Brodalumab for the Treatment of Moderate-to-Severe Psoriasis: An Expert Delphi Consensus Statement
Abstract
:1. Introduction
2. Methods
2.1. Study Aims
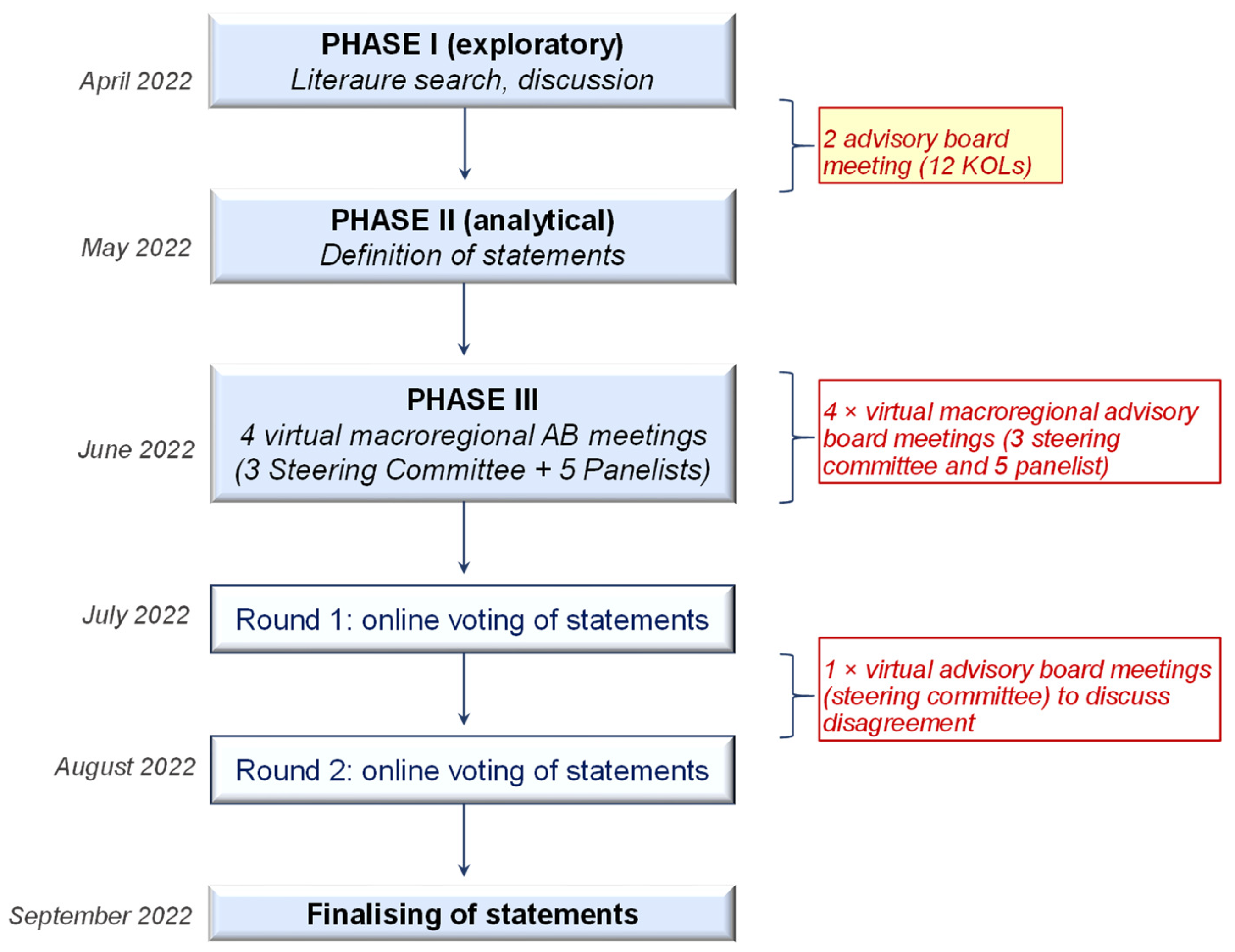
2.2. Study Design
- (a)
- Phase I (exploratory phase): The steering committee was responsible for the preliminary literature review and subsequent development of statements to be included and the definition of a cut-off value for cumulative agreement. Statements characterizing brodalumab were developed through two virtual advisory board meetings, upstream of which a bibliographic search was carried out on the use of brodalumab in psoriasis, shared with the steering committee as a basis for discussion and eventual revision.
- (b)
- Phase II (analytical phase): Statements were developed by the steering committee.
- (c)
- Phase III: A series of 4 macro-regional virtual meetings were undertaken, each having the participation of 8 KOLs: 3 steering committee members and 5 panelists.
2.3. Scientific Board
2.4. Literature Review
2.5. First and Second Round Online Delphi Voting
3. Results
3.1. Literature Search
3.2. Development of Statements and Delphi Voting
4. Discussion
4.1. Main Principles (Statements 1–5)
4.2. Consensus Statements (No. 1–10)
Comments specific to statement No. 1: “Brodalumab, with its unique mechanism of action, represents an appropriate therapeutic option in psoriatic patients non-responsive to anti-IL-17A agents”.
