Not Just a One-Way: Mahaim Accessory Pathway Concomitantly Supporting Orthodromic Atrioventricular Re-Entrant Tachycardia
Abstract
:1. Introduction
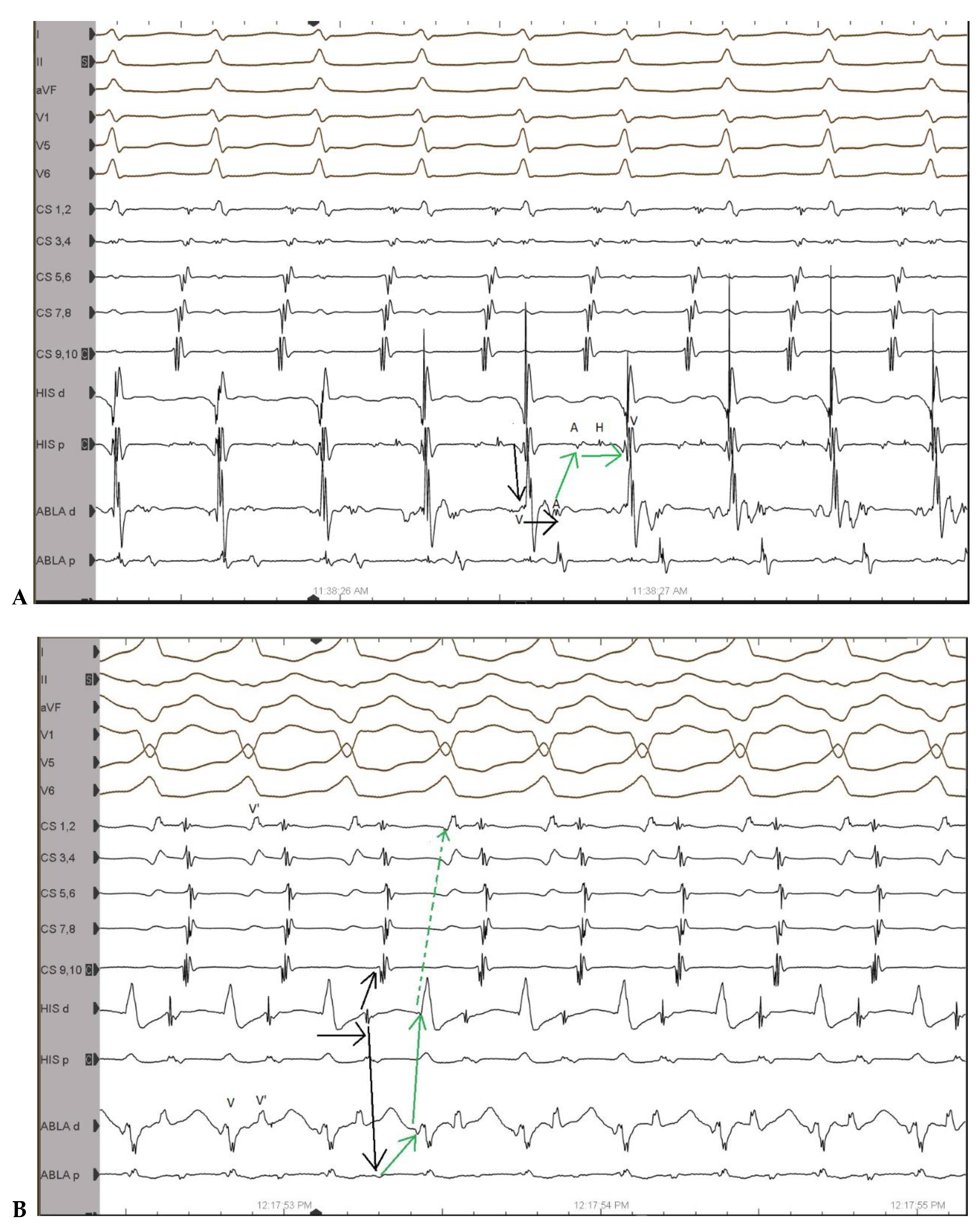
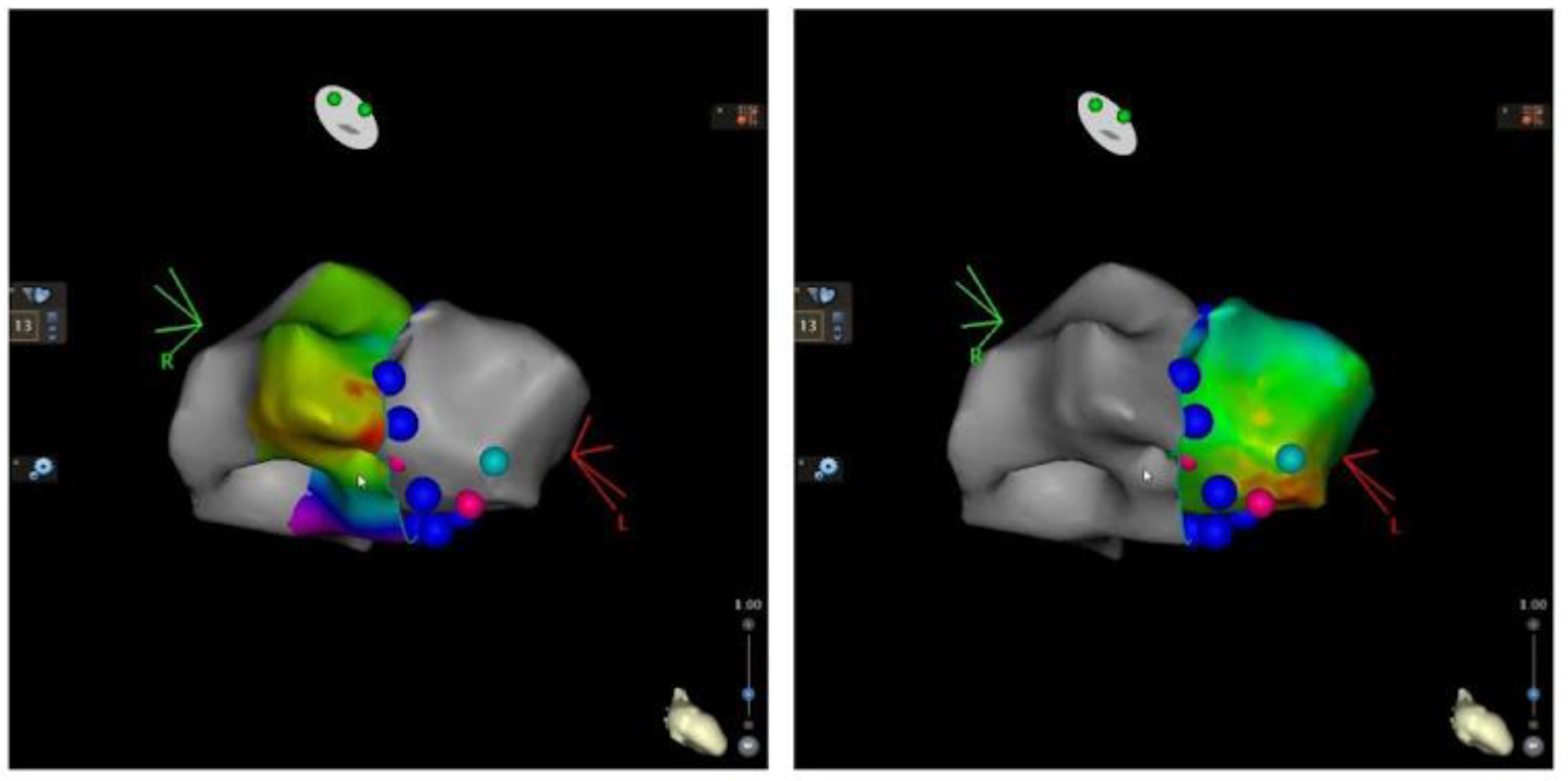
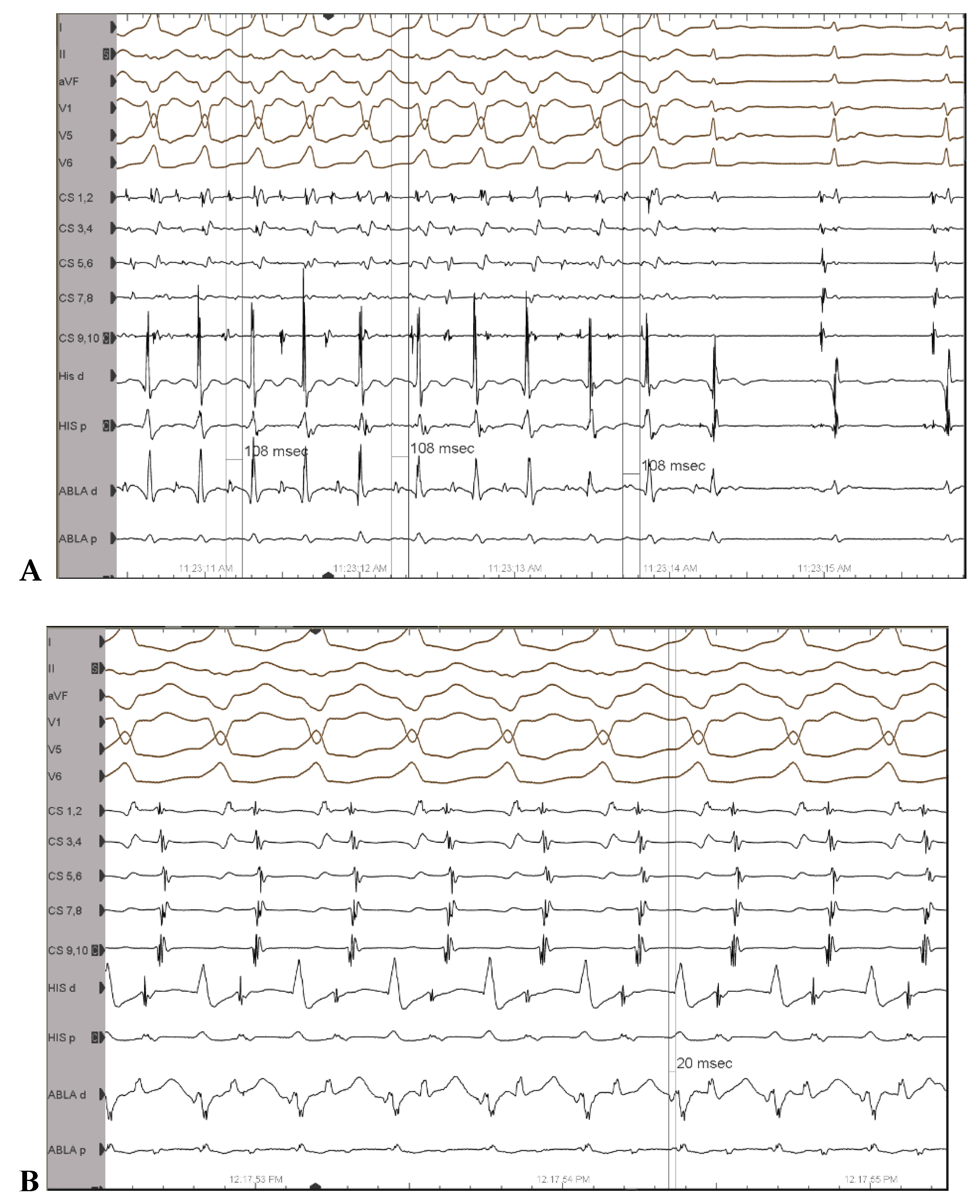
2. Case Presentation
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Mahaim, I.; Winston, M.R. Recherches d’Anatomie Comparée et de Pathologie Expérimentale Sur Les Connexions Hautes Du Faisceau de His-Tawara. Cardiology 1941, 5, 189–260. [Google Scholar] [CrossRef]
- Haïssaguerre, M.; Cauchemez, B.; Marcus, F.; Le Métayer, P.; Lauribe, P.; Poquet, F.; Gencel, L.; Clémenty, J. Characteristics of the Ventricular Insertion Sites of Accessory Pathways With Anterograde Decremental Conduction Properties. Circulation 1995, 91, 1077–1085. [Google Scholar] [CrossRef] [PubMed]
- Gandhavadi, M.; Sternick, E.B.; Jackman, W.M.; Wellens, H.J.J.; Josephson, M.E. Characterization of the Distal Insertion of Atriofascicular Accessory