Impact of COVID-19 Diagnosis on Mortality in Patients with Ischemic Stroke Admitted during the 2020 Pandemic in Italy
Abstract
:1. Introduction
2. Methods
2.1. Study Design
2.2. Study Population
2.3. Statistical Analysis
3. Results
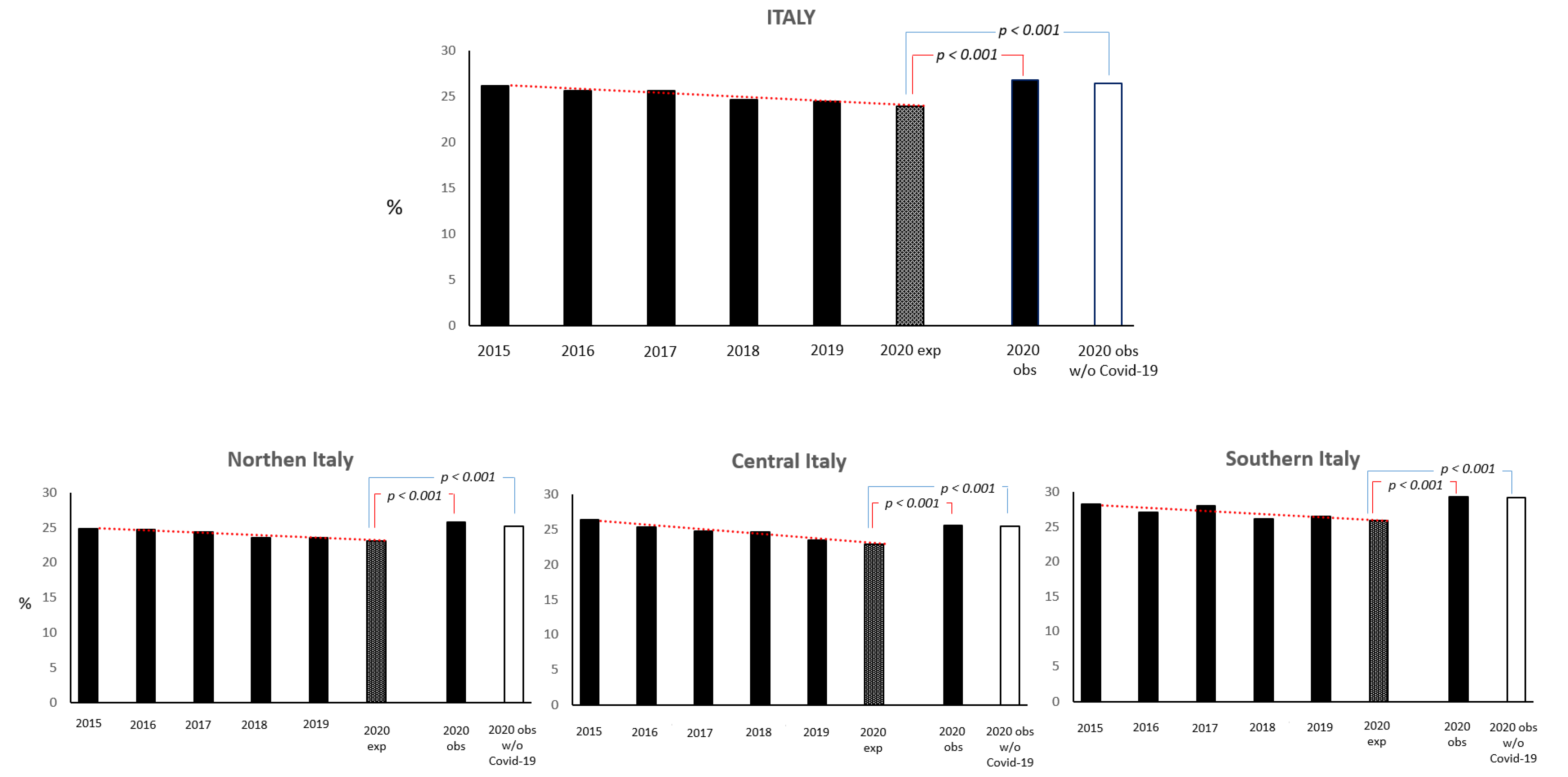
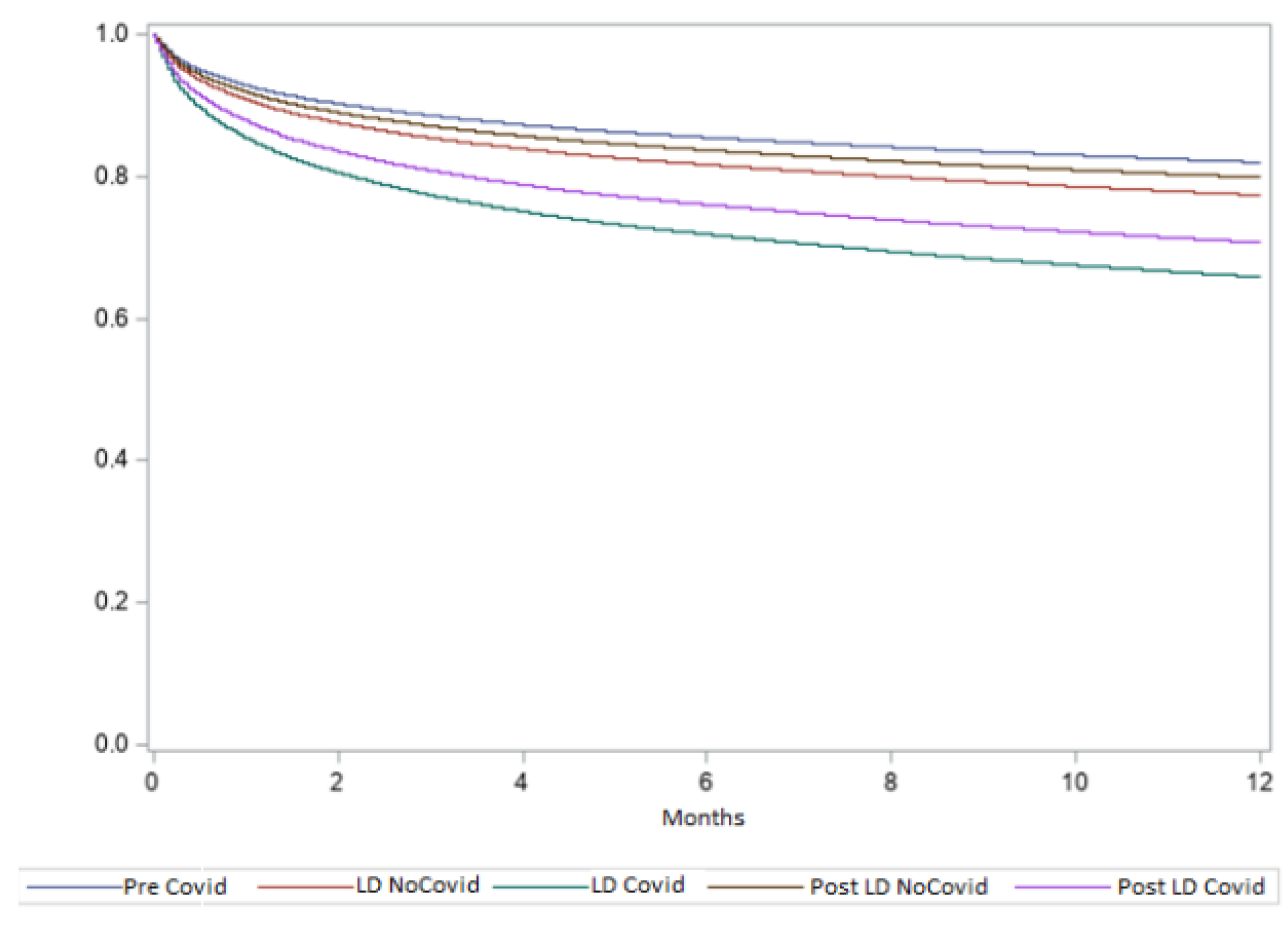
Mortality Trends
4. Discussion
Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Dong, E.; Du, H.; Gardner, L. An interactive web-based dashboard to track COVID-19 in real time. Lancet Infect. Dis. 2020, 20, 533–534. [Google Scholar] [PubMed]
- Aveyard, P.; Gao, M.; Lindson, N.; Hartmann-Boyce, J.; Watkinson, P.; Young, D.; Coupland, C.A.C.; Tan, P.S.; Clift, A.K.; Harrison, D.; et al. Association between pre-existing respiratory disease and its treatment, and severe COVID-19: A population cohort study. Lancet Respir. Med. 2021, 9, 909–923. [Google Scholar] [PubMed]
- Gluckman, T.J.; Wilson, M.A.; Chiu, S.T.; Penny, B.W.; Chepuri, V.B.; Waggoner, J.W.; Spinelli, K.J. Case Rates, Treatment Approaches, and Outcomes in Acute Myocardial Infarction During the Coronavirus Disease 2019 Pandemic. JAMA Cardiol. 2020, 5, 1419–1424. [Google Scholar] [PubMed]
- De Luca, L.; Rosato, S.; D’Errigo, P.; Giordani, B.; Mureddu, G.F.; Badoni, G.; Seccareccia, F.; Baglio, G. COVID-19 diagnosis and mortality in patients with non-ST-elevation myocardial infarction admitted in Italy during the national outbreak. Int. J. Cardiol. 2023, 370, 447–453. [Google Scholar] [PubMed]
