, S.; Khin, L.-W.; Tan, J.-L.; Low, C.-O. Necrotizing fasciitis: Clinical presentation, microbiology, and determinants of mortality. J. Bone Jt. Surg. Am. 2003, 85, 1454–1460. [Google Scholar] [CrossRef] [Green Version]
- Angoules, A.G.; Kontakis, G.; Drakoulakis, E.; Vrentzos, G.; Granick, M.S.; Giannoudis, P.V. Necrotising fasciitis of upper and lower limb: A systematic review. Injury 2007, 38 (Suppl. S5), S18–S25. [Google Scholar] [CrossRef]
- Chan, T.; Yaghoubian, A.; Rosing, D.; Kaji, A.; de Virgilio, C. Low sensitivity of physical examination findings in necrotizing soft tissue infection is improved with laboratory values: A prospective study. Am. J. Surg. 2008, 196, 926–930. [Google Scholar] [CrossRef]
- Elliott, D.C.; Kufera, J.A.; Myers, R.A. Necrotizing soft tissue infections. Risk factors for mortality and strategies for management. Ann. Surg. 1996, 224, 672–683. [Google Scholar] [CrossRef]
- Singh, G.; Sinha, S.K.; Adhikary, S.; Babu, K.S.; Ray, P.; Khanna, S.K. Necrotising infections of soft tissues—A clinical profile. Eur. J. Surg. 2002, 168, 366–371. [Google Scholar] [CrossRef]
- Wall, D.B.; de Virgilio, C.; Black, S.; Klein, S.R. Objective criteria may assist in distinguishing necrotizing fasciitis from nonnecrotizing soft tissue infection. Am. J. Surg. 2000, 179, 17–21. [Google Scholar] [CrossRef]
- Kao, L.S.; Lew, D.F.; Arab, S.N.; Todd, S.R.; Awad, S.S.; Carrick, M.M.; Corneille, M.G.; Lally, K.P. Local variations in the epidemiology, microbiology, and outcome of necrotizing soft-tissue infections: A multicenter study. Am. J. Surg. 2011, 202, 139–145. [Google Scholar] [CrossRef] [Green Version]
- McHenry, C.R.; Piotrowski, J.J.; Petrinic, D.; Malangoni, M.A. Determinants of mortality for necrotizing soft-tissue infections. Ann. Surg. 1995, 221, 558–565. [Google Scholar] [CrossRef]
- Fernando, S.M.; Tran, A.; Cheng, W.; Rochwerg, B.; Kyeremanteng, K.; Seely, A.J.; Inaba, K.; Perry, J.J. Necrotizing Soft Tissue Infection: Diagnostic Accuracy of Physical Examination, Imaging, and LRINEC Score: A Systematic Review and Meta-Analysis. Ann. Surg. 2019, 269, 58–65. [Google Scholar] [CrossRef]
- Whallett, E.J.; Stevenson, J.H.; Wilmshurst, A.D. Necrotising fasciitis of the extremity. J. Plast. Reconstr. Aesthetic Surg. 2010, 63, e469–e473. [Google Scholar] [CrossRef]
- Cheng, N.-C.; Su, Y.-M.; Kuo, Y.-S.; Tai, H.-C.; Tang, Y.-B. Factors affecting the mortality of necrotizing fasciitis involving the upper extremities. Surg. Today 2008, 38, 1108–1113. [Google Scholar] [CrossRef]
- Schecter, W.; Meyer, A.; Schecter, G.; Giuliano, A.; Newmeyer, W.; Kilgore, E. Necrotizing fasciitis of the upper extremity. J. Hand Surg. Am. 1982, 7, 15–20. [Google Scholar] [CrossRef]
- Bleton, R.; Oberlin, C.; Alnot, J.Y.; Fichelle, A.; Chastre, J. Necrotizing fasciitis of the upper limb. 12 cases. Ann. Chir. Main Memb. Super. 1991, 10, 286–296. [Google Scholar]
- Sunderland, I.R.; Friedrich, J.B. Predictors of mortality and limb loss in necrotizing soft tissue infections of the upper extremity. J. Hand Surg. Am. 2009, 34, 1900–1901. [Google Scholar] [CrossRef]
- Gonzalez, M.H.; Kay, T.; Weinzweig, N.; Brown, A.; Pulvirenti, J. Necrotizing fasciitis of the upper extremity. J. Hand Surg. Am. 1996, 21, 689–692. [Google Scholar] [CrossRef]
