The Effect of Bite Raise on AHI Values in Adult Patients Affected by OSA: A Systematic Review with Meta-Regression
Abstract
1. Introduction
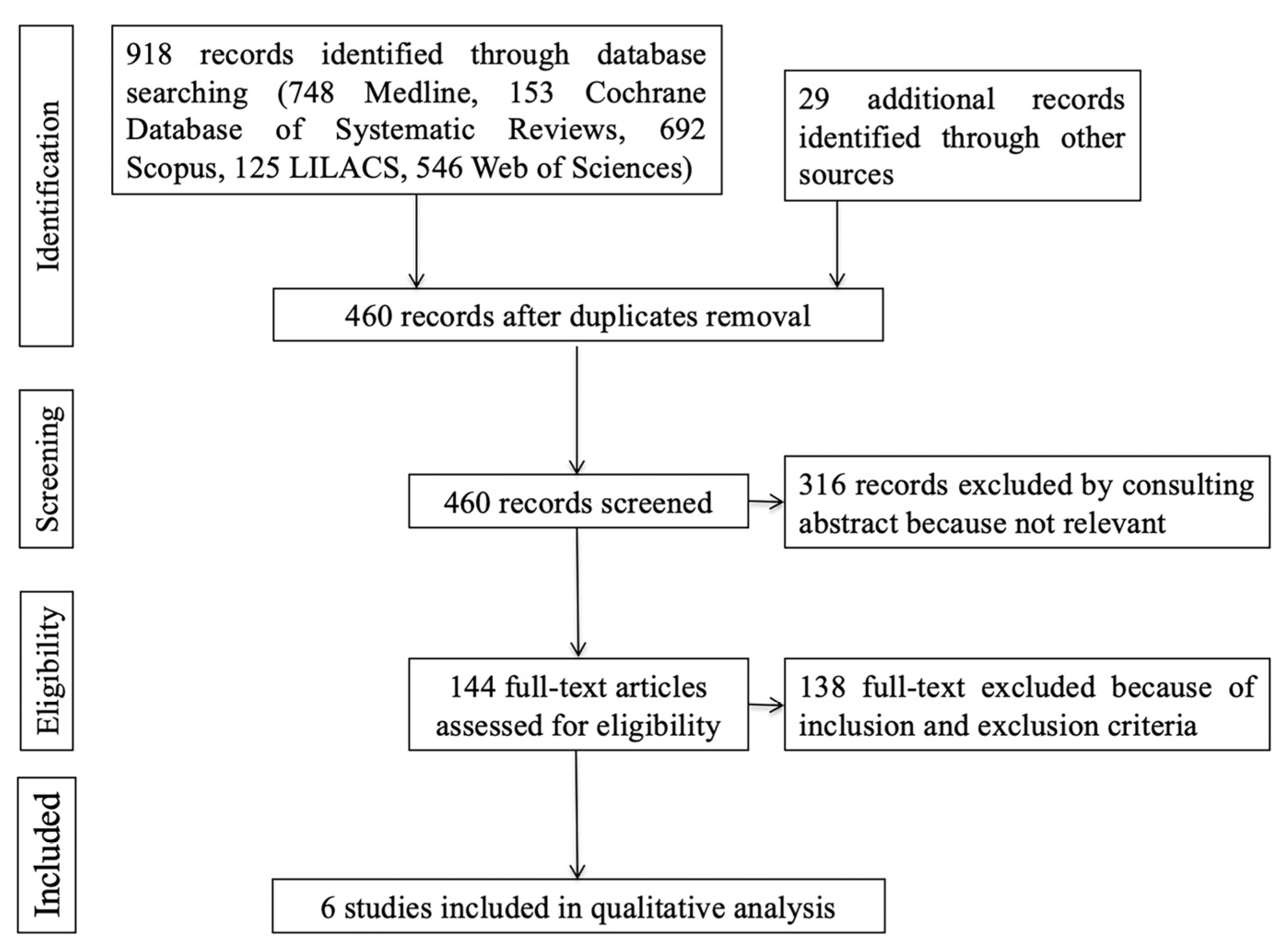
2. Materials and Methods
2.1. Search Strategy
2.2. Inclusion Criteria
2.3. Data Items and Collection
2.4. Risk of Bias in Individual Studies and across the Studies
2.5. Methodology of Synthesis of the Results of the Individual Studies
3. Results
3.1. Quality Analysis and Risk of Bias in Individual Studies
3.2. Results of Individual Studies
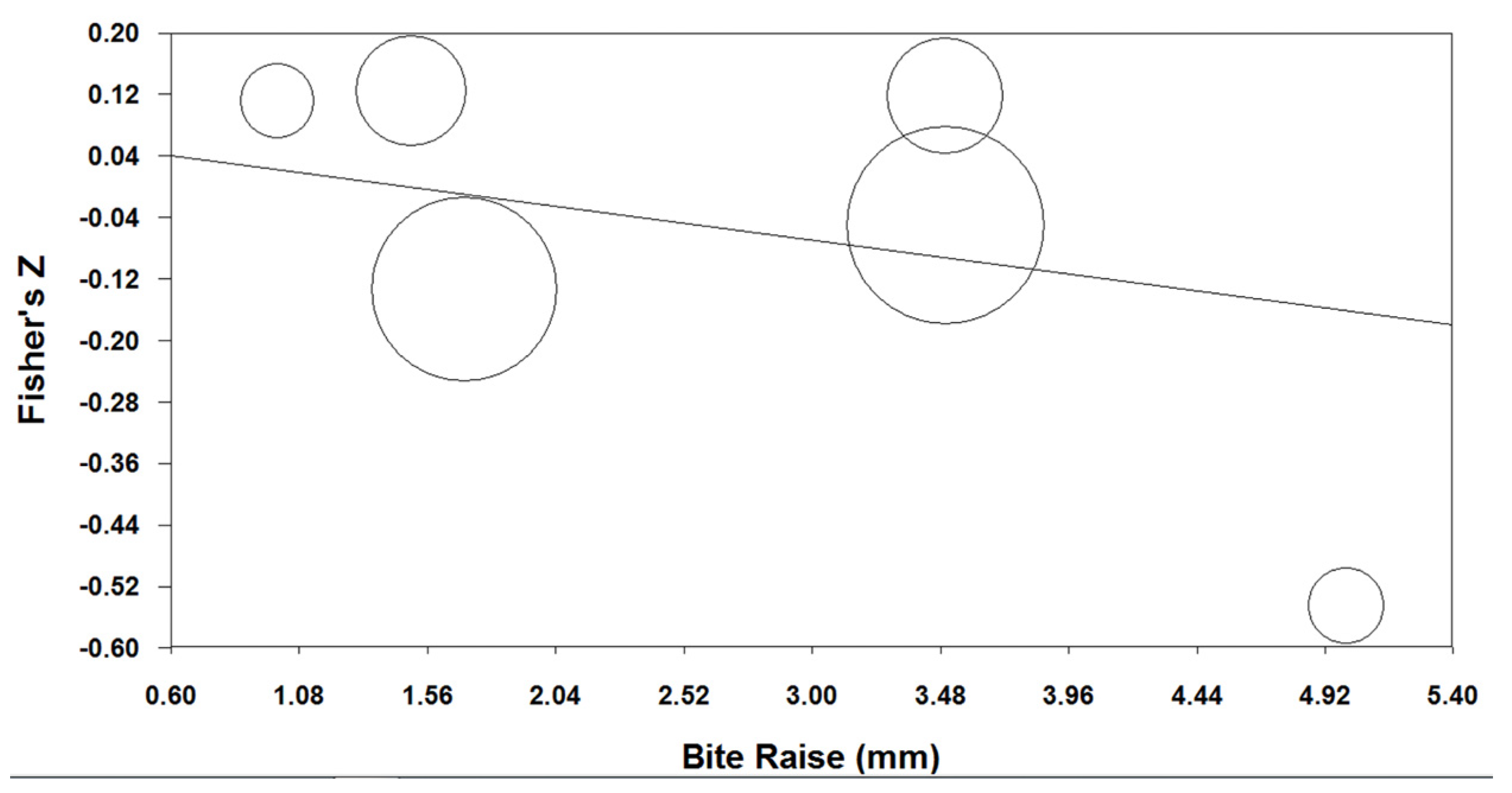
3.3. Synthesis of Results
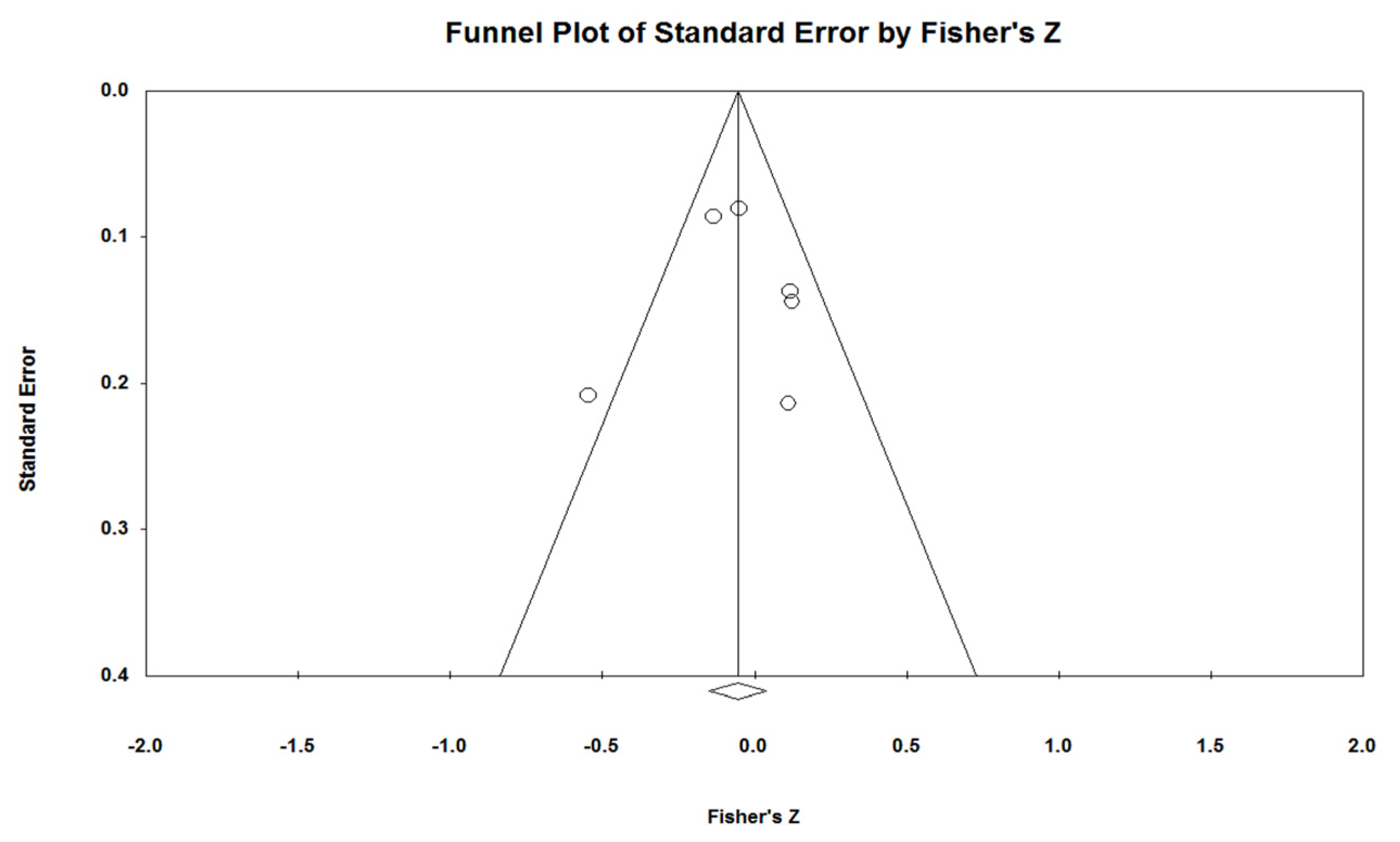
3.4. Risk of Bias across Studies
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Heinzer, R.; Marti-Soler, H.; Haba-Rubio, J. Prevalence of Sleep Apnoea Syndrome in the Middle to Old Age General Population. Lancet Respir. Med. 2016, 4, e5–e6. [Google Scholar] [CrossRef] [PubMed]
- Epstein, L.J.; Kristo, D.; Strollo, P.J.; Friedman, N.; Malhotra, A.; Patil, S.P.; Ramar, K.; Rogers, R.; Schwab, R.J.; Weaver, E.M.; et al. Clinical Guideline for the Evaluation, Management and Long-Term Care of Obstructive Sleep Apnea in Adults. J. Clin. Sleep Med. 2009, 5, 263–276. [Google Scholar] [PubMed]
- Shawon, M.S.R.; Perret, J.L.; Senaratna, C.V.; Lodge, C.; Hamilton, G.S.; Dharmage, S.C. Current Evidence on Prevalence and Clinical Outcomes of Co-Morbid Obstructive Sleep Apnea and Chronic Obstructive Pulmonary Disease: A Systematic Review. Sleep Med. Rev. 2017, 32, 58–68. [Google Scholar] [CrossRef] [PubMed]
- Ahrens, A.; McGrath, C.; Hägg, U. A Systematic Review of the Efficacy of Oral Appliance Design in the Management of Obstructive Sleep Apnoea. Eur. J. Orthod. 2011, 33, 318–324. [Google Scholar] [CrossRef]
- Lim, J.; Lasserson, T.J.; Fleetham, J.; Wright, J.J. Oral Appliances for Obstructive Sleep Apnoea. Cochrane Database Syst. Rev. 2006, 2006, CD004435. [Google Scholar] [CrossRef]
- Levrini, L.; Sacchi, F.; Milano, F.; Polimeni, A.; Cozza, P.; Bernkopf, E.; Segù, M. Italian recommendations on dental support in the treatment of adult obstructive sleep apnea syndrome (OSAS). Ann. Stomatol. 2015, 6, 81–86. [Google Scholar] [CrossRef]
- Chan, A.S.L.; Sutherland, K.; Schwab, R.J.; Zeng, B.; Petocz, P.; Lee, R.W.W.; Darendeliler, M.A.; Cistulli, P.A. The Effect of Mandibular Advancement on Upper Airway Structure in Obstructive Sleep Apnoea. Thorax 2010, 65, 726–732. [Google Scholar] [CrossRef]
