Is Modular Dual Mobility Superior to Standard Bearings for Reducing Dislocation Risk after Primary Total Hip Arthroplasty? A Retrospective Comparative Multicenter Study
Abstract
:1. Introduction
2. Material and Methods
2.1. Study Design
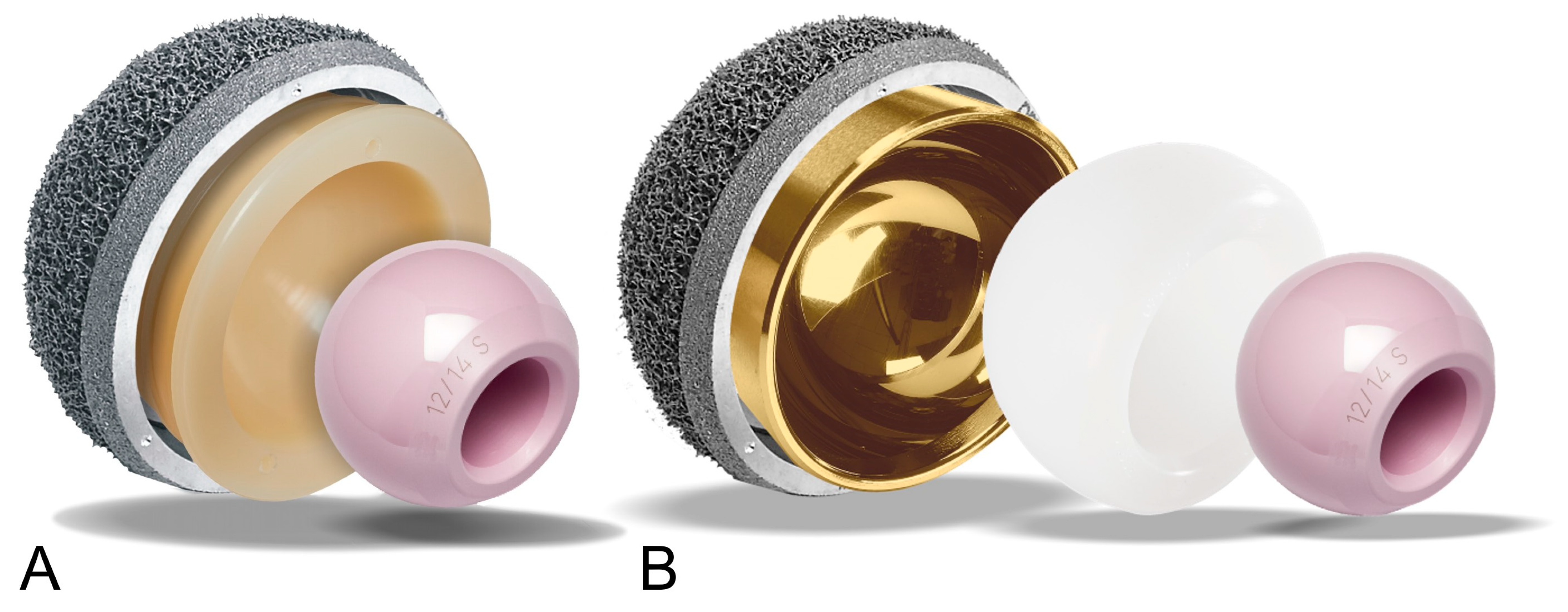
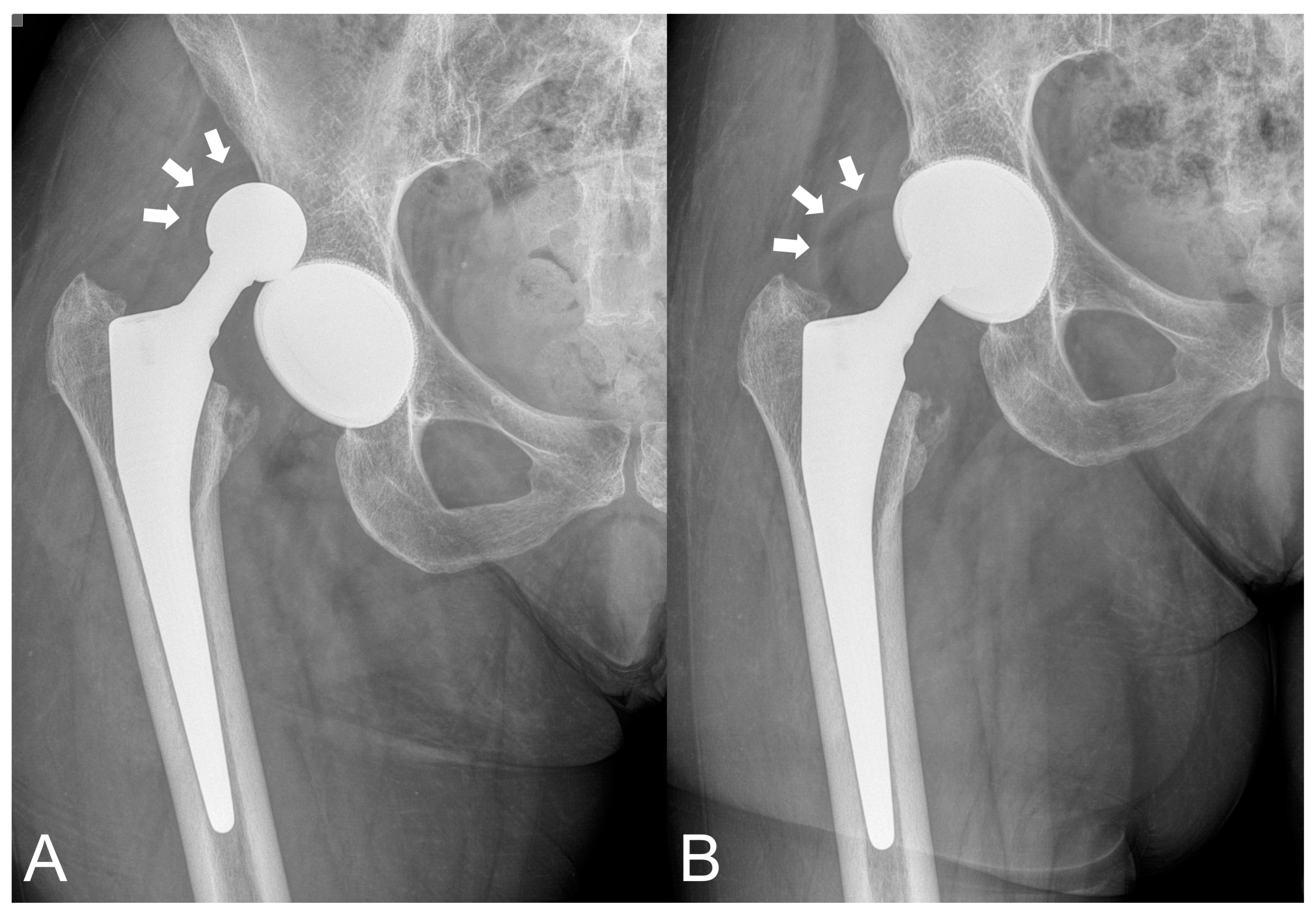
2.2. Prosthetic Device
2.3. Study Procedure
2.4. Clinical Evaluation
2.5. Radiographic Analysis
2.6. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Australian Orthopaedic Association National Joint Replacement Registry (AOANJRR). Hip, Knee & Shoulder Arthroplasty: 2022 Annual Report; AOA: Adelaide, Australia, 2022; pp. 1–487. Available online: https://aoanjrr.sahmri.com/annual-reports-2022 (accessed on 8 May 2023).