Comments specific to statement No. 2: “It is the opinion of the Expert Panel that brodalumab may also be effective in psoriatic patients non-responsive to IL-23 inhibitors”.
Comments specific to statement No. 3: “The speed of action of brodalumab makes it an appropriate choice in patients where a rapid therapeutic response is necessary”.
Comments specific to statement No. 4: “Brodalumab, due to its rapid action on itching, represents an appropriate therapeutic choice in patients where itching affects their quality of life”.
Comments specific to statement No. 5: “Brodalumab represents an appropriate therapeutic choice when there is involvement of difficult-to-treat areas, such as scalp/nails or palmo-plantar area.”
Comments specific to statement No. 6: “Experience from clinical practice suggests that brodalumab may also be effective in erythrodermic psoriatic patients.”
Comments specific to statement No. 7: “Experience from clinical practice indicates that brodalumab may also be effective in pustular psoriasis.”
Comments specific to statement No. 8: “Brodalumab exhibits high rates of efficacy and acts with the same rapidity of action in patients undergoing retreatment after its discontinuation.”
Comments specific to statement No. 9: ”Brodalumab represents an appropriate therapeutic option in obese psoriatic patients and/or in psoriatic patients with metabolic syndrome.”
Comments specific to statement No. 10: “The presence of non-dominant arthropathy does not preclude the use of brodalumab.”
5. Study Limitations
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Gisondi, P. The multidimensional burden of psoriasis. Br. J. Dermatol. 2018, 179, 13–14. [Google Scholar] [CrossRef] [PubMed]
- Gisondi, P.; Altomare, G.; Ayala, F.; Bardazzi, F.; Bianchi, L.; Chiricozzi, A.; Costanzo, A.; Conti, A.; Dapavo, P.; De Simone, C.; et al. Italian guidelines on the systemic treatments of moderate-to-severe plaque psoriasis. J. Eur. Acad. Derm. Venereol 2017, 31, 774–790. [Google Scholar] [CrossRef] [PubMed]
- Boehncke, W.-H.; Schön, M.P. Psoriasis. Lancet 2015, 386, 983–994. [Google Scholar] [CrossRef] [PubMed]
- Feldman, S.R.; Goffe, B.; Rice, G.; Mitchell, M.; Kaur, M.; Robertson, D.; Sierka, D.; Bourret, J.A.; Evans, T.S.; Gottlieb, A. The Challenge of Managing Psoriasis: Unmet Medical Needs and Stakeholder Perspectives. Am. Health Drug Benefits 2016, 9, 504–513. [Google Scholar] [PubMed]
- Gisondi, P.; Del Giglio, M.; Girolomoni, G. Treatment Approaches to Moderate to Severe Psoriasis. Int. J. Mol. Sci. 2017, 18, 2427. [Google Scholar] [CrossRef]
- Aldredge, L.M.; Higham, R.C. Manifestations and Management of Difficult-to-Treat Psoriasis. J. Dermatol. Nurses’ Assoc. 2018, 10, 189–197. [Google Scholar] [CrossRef]
- Armstrong, A.W.; Puig, L.; Joshi, A.; Skup, M.; Williams, D.; Li, J.; Betts, K.A.; Augustin, M. Comparison of Biologics and Oral Treatments for Plaque Psoriasis: A Meta-analysis. JAMA Derm. 2020, 156, 258–269. [Google Scholar] [CrossRef]
- Papp, K.A.; Merola, J.F.; Gottlieb, A.B.; Griffiths, C.E.M.; Cross, N.; Peterson, L.; Cioffi, C.; Blauvelt, A. Dual neutralization of both interleukin 17A and interleukin 17F with bimekizumab in patients with psoriasis: Results from BE ABLE 1, a 12-week randomized, double-blinded, placebo-controlled phase 2b trial. J. Am. Acad. Derm. 2018, 79, 277–286.e10. [Google Scholar] [CrossRef]
- Naik, G.S.; Ming, W.K.; Magodoro, I.M.; Akinwunmi, B.; Dar, S.; Poulsen, H.E.; Kristensen, L.E.; Ellervik, C. Th17 Inhibitors in Active Psoriatic Arthritis: A Systematic Review and Meta-Analysis of Randomized Controlled Clinical Trials. Dermatology 2017, 233, 366–377. [Google Scholar] [CrossRef]
- Gisondi, P.; Fargnoli, M.C.; Amerio, P.; Argenziano, G.; Bardazzi, F.; Bianchi, L.; Chiricozzi, A.; Conti, A.; Corazza, M.; Costanzo, A.; et al. Italian adaptation of EuroGuiDerm guideline on the systemic treatment of chronic plaque psoriasis. Ital. J. Derm. Venerol. 2022, 157, 1–78. [Google Scholar] [CrossRef]
- Nast, A.; Smith, C.; Spuls, P.I.; Avila Valle, G.; Bata-Csörgö, Z.; Boonen, H.; De Jong, E.M.; Garcia-Doval, I.; Gisondi, P.; Kaur-Knudsen, D.; et al. EuroGuiDerm Guideline on the systemic treatment of Psoriasis vulgaris—Part 1: Treatment and monitoring recommendations. J. Eur. Acad. Dermatol. Venereol. 2020, 34, 2461–2498. [Google Scholar] [CrossRef] [PubMed]
- Prignano, F.; Pescitelli, L.; Trovato, E.; DI Cesare, A.; Cuccia, A.; Mazzatenta, C.; Pellegrino, M.; Marsili, F.; Castelli, A.; Brandini, L.; et al. Tuscany consensus for the treatment of moderate-severe psoriasis: Update and focus on practical guidelines for place in therapy of anti-IL-17 and anti-IL-23 biologics. Ital. J. Dermatol. Venereol. 2022, 157, 469–479. [Google Scholar] [CrossRef] [PubMed]
- European Medicines Agency Kyntheum|European Medicines Agency. Available online: https://www.ema.europa.eu/en/medicines/human/EPAR/kyntheum (accessed on 20 April 2021).