- Mehta, A.; Qian, J.; Petocz, P.; Ali Darendeliler, M.; Cistulli, P.A. A Randomized, Controlled Study of a Mandibular Advancement Splint for Obstructive Sleep Apnea. Am. J. Respir. Crit. Care Med. 2001, 163, 1457–1461. [Google Scholar] [CrossRef]
- Bosi, M.; De Vito, A.; Kotecha, B.; Viglietta, L.; Braghiroli, A.; Steier, J.; Pengo, M.; Sorrenti, G.; Gobbi, R.; Vicini, C.; et al. Phenotyping the Pathophysiology of Obstructive Sleep Apnea Using Polygraphy/Polysomnography: A Review of the Literature. Sleep Breath. 2018, 22, 579–592. [Google Scholar] [CrossRef]
- Redline, S.; Sands, S.A.; Owens, R.L.; Edwards, B.A. More Than the Sum of the Respiratory Events: Personalized Medicine Approaches for Obstructive Sleep Apnea. Am. J. Respir. Crit. Care Med. 2019, 200, 691–703. [Google Scholar] [CrossRef]
- Bosi, M.; Incerti Parenti, S.; Sanna, A.; Plazzi, G.; De Vito, A.; Alessandri-Bonetti, G. Non-Continuous Positive Airway Pressure Treatment Options in Obstructive Sleep Apnoea: A Pathophysiological Perspective. Sleep Med. Rev. 2021, 60, 101521. [Google Scholar] [CrossRef] [PubMed]
- Fransson, A.M.C.; Tegelberg, Å.; Johansson, A.; Wenneberg, B. Influence on the Masticatory System in Treatment of Obstructive Sleep Apnea and Snoring with a Mandibular Protruding Device: A 2-Year Follow-Up. Am. J. Orthod. Dentofac. Orthop. 2004, 126, 687–693. [Google Scholar] [CrossRef] [PubMed]
- Long, J.; Ogawa, T.; Ito, T.; Matsuda, M.; Li, W.; Yu, H.; Sasaki, K. Effect of Bite Openings and Mandibular Protrusion on Genioglossus Muscle Activity in Healthy Adults with Oral Appliance. Odontology 2018, 106, 90–95. [Google Scholar] [CrossRef] [PubMed]
- Iftikhar, I.H.; Cistulli, P.A.; Jahrami, H.; Alamoud, K.A.; Saeed, M.; Soulimiotis, A.P.; BaHammam, A.S. Comparative Efficacy of Mandibular Advancement Devices in Obstructive Sleep Apnea: A Network Meta-Analysis. Sleep Breath. 2022. [Google Scholar] [CrossRef]
- Bartolucci, M.L.; Bortolotti, F.; Corazza, G.; Incerti Parenti, S.; Paganelli, C.; Alessandri Bonetti, G. Effectiveness of Different Mandibular Advancement Device Designs in Obstructive Sleep Apnoea Therapy: A Systematic Review of Randomised Controlled Trials with Meta-Analysis. J. Oral Rehabil. 2021, 48, 469–486. [Google Scholar] [CrossRef]
- Aarab, G.; Lobbezoo, F.; Hamburger, H.L.; Naeije, M. Effects of an Oral Appliance with Different Mandibular Protrusion Positions at a Constant Vertical Dimension on Obstructive Sleep Apnea. Clin. Oral Investig. 2010, 14, 339–345. [Google Scholar] [CrossRef]