- Kwon, M.S.; Kuskowski, M.; Mulhall, K.J.; Macaulay, W.; Brown, T.E.; Saleh, K.J. Does surgical approach affect total hip arthroplasty dislocation rates? Clin. Orthop. Relat. Res. 2006, 447, 34–38. [Google Scholar] [CrossRef] [PubMed]
- Enocson, A.; Hedbeck, C.J.; Tidermark, J.; Pettersson, H.; Ponzer, S.; Lapidus, L.J. Dislocation of total hip replacement in patients with fractures of the femoral neck. Acta Orthop. 2009, 80, 184–189. [Google Scholar] [CrossRef] [PubMed]
- Bousquet, G.; Gazielly, D.; Girardin, P.; Debiesse, J.L.; Relave, M.; Israeli, A. The ceramic coated cementless total hip arthroplasty. Basic concepts and surgical technique. J. Orthop. Surg. Tech. 1985, 1, 15–28. [Google Scholar]
- Farizon, F.; de Lavison, R.; Azoulai, J.J.; Bousquet, G. Results with a cementless alumina-coated cup with dual mobility: A twelve-year follow-up study. Int. Orthop. 1998, 22, 219–224. [Google Scholar] [CrossRef] [Green Version]
- Jonker, R.C.; van Beers, L.W.A.H.; van der Wal, B.C.H.; Vogely, H.C.; Parratte, S.; Castelein, R.M.; Poolman, R.W. Can dual mobility cups prevent dislocation without increasing revision rates in primary total hip arthroplasty? A systematic review. Orthop. Traumatol. Surg. Res. 2020, 106, 509–517. [Google Scholar] [CrossRef] [PubMed]
- Cha, Y.H.; Yoo, J.I.; Kim, J.T.; Park, C.H.; Ahn, Y.S.; Choy, W.S.; Ha, Y.C.; Koo, K.H. Dual mobility total hip arthroplasty in the treatment of femoral neck fractures. Bone Joint J. 2020, 102, 1457–1466. [Google Scholar] [CrossRef] [PubMed]
- Matsen Ko, L.J.; Pollag, K.E.; Yoo, J.Y.; Sharkey, P.F. Serum metal ion levels following total hip arthroplasty with modular dual mobility components. J. Arthroplast. 2016, 31, 186–189. [Google Scholar] [CrossRef]
- Sutter, E.G.; McClellan, T.R.; Attarian, D.E.; Bolognesi, M.P.; Lachiewicz, P.F.; Wellman, S.S. Outcomes of modular dual mobility acetabular components in revision total hip arthroplasty. J. Arthroplast. 2017, 32 (Suppl. S9), 220–224. [Google Scholar] [CrossRef]
- Greenberg, A.; Nocon, A.; De Martino, I.; Mayman, D.J.; Sculco, T.P.; Sculco, P.K. Serum metal ions in contemporary monoblock and modular dual mobility articulations. Arthroplast. Today 2021, 12, 51–56. [Google Scholar] [CrossRef]
- Farey, J.E.; Masters, J.; Cuthbert, A.R.; Iversen, P.; van Steenbergen, L.N.; Prentice, H.A.; Adie, S.; Sayers, A.; Whitehouse, M.R.; Paxton, E.W.; et al. Do dual-mobility cups reduce revision risk in femoral neck fractures compared with conventional THA designs? An international meta-analysis of arthroplasty registries. Clin. Orthop. Relat. Res. 2022, 480, 1912–1925. [Google Scholar] [CrossRef]
- French, J.M.R.; Bramley, P.; Scattergood, S.; Sandiford, N.A. Adverse reaction to metal debris due to fretting corrosion between the acetabular components of modular dual-mobility constructs in total hip replacement: A systematic review and meta-analysis. EFORT Open Rev. 2021, 6, 343–353. [Google Scholar] [CrossRef] [PubMed]
