The Prognostic and Diagnostic Value of [18F]FDG PET/CT in Untreated Laryngeal Carcinoma
Abstract
:1. Introduction
2. Materials and Methods
2.1. Patients
2.2. [18F]FDG PET/CT Imaging and Interpretation
2.3. Neck MR Imaging and Interpretation
2.4. Reference Standard
2.5. Statistical Analysis
3. Results
3.1. Patient and Tumor Characteristics
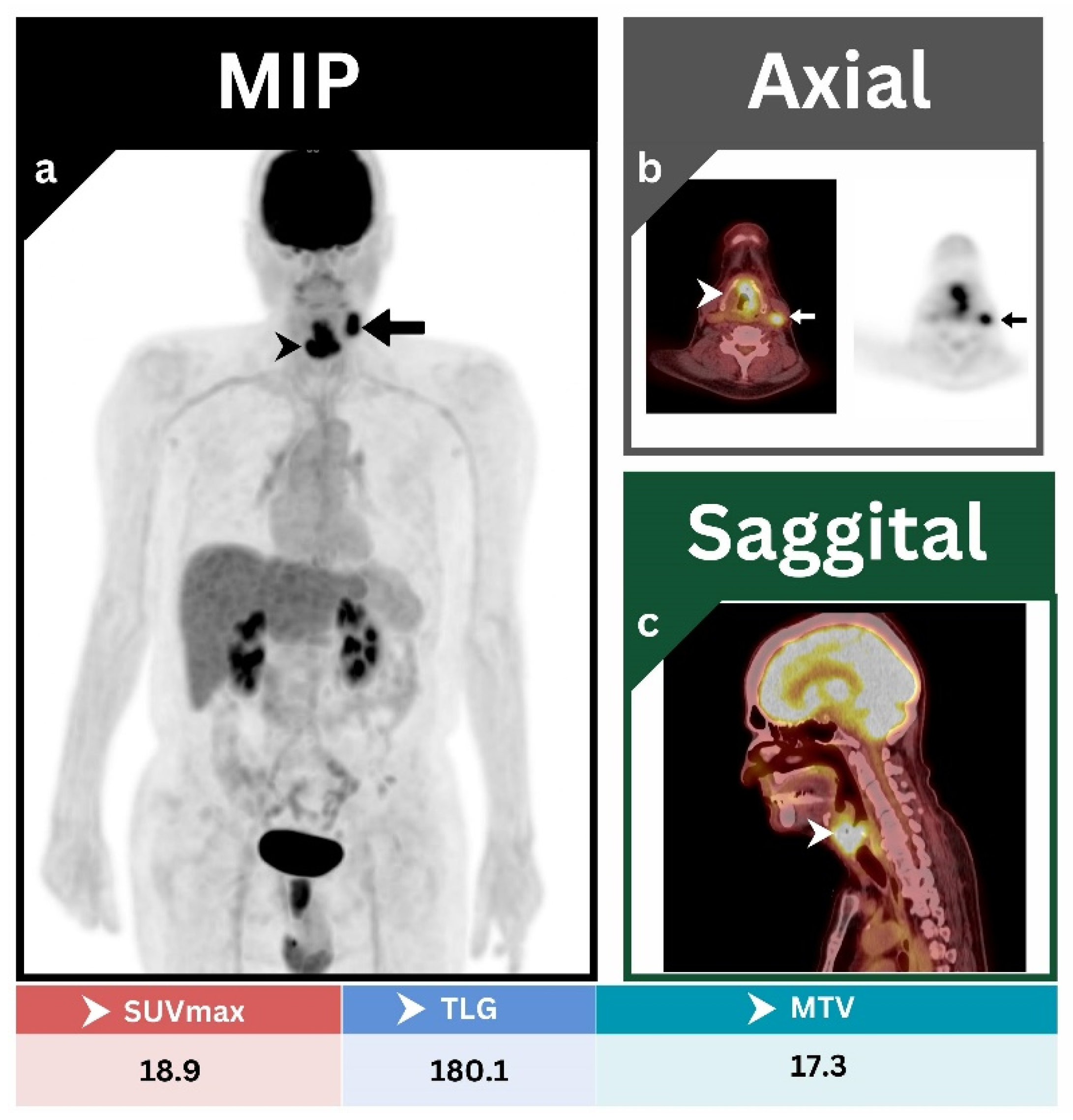
3.2. Primary Tumor
3.3. Cervical-Lymph-Node Metastases
3.3.1. Patient-Based Analysis
3.3.2. Side-by-Side Analysis
3.3.3. Assessment of Correct Nodal Staging
3.4. Role of [18F]FDG-PET/CT in Predicting PFS and OS
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Steuer, C.E.; El-Deiry, M.; Parks, J.R.; Higgins, K.A.; Saba, N.F. An update on larynx cancer. CA Cancer J. Clin. 2017, 67, 31–50. [Google Scholar] [CrossRef]
- Almadori, G.; Bussu, F.; Cadoni, G.; Galli, J.; Paludetti, G.; Maurizi, M. Molecular markers in laryngeal squamous cell carcinoma: Towards an integrated clinicobiological approach. Eur. J. Cancer 2005, 41, 683–693. [Google Scholar] [CrossRef] [PubMed]
- Forastiere, A.A.; Ismaila, N.; Lewin, J.S.; Nathan, C.A.; Adelstein, D.J.; Eisbruch, A.; Fass, G.; Fisher, S.G.; Laurie, S.A.; Le, Q.T.; et al. Use of Larynx-Preservation Strategies in the Treatment of Laryngeal Cancer: American Society of Clinical Oncology Clinical Practice Guideline Update. J. Clin. Oncol. 2018, 36, 1143–1169. [Google Scholar] [CrossRef] [PubMed]
- Kyzas, P.A.; Evangelou, E.; Denaxa-Kyza, D.; Ioannidis, J.P. 18F-fluorodeoxyglucose positron emission tomography to evaluate cervical node metastases in patients with head and neck squamous cell carcinoma: A meta-analysis. J. Natl. Cancer Inst. 2008, 100, 712–720. [Google Scholar] [CrossRef]
- Yongkui, L.; Jian, L.; Wanghan; Jingui, L. 18FDG-PET/CT for the detection of regional nodal metastasis in patients with primary head and neck cancer before treatment: A meta-analysis. Surg. Oncol. 2013, 22, e11–e16. [Google Scholar] [CrossRef] [PubMed]
- Sun, R.; Tang, X.; Yang, Y.; Zhang, C. (18)FDG-PET/CT for the detection of regional nodal metastasis in patients with head and neck cancer: A meta-analysis. Oral Oncol. 2015, 51, 314–320. [Google Scholar] [CrossRef]
- Jin, F.; Qu, B.; Fu, Z.; Zhang, Y.; Han, A.; Kong, L.; Yu, J. Prognostic Value of Metabolic Parameters of Metastatic Lymph Nodes on (18)F-FDG PET/CT in Patients With Limited-stage Small-cell Lung Cancer With Lymph Node Involvement. Clin. Lung Cancer 2018, 19, e101–e108. [Google Scholar] [CrossRef]
