A 10-Year Follow-Up of Ankle Syndesmotic Injuries: Prospective Comparison of Knotless Suture-Button Fixation and Syndesmotic Screw Fixation
Abstract
:1. Introduction
2. Materials and Methods
2.1. Population
2.2. Inclusion and Exclusion Criteria
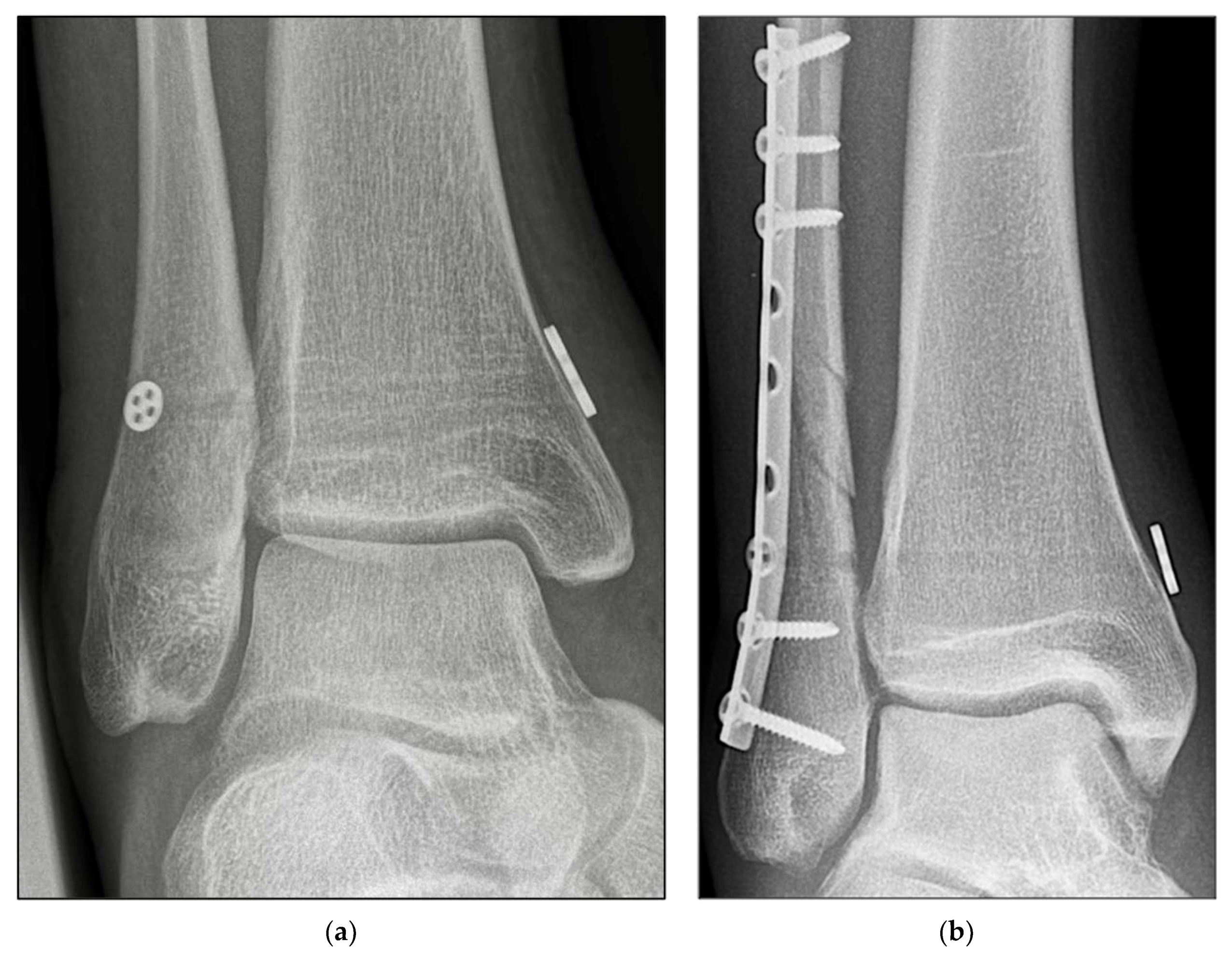
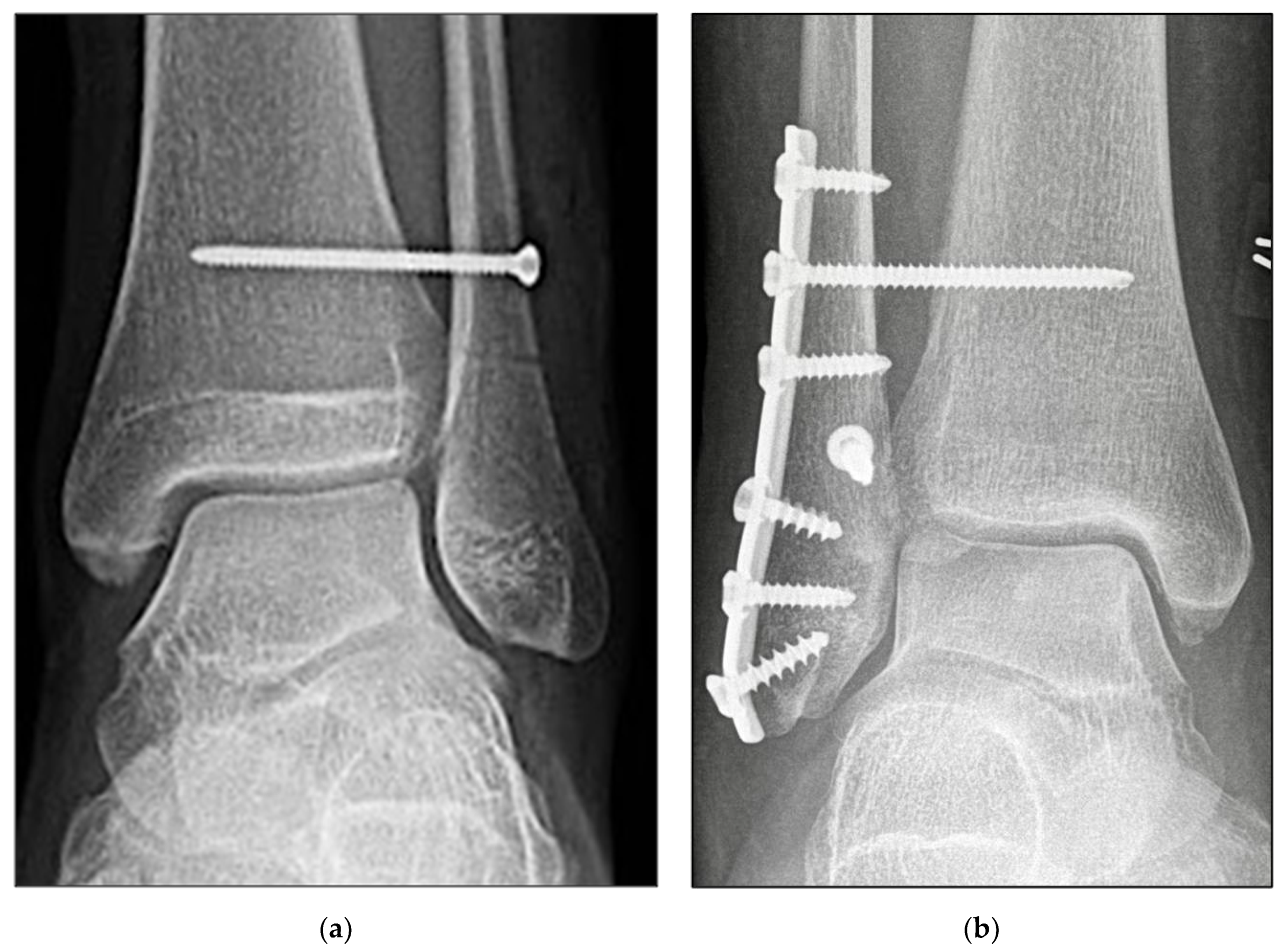
2.3. Surgical Procedure
2.4. Rehabilitation Protocol
2.5. Assessment Methods
2.6. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Lubberts, B.; D’Hooghe, P.; Bengtsson, H.; DiGiovanni, C.W.; Calder, J.; Ekstrand, J. Epidemiology and return to play following isolated syndesmotic injuries of the ankle: A prospective cohort study of 3677 male professional footballers in the UEFA Elite Club Injury Study. Br. J. Sports Med. 2019, 53, 959–964. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lee, S.W.; Lee, K.J.; Park, C.H.; Kwon, H.J.; Kim, B.S. The Valid Diagnostic Parameters in Bilateral CT Scan to Predict Unstable Syndesmotic Injury with Ankle Fracture. Diagnostics 2020, 10, 812. [Google Scholar] [CrossRef]
- Prakash, A.A. Epidemiology of High Ankle Sprains: A Systematic Review. Foot Ankle Spec. 2020, 13, 420–430. [Google Scholar] [CrossRef] [PubMed]
- Doherty, C.; Delahunt, E.; Caulfield, B.; Hertel, J.; Ryan, J.; Bleakley, C. The incidence and prevalence of ankle sprain injury: A systematic review and meta-analysis of prospective epidemiological studies. Sports Med. 2014, 44, 123–140. [Google Scholar] [CrossRef] [PubMed]
- Cornu, O.; Manon, J.; Tribak, K.; Putineanu, D. Traumatic injuries of the distal tibiofibular syndesmosis. Orthop. Traumatol. Surg. Res. 2021, 107, 102778. [Google Scholar] [CrossRef]
- Jeong, B.O.; Baek, J.H.; Song, W.J. Ankle Arthritis Combined With Chronic Instability of the Syndesmosis After Ankle Fracture With Syndesmotic Injury: A Case Report. J. Foot Ankle Surg. 2018, 57, 1000–1004. [Google Scholar] [CrossRef]
- Pogliacomi, F.; De Filippo, M.; Casalini, D.; Longhi, A.; Tacci, F.; Perotta, R.; Pagnini, F.; Tocco, S.; Ceccarelli, F. Acute syndesmotic injuries in ankle fractures: From diagnosis to treatment and current concepts. World J. Orthop. 2021, 12, 270–291. [Google Scholar] [CrossRef]