- Siljander, M.P.; Gausden, E.B.; Wooster, B.M.; Karczewski, D.; Sierra, R.J.; Trousdale, R.T.; Abdel, M.P. Liner malseating is rare with two modular dual-mobility designs. Bone Joint J. 2022, 104, 598–603. [Google Scholar] [CrossRef] [PubMed]
- Philippot, R.; Boyer, B.; Farizon, F. Intraprosthetic dislocation: A specific complication of the dual-mobility system. Clin. Orthop. Relat. Res. 2013, 471, 965–970. [Google Scholar] [CrossRef] [Green Version]
- De Martino, I.; D’Apolito, R.; Waddell, B.S.; McLawhorn, A.S.; Sculco, P.K.; Sculco, T.P. Early intraprosthetic dislocation in dual-mobility implants: A systematic review. Arthroplast. Today 2017, 3, 197–202. [Google Scholar] [CrossRef] [Green Version]
- Addona, J.L.; Gu, A.; De Martino, I.; Malahias, M.A.; Sculco, T.P.; Sculco, P.K. High rate of early intraprosthetic dislocations of dual mobility implants: A single surgeon series of primary and revision total hip replacements. J. Arthroplast. 2019, 34, 2793–2798. [Google Scholar] [CrossRef]
- Tyagi, V.; Akinbo, O. Early intraprosthetic dislocation of a dual mobility acetabular construct after total hip arthroplasty. J. Orthop. Case Rep. 2017, 7, 21–24. [Google Scholar]
- Harris, W.H. Traumatic arthritis of the hip after dislocation and acetabular fractures: Treatment by mold arthroplasty. An end-result study using a new method of result evaluation. J. Bone Joint Surg. Am. 1969, 51, 737–755. [Google Scholar] [CrossRef] [PubMed]
- Lewinnek, G.E.; Lewis, J.L.; Tarr, R.; Compere, C.L.; Zimmerman, J.R. Dislocations after total hip-replacement arthroplasties. J. Bone Joint Surg. Am. 1978, 60, 217–220. [Google Scholar] [CrossRef]
- McCollum, D.E.; Gray, W.J. Dislocation after total hip arthroplasty. Causes and prevention. Clin. Orthop. Relat. Res. 1990, 261, 159–170. [Google Scholar] [CrossRef]
- Brooker, A.F.; Bowerman, J.W.; Robinson, R.A.; Riley, L.H. Ectopic ossification following total hip replacement. Incidence and a method of classification. J. Bone Joint Surg. Am. 1973, 55, 1629–1632. [Google Scholar] [CrossRef]
- DeLee, J.G.; Charnley, J. Radiological demarcation of cemented sockets in total hip replacement. Clin. Orthop. Relat. Res. 1976, 121, 20–32. [Google Scholar] [CrossRef]
- Moore, M.S.; McAuley, J.P.; Young, A.M.; Engh, C.A., Sr. Radiographic signs of osseointegration in porous-coated acetabular components. Clin. Orthop. Relat. Res. 2006, 444, 176–183. [Google Scholar] [CrossRef] [PubMed]
- Massin, P.; Schmidt, L.; Engh, C.A. Evaluation of cementless acetabular component migration. An experimental study. J. Arthroplast. 1989, 4, 245–251. [Google Scholar] [CrossRef] [PubMed]
- Singh, V.; Loloi, J.; Macaulay, W.; Hepinstall, M.S.; Schwarzkopf, R.; Aggarwal, V.K. Dual-mobility versus fixed-bearing in primary total hip arthroplasty: Outcome comparison. Hip Pelvis. 2022, 34, 96–105. [Google Scholar] [CrossRef]