- Rudilosso, S.; Laredo, C.; Vera, V.; Vargas, M.; Renú, A.; Llull, L.; Obach, V.; Amaro, S.; Urra, X.; Torres, F.; et al. Acute stroke care is at risk in the era of COVID-19: Experience at a comprehensive stroke center in Barcelona. Stroke 2020, 51, 1991–1995. [Google Scholar] [PubMed]
- Nguyen-Huynh, M.N.; Tang, X.N.; Vinson, D.R.; Flint, A.C.; Alexander, J.G.; Meighan, M.; Burnett, M.; Sidney, S.; Klingman, J.G. Acute stroke presentation, care, and outcomes in community hospitals in Northern California during the COVID-19 pandemic. Stroke 2020, 51, 2918–2924. [Google Scholar]
- Outcomes Evaluation National Program [PNE] Ed. 2022. Available online: https://pne.agenas.it (accessed on 12 January 2023).
- Sacco, S.; Ricci, S.; Ornello, R.; Eusebi, P.; Petraglia, L.; Toni, D.; Italian Stroke Organization. Reduced Admissions for Cerebrovascular Events During COVID-19 Outbreak in Italy. Stroke 2020, 51, 3746–3750. [Google Scholar]
- Mariet, A.; Giroud, M.; Benzenine, E.; Cottenet, J.; Roussot, A.; Aho-Glélé, L.S.; Tubert-Bitter, P.; Béjot, Y.; Quantin, C. Hospitalizations for Stroke in France During the COVID-19 Pandemic Before, During, and After the National Lockdown. Stroke 2021, 52, 1362–1369. [Google Scholar]
- Zhao, J.; Li, H.; Kung, D.; Fisher, M.; Shen, Y.; Liu, R. Impact of the COVID-19 epidemic on stroke care and potential solutions. Stroke 2020, 51, 1996–2001. [Google Scholar]
- Baracchini, C.; Pieroni, A.; Viaro, F.; Cianci, V.; Cattelan, A.M.; Tiberio, I.; Munari, M.; Causin, F. Acute stroke management pathway during coronavirus-19 pandemic. Neurol. Sci. 2020, 41, 1003–1005. [Google Scholar]