- Tourne, Y.; Molinier, F.; Andrieu, M.; Porta, J.; Barbier, G. Diagnosis and treatment of tibiofibular syndesmosis lesions. Orthop. Traumatol. Surg. Res. 2019, 105, S275–S286. [Google Scholar] [CrossRef]
- Stenquist, D.S.; Ye, M.Y.; Kwon, J.Y. Acute and Chronic Syndesmotic Instability: Role of Surgical Stabilization. Clin. Sports Med. 2020, 39, 745–771. [Google Scholar] [CrossRef]
- Switaj, P.J.; Mendoza, M.; Kadakia, A.R. Acute and Chronic Injuries to the Syndesmosis. Clin. Sports Med. 2015, 34, 643–677. [Google Scholar] [CrossRef]
- Swords, M.; Brilhault, J.; Sands, A. Acute and Chronic Syndesmotic Injury: The Authors’ Approach to Treatment. Foot Ankle Clin. 2018, 23, 625–637. [Google Scholar] [CrossRef] [PubMed]
- Colcuc, C.; Blank, M.; Stein, T.; Raimann, F.; Weber-Spickschen, S.; Fischer, S.; Hoffmann, R. Lower complication rate and faster return to sports in patients with acute syndesmotic rupture treated with a new knotless suture button device. Knee Surg. Sports Traumatol. Arthrosc. 2018, 26, 3156–3164. [Google Scholar] [CrossRef] [PubMed]
- Marasco, D.; Russo, J.; Izzo, A.; Vallefuoco, S.; Coppola, F.; Patel, S.; Smeraglia, F.; Balato, G.; Mariconda, M.; Bernasconi, A. Static versus dynamic fixation of distal tibiofibular syndesmosis: A systematic review of overlapping meta-analyses. Knee Surg. Sports Traumatol. Arthrosc. 2021, 29, 3534–3542. [Google Scholar] [CrossRef]
- Ramsey, D.C.; Friess, D.M. Cost-Effectiveness Analysis of Syndesmotic Screw Versus Suture Button Fixation in Tibiofibular Syndesmotic Injuries. J. Orthop Trauma 2018, 32, e198–e203. [Google Scholar] [CrossRef] [PubMed]
- Kortekangas, T.H.; Pakarinen, H.J.; Savola, O.; Niinimaki, J.; Lepojarvi, S.; Ohtonen, P.; Flinkkila, T.; Ristiniemi, J. Syndesmotic fixation in supination-external rotation ankle fractures: A prospective randomized study. Foot Ankle Int. 2014, 35, 988–995. [Google Scholar] [CrossRef]
- Hennings, R.; Souleiman, F.; Heilemann, M.; Hennings, M.; Klengel, A.; Osterhoff, G.; Hepp, P.; Ahrberg, A.B. Suture button versus syndesmotic screw in ankle fractures-evaluation with 3D imaging-based measurements. BMC Musculoskelet. Disord. 2021, 22, 970. [Google Scholar] [CrossRef]
- Li, Y.; Hong, H.; Liu, H.; Ding, Z. Short-term effectiveness of tightrope system for treatment of syndesmotic tibiofibular diastasis. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi 2016, 30, 971–974. [Google Scholar] [CrossRef]