- Hankins, C.L.; Southern, S. Factors that affect the clinical course of group A beta-haemolytic streptococcal infections of the hand and upper extremity: A retrospective study. Scand. J. Plast. Reconstr. Surg. Hand Surg. 2008, 42, 153–157. [Google Scholar] [CrossRef]
- Swartz, M.N. Clinical practice. Cellulitis. N. Engl. J. Med. 2004, 350, 904–912. [Google Scholar] [CrossRef]
- de Prost, N.; Bosc, R.; Brun-Buisson, C.; Chosidow, O.; Decousser, J.W.; Dhonneur, G.; Lepeule, R.; Rahmouni, A.; Sbidian, E.; Amathieu, R.; et al. Necrotizing fasciitis: Results of a survey on management practices in Frenchspeaking intensive care units. Ann. Fr. Danesthesie Reanim. 2014, 33, 638–642. [Google Scholar] [CrossRef]
- La Padula, S.; Hersant, B.; Noel, W.; Niddam, J.; Hermeziu, O.; Bouhassira, J.; Bosc, R.; Meningaud, J.P. Use of the retrograde limb of the internal mammary vein to avoid venous congestion in DIEP flap breast reconstruction: Further evidences of a reliable and timesparing procedure. Microsurgery 2016, 36, 447–452. [Google Scholar] [CrossRef]
- La Padula, S.; Hersant, B.; Meningaud, J.P. Intraoperative use of indocyanine green angiography for selecting the more reliable perforator of the anterolateral thigh flap: A comparison study. Microsurgery 2018, 38, 738–744. [Google Scholar] [CrossRef]
- La Padula, S.; Hersant, B.; Pizza, C.; Chesné, C.; Jamin, A.; Ben Mosbah, I.; Errico, C.; D’Andrea, F.; Rega, U.; Persichetti, P.; et al. Striae Distensae: In Vitro Study and Assessment of Combined Treatment With Sodium Ascorbate and Platelet-Rich Plasma on Fibroblasts. Aesthetic Plast Surg. 2021, 45, 1282–1293. [Google Scholar] [CrossRef]

| Patients n = 21 | 17 Men–4 Women |
|---|---|
| Affected areas | Hand and wrist n = 3 Hand, wrist and forearm n = 10 Hand, forearm and arm n = 8 |
| Point of entry | Hand (n = 17) Wrist (n = 2) Unidentified (n = 2) |
| Mean age | 51 ± 9.3 |
| Co-morbidities | |
| n = 7 (33%) n = 6 (28.5%) n = 13 (61%) |
| Mean delay between the appearance of symptoms and hospitalization (hours) | 48 ± 5.6 (6–72) |
| Mean delay between hospitalization and first operation (minutes) | 150 ± 23 (100–290) |
| Patients requiring only one revision surgery | 12 |
| Patients requiring two revision surgeries | 9 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
La Padula, S.; Pensato, R.; Zaffiro, A.; Hermeziu, O.; D’Andrea, F.; Pizza, C.; Meningaud, J.P.; Hersant, B. Necrotizing Fasciitis of the Upper Limb: Optimizing Management to Reduce Complications. J. Clin. Med. 2022, 11, 2182. https://doi.org/10.3390/jcm11082182
La Padula S, Pensato R, Zaffiro A, Hermeziu O, D’Andrea F, Pizza C, Meningaud JP, Hersant B. Necrotizing Fasciitis of the Upper Limb: Optimizing Management to Reduce Complications. Journal of Clinical Medicine. 2022; 11(8):2182. https://doi.org/10.3390/jcm11082182
Chicago/Turabian StyleLa Padula, Simone, Rosita Pensato, Antonio Zaffiro, Oana Hermeziu, Francesco D’Andrea, Chiara Pizza, Jean Paul Meningaud, and Barbara Hersant. 2022. "Necrotizing Fasciitis of the Upper Limb: Optimizing Management to Reduce Complications" Journal of Clinical Medicine 11, no. 8: 2182. https://doi.org/10.3390/jcm11082182
APA StyleLa Padula, S., Pensato, R., Zaffiro, A., Hermeziu, O., D’Andrea, F., Pizza, C., Meningaud, J. P., & Hersant, B. (2022). Necrotizing Fasciitis of the Upper Limb: Optimizing Management to Reduce Complications. Journal of Clinical Medicine, 11(8), 2182. https://doi.org/10.3390/jcm11082182