Pathways and Mechanisms of QRS Patterns in Atriofascicular Antidromic Tachycardia. Heart Rhythm 2013, 10, 1385–1392. [Google Scholar] [CrossRef] [PubMed]
- Katritsis, D.G.; Wellens, H.J.; Josephson, M.E. Mahaim Accessory Pathways. Arrhythmia Electrophysiol. Rev. 2017, 6, 29–32. [Google Scholar] [CrossRef] [PubMed]
- Arias, M.A.; Pachón, M.; Martín-Sierra, C. Spontaneous Wide QRS Complex Rhythm in a Patient With Wide QRS Complex Tachycardia. Circulation 2020, 141, 1498–1503. [Google Scholar] [CrossRef] [PubMed]
- Hluchy, J.; Schlegelmilch, P.; Schickel, S.; Jörger, U.; Jurkovicova, O.; Sabin, G.V. Radiofrequency Ablation of a Concealed Nodoventricular Mahaim Fiber Guided by a Discrete Potential. J. Cardiovasc. Electrophysiol. 1999, 10, 603–610. [Google Scholar] [CrossRef] [PubMed]
- Josephson, M.E. Electrophysiology at a Crossroads. Heart Rhythm 2007, 4, 658–661. [Google Scholar] [CrossRef] [PubMed]
- Sternick, E.B. Mahaim Fibre Tachycardia: Recognition and Management. Indian Pacing Electrophysiol. J. 2003, 3, 47–59. [Google Scholar] [PubMed]