- Tegelberg, Å.; Walker-Engström, M.L.; Vesding, O.; Wilhelmsson, B. Two Different Degrees of Mandibular Advancement with a Dental Appliance in Treatment of Patients with Mild to Moderate Obstructive Sleep Apnea. Acta Odontol. Scand. 2003, 61, 356–362. [Google Scholar] [CrossRef]
- Walker-Engström, M.L.; Ringqvist, I.; Vestling, O.; Wilhelmsson, B.; Tegelberg, A. A Prospective Randomized Study Comparing Two Different Degrees of Mandibular Advancement with a Dental Appliance in Treatment of Severe Obstructive Sleep Apnea. Sleep Breath. 2003, 7, 119–130. [Google Scholar] [CrossRef]
- Gindre, L.; Gagnadoux, F.; Meslier, N.; Gustin, J.M.; Racineux, J.L. Mandibular Advancement for Obstructive Sleep Apnea: Dose Effect on Apnea, Long-Term Use and Tolerance. Respiration 2008, 76, 386–392. [Google Scholar] [CrossRef]
- Gagnadoux, F.; Fleury, B.; Vielle, B.; Pételle, B.; Meslier, N.; N’Guyen, X.L.; Trzepizur, W.; Racineux, J.L. Titrated Mandibular Advancement versus Positive Airway Pressure for Sleep Apnoea. Eur. Respir. J. 2009, 34, 914–920. [Google Scholar] [CrossRef]
- Campbell, A.J.; Reynolds, G.; Trengrove, H.; Neill, A.M. Mandibular Advancement Splint Titration in Obstructive Sleep Apnoea. Sleep Breath. 2009, 13, 157–162. [Google Scholar] [CrossRef]
- Bartolucci, M.L.; Bortolotti, F.; Raffaelli, E.; D’Antò, V.; Michelotti, A.; Alessandri Bonetti, G. The Effectiveness of Different Mandibular Advancement Amounts in OSA Patients: A Systematic Review and Meta-Regression Analysis. Sleep Breath. 2016, 20, 911–919. [Google Scholar] [CrossRef]
- Kato, J.; Isono, S.; Tanaka, A.; Watanabe, T.; Araki, D.; Tanzawa, H.; Nishino, T. Dose-Dependent Effects of Mandibular Advancement on Pharyngeal Mechanics and Nocturnal Oxygenation in Patients with Sleep-Disordered Breathing. Chest 2000, 117, 1065–1072. [Google Scholar] [CrossRef]
- Alhajj, M.N.; Khalifa, N.; Abduo, J.; Amran, A.G.; Ismail, I.A. Determination of Occlusal Vertical Dimension for Complete Dentures Patients: An Updated Review. J. Oral Rehabil. 2017, 44, 896–907. [Google Scholar] [CrossRef]
- Kuna, S.T.; Remmers, J.E. Neural and Anatomic Factors Related to Upper Airway Occlusion during Sleep. Med. Clin. North Am. 1985, 69, 1221–1242. [Google Scholar] [CrossRef]