- Morelli, N.; Rota, E.; Terracciano, C.; Immovilli, P.; Spallazzi, M.; Colombi, D.; Zaino, D.; Michieletti, E.; Guidetti, D. The baffing case of ischemic stroke disappearance from the casualty department in the COVID-19 era. Eur. Neurol. 2020, 83, 213–215. [Google Scholar] [PubMed]
- Liu, R.; Zhao, J.; Fischer, M. The global impact of COVID-19 on acute stroke care. CNS Neurosci. Ther. 2020, 26, 1103–1105. [Google Scholar]
- Pop, R.; Quenardelle, V.; Hasiu, A.; Mihoc, D.; Sellal, F.; Dugay, M.H.; Lebedinsky, P.A.; Schluck, E.; LA Porta, A.; Courtois, S.; et al. Impact of the COVID-19 outbreak on acute stroke pathways—Insights from the Alsace region in France. Eur. J. Neurol. 2020, 27, 1783–1787. [Google Scholar] [PubMed]
- July, J.; Pranata, R. Impact of the coronavirus disease pandemic on the number of strokes and mechanical thrombectomy: A systematic review and meta-analysis. J. Stroke Cerebrovasc. Dis. 2020, 29, 105–185. [Google Scholar]
- Benussi, A.; Premi, E.; Pilotto, A.; Libri, I.; Pezzini, A.; Paolillo, C.; Borroni, B.; Magoni, M.; Padovani, A. Effects of COVID-19 outbreak on stroke admissions in Brescia, Lombardy, Italy. Eur. J. Neurol. 2021, 28, e4–e5. [Google Scholar]
- Man, S.; Cox, M.; Patel, P.; Smith, E.E.; Reeves, M.J.; Saver, J.L.; Bhatt, D.L.; Xian, Y.; Schwamm, L.H.; Fonarow, G.C. Differences in acute ischemic stroke quality of care and outcomes by primary stroke center certification organization. Stroke 2017, 48, 412–419. [Google Scholar] [PubMed]