- Papp, K.A.; Reid, C.; Foley, P.; Sinclair, R.; Salinger, D.H.; Williams, G.; Dong, H.; Krueger, J.G.; Russell, C.B.; Martin, D.A. Anti-IL-17 receptor antibody AMG 827 leads to rapid clinical response in subjects with moderate to severe psoriasis: Results from a phase I, randomized, placebo-controlled trial. J. Investig. Dermatol. 2012, 132, 2466–2469. [Google Scholar] [CrossRef]
- Russell, C.B.; Rand, H.; Bigler, J.; Kerkof, K.; Timour, M.; Bautista, E.; Krueger, J.G.; Salinger, D.H.; Welcher, A.A.; Martin, D.A. Gene expression profiles normalized in psoriatic skin by treatment with brodalumab, a human anti-IL-17 receptor monoclonal antibody. J. Immunol. 2014, 192, 3828–3836. [Google Scholar] [CrossRef] [PubMed]
- Martin, D.A.; Towne, J.E.; Kricorian, G.; Klekotka, P.; Gudjonsson, J.E.; Krueger, J.G.; Russell, C.B. The emerging role of IL-17 in the pathogenesis of psoriasis: Preclinical and clinical findings. J. Investig. Derm. 2013, 133, 17–26. [Google Scholar] [CrossRef] [PubMed]
- Papp, K.A.; Leonardi, C.; Menter, A.; Ortonne, J.-P.; Krueger, J.G.; Kricorian, G.; Aras, G.; Li, J.; Russell, C.B.; Thompson, E.H.Z.; et al. Brodalumab, an Anti–Interleukin-17–Receptor Antibody for Psoriasis. N. Engl. J. Med. 2012, 366, 1181–1189. [Google Scholar] [CrossRef]
- Green, L.; Weinberg, J.M.; Menter, A.; Soung, J.; Lain, E.; Jacobson, A. Clinical and Molecular Effects of Interleukin-17 Pathway Blockade in Psoriasis. J. Drugs Derm. 2020, 19, 138–143. [Google Scholar] [CrossRef]
- Pinter, A.; Bonnekoh, B.; Hadshiew, I.M.; Zimmer, S. Brodalumab for the treatment of moderate-to-severe psoriasis: Case series and literature review. Clin. Cosmet. Investig. Dermatol. 2019, 12, 509–517. [Google Scholar] [CrossRef]
- Langley, R.G.; Armstrong, A.W.; Lebwohl, M.G.; Blauvelt, A.; Hsu, S.; Tyring, S.; Rastogi, S.; Pillai, R.; Israel, R. Efficacy and safety of brodalumab in patients with psoriasis who had inadequate responses to ustekinumab: Subgroup analysis of two randomized phase III trials. Br. J. Dermatol. 2019, 180, 306–314. [Google Scholar] [CrossRef]
- Tollenaere, M.A.X.; Hebsgaard, J.; Ewald, D.A.; Lovato, P.; Garcet, S.; Li, X.; Pilger, S.D.; Tiirikainen, M.L.; Bertelsen, M.; Krueger, J.G.; et al. Signalling of multiple interleukin (IL)-17 family cytokines via IL-17 receptor A drives psoriasis-related inflammatory pathways. Br. J. Dermatol. 2021, 185, 585–594. [Google Scholar] [CrossRef]
- Kimmel, G.; Chima, M.; Kim, H.J.; Bares, J.; Yao, C.J.; Singer, G.; Kim, S.J.; Bagel, J.; Lebwohl, M. Brodalumab in the treatment of moderate to severe psoriasis in patients when previous anti-interleukin 17A therapies have failed. J. Am. Acad. Derm. 2019, 81, 857–859. [Google Scholar] [CrossRef]
- Papp, K.A.; Reich, K.; Paul, C.; Blauvelt, A.; Baran, W.; Bolduc, C.; Toth, D.; Langley, R.G.; Cather, J.; Gottlieb, A.B.; et al. A prospective phase III, randomized, double-blind, placebo-controlled study of brodalumab in patients with moderate-to-severe plaque psoriasis. Br. J. Derm. 2016, 175, 273–286. [Google Scholar] [CrossRef] [PubMed]
- Lebwohl, M.; Strober, B.; Menter, A.; Gordon, K.; Weglowska, J.; Puig, L.; Papp, K.; Spelman, L.; Toth, D.; Kerdel, F.; et al. Phase 3 Studies Comparing Brodalumab with Ustekinumab in Psoriasis. N. Engl. J. Med. 2015, 373, 1318–1328. [Google Scholar] [CrossRef] [PubMed]