- L’Estrange, P.R.; Battagel, J.M.; Harkness, B.; Spratley, M.H.; Nolan, P.J.; Jorgensen, G.I. A Method of Studying Adaptive Changes of the Oropharynx to Variation in Mandibular Position in Patients with Obstructive Sleep Apnoea. J. Oral Rehabil. 1996, 23, 699–711. [Google Scholar] [CrossRef]
- Meurice, J.C.; Marc, I.; Carrier, G.; Sériès, F. Effects of Mouth Opening on Upper Airway Collapsibility in Normal Sleeping Subjects. Am. J. Respir. Crit. Care Med. 1996, 153, 255–259. [Google Scholar] [CrossRef]
- Mayoral, P.; Lagravère, M.O.; Míguez-Contreras, M.; Garcia, M. Antero-Posterior Mandibular Position at Different Vertical Levels for Mandibular Advancing Device Design. BMC Oral Health 2019, 19, 85. [Google Scholar] [CrossRef]
- Lowe, A. Principles and Practice of Sleep Medicine, 3rd ed.; Kryger, M., Roth, T., Dement, W., Eds.; Saunders: Philadelphia, PA, USA, 2000. [Google Scholar]
- Pitsis, A.J.; Ali Darendeliler, M.; Gotsopoulos, H.; Petocz, P.; Cistulli, P.A. Effect of Vertical Dimension on Efficacy of Oral Appliance Therapy in Obstructive Sleep Apnea. Am. J. Respir. Crit. Care Med. 2002, 166, 860–864. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. J. Clin. Epidemiol. 2009, 62, 1006–1012. [Google Scholar] [CrossRef]
- Sterne, J.A.C.; Savović, J.; Page, M.J.; Elbers, R.G.; Blencowe, N.S.; Boutron, I.; Cates, C.J.; Cheng, H.Y.; Corbett, M.S.; Eldridge, S.M.; et al. RoB 2: A Revised Tool for Assessing Risk of Bias in Randomised Trials. BMJ 2019, 366, l4898. [Google Scholar] [CrossRef]
- Guyatt, G.; Oxman, A.D.; Akl, E.A.; Kunz, R.; Vist, G.; Brozek, J.; Norris, S.; Falck-Ytter, Y.; Glasziou, P.; Debeer, H.; et al. GRADE Guidelines: 1. Introduction—GRADE Evidence Profiles and Summary of Findings Tables. J. Clin. Epidemiol. 2011, 64, 383–394. [Google Scholar] [CrossRef] [PubMed]
- Borenstein, M.; Hedges, L.; Higgins, J.; Rothstein, H. Introduction to Meta-Analysis; John Wiley & Sons: Hoboken, NJ, USA, 2009. [Google Scholar]
- Blanco, J.; Zamarrón, C.; Abeleira Pazos, M.T.; Lamela, C.; Suarez Quintanilla, D. Prospective Evaluation of an Oral Appliance in the Treatment of Obstructive Sleep Apnea Syndrome. Sleep Breath. 2005, 9, 20–25. [Google Scholar] [CrossRef]
- Gotsopoulos, H.; Kelly, J.J.; Cistulli, P.A. Oral Appliance Therapy Reduces Blood Pressure in Obstructive Sleep Apnea: A Randomized, Controlled Trial. Sleep 2004, 27, 934–941. [Google Scholar] [CrossRef]
- Johnston, C.D.; Gleadhill, I.C.; Cinnamond, M.J.; Gabbey, J.; Burden, D.J. Mandibular Advancement Appliances and Obstructive Sleep Apnoea: A Randomized Clinical Trial. Eur. J. Orthod. 2002, 24, 251–262. [Google Scholar] [CrossRef]