- McKenzie, A.C.; Hesselholt, K.E.; Larsen, M.S.; Schmal, H. A Systematic Review and Meta-Analysis on Treatment of Ankle Fractures With Syndesmotic Rupture: Suture-Button Fixation Versus Cortical Screw Fixation. J. Foot Ankle Surg. 2019, 58, 946–953. [Google Scholar] [CrossRef]
- Raeder, B.W.; Figved, W.; Madsen, J.E.; Frihagen, F.; Jacobsen, S.B.; Andersen, M.R. Better outcome for suture button compared with single syndesmotic screw for syndesmosis injury: Five-year results of a randomized controlled trial. Bone Joint J. 2020, 102-B, 212. [Google Scholar] [CrossRef]
- Zhang, L.; Xiong, J.X.; Zhou, X.; Xiong, L.J.; Yu, L. Biomechanical comparison of screw, tightrope and novel double endobutton in the treatment of tibiofibular syndesmotic injuries. Injury 2021, 52, 2813–2819. [Google Scholar] [CrossRef]
- Yawar, B.; Hanratty, B.; Asim, A.; Niazi, A.K.; Khan, A.M. Suture-Button Versus Syndesmotic Screw Fixation of Ankle Fractures: A Comparative Retrospective Review Over One Year. Cureus 2021, 13, e17826. [Google Scholar] [CrossRef] [PubMed]
- Andersen, M.R.; Frihagen, F.; Hellund, J.C.; Madsen, J.E.; Figved, W. Randomized Trial Comparing Suture Button with Single Syndesmotic Screw for Syndesmosis Injury. J. Bone Joint Surg. Am. 2018, 100, 2–12. [Google Scholar] [CrossRef]
- Gan, K.; Xu, D.; Hu, K.; Wu, W.; Shen, Y. Dynamic fixation is superior in terms of clinical outcomes to static fixation in managing distal tibiofibular syndesmosis injury. Knee Surg. Sports Traumatol. Arthrosc. 2020, 28, 270–280. [Google Scholar] [CrossRef] [PubMed]
- D’Hooghe, P.; Grassi, A.; Alkhelaifi, K.; Calder, J.; Baltes, T.P.A.; Zaffagnini, S.; Ekstrand, J. Return to play after surgery for isolated unstable syndesmotic ankle injuries (West Point grade IIB and III) in 110 male professional football players: A retrospective cohort study. Br. J. Sports Med. 2020, 54, 1168–1173. [Google Scholar] [CrossRef] [Green Version]
- Nishikawa, D.R.C.; Saito, G.H.; de Oliveira Junior, A.S.; Mendes, A.A.M.; Devito, L.P.; Prado, M.P. Clinical outcomes of isolated acute instability of the syndesmosis treated with arthroscopy and percutaneous suture-button fixation. Arch. Orthop. Trauma Surg. 2021, 141, 1567–1574. [Google Scholar] [CrossRef] [PubMed]