- Sawyer, L.; Fotheringham, I.; Wright, E.; Yasmeen, N.; Gibbons, C.; Holmen Møller, A. The comparative efficacy of brodalumab in patients with moderate-to-severe psoriasis: A systematic literature review and network meta-analysis. J. Dermatol. Treat. 2018, 29, 557–568. [Google Scholar] [CrossRef] [PubMed]
- Blauvelt, A.; Papp, K.A.; Lebwohl, M.G.; Green, L.J.; Hsu, S.; Bhatt, V.; Rastogi, S.; Pillai, R.; Israel, R. Rapid onset of action in patients with moderate-to-severe psoriasis treated with brodalumab: A pooled analysis of data from two phase 3 randomized clinical trials (AMAGINE-2 and AMAGINE-3). J. Am. Acad. Derm. 2017, 77, 372–374. [Google Scholar] [CrossRef]
- Lebwohl, M.; Koo, J.; Leonardi, C.; Armstrong, A.; Rawnsley, N.; Goehring, E.; Jacobson, A. Brodalumab: 4-Year US Pharmacovigilance Report. J. Drugs Derm. 2023, 22, 419–422. [Google Scholar] [CrossRef]
- Egeberg, A.; Andersen, Y.M.F.; Halling-Overgaard, A.-S.; Alignahi, F.; Thyssen, J.P.; Burge, R.; Mallbris, L. Systematic review on rapidity of onset of action for interleukin-17 and interleukin-23 inhibitors for psoriasis. J. Eur. Acad. Derm. Venereol. 2020, 34, 39–46. [Google Scholar] [CrossRef]
- Gottlieb, A.B.; Gordon, K.; Hsu, S.; Elewski, B.; Eichenfield, L.F.; Kircik, L.; Rastogi, S.; Pillai, R.; Israel, R. Improvement in itch and other psoriasis symptoms with brodalumab in phase 3 randomized controlled trials. J. Eur. Acad. Derm. Venereol. 2018, 32, 1305–1313. [Google Scholar] [CrossRef]
- Elewski, B.; Rich, P.; Lain, E.; Soung, J.; Lewitt, G.M.; Jacobson, A. Efficacy of brodalumab in the treatment of scalp and nail psoriasis: Results from three phase 3 trials. J. Dermatol. Treat. 2022, 33, 261–265. [Google Scholar] [CrossRef]
- Brown, A.K.; O’connor, P.J.; Roberts, T.E.; Wakefield, R.J.; Karim, Z.; Emery, P. Recommendations for musculoskeletal ultrasonography by rheumatologists: Setting global standards for best practice by expert consensus. Arthritis Rheum. 2005, 53, 83–92. [Google Scholar] [CrossRef]
- Zafar, S.Y.; Currow, D.C.; Cherny, N.; Strasser, F.; Fowler, R.; Abernethy, A.P. Consensus-based standards for best supportive care in clinical trials in advanced cancer. Lancet Oncol. 2012, 13, e77–e82. [Google Scholar] [CrossRef] [PubMed]
- Mahler, D.A.; Selecky, P.A.; Harrod, C.G.; Benditt, J.O.; Carrieri-Kohlman, V.; Curtis, J.R.; Manning, H.L.; Mularski, R.A.; Varkey, B.; Campbell, M.; et al. American College of Chest Physicians consensus statement on the management of dyspnea in patients with advanced lung or heart disease. Chest 2010, 137, 674–691. [Google Scholar] [CrossRef] [PubMed]
- SILIQ™ (Brodalumab) Injection, for Subcutaneous Use Initial U.S. Approval: 2017. Available online: https://www.accessdata.fda.gov/drugsatfda_docs/label/2017/761032lbl.pdf (accessed on 5 October 2022).
- Foglio Illustrativo: Informazioni per il Paziente Kyntheum 210 mg Soluzione Iniettabile in Siringa Preriempita Brodalumab. Available online: https://farmaci.agenziafarmaco.gov.it/aifa/servlet/PdfDownloadServlet?pdfFileName=footer_000819_045484_FI.pdf&sys=m0b1l3 (accessed on 12 November 2022).