- Naismith, S.L.; Winter, V.R.; Hickie, I.B.; Cistulli, P.A. Effect of Oral Appliance Therapy on Neurobehavioral Functioning in Obstructive Sleep Apnea: A Randomized Controlled Trial. J. Clin. Sleep Med. 2005, 1, 374–380. [Google Scholar] [CrossRef]
- Nikolopoulou, M.; Ahlberg, J.; Visscher, C.; Hamburger, H.; Naeije, M.; Lobbezoo, F. Effects of Occlusal Stabilization Splints on Obstructive Sleep Apnea: A Randomized Controlled Trial. J. Orofac. Pain 2013, 27, 199–205. [Google Scholar] [CrossRef]
- Aarab, G.; Lobbezoo, F.; Heymans, M.W.; Hamburger, H.L.; Naeije, M. Long-Term Follow-up of a Randomized Controlled Trial of Oral Appliance Therapy in Obstructive Sleep Apnea. Respiration 2011, 82, 162–168. [Google Scholar] [CrossRef]
- Petri, N.; Svanholt, P.; Solow, B.; Wildschiødtz, G.; Winkel, P. Mandibular Advancement Appliance for Obstructive Sleep Apnoea: Results of a Randomised Placebo Controlled Trial Using Parallel Group Design. J. Sleep Res. 2008, 17, 221–229. [Google Scholar] [CrossRef]
- Andrén, A.; Hedberg, P.; Walker-Engström, M.L.; Wahlén, P.; Tegelberg, Å. Effects of Treatment with Oral Appliance on 24-h Blood Pressure in Patients with Obstructive Sleep Apnea and Hypertension: A Randomized Clinical Trial. Sleep Breath. 2013, 17, 705–712. [Google Scholar] [CrossRef]
- Durán-Cantolla, J.; Crovetto-Martínez, R.; Alkhraisat, M.H.; Crovetto, M.; Municio, A.; Kutz, R.; Aizpuru, F.; Miranda, E.; Anitua, E. Efficacy of Mandibular Advancement Device in the Treatment of Obstructive Sleep Apnea Syndrome: A Randomized Controlled Crossover Clinical Trial. Med. Oral Patol. Oral Cir. Bucal 2015, 20, e605–e615. [Google Scholar] [CrossRef] [PubMed]
- Gagnadoux, F.; Pépin, J.L.; Vielle, B.; Bironneau, V.; Chouet-Girard, F.; Launois, S.; Meslier, N.; Meurice, J.C.; Nguyen, X.L.; Paris, A.; et al. Impact of Mandibular Advancement Therapy on Endothelial Function in Severe Obstructive Sleep Apnea. Am. J. Respir. Crit. Care Med. 2017, 195, 1244–1252. [Google Scholar] [CrossRef] [PubMed]
- Recoquillon, S.; Pépin, J.L.; Vielle, B.; Andriantsitohaina, R.; Bironneau, V.; Chouet-Girard, F.; Fleury, B.; Goupil, F.; Launois, S.; Martinez, M.C.; et al. Effect of Mandibular Advancement Therapy on Inflammatory and Metabolic Biomarkers in Patients with Severe Obstructive Sleep Apnoea: A Randomised Controlled Trial. Thorax 2019, 74, 496–499. [Google Scholar] [CrossRef]