- Forschner, P.F.; Beitzel, K.; Imhoff, A.B.; Buchmann, S.; Feuerriegel, G.; Hofmann, F.; Karampinos, D.C.; Jungmann, P.; Pogorzelski, J. Five-Year Outcomes After Treatment for Acute Instability of the Tibiofibular Syndesmosis Using a Suture-Button Fixation System. Orthop. J. Sports Med. 2017, 5, 2325967117702854. [Google Scholar] [CrossRef] [Green Version]
- Vetter, S.Y.; Euler, J.; Beisemann, N.; Swartman, B.; Keil, H.; Grutzner, P.A.; Franke, J. Validation of radiological reduction criteria with intraoperative cone beam CT in unstable syndesmotic injuries. Eur. J. Trauma Emerg. Surg. 2021, 47, 897–903. [Google Scholar] [CrossRef] [Green Version]
- Colcuc, C.; Fischer, S.; Colcuc, S.; Busse, D.; Bliemel, C.; Neun, O.; Abt, H.P.; Hoffmann, R. Treatment strategies for partial chronic instability of the distal syndesmosis: An arthroscopic grading scale and operative staging concept. Arch. Orthop. Trauma Surg. 2016, 136, 157–163. [Google Scholar] [CrossRef]
- Ebramzadeh, E.; Knutsen, A.R.; Sangiorgio, S.N.; Brambila, M.; Harris, T.G. Biomechanical comparison of syndesmotic injury fixation methods using a cadaveric model. Foot Ankle Int. 2013, 34, 1710–1717. [Google Scholar] [CrossRef]
- Clanton, T.O.; Whitlow, S.R.; Williams, B.T.; Liechti, D.J.; Backus, J.D.; Dornan, G.J.; Saroki, A.J.; Turnbull, T.L.; LaPrade, R.F. Biomechanical Comparison of 3 Current Ankle Syndesmosis Repair Techniques. Foot Ankle Int. 2017, 38, 200–207. [Google Scholar] [CrossRef]
- Klitzman, R.; Zhao, H.; Zhang, L.Q.; Strohmeyer, G.; Vora, A. Suture-button versus screw fixation of the syndesmosis: A biomechanical analysis. Foot Ankle Int. 2010, 31, 69–75. [Google Scholar] [CrossRef] [PubMed]
- Alastuey-Lopez, D.; Seral, B.; Perez, M.A. Biomechanical evaluation of syndesmotic fixation techniques via finite element analysis: Screw vs. suture button. Comput. Methods Programs Biomed. 2021, 208, 106272. [Google Scholar] [CrossRef] [PubMed]
- Wikeroy, A.K.; Hoiness, P.R.; Andreassen, G.S.; Hellund, J.C.; Madsen, J.E. No difference in functional and radiographic results 8.4 years after quadricortical compared with tricortical syndesmosis fixation in ankle fractures. J. Orthop. Trauma 2010, 24, 17–23. [Google Scholar] [CrossRef] [PubMed]