- Dubin, J.A.; Westrich, G.H. Anatomic dual mobility compared to modular dual mobility in primary total hip arthroplasty: A matched cohort study. Arthroplast. Today 2019, 5, 509–514. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Harwin, S.F.; Mistry, J.B.; Chughtai, M.; Khlopas, A.; Gwam, C.; Newman, J.M.; Higuera, C.A.; Bonutti, P.M.; Malkani, A.L.; Kolisek, F.R.; et al. Dual mobility acetabular cups in primary total hip arthroplasty in patients at high risk for dislocation. Surg. Technol. Int. 2017, 30, 251–258. [Google Scholar] [PubMed]
- Pai, F.Y.; Ma, H.H.; Chou, T.A.; Huang, T.W.; Huang, K.C.; Tsai, S.W.; Chen, C.F.; Chen, W.M. Risk factors and modes of failure in the modern dual mobility implant. A systematic review and meta-analysis. BMC Musculoskelet. Disord. 2021, 22, 541. [Google Scholar] [CrossRef]
- Epinette, J.A.; Coulomb, R.; Pradel, S.; Kouyoumdjian, P. Do modular dual mobility cups offer a reliable benefit? Minimum 5-year follow-up of 102 cups. J. Arthroplast. 2022, 37, 910–916. [Google Scholar] [CrossRef]
- Park, C.W.; Lim, S.J.; Kim, I.S.; Jang, M.C.; Moon, Y.W.; Park, Y.S. Outcomes of revision total hip arthroplasty using the modular dual mobility acetabular system to treat recurrent dislocation. Int. Orthop. 2022, 46, 789–795. [Google Scholar] [CrossRef]
- Hernandez, N.M.; Hinton, Z.W.; Wu, C.J.; Lachiewicz, P.F.; Ryan, S.P.; Wellman, S.S. Is there a problem with modular dual mobility acetabular components in revision total hip arthroplasty at mid-term follow-up? Bone Joint J. 2021, 103 (Suppl. S7), 66–72. [Google Scholar] [CrossRef]
- Guntin, J.; Plummer, D.; Della Valle, C.; DeBenedetti, A.; Nam, D. Malseating of modular dual mobility liners. Bone Jt. Open. 2021, 2, 858–864. [Google Scholar] [CrossRef] [PubMed]
- Tigani, D.; Banci, L.; Valtorta, R.; Amendola, L. Hip stability parameters with dual mobility, modular dual mobility and fixed bearing in total hip arthroplasty: An analytical evaluation. BMC Musculoskelet. Disord. 2022, 23, 373. [Google Scholar] [CrossRef] [PubMed]
- Lecuire, F.; Benareau, I.; Rubini, J.; Basso, M. Luxation intra-prothétique dans la cupule à double mobilité de Bousquet. A propos de 7 cas [Intra-prosthetic dislocation of the Bousquet dual mobility socket]. Rev. Chir. Orthop. Reparatrice Appar. Mot. 2004, 90, 249–255. [Google Scholar] [CrossRef] [PubMed]
- Hernigou, P.; Dubory, A.; Potage, D.; Roubineau, F.; Flouzat Lachaniette, C.H. Dual-mobility arthroplasty failure: A rationale review of causes and technical considerations for revision. Int. Orthop. 2017, 41, 481–490. [Google Scholar] [CrossRef] [PubMed]
- Sidhu, G.A.S.; Kotecha, A.; Mulay, S.; Ashwood, N. Spontaneous early intraprosthetic dislocation of 22 mm skirted femoral head in dual mobility hip prosthesis: A case report. J. Orthop. Case Rep. 2021, 11, 6–9. [Google Scholar] [CrossRef] [PubMed]
- Smuin, D.M.; Tucker, S.M.; Rothermel, S.D.; Lewis, G.S.; Mason, M. Effect of bone coverage on acetabular implant stresses in standard and dual-mobility total hip arthroplasty constructs: A finite element model. Orthopedics 2021, 44, 280–284. [Google Scholar] [CrossRef] [PubMed]