- Fresegna, D.; Bullitta, S.; Musella, A.; Rizzo, F.R.; De Vito, F.; Guadalupi, L.; Caioli, S.; Balletta, S.; Sanna, K.; Dolcetti, E.; et al. Re-Examining the Role of TNF in MS Pathogenesis and Therapy. Cells 2020, 9, 2290. [Google Scholar] [CrossRef]
- Kunchok, A.; Aksamit, A.J., Jr.; Davis, J.M., III; Kantarci, O.H.; Keegan, B.M.; Pittock, S.J.; Weinshenker, B.G.; McKeon, A. Association Between Tumor Necrosis Factor Inhibitor Exposure and Inflammatory Central Nervous System Events. JAMA Neurol. 2020, 77, 937–946. [Google Scholar] [CrossRef] [PubMed]
- Chung, E.S.; Packer, M.; Lo, K.H.; Fasanmade, A.A.; Willerson, J.T. Anti-TNF Therapy Against Congestive Heart Failure Investigators Randomized, double-blind, placebo-controlled, pilot trial of infliximab, a chimeric monoclonal antibody to tumor necrosis factor-alpha, in patients with moderate-to-severe heart failure: Results of the anti-TNF Therapy Against Congestive Heart Failure (ATTACH) trial. Circulation 2003, 107, 3133–3140. [Google Scholar] [CrossRef]
- Sinagra, E.; Perricone, G.; Romano, C.; Cottone, M. Heart failure and anti tumor necrosis factor-alpha in systemic chronic inflammatory diseases. Eur. J. Intern. Med. 2013, 24, 385–392. [Google Scholar] [CrossRef]
- Papp, K.; Menter, A.; Leonardi, C.; Soung, J.; Weiss, S.; Pillai, R.; Jacobson, A. Long-term efficacy and safety of brodalumab in psoriasis through 120 weeks and after withdrawal and retreatment: Subgroup analysis of a randomized phase III trial (AMAGINE-1). Br. J. Derm. 2020, 183, 1037–1048. [Google Scholar] [CrossRef]
- Foulkes, A.C.; Warren, R.B. Brodalumab in psoriasis: Evidence to date and clinical potential. Drugs Context 2019, 8, 212570. [Google Scholar] [CrossRef]
- Warren, R.B.; Hansen, J.B.; Reich, K.; Paul, C.; Puig, L. Complete clearance and psoriasis area and severity index response for brodalumab and ustekinumab in AMAGINE-2 and -3. J. Eur. Acad. Dermatol. Venereol. 2021, 35, 450–457. [Google Scholar] [CrossRef]
- Kokolakis, G.; Vadstrup, K.; Hansen, J.B.; Carrascosa, J.M. Increased Skin Clearance and Quality of Life Improvement with Brodalumab Compared with Ustekinumab in Psoriasis Patients with Aggravating Lifestyle Factors. Dermatol. Ther. 2021, 11, 2027–2042. [Google Scholar] [CrossRef]
- Saunte, D.M.; Mrowietz, U.; Puig, L.; Zachariae, C. Candida infections in patients with psoriasis and psoriatic arthritis treated with interleukin-17 inhibitors and their practical management. Br. J. Derm. 2017, 177, 47–62. [Google Scholar] [CrossRef] [PubMed]
- Davidson, L.; van den Reek, J.M.P.A.; Bruno, M.; van Hunsel, F.; Herings, R.M.C.; Matzaraki, V.; Boahen, C.K.; Kumar, V.; Groenewoud, H.M.M.; van de Veerdonk, F.L.; et al. Risk of candidiasis associated with interleukin-17 inhibitors: A real-world observational study of multiple independent sources. Lancet Reg. Health Eur. 2022, 13, 100266. [Google Scholar] [CrossRef] [PubMed]
- Puig, L.; Lebwohl, M.; Bachelez, H.; Sobell, J.; Jacobson, A.A. Long-term efficacy and safety of brodalumab in the treatment of psoriasis: 120-week results from the randomized, double-blind, placebo- and active comparator-controlled phase 3 AMAGINE-2 trial. J. Am. Acad. Derm. 2020, 82, 352–359. [Google Scholar] [CrossRef] [PubMed]
- Yeung, J.; Bunce, P.E.; Lynde, C.W.; Turchin, I.; Vender, R.B. Review and Practical Guidance on Managing Fungal Infections in Patients With Psoriasis Receiving Anti-IL-17 Therapies. J. Cutan. Med. Surg. 2022, 26, 3S–23S. [Google Scholar] [CrossRef]
- Roman, M.; Chiu, M.W. Spotlight on brodalumab in the treatment of moderate-to-severe plaque psoriasis: Design, development, and potential place in therapy. Drug Des. Dev. Ther. 2017, 11, 2065–2075. [Google Scholar] [CrossRef]
- Yeung, J.; Vender, R.; Turchin, I.; Shukla, R.; Maari, C.; Hong, C.-H.; Barakat, M.; Lansang, P. Brodalumab success in patients with moderate-to-severe psoriasis who failed previous interleukin-17A inhibitors. J. Am. Acad. Derm. 2021, 84, 1169–1171. [Google Scholar] [CrossRef]
- Loft, N.; Bregnhøj, A.; Fage, S.; Nielsen, C.H.; Enevold, C.; Zachariae, C.; Iversen, L.; Skov, L. Effectiveness of brodalumab after previous treatment failure of interleukin-17A inhibitors in patients with psoriasis. Dermatol. Ther. 2021, 34, e15106. [Google Scholar] [CrossRef]
- Miyagawa, F. Pathogenesis of Paradoxical Reactions Associated with Targeted Biologic Agents for Inflammatory Skin Diseases. Biomedicines 2022, 10, 1485. [Google Scholar] [CrossRef]