- Parker, A.S.; Beason, D.P.; Slowik, J.S.; Sabatini, J.B.; Waldrop, N.E., 3rd. Biomechanical Comparison of 3 Syndesmosis Repair Techniques With Suture Button Implants. Orthop. J. Sports Med. 2018, 6, 2325967118804204. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kurtoglu, A.; Kochai, A.; Inanmaz, M.E.; Sukur, E.; Keskin, D.; Turker, M.; Uysal, M.; Sen, Z.; Daldal, I. A comparison of double single suture-button fixation, suture-button fixation, and screw fixation for ankle syndesmosis injury: A retrospective cohort study. Medicine 2021, 100, e25328. [Google Scholar] [CrossRef] [PubMed]
- Walley, K.C.; Hofmann, K.J.; Velasco, B.T.; Kwon, J.Y. Removal of Hardware After Syndesmotic Screw Fixation: A Systematic Literature Review. Foot Ankle Spec. 2017, 10, 252–257. [Google Scholar] [CrossRef]
- Weber, A.C.; Hull, M.G.; Johnson, A.J.; Henn, R.F., 3rd. Cost analysis of ankle syndesmosis internal fixation. J. Clin. Orthop. Trauma 2019, 10, 173–177. [Google Scholar] [CrossRef]
- Kim, J.; Kwon, M.; Day, J.; Seilern und Aspang, J.; Shim, J.; Cho, J. The Impact of Suture Button Removal in Syndesmosis Fixation. J. Clin. Med. 2021, 10, 3726. [Google Scholar] [CrossRef]
- King, C.M.; Hamilton, G.A.; Cobb, M.; Carpenter, D.; Ford, L.A. Association between ankle fractures and obesity. J. Foot Ankle Surg. 2012, 51, 543–547. [Google Scholar] [CrossRef]
- Porter, S.E.; Hanley, E.N., Jr. The musculoskeletal effects of smoking. J. Am. Acad. Orthop. Surg. 2001, 9, 9–17. [Google Scholar] [CrossRef]
- Lee, D.O.; Eom, J.S.; Jung, H.G. The effect of smoking on the outcomes of lateral ankle ligament reconstruction. J. Orthop. Sci. 2018, 23, 88–91. [Google Scholar] [CrossRef] [PubMed]
- Ray, R.; Koohnejad, N.; Clement, N.D.; Keenan, G.F. Ankle fractures with syndesmotic stabilisation are associated with a high rate of secondary osteoarthritis. Foot Ankle Surg. 2019, 25, 180–185. [Google Scholar] [CrossRef] [PubMed]