- Nikolopoulou, M.; Naeije, M.; Aarab, G.; Hamburger, H.L.; Visscher, C.M.; Lobbezoo, F. The Effect of Raising the Bite without Mandibular Protrusion on Obstructive Sleep Apnoea. J. Oral Rehabil. 2011, 38, 643–647. [Google Scholar] [CrossRef]
- Nikolopoulou, M.; Aarab, G.; Ahlberg, J.; Hamburger, H.L.; de Lange, J.; Lobbezoo, F. Oral Appliance Therapy versus Nasal Continuous Positive Airway Pressure in Obstructive Sleep Apnea: A Randomized, Placebo-Controlled Trial on Temporomandibular Side-Effects. Clin. Exp. Dent. Res. 2020, 6, 400–406. [Google Scholar] [CrossRef]
- Venema, J.A.M.U.; Rosenmöller, B.R.A.M.; de Vries, N.; de Lange, J.; Aarab, G.; Lobbezoo, F.; Hoekema, A. Mandibular Advancement Device Design: A Systematic Review on Outcomes in Obstructive Sleep Apnea Treatment. Sleep Med. Rev. 2021, 60, 101557. [Google Scholar] [CrossRef] [PubMed]
- Sari, E.; Menillo, S. Comparison of Titratable Oral Appliance and Mandibular Advancement Splint in the Treatment of Patients with Obstructive Sleep Apnea. ISRN Dent. 2011, 2011, 581692. [Google Scholar] [CrossRef]
- Rose, E.; Staats, R.; Virchow, C.; Jonas, I.E. A Comparative Study of Two Mandibular Advancement Appliances for the Treatment of Obstructive Sleep Apnoea. Eur. J. Orthod. 2002, 24, 191–198. [Google Scholar] [CrossRef]
- Zhou, J.; Liu, Y.H. A Randomised Titrated Crossover Study Comparing Two Oral Appliances in the Treatment for Mild to Moderate Obstructive Sleep Apnoea/Hypopnoea Syndrome. J. Oral Rehabil. 2012, 39, 914–922. [Google Scholar] [CrossRef]
- Isacsson, G.; Fodor, C.; Sturebrand, M. Obstructive Sleep Apnea Treated with Custom-Made Bibloc and Monobloc Oral Appliances: A Retrospective Comparative Study. Sleep Breath. 2017, 21, 93–100. [Google Scholar] [CrossRef]
- Gagnon, Y.; Mayer, P.; Morisson, F.; Rompré, P.H.; Lavigne, G.J. Aggravation of Respiratory Disturbances by the Use of an Occlusal Splint in Apneic Patients: A Pilot Study. Int. J. Prosthdontics 2004, 17, 447–453. [Google Scholar]
- Barbero, M.; Flores-Mir, C.; Blanco, J.C.; Nuño, V.C.; Casellas, J.B.; Girado, J.L.C.; Amezaga, J.A.; Carlos, F. De Tridimensional Upper Airway Assessment in Male Patients with OSA Using Oral Advancement Devices Modifying Their Vertical Dimension. J. Clin. Sleep Med. 2020, 6, 1721–1729. [Google Scholar] [CrossRef]