- Menter, A.; Armstrong, A.; Van Voorhees, A.; Liu, C.; Jacobson, A. Brodalumab to the Rescue: Efficacy and Safety of Brodalumab in Patients with Psoriasis and Prior Exposure or Inadequate Response to Biologics. Dermatol. Ther. 2020, 10, 615–621. [Google Scholar] [CrossRef]
- Reich, A.; Szepietowski, J.C. Clinical Aspects of Itch: Psoriasis. In Itch: Mechanisms and Treatment; Carstens, E., Akiyama, T., Eds.; Frontiers in Neuroscience; CRC Press/Taylor & Francis: Boca Raton, FL, USA, 2014; ISBN 978-1-4665-0543-8. [Google Scholar]
- Prignano, F.; Ricceri, F.; Pescitelli, L.; Lotti, T. Itch in psoriasis: Epidemiology, clinical aspects and treatment options. Clin. Cosmet. Investig. Dermatol. 2009, 2, 9–13. [Google Scholar] [CrossRef]
- Galluzzo, M.; Caldarola, G.; De Simone, C.; Bernardini, N.; Moretta, G.; Pallotta, S.; Botti, E.; Campione, E.; Pirro, F.; Potenza, C.; et al. Use of brodalumab for the treatment of chronic plaque psoriasis: A one-year real-life study in the Lazio region, Italy. Expert Opin. Biol. Ther. 2021, 21, 1299–1310. [Google Scholar] [CrossRef]
- Callis Duffin, K.; Mason, M.A.; Gordon, K.; Harrison, R.W.; Crabtree, M.M.; Guana, A.; Germino, R.; Lebwohl, M. Characterization of Patients with Psoriasis in Challenging-to-Treat Body Areas in the Corrona Psoriasis Registry. DRM 2021, 237, 46–55. [Google Scholar] [CrossRef] [PubMed]
- Nicolescu, A.C.; Ionescu, M.-A.; Constantin, M.M.; Ancuta, I.; Ionescu, S.; Niculet, E.; Tatu, A.L.; Zirpel, H.; Thaçi, D. Psoriasis Management Challenges Regarding Difficult-to-Treat Areas: Therapeutic Decision and Effectiveness. Life 2022, 12, 2050. [Google Scholar] [CrossRef] [PubMed]
- Sarma, N. Evidence and Suggested Therapeutic Approach in Psoriasis of Difficult-to-treat Areas: Palmoplantar Psoriasis, Nail Psoriasis, Scalp Psoriasis, and Intertriginous Psoriasis. Indian J Derm. 2017, 62, 113–122. [Google Scholar] [CrossRef] [PubMed]
- Blakely, K.; Gooderham, M. Management of scalp psoriasis: Current perspectives. Psoriasis 2016, 6, 33–40. [Google Scholar] [CrossRef]
- Lanna, C.; Galluzzi, C.; Zangrilli, A.; Bavetta, M.; Bianchi, L.; Campione, E. Psoriasis in difficult to treat areas: Treatment role in improving health-related quality of life and perception of the disease stigma. J. Dermatol. Treat. 2022, 33, 531–534. [Google Scholar] [CrossRef]
- Schons, K.R.R.; Knob, C.F.; Murussi, N.; Beber, A.A.C.; Neumaier, W.; Monticielo, O.A. Nail psoriasis: A review of the literature. An. Bras. Dermatol. 2014, 89, 312–317. [Google Scholar] [CrossRef]
- Crowley, J.J.; Weinberg, J.M.; Wu, J.J.; Robertson, A.D.; Van Voorhees, A.S. National Psoriasis Foundation Treatment of nail psoriasis: Best practice recommendations from the Medical Board of the National Psoriasis Foundation. JAMA Derm. 2015, 151, 87–94. [Google Scholar] [CrossRef]
- Meeuwis, K.A.P.; Potts Bleakman, A.; van de Kerkhof, P.C.M.; Dutronc, Y.; Henneges, C.; Kornberg, L.J.; Menter, A. Prevalence of genital psoriasis in patients with psoriasis. J. Dermatol. Treat 2018, 29, 754–760. [Google Scholar] [CrossRef]
- Papp, K.; Menter, A.; Strober, B.; Kricorian, G.; Thompson, E.H.Z.; Milmont, C.E.; Nirula, A.; Klekotka, P. Efficacy and safety of brodalumab in subpopulations of patients with difficult-to-treat moderate-to-severe plaque psoriasis. J. Am. Acad. Derm. 2015, 72, 436–439.e1. [Google Scholar] [CrossRef]
- Menter, A.; Bhutani, T.; Ehst, B.; Elewski, B.; Jacobson, A. Narrative Review of the Emerging Therapeutic Role of Brodalumab in Difficult-to-Treat Psoriasis. Dermatol. Ther. 2022, 12, 1289–1302. [Google Scholar] [CrossRef] [PubMed]
- Segaert, S.; Andersen, J.; Nielsen, V. Efficacy of Brodalumab, an Interleukin-17 Receptor Antibody, on Clinical Signs of Moderate to Severe Plaque Psoriasis in Different Body Regions. Abstract P0457. In Proceedings of the 27th EADV Congress, Paris, France, 12−16 September 2018. [Google Scholar]
- Improvement of nail psoriasis with brodalumab in phase 3 trials. J. Am. Acad. Dermatol. 2017, 76, AB410. [CrossRef]
- Kassir, M.; Kircik, L.; Weinberg, J.; Fatima, F.; Yamauchi, P.; Lotti, T.; Wollina, U.; Grabbe, S.; Goldust, M. Treatment of Nail Psoriasis. J. Drugs Dermatol. 2022, 21, 146–150. [Google Scholar] [CrossRef] [PubMed]
- Megna, M.; Fabbrocini, G.; Ferrillo, M.; Cinelli, E. Erythrodermic psoriasis successfully and rapidly treated with brodalumab: Report of two cases. Dermatol. Ther. 2020, 33, e14351. [Google Scholar] [CrossRef]