- Goel, R.; Moore, W.; Sumer, B.; Khan, S.; Sher, D.; Subramaniam, R.M. Clinical Practice in PET/CT for the Management of Head and Neck Squamous Cell Cancer. AJR Am. J. Roentgenol. 2017, 209, 289–303. [Google Scholar] [CrossRef]
- Lydiatt, W.M.; Patel, S.G.; O’Sullivan, B.; Brandwein, M.S.; Ridge, J.A.; Migliacci, J.C.; Loomis, A.M.; Shah, J.P. Head and neck cancers—Major changes in the American Joint Committee on cancer eighth edition cancer staging manual. CA Cancer J. Clin. 2017, 67, 122–137. [Google Scholar] [CrossRef]
- van Dijken, B.R.J.; Ankrah, A.O.; Stormezand, G.N.; Dierckx, R.; Jan van Laar, P.; van der Hoorn, A. Prognostic value of 11C-methionine volume-based PET parameters in IDH wild type glioblastoma. PLoS ONE 2022, 17, e0264387. [Google Scholar] [CrossRef]
- Kolinger, G.D.; Vallez Garcia, D.; Kramer, G.M.; Frings, V.; Smit, E.F.; de Langen, A.J.; Dierckx, R.; Hoekstra, O.S.; Boellaard, R. Repeatability of [(18)F]FDG PET/CT total metabolic active tumour volume and total tumour burden in NSCLC patients. EJNMMI Res. 2019, 9, 14. [Google Scholar] [CrossRef]
- Albano, D.; Dondi, F.; Paderno, A.; Nocivelli, G.; Maddalo, M.; Magrini, S.M.; Nicolai, P.; Maroldi, R.; Giubbini, R.; Bertagna, F. 18F-FDG-PET/CT in laryngeal cancer: Comparison with conventional imaging and prognostic role. Rev. Esp. Med. Nucl. Imagen Mol. (Engl. Ed.) 2021, 40, 229–238. [Google Scholar] [CrossRef]
- Chun, B.J.; Yoo Ie, R.; Joo, Y.H.; Nam, I.C.; Cho, J.H.; Kim, C.S.; Cho, K.J.; Kim, M.S. Efficacy of 18F-fluorodeoxyglucose positron emission tomography/CT imaging for extracapsular spread of laryngeal squamous cell carcinoma. Head Neck 2016, 38, 290–293. [Google Scholar] [CrossRef] [PubMed]
- Kandathil, A.; Subramaniam, R.M. PET/Computed Tomography: Laryngeal and Hypopharyngeal Cancers. PET Clin. 2022, 17, 235–248. [Google Scholar] [CrossRef]
- Chaput, A.; Robin, P.; Podeur, F.; Ollivier, M.; Keromnes, N.; Tissot, V.; Nonent, M.; Salaun, P.Y.; Rousset, J.; Abgral, R. Diagnostic performance of (18) fluorodesoxyglucose positron emission/computed tomography and magnetic resonance imaging in detecting T1-T2 head and neck squamous cell carcinoma. Laryngoscope 2018, 128, 378–385. [Google Scholar] [CrossRef]
- Subramaniam, R.M.; Truong, M.; Peller, P.; Sakai, O.; Mercier, G. Fluorodeoxyglucose-positron-emission tomography imaging of head and neck squamous cell cancer. AJNR Am. J. Neuroradiol. 2010, 31, 598–604. [Google Scholar] [CrossRef] [PubMed]
- Tatar, G.; Cermik, T.F.; Karagoz, Y.; Gundogan, C.; Karacetin, D.; Yildiz, E.; Yigit, O. The value of whole-body contrast-enhanced 18F-FDG PET/CT imaging in the diagnosis and staging of patients with laryngeal carcinoma. Nucl. Med. Commun. 2018, 39, 334–342. [Google Scholar] [CrossRef] [PubMed]