- Gormel, S.; Yasar, S.; Yildirim, E.; Asil, S.; Baris, V.O.; Gokoglan, Y.; Celik, M.; Yuksel, U.C.; Vurgun, V.K.; Kabul, H.K.; et al. Comprehensive Assessment of Mahaim Accessory Pathways’ Anatomic Distribution. J. Int. Med. Res. 2022, 50, 03000605211069751. [Google Scholar] [CrossRef] [PubMed]
- Vali, Z.; Ng, G.A.; Aboulmaaty, M.; Ibrahim, M. Mahaim-Mediated Tachycardia Using at Times the Atrioventricular Node and Other Times a Left Lateral Accessory Pathway. Heart. Case Rep. 2021, 7, 641–649. [Google Scholar] [CrossRef] [PubMed]
- McClelland, J.H.; Wang, X.; Beckman, K.J.; Hazlitt, H.A.; Prior, M.I.; Nakagawa, H.; Lazzara, R.; Jackman, W.M. Radiofrequency Catheter Ablation of Right Atriofascicular (Mahaim) Accessory Pathways Guided by Accessory Pathway Activation Potentials. Circulation 1994, 89, 2655–2666. [Google Scholar] [CrossRef] [PubMed] [Green Version]


Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Deaconu, A.; Gondos, V.; Vatasescu, R. Not Just a One-Way: Mahaim Accessory Pathway Concomitantly Supporting Orthodromic Atrioventricular Re-Entrant Tachycardia. J. Clin. Med. 2023, 12, 159. https://doi.org/10.3390/jcm12010159
Deaconu A, Gondos V, Vatasescu R. Not Just a One-Way: Mahaim Accessory Pathway Concomitantly Supporting Orthodromic Atrioventricular Re-Entrant Tachycardia. Journal of Clinical Medicine. 2023; 12(1):159. https://doi.org/10.3390/jcm12010159
Chicago/Turabian StyleDeaconu, Alexandru, Viviana Gondos, and Radu Vatasescu. 2023. "Not Just a One-Way: Mahaim Accessory Pathway Concomitantly Supporting Orthodromic Atrioventricular Re-Entrant Tachycardia" Journal of Clinical Medicine 12, no. 1: 159. https://doi.org/10.3390/jcm12010159
APA StyleDeaconu, A., Gondos, V., & Vatasescu, R. (2023). Not Just a One-Way: Mahaim Accessory Pathway Concomitantly Supporting Orthodromic Atrioventricular Re-Entrant Tachycardia. Journal of Clinical Medicine, 12(1), 159. https://doi.org/10.3390/jcm12010159