- Yamasaki, K.; Nakagawa, H.; Kubo, Y.; Ootaki, K. Japanese Brodalumab Study Group Efficacy and safety of brodalumab in patients with generalized pustular psoriasis and psoriatic erythroderma: Results from a 52-week, open-label study. Br. J. Derm. 2017, 176, 741–751. [Google Scholar] [CrossRef]
- Bernardini, N.; Skroza, N.; Tolino, E.; Mambrin, A.; Balduzzi, V.; Marchesiello, A.; Michelini, S.; Volpe, S.; Maddalena, P.; Proietti, I.; et al. Recurrent erythrodermic psoriasis and polycythemia successfully treated with brodalumab. Dermatol. Ther. 2020, 33, e14338. [Google Scholar] [CrossRef]
- Menter, A.; Van Voorhees, A.S.; Hsu, S. Pustular Psoriasis: A Narrative Review of Recent Developments in Pathophysiology and Therapeutic Options. Dermatol. Ther. 2021, 11, 1917–1929. [Google Scholar] [CrossRef]
- Burden, A.D.; Mrowietz, U.; Skalicky, A.M.; Rentz, A.M.; Esser, D.; Gloede, T.; Thoma, C.; Menter, A. Symptom Experience and Content Validity of the Psoriasis Symptom Scale (PSS) in Patients with Generalized Pustular Psoriasis (GPP). Dermatol. Ther. 2022, 12, 1367–1381. [Google Scholar] [CrossRef]
- Armstrong, A.; Keegan, B.; Han, G.; Jacobson, A. Retreatment With Brodalumab Results in Skin Clearance and Improvements in Quality of Life in Patients with Psoriasis After Treatment Interruption. J. Ski. 2021, 5, s50. [Google Scholar] [CrossRef]
- Hsu, S.; Green, L.J.; Lebwohl, M.G.; Wu, J.J.; Blauvelt, A.; Jacobson, A.A. Comparable efficacy and safety of brodalumab in obese and nonobese patients with psoriasis: Analysis of two randomized controlled trials. Br. J. Dermatol. 2020, 182, 880–888. [Google Scholar] [CrossRef]
- Naldi, L.; Addis, A.; Chimenti, S.; Giannetti, A.; Picardo, M.; Tomino, C.; Maccarone, M.; Chatenoud, L.; Bertuccio, P.; Caggese, E.; et al. Impact of body mass index and obesity on clinical response to systemic treatment for psoriasis. Evidence from the Psocare project. Dermatology 2008, 217, 365–373. [Google Scholar] [CrossRef] [PubMed]
- Mourad, A.; Straube, S.; Armijo-Olivo, S.; Gniadecki, R. Factors predicting persistence of biologic drugs in psoriasis: A systematic review and meta-analysis. Br. J. Dermatol. 2019, 181, 450–458. [Google Scholar] [CrossRef] [PubMed]
- Kisielnicka, A.; Szczerkowska-Dobosz, A.; Nowicki, R.J. The influence of body weight of patients with chronic plaque psoriasis on biological treatment response. Adv. Dermatol. Allergol. 2020, 37, 168–173. [Google Scholar] [CrossRef]
- Strober, B.; Lain, E.; Kircik, L.; Guenthner, S.; Jacobson, A. 15908 Long-term efficacy and safety of brodalumab in patients with or without metabolic syndrome. J. Am. Acad. Dermatol. 2020, 83, AB163. [Google Scholar] [CrossRef]
- Mease, P.J.; Helliwell, P.S.; Hjuler, K.F.; Raymond, K.; McInnes, I. Brodalumab in psoriatic arthritis: Results from the randomised phase III AMVISION-1 and AMVISION-2 trials. Ann. Rheum. Dis. 2021, 80, 185–193. [Google Scholar] [CrossRef]

| No. | Domain and Description |
|---|---|
| 1 | Mechanism of action/effectiveness/safety in patients with previous failure/multifailure. Literature suggests that brodalumab may represent a good therapeutic option both in patients who are bionaïve and in patients not responsive to other biological drugs, even after primary failure, including anti IL-17A agents. |
| 2 | Effectiveness/rapidity of action and severity of disease. A rapid onset of action, as in the case of brodalumab, could be advantageous, particularly in psoriasis patients with severe disease. |
| 3 | Efficacy at different sites. Literature on the use of brodalumab on scalp and in nail psoriasis may be considered by clinicians when choosing this treatment. |
| 4 | Long-term effectiveness/recapture rate/immunogenicity patient discontinuation, relapse. Literature shows that brodalumab is an effective long-term treatment option for psoriasis even after suspension. Brodalumab shows a low incidence of immunogenicity and high rates of regaining efficacy after withdrawal. |
| 5 | Mechanism of action/effectiveness/safety in patients with comorbidities. Literature shows the multiple uses of brodalumab in a broad spectrum of patients with comorbidities such as obesity, hypertension, metabolic syndrome, and psoriatic arthritis. |
| 6 | Impact on quality of life. Treatment with brodalumab shows a positive impact on the quality of life of patients with psoriasis, both in bionaïve patients and in patients not responsive to other biological drugs, with significant improvement also with respect to aspects related to work-related issues (absenteeism, work impairment, and productivity). |