- Roh, J.L.; Park, J.P.; Kim, J.S.; Lee, J.H.; Cho, K.J.; Choi, S.H.; Nam, S.Y.; Kim, S.Y. 18F fluorodeoxyglucose PET/CT in head and neck squamous cell carcinoma with negative neck palpation findings: A prospective study. Radiology 2014, 271, 153–161. [Google Scholar] [CrossRef]
- Gordin, A.; Golz, A.; Keidar, Z.; Daitzchman, M.; Bar-Shalom, R.; Israel, O. The role of FDG-PET/CT imaging in head and neck malignant conditions: Impact on diagnostic accuracy and patient care. Otolaryngol. Head Neck Surg. 2007, 137, 130–137. [Google Scholar] [CrossRef]
- Schwartz, D.L.; Ford, E.; Rajendran, J.; Yueh, B.; Coltrera, M.D.; Virgin, J.; Anzai, Y.; Haynor, D.; Lewellyn, B.; Mattes, D.; et al. FDG-PET/CT imaging for preradiotherapy staging of head-and-neck squamous cell carcinoma. Int. J. Radiat. Oncol. Biol. Phys. 2005, 61, 129–136. [Google Scholar] [CrossRef]
- Roh, J.L.; Yeo, N.K.; Kim, J.S.; Lee, J.H.; Cho, K.J.; Choi, S.H.; Nam, S.Y.; Kim, S.Y. Utility of 2-[18F] fluoro-2-deoxy-D-glucose positron emission tomography and positron emission tomography/computed tomography imaging in the preoperative staging of head and neck squamous cell carcinoma. Oral Oncol. 2007, 43, 887–893. [Google Scholar] [CrossRef]
- Liao, C.T.; Wang, H.M.; Huang, S.F.; Chen, I.H.; Kang, C.J.; Lin, C.Y.; Fan, K.H.; Ng, S.H.; Hsueh, C.; Lee, L.Y.; et al. PET and PET/CT of the neck lymph nodes improves risk prediction in patients with squamous cell carcinoma of the oral cavity. J. Nucl. Med. 2011, 52, 180–187. [Google Scholar] [CrossRef] [PubMed]
- Krabbe, C.A.; Pruim, J.; van der Laan, B.F.; Rodiger, L.A.; Roodenburg, J.L. FDG-PET and detection of distant metastases and simultaneous tumors in head and neck squamous cell carcinoma: A comparison with chest radiography and chest CT. Oral. Oncol. 2009, 45, 234–240. [Google Scholar] [CrossRef]
- Rohde, M.; Nielsen, A.L.; Johansen, J.; Sorensen, J.A.; Nguyen, N.; Diaz, A.; Nielsen, M.K.; Asmussen, J.T.; Christiansen, J.M.; Gerke, O.; et al. Head-to-Head Comparison of Chest X-Ray/Head and Neck MRI, Chest CT/Head and Neck MRI, and (18)F-FDG PET/CT for Detection of Distant Metastases and Synchronous Cancer in Oral, Pharyngeal, and Laryngeal Cancer. J. Nucl. Med. 2017, 58, 1919–1924. [Google Scholar] [CrossRef] [PubMed]
- Manca, G.; Vanzi, E.; Rubello, D.; Giammarile, F.; Grassetto, G.; Wong, K.K.; Perkins, A.C.; Colletti, P.M.; Volterrani, D. (18)F-FDG PET/CT quantification in head and neck squamous cell cancer: Principles, technical issues and clinical applications. Eur. J. Nucl. Med. Mol. Imaging 2016, 43, 1360–1375. [Google Scholar] [CrossRef] [PubMed]