- Bai, L.; Zhang, W.; Guan, S.; Liu, J.; Chen, P. Syndesmotic malreduction may decrease fixation stability: A biomechanical study. J. Orthop. Surg. Res. 2020, 15, 64. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kubik, J.F.; Rollick, N.C.; Bear, J.; Diamond, O.; Nguyen, J.T.; Kleeblad, L.J.; Helfet, D.L.; Wellman, D.S. Assessment of malreduction standards for the syndesmosis in bilateral CT scans of uninjured ankles. Bone Joint J. 2021, 103-B, 178–183. [Google Scholar] [CrossRef] [PubMed]
- Lehtola, R.; Leskela, H.V.; Flinkkila, T.; Pakarinen, H.; Niinimaki, J.; Savola, O.; Ohtonen, P.; Kortekangas, T. Suture button versus syndesmosis screw fixation in pronation-external rotation ankle fractures: A minimum 6-year follow-up of a randomised controlled trial. Injury 2021, 52, 3143–3149. [Google Scholar] [CrossRef]


| Characteristic | SB (n = 21) | SF (n = 20) | All (n = 41) | p | |
|---|---|---|---|---|---|
| Age, years | |||||
| Mean | 44.43 | 47.20 | 45.78 | 0.458 | |
| Minimum | 27.00 | 25.00 | 25.00 | ||
| Maximum | 61.00 | 77.00 | 77.00 | ||
| BMI, kg/m2 | |||||
| Mean | 27.810 | 28.05 | 27.92 | 0.880 | |
| Minimum | 21.600 | 19.50 | 19.50 | ||
| Maximum | 39.100 | 37.60 | 39.10 | ||
| Sex, n (%) | |||||
| Male | 16 (76.19) | 15 (75) | 31 (75.61) | 0.931 | |
| Female | 5 (23.81) | 5 (25) | 10 (24.39) | ||
| Affected side, n (%) | |||||
| Left | 11 (52.38) | 14 (70.00) | 25 (60.98) | 0.259 | |
| Right | 10 (47.61) | 6 (30.00) | 16 (39.02) | ||
| Smoker, n (%) | |||||
| Yes | 5 (23.81) | 3 (15.00) | 8 (19.15) | 0.489 | |
| No | 16 (76.19) | 17 (85.00) | 33 (80.49) | ||
| Pre-existing conditions, n (%) | |||||
| Metabolic syndrome-associated | 7 (33.33) | 3 (15.00) | 10 (24.39) | 0.633 | |
| Others | 4 (19.07) | 9 (45.00) | 13 (31.71) | ||
| None | 10 (47.60) | 8 (40.00) | 18 (43.90) | ||
| Injury classification, n (%) | |||||
| Weber B | 2 (9.53) | 4 (20.00) | 6 (14.63) | 0.338 | |
| Weber C | 2 (9.53) | 3 (15.00) | 5 (12.19) | ||
| Isolated a | 11 (52.38) | 8 (40.00) | 19 (46.34) | ||
| Maisonneuve | 6 (28.57) | 5 (25.00) | 11 (26.83) |
| Measurements | SB (n = 21) | SF (n = 20) | All (n = 41) | p |
|---|---|---|---|---|
| Follow-up in months | ||||
| Mean | 116.52 | 120.25 | 118.34 | 0.056 |
| Range | 105.00–124.00 | 107.00–128.00 | 105.00–128.00 | |
| OMAS | ||||
| Mean | 98.81 | 93.00 | 95.98 | 0.101 |
| SEM | 0.59 | 3.49 | 1.77 | |
| Minimum | 90.00 | 30.00 | 30.00 | |
| Maximum | 100.00 | 100.00 | 100.00 | |
| FADI Score ADL | ||||