| 7 | Safety. Brodalumab has a favorable safety profile; it is safe and well tolerated both in the early and long-term, with relatively low rates of adverse events of particular concern, such as candida infection. |
| No. | Main Principles | |
| 1 | Brodalumab is indicated for the treatment of moderate-to-severe plaque psoriasis in adult patients who are candidates for systemic therapy. | Not voted on |
| 2 | Brodalumab represents an appropriate therapeutic choice in bionaïve psoriatic patients either non-responsive to conventional drugs or in whom conventional drugs are contraindicated. | Not voted on |
| 3 | Brodalumab represents an appropriate therapeutic option in psoriatic patients non-responsive to TNF-alpha inhibitors or in bionaïve psoriatic patients who have contraindications to TNF-alpha inhibitors. | Not voted on |
| 4 | Brodalumab shows a positive impact on the quality of life of psoriatic patients, both bionaïve and non-responsive to conventional treatments or other biological drugs, with significant improvements in work productivity. | Not voted on |
| 5 | Brodalumab has a favorable safety profile with few and easily manageable adverse events, such as Candida infections which do not represent a relevant clinical problem. | Not voted on |
| No. | Revised statements after Delphi voting | Final TCA (%) |
| 1 | Brodalumab, with its unique mechanism of action, represents an appropriate therapeutic option in psoriatic patients non-responsive to anti-IL-17A agents. | 93.8 |
| 2 | It is the opinion of the Expert Panel that brodalumab may also be effective in psoriatic patients non-responsive to IL-23 inhibitors. | 93.8 |
| 3 | The speed of action of brodalumab makes it an appropriate choice in patients where a rapid therapeutic response is necessary. | 96.9 |
| 4 | Brodalumab, due to its rapid action on itching, represents an appropriate therapeutic choice in patients where itching affects their quality of life. | 96.9 |
| 5 | Brodalumab represents an appropriate therapeutic choice when there is involvement of difficult-to-treat areas, such as scalp/nails or palmo-plantar area. | 96.9 |
| 6 | Experience from clinical practice suggests that brodalumab may also be effective in erythrodermic psoriatic patients. | 81.3 |
| 7 | Experience from clinical practice indicates that brodalumab may also be effective in pustular psoriasis. | 65.6 |
| 8 | Brodalumab exhibits high rates of efficacy and acts with the same rapidity of action in patients undergoing retreatment after its discontinuation. | 93.8 |
| 9 | Brodalumab represents an appropriate therapeutic option in obese psoriatic patients and/or in psoriatic patients with metabolic syndrome. | 93.8 |
| 10 | The presence of non-dominant arthropathy does not preclude the use of brodalumab. | 59.4 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fargnoli, M.C.; Bardazzi, F.; Bianchi, L.; Dapavo, P.; Fabbrocini, G.; Gisondi, P.; Micali, G.; Offidani, A.M.; Pellacani, G.; Skroza, N.; et al. Brodalumab for the Treatment of Moderate-to-Severe Psoriasis: An Expert Delphi Consensus Statement. J. Clin. Med. 2023, 12, 3545. https://doi.org/10.3390/jcm12103545
Fargnoli MC, Bardazzi F, Bianchi L, Dapavo P, Fabbrocini G, Gisondi P, Micali G, Offidani AM, Pellacani G, Skroza N, et al. Brodalumab for the Treatment of Moderate-to-Severe Psoriasis: An Expert Delphi Consensus Statement. Journal of Clinical Medicine. 2023; 12(10):3545. https://doi.org/10.3390/jcm12103545
Chicago/Turabian StyleFargnoli, Maria Concetta, Federico Bardazzi, Luca Bianchi, Paolo Dapavo, Gabriella Fabbrocini, Paolo Gisondi, Giuseppe Micali, Anna Maria Offidani, Giovanni Pellacani, Nevena Skroza, and et al. 2023. "Brodalumab for the Treatment of Moderate-to-Severe Psoriasis: An Expert Delphi Consensus Statement" Journal of Clinical Medicine 12, no. 10: 3545. https://doi.org/10.3390/jcm12103545
APA StyleFargnoli, M. C., Bardazzi, F., Bianchi, L., Dapavo, P., Fabbrocini, G., Gisondi, P., Micali, G., Offidani, A. M., Pellacani, G., Skroza, N., Angileri, R. G., Burlando, M., Campanati, A., Carrera, C. G., Chiricozzi, A., Conti, A., Simone, C. D., Di Lernia, V., Errichetti, E., ... Pinton, P. C. (2023). Brodalumab for the Treatment of Moderate-to-Severe Psoriasis: An Expert Delphi Consensus Statement. Journal of Clinical Medicine, 12(10), 3545. https://doi.org/10.3390/jcm12103545