- Al-Ibraheem, A.; Buck, A.; Krause, B.J.; Scheidhauer, K.; Schwaiger, M. Clinical Applications of FDG PET and PET/CT in Head and Neck Cancer. J. Oncol. 2009, 2009, 208725. [Google Scholar] [CrossRef]
- Kitajima, K.; Suenaga, Y.; Kanda, T.; Miyawaki, D.; Yoshida, K.; Ejima, Y.; Sasaki, R.; Komatsu, H.; Saito, M.; Otsuki, N.; et al. Prognostic value of FDG PET imaging in patients with laryngeal cancer. PLoS ONE 2014, 9, e96999. [Google Scholar] [CrossRef]
- Suzuki, H.; Tamaki, T.; Terada, H.; Nishio, M.; Nishikawa, D.; Beppu, S.; Sawabe, M.; Hanai, N. Total lesion glycolysis as a predictor of clinical T3-4a laryngeal cancer with laryngectomy or nonlaryngectomy. Medicine 2021, 100, e27427. [Google Scholar] [CrossRef]
- Ferrari, C.; Santo, G.; Mammucci, P.; Rubini, D.; Sciacqua, A.; Sardaro, A.; Pisani, A.R.; Rubini, G. [(18)F]FDG PET/CT in head and neck squamous cell carcinoma: A head-to-head between visual point-scales and the added value of multi-modality imaging. BMC Med. Imaging 2023, 23, 34. [Google Scholar] [CrossRef]
- Zhang, B.; Li, X.; Lu, X. Standardized uptake value is of prognostic value for outcome in head and neck squamous cell carcinoma. Acta Otolaryngol. 2010, 130, 756–762. [Google Scholar] [CrossRef]
- Wang, L.; Bai, J.; Duan, P. Prognostic value of 18F-FDG PET/CT functional parameters in patients with head and neck cancer: A meta-analysis. Nucl. Med. Commun. 2019, 40, 361–369. [Google Scholar] [CrossRef]
- Ryan, J.L.; Aaron, V.D.; Sims, J.B. PET/MRI vs PET/CT in Head and Neck Imaging: When, Why, and How? Semin. Ultrasound CT MR 2019, 40, 376–390. [Google Scholar] [CrossRef]
- Pak, K.; Cheon, G.J.; Nam, H.Y.; Kim, S.J.; Kang, K.W.; Chung, J.K.; Kim, E.E.; Lee, D.S. Prognostic value of metabolic tumor volume and total lesion glycolysis in head and neck cancer: A systematic review and meta-analysis. J. Nucl. Med. 2014, 55, 884–890. [Google Scholar] [CrossRef]
- Peng, Z.; Wang, Y.; Wang, Y.; Jiang, S.; Fan, R.; Zhang, H.; Jiang, W. Application of radiomics and machine learning in head and neck cancers. Int. J. Biol. Sci. 2021, 17, 475–486. [Google Scholar] [CrossRef]
- Liu, Z.; Cao, Y.; Diao, W.; Cheng, Y.; Jia, Z.; Peng, X. Radiomics-based prediction of survival in patients with head and neck squamous cell carcinoma based on pre- and post-treatment (18)F-PET/CT. Aging 2020, 12, 14593–14619. [Google Scholar] [CrossRef]