| Mean | 99.22 | 95.86 | 97.58 | 0.154 |
| SEM | 0.36 | 2.34 | 1.17 | |
| Minimum | 94.20 | 54.80 | 54.80 | |
| Maximum | 100.00 | 100.00 | 100.00 | |
| FADI Score Sport | ||||
| Mean | 97.03 | 91.10 | 94.14 | 0.254 |
| SEM | 1.41 | 4.99 | 2.55 | |
| Minimum | 78.10 | 15.60 | 15.60 | |
| Maximum | 100.00 | 100.00 | 100.00 |
| Measurements | Isolated Syndesmotic Injury | Weber B and Syndesmotic Injury | Weber C and Syndesmotic Injury | Maisonneuve and Syndesmotic Injury | p |
|---|---|---|---|---|---|
| OMAS | |||||
| Mean (range) | 97.90 | 85.00 | 98.00 | 97.73 | 0.079 |
| SEM | 0.88 | 11.18 | 1.23 | 1.41 | |
| Minimum | 90.00 | 30.00 | 95.00 | 85.00 | |
| Maximum | 100.00 | 100.00 | 100.00 | 100.00 | |
| FADI Score ADL | |||||
| Mean | 99.089 | 91.017 | 98.640 | 98.073 | 0.135 |
| SEM | 0.371 | 7.296 | 1.127 | 1.560 | |
| Minimum | 95.200 | 54.800 | 94.200 | 82.700 | |
| Maximum | 100.000 | 100.000 | 100.000 | 100.000 | |
| FADI Score Sport | |||||
| Mean | 97.21 | 82.82 | 96.88 | 93.76 | 0.303 |
| SEM | 1.37 | 13.79 | 3.12 | 5.35 | |
| Minimum | 78.10 | 15.60 | 84.40 | 40.60 | |
| Maximum | 100.00 | 100.00 | 100.00 | 100.00 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Altmeppen, J.N.; Colcuc, C.; Balser, C.; Gramlich, Y.; Klug, A.; Neun, O.; Manegold, S.; Hoffmann, R.; Fischer, S. A 10-Year Follow-Up of Ankle Syndesmotic Injuries: Prospective Comparison of Knotless Suture-Button Fixation and Syndesmotic Screw Fixation. J. Clin. Med. 2022, 11, 2524. https://doi.org/10.3390/jcm11092524
Altmeppen JN, Colcuc C, Balser C, Gramlich Y, Klug A, Neun O, Manegold S, Hoffmann R, Fischer S. A 10-Year Follow-Up of Ankle Syndesmotic Injuries: Prospective Comparison of Knotless Suture-Button Fixation and Syndesmotic Screw Fixation. Journal of Clinical Medicine. 2022; 11(9):2524. https://doi.org/10.3390/jcm11092524
Chicago/Turabian StyleAltmeppen, Jan Niklas, Christian Colcuc, Christian Balser, Yves Gramlich, Alexander Klug, Oliver Neun, Sebastian Manegold, Reinhard Hoffmann, and Sebastian Fischer. 2022. "A 10-Year Follow-Up of Ankle Syndesmotic Injuries: Prospective Comparison of Knotless Suture-Button Fixation and Syndesmotic Screw Fixation" Journal of Clinical Medicine 11, no. 9: 2524. https://doi.org/10.3390/jcm11092524