- Op de Beeck, S.; Dieltjens, M.; Verbruggen, A.E.; Vroegop, A.V.; Wouters, K.; Hamans, E.; Willemen, M.; Verbraecken, J.; De Backer, W.A.; Van De Heyning, P.H.; et al. Phenotypic Labelling Using Drug-Induced Sleep Endoscopy Improves Patient Selection for Mandibular Advancement Device Outcome: A Prospective Study. J. Clin. Sleep Med. 2019, 15, 1089–1099. [Google Scholar] [CrossRef]
- Saffer, F.; Lubianca, J.F.L.; Rösing, C.; Dias, C.; Closs, L. Predictors of Success in the Treatment of Obstructive Sleep Apnea Syndrome with Mandibular Repositioning Appliance: A Systematic Review. Int. Arch. Otorhinolaryngol. 2013, 19, 80–85. [Google Scholar] [CrossRef] [PubMed]

| Study | Study Design | Control | Sample Size | Age (Mean ± SD) | BMI (Mean ± SD) | Degree of Vertical Opening | AHI Pre (Mean ± SD) | AHI Post (Mean ± SD) | Follow-Up | Author’s Main Conclusions |
|---|---|---|---|---|---|---|---|---|---|---|
| Blanco 2005 [35] | RCT | MAD with advancement vs. without advancement | 7 | 53.0 ± 12.7 | 28.4 ± 4.2 | 5 mm | 24.0 ± 12.2 | 11.7 ± 7.9 | 3 months | Mean AHI significantly decreases in both groups. |
| Gotsopoulos 2004 [36] | RCT cross-over | MAD vs. Placebo | 67 (53 M;14 F) | 48 ± 11 | 29.2 ± 4.8 | 3.5 mm | 27 ± 15 | 24 ± 2 | 1 month | A reduction of 50% in mean AHI value was obtained in MAD group, while no significant reduction was seen in Placebo group (p = 0.18). |
| Johnston 2002 [37] | RCT cross-over | MAD vs. Placebo | 20 (16 M;4 F) | 55.10 ± 6.87 | 31.63 ± 5.94 | 1.5 mm | 31.93 ± 21.18 | 37.68 ± 24.68 | 4–6 weeks | MAD is significantly more efficient in improving AHI values compared to the placebo, with a success rate of 33%. |
| Mehta 2001 [8] | RCT cross-over | MAD vs. Placebo | 24 (19 M;5 F) | 48 ± 9 | 29.4 ± 3.1 | 3.5 mm | 27.0 ± 17 | 30.0 ± 2 | 5 weeks | The Placebo device has no effects on AHI values. |
| Naismith 2005 [38] | RCT cross-over | MAD vs. Placebo | 73 (59 M;14 F) | 48.4 ± 11.00 | 29.0 ± 5.0 | 3.5 mm | 26.9 ± 15.4 | 25.4 ± 14.5 | 2 months | The mean AHI value is reduced of 50% in MAD group; the reduction is not significant in Placebo group (p = 0.18). |
| Nikolopoulou 2013 [39] | RCT cross-over | MAD in situ vs. non in situ | 10 (3 M;7 F) | 47.3 ± 11.7 | <40 | 1 mm | 15.9 ± 6.4 | 17.4 ± 7.0 | 3 nights | A small but significant increase in AHI values is noted in OSA patients with MAD in situ. |
| Study | Bias Arising from the Randomisation Process | Bias Due to Deviations from Intended Interventions | Bias Due to Missing Outcome Data | Bias in Measurement of the Outcome | Bias in Selection of Reported Result | Response |