- Zhong, J.; Frood, R.; Brown, P.; Nelstrop, H.; Prestwich, R.; McDermott, G.; Currie, S.; Vaidyanathan, S.; Scarsbrook, A.F. Machine learning-based FDG PET-CT radiomics for outcome prediction in larynx and hypopharynx squamous cell carcinoma. Clin. Radiol. 2021, 76, 78.e9–78.e17. [Google Scholar] [CrossRef]
- Ermongkonchai, T.; Khor, R.; Wada, M.; Lau, E.; Xing, D.T.; Ng, S.P. A review of diffusion-weighted magnetic resonance imaging in head and neck cancer patients for treatment evaluation and prediction of radiation-induced xerostomia. Radiat. Oncol. 2023, 18, 20. [Google Scholar] [CrossRef]



| Demographics | |
|---|---|
| Age (in Years) | |
| Median | 58.5 years |
| Range | 45–85 years |
| Gender (Number, Percentage) | |
| Male | 67, 98.5% |
| Female | 1, 1.5% |
| Histopathological Characteristics | |
| Tumor Site (Number, Percentage) | |
| Glottic | 39, 57.4% |
| Supraglottic | 26, 38.2% |
| Subglottic | 3, 4.4% |
| Tumor Size (Cm Mean & Range) | 3.8 cm, (1.5–7.5 cm) |
| T-Category (Number, Percentage) | |
| T1 | 0 |
| T2 | 2, 3% |
| T3 | 10, 15% |
| T4 | 56, 82% |
| N-Category (Number, Percentage) | |
| N0 | 37, 55% |
| N1 | 13, 19% |
| N2 | 11, 16% |
| N3 | 7, 10% |
| Tumor Grade (Number, Percentage) | |
| Well differentiated | 4, 6% |
| Well–moderately differentiated | 1, 1.5% |
| Moderately differentiated | 43, 63.2% |
| Moderate–poorly differentiated | 10, 14.7% |
| Poorly differentiated | 10, 14.7% |
| Treatment Modality (Number, Percentage) | |
| Total laryngectomy | 68, 100% |
| Bilateral neck dissection | 51, 75% |
| Unilateral neck dissection | 17, 25% |
| Adjuvant chemoradiation | 11, 16% |
| Adjuvant local radiotherapy | 9, 13% |
| Neck-Dissection Side | [18F]FDG PET/CT | Neck MRI |
|---|---|---|
| Right | -TP 1: 22 | -TP: 16 |
| -FN 2: 1 | -FN: 7 | |
| -TN 3: 24 | -TN: 28 | |
| -FP 4: 17 | -FP: 13 | |
| -Sensitivity: 95.7% | -Sensitivity: 69.6% | |
| -Specificity: 58.5% | -Specificity: 68.3% | |
| -PPV 5: 56.4% | -PPV: 55.2% | |
| -NPV 6: 96% | -NPV: 80% | |
| -Accuracy: 71.9% | -Accuracy: 68.8% | |
| Left | -TP: 21 | -TP: 16 |
| -FN: 1 | -FN: 6 | |
| -TN: 20 | -TN: 18 | |
| -FP: 13 | -FP: 15 | |
| -Sensitivity: 95.5% | -Sensitivity: 72.7% | |
| -Specificity: 60.6% | -Specificity: 54.5% | |
| -PPV: 61.8% | -PPV: 51.6% | |
| -NPV: 95.2% | -NPV: 75% | |
| -Accuracy: 74.5% | -Accuracy: 61.8% | |
| Overall | -TP: 30 | -TP: 22 |
| -FN: 2 | -FN: 10 | |
| -TN: 21 | -TN: 22 | |
| -FP: 15 | -FP: 14 | |
| -Sensitivity: 93.8% | -Sensitivity: 68.8% | |
| -Specificity: 58.3% | -Specificity: 61.1% | |
| -PPV: 66.7% | -PPV: 61.1% | |
| -NPV: 91.3% | -NPV: 68.8% | |
| -Accuracy: 75% | -Accuracy: 64.7% | |
| McNemar Test 0.022 | ||
| Parameter | ROC Curve for PFS | ||||
|---|---|---|---|---|---|