- Chalmers, B.P.; Dubin, J.; Westrich, G.H. Modular dual-mobility liner malseating: A radiographic analysis. Arthroplast. Today 2020, 6, 699–703. [Google Scholar] [CrossRef]
- Romero, J.; Wach, A.; Silberberg, S.; Chiu, Y.F.; Westrich, G.; Wright, T.M.; Padgett, D.E. 2020 Otto Aufranc Award: Malseating of modular dual mobility liners. Bone Joint J. 2020, 102 (Suppl. S7), 20–26. [Google Scholar] [CrossRef]
- Rashed, R.A.; Abdalaziz, A.; Veivenn, V.Y.; Tetali, S.R.; Choudry, Q.A.; Sloan, A.G.; Helm, A. Is dual mobility cup total hip replacement associated with increased incidence of heterotopic ossification compared to conventional total hip replacements in fracture neck of femur patients? Injury 2020, 51, 2676–2681. [Google Scholar] [CrossRef]




| Group | Standard Bearing | Modular DM | p-Value |
|---|---|---|---|
| N. of hips | 129 | 133 | |
| Mean follow-up (SD; range) | 2.4 (0.7; 0.9–4.1) | 2.6 (0.7; 0.2–4.1) | 0.0247 |
| Diagnosis, N. of hips | |||
| Osteoarthritis | 93 | 60 | 0.0001 |
| Dysplasia | 9 | 8 | 0.7520 |
| Osteonecrosis | 7 | 22 | 0.0041 |
| Rheumatoid arthritis | 3 | 2 | 0.6815 |
| Femoral neck fracture | 17 | 41 | 0.0006 |
| Gender (male:female) | 54:75 | 39:94 | 0.0340 |
| Mean age (SD; range) | 67.1 (9.5; 26–87) | 75.6 (7.6; 54–94) | 0.0001 |
| Mean BMI (SD; range) | 25.8 (3.0; 21–39) | 24.7 (3.6; 21–42) | 0.0002 |
| Mean preop. HHS (SD; range) | 51.9 (16.1; 3–81) | 45.1 (18.3; 0–86) | 0.0049 |
| N. of hips with history of osteoporosis or poor bone quality | 22 | 44 | 0.0028 |
| Mean acetabular cup size, mm (SD; range) | 52.6 (3.5; 46–60) | 51.0 (3.6; 44–62) | 0.0003 |
| N. of acetabular cups with additional fixation screws (mean N. of screws) | 13 (1.7) | 27 (2.1) | 0.0214 |
| N. of hips with cup malpositioning | 1 | 6 | 0.1203 |
| Group | Standard Bearing | Modular DM | p-Value |
|---|---|---|---|
| Hips | 129 | 133 | |
| N. of hips with dislocation * | 4 (3.1%) | 2 (1.5%) | 0.4416 |
| Femoral head size (mm) of dislocation cases | 36, 36, 32, 32 | 28, 28 | |
| Acetabular cup size (mm) of dislocation cases | 60, 54, 52, 48 | 50, 48 | 0.0557 |
| N. of acetabular insert revisions for dislocation (any reason) | 3 (2.3%) | 2 (1.5%) | 0.6804 |
| Implant survival rate with revision of any component due to dislocation [95% CI] | 95.17% [82.98–98.69%] | 95.87% [80.77–99.16%] | 0.5019 |
| Other complications | 2 groin pain 1 spe deficit 3 superficial infections 1 intraop acetabular fracture 1 intraop femoral fracture 14 HO | 1 pulmonary embolism 2 superficial infections 1 intraop acetabular fracture 1 intraop femoral fracture 1 bone fracture for trauma 8 HO |
| Patient/Implant Factors | Univariate Analysis | Multivariate Analysis | ||||||
|---|---|---|---|---|---|---|---|---|
| OR | p-Value | 95% CI | OR | p-Value | 95% CI | |||
| Osteoarthritis | 1.43 | 0.67 | 0.27 | 10.49 | 0.23 | 0.41 | 0.01 | 8.86 |