|---|---|---|---|---|---|---|
| Blanco 2005 [35] | Some concerns | Some concerns | High risk | Low risk | Low risk | High risk |
| Gotsopoulos 2004 [36] | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk |
| Johnston 2002 [37] | Some concerns | Some concerns | Low risk | Low risk | Low risk | Some concerns |
| Mehta 2001 [8] | Some concerns | Some concerns | High risk | Low risk | Low risk | High risk |
| Naismith 2005 [38] | Low risk | Some concerns | Low risk | Low risk | Low risk | Some concerns |
| Nikolopoulou 2013 [39] | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk |
| Success Rate | ||||||||
|---|---|---|---|---|---|---|---|---|
| Quality Assessment | Summary of Findings | |||||||
| Number of Subgroups | Risk of Bias | Inconsistency | Indirectness | Imprecision | Publication Bias (Egger’s Test) | Number of Patients | Success Rate (95% CI) | Quality |
| 6 | Serious | Serious (I2 = 50.54, p = 0.072) | Serious | Not serious | Not serious (p = 0.977) | 195 | −0.054 [−0.054 − 0.040] | Very Low |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bartolucci, M.L.; Incerti Parenti, S.; Bortolotti, F.; Corazza, G.; Solidoro, L.; Paganelli, C.; Alessandri-Bonetti, G. The Effect of Bite Raise on AHI Values in Adult Patients Affected by OSA: A Systematic Review with Meta-Regression. J. Clin. Med. 2023, 12, 3619. https://doi.org/10.3390/jcm12113619
Bartolucci ML, Incerti Parenti S, Bortolotti F, Corazza G, Solidoro L, Paganelli C, Alessandri-Bonetti G. The Effect of Bite Raise on AHI Values in Adult Patients Affected by OSA: A Systematic Review with Meta-Regression. Journal of Clinical Medicine. 2023; 12(11):3619. https://doi.org/10.3390/jcm12113619
Chicago/Turabian StyleBartolucci, Maria Lavinia, Serena Incerti Parenti, Francesco Bortolotti, Giulia Corazza, Livia Solidoro, Corrado Paganelli, and Giulio Alessandri-Bonetti. 2023. "The Effect of Bite Raise on AHI Values in Adult Patients Affected by OSA: A Systematic Review with Meta-Regression" Journal of Clinical Medicine 12, no. 11: 3619. https://doi.org/10.3390/jcm12113619
APA StyleBartolucci, M. L., Incerti Parenti, S., Bortolotti, F., Corazza, G., Solidoro, L., Paganelli, C., & Alessandri-Bonetti, G. (2023). The Effect of Bite Raise on AHI Values in Adult Patients Affected by OSA: A Systematic Review with Meta-Regression. Journal of Clinical Medicine, 12(11), 3619. https://doi.org/10.3390/jcm12113619