| Cutoff | AUC 1 (95% CI) | p-Value | Sensitivity | Specificity | |
| SUVmax | 16.8 | 0.656 (0.532–0.767) | 0.029 | 65.2% | 71.7% |
| TLG | 102.3 | 0.707 (0.585–0.810) | 0.001 | 82.6% | 69.6% |
| MTV | 11.7 | 0.827 (0.717–0.907) | <0.001 | 91.3% | 71.7% |
| ROC Curve for OS | |||||
| Cutoff | AUC (95% CI) | p-Value | Sensitivity | Specificity | |
| SUVmax | 16.8 | 0.637 (0.512–0.749) | 0.105 | 70.6% | 69.2% |
| TLG | 102.3 | 0.683 (0.560–0.790) | 0.009 | 88.2% | 65.4% |
| MTV | 11.7 | 0.767 (0.650–0.860) | <0.001 | 88.2% | 65.4% |
| Criterion | Univariate Analysis | Multivariate Analysis | ||
|---|---|---|---|---|
| p-Value | HR 1 (95% CI) | p Value | HR 1 (95% CI) | |
| PFS | ||||
| Age | 0.437 | 1.277 (0.689–2.366) | ||
| Tumor site | 0.883 | 0.972 (0.662–1.425) | ||
| Tumor grade | 0.071 | 0.674 (0.439–1.034) | ||
| Smoking | 0.282 | 0.775 (0.488–1.233) | ||
| SUVmax | 0.003 | 3.640 (1.530–8.662) | 0.734 | 1.182 (0.452–3.093) |
| TLG | 0.001 | 8.049 (2.704–23.961) | 0.021 | 4.241 (1.240–14.502) |
| MTV | <0.001 | 11.994 (3.536–40.682) | 0.002 | 7.504 (2.107–26.720) |
| OS | ||||
| Age | 0.315 | 1.454 (0.701–3.019) | ||
| Tumor site | 0.038 | 0.551 (0.315–0.966) | 0.079 | 0.571 (0.305–1.068) |
| Tumor grade | 0.109 | 0.677 (0.420–1.091) | ||
| Smoking | 0.041 | 0.536 (0.295–0.975) | 0.742 | 0.901 (0.484–1.068) |
| SUVmax | 0.008 | 4.275 (1.473–12.409) | 0.820 | 1.162 (0.318–4.246) |
| TLG | 0.002 | 10.539 (2.394–46.398) | 0.070 | 5.009 (0.874–28.694) |
| MTV | 0.003 | 9.337 (2.132–40.881) | 0.117 | 3.716 (0.718–19.228) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Al-Ibraheem, A.; Abdlkadir, A.S.; Al-Adhami, D.; Hejleh, T.A.; Mansour, A.; Mohamad, I.; Juweid, M.E.; Al-Rasheed, U.; Al-Hajaj, N.; Laban, D.A.; et al. The Prognostic and Diagnostic Value of [18F]FDG PET/CT in Untreated Laryngeal Carcinoma. J. Clin. Med. 2023, 12, 3514. https://doi.org/10.3390/jcm12103514
Al-Ibraheem A, Abdlkadir AS, Al-Adhami D, Hejleh TA, Mansour A, Mohamad I, Juweid ME, Al-Rasheed U, Al-Hajaj N, Laban DA, et al. The Prognostic and Diagnostic Value of [18F]FDG PET/CT in Untreated Laryngeal Carcinoma. Journal of Clinical Medicine. 2023; 12(10):3514. https://doi.org/10.3390/jcm12103514
Chicago/Turabian StyleAl-Ibraheem, Akram, Ahmed Saad Abdlkadir, Dhuha Al-Adhami, Taher Abu Hejleh, Asem Mansour, Issa Mohamad, Malik E. Juweid, Ula Al-Rasheed, Nabeela Al-Hajaj, Dima Abu Laban, and et al. 2023. "The Prognostic and Diagnostic Value of [18F]FDG PET/CT in Untreated Laryngeal Carcinoma" Journal of Clinical Medicine 12, no. 10: 3514. https://doi.org/10.3390/jcm12103514