| Femoral neck fracture | 0.69 | 0.74 | 0.03 | 4.44 | 2.13 | 0.67 | 0.03 | 81.95 |
| Dysplasia | 3.00 | 0.32 | 0.15 | 20.13 | - | - | - | - |
| Gender (male) | 0.90 | 0.91 | 0.12 | 4.73 | - | - | - | - |
| Age | 1.00 | 0.96 | 0.92 | 1.10 | 1.03 | 0.70 | 0.88 | 1.28 |
| BMI | 1.15 | 0.21 | 0.89 | 1.41 | 1.24 | 0.15 | 0.91 | 1.74 |
| Preop. HHS | 0.99 | 0.78 | 0.95 | 1.04 | 0.97 | 0.46 | 0.89 | 1.04 |
| History of osteoporosis or poor bone quality | 0.58 | 0.63 | 0.03 | 3.73 | - | - | - | - |
| Acetabular cup size | 1.01 | 0.91 | 0.79 | 1.25 | 0.92 | 0.74 | 0.52 | 1.36 |
| Cup malpositioning | 25.10 | 0.001 | 3.00 | 166.3 | 7.58 | 0.26 | 0.15 | 336.7 |
| Group (modDM) | 0.47 | 0.39 | 0.06 | 2.48 | 2.07 | 0.66 | 0.04 | 83.63 |
| Group | Standard Bearing | Modular DM | p-Value |
|---|---|---|---|
| Hips | 112 | 92 | |
| N dislocations | 4 (3.5%) | 1 (1.1%) | 0.3810 |
| N. of acetabular insert revisions for any reason | 3 (2.7%) | 1 (1.1%) | 0.6286 |
| Implant survival rate with revision of any component due to dislocation [95% CI] | 94.62% [81.37–98.52%] | 93.75% [63.24–99.09%] | 0.3979 |
| Complications | 2 groin pain 3 superficial infections 1 intraop acetabular fracture 1 intraop femoral fracture 8 HO | 2 superficial infections 1 intraop acetabular fracture 1 bone fracture for trauma 5 HO |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ciriello, V.; La China, R.; Chirillo, D.F.; Bianco, G.; Fusini, F.; Scarlato, U.; Albanese, C.; Bonzanini, G.; Banci, L.; Piovani, L. Is Modular Dual Mobility Superior to Standard Bearings for Reducing Dislocation Risk after Primary Total Hip Arthroplasty? A Retrospective Comparative Multicenter Study. J. Clin. Med. 2023, 12, 4200. https://doi.org/10.3390/jcm12134200
Ciriello V, La China R, Chirillo DF, Bianco G, Fusini F, Scarlato U, Albanese C, Bonzanini G, Banci L, Piovani L. Is Modular Dual Mobility Superior to Standard Bearings for Reducing Dislocation Risk after Primary Total Hip Arthroplasty? A Retrospective Comparative Multicenter Study. Journal of Clinical Medicine. 2023; 12(13):4200. https://doi.org/10.3390/jcm12134200
Chicago/Turabian StyleCiriello, Vincenzo, Roberta La China, Danilo Francesco Chirillo, Giuseppe Bianco, Federico Fusini, Ugo Scarlato, Carlo Albanese, Giancarlo Bonzanini, Lorenzo Banci, and Lucio Piovani. 2023. "Is Modular Dual Mobility Superior to Standard Bearings for Reducing Dislocation Risk after Primary Total Hip Arthroplasty? A Retrospective Comparative Multicenter Study" Journal of Clinical Medicine 12, no. 13: 4200. https://doi.org/10.3390/jcm12134200
APA StyleCiriello, V., La China, R., Chirillo, D. F., Bianco, G., Fusini, F., Scarlato, U., Albanese, C., Bonzanini, G., Banci, L., & Piovani, L. (2023). Is Modular Dual Mobility Superior to Standard Bearings for Reducing Dislocation Risk after Primary Total Hip Arthroplasty? A Retrospective Comparative Multicenter Study. Journal of Clinical Medicine, 12(13), 4200. https://doi.org/10.3390/jcm12134200