- Yaghi, S.; Ishida, K.; Torres, J.; Mac Grory, B.; Raz, E.; Humbert, K.; Henninger, N.; Trivedi, T.; Lillemoe, K.; Alam, S.; et al. SARS-CoV-2 and stroke in a New York healthcare system. Stroke 2020, 51, 2002–2011. [Google Scholar]
- Lange, S.J.; Ritchey, M.D.; Goodman, A.B.; Dias, T.; Twentyman, E.; Fuld, J.; Schieve, L.A.; Imperatore, G.; Benoit, S.R.; Kite-Powell, A.; et al. Potential indirect effects of the COVID-19 pandemic on use of emergency departments for acute life-threatening conditions—United States, January–May 2020. MMWR Morb. Mortal. Wkly. Rep. 2020, 69, 795–800. [Google Scholar]
- Sharma, R.; Kuohn, L.R.; Weinberger, D.M.; Warren, J.L.; Sansing, L.H.; Jasne, A.; Falcone, G.; Dhand, A.; Sheth, K.N. Excess Cerebrovascular Mortality in the United States During the COVID-19 Pandemic. Stroke 2021, 52, 563–572. [Google Scholar]
- Lazzerini, M.; Putoto, G. COVID-19 in Italy: Momentous decisions and many uncertainties. Lancet Glob. Health 2020, 8, e641–e642. [Google Scholar]
- Tan, C.W.; Low, J.G.H.; Wong, W.H.; Chua, Y.Y.; Goh, S.L.; Ng, H.J. Critically ill COVID-19 infected patients exhibit increased clot waveform analysis parameters consistent with hypercoagulability. Am. J. Hematol. 2020, 95, E156–E158. [Google Scholar] [PubMed]
- Goshua, G.; Pine, A.B.; Meizlish, M.L.; Chang, C.H.; Zhang, H.; Bahel, P.; Baluha, A.; Bar, N.; Bona, R.D.; Burns, A.J.; et al. Endotheliopathy in COVID-19-associated coagulopathy: Evidence from a single-centre, cross-sectional study. Lancet Haematol. 2020, 7, e575–e582. [Google Scholar] [PubMed]
- Merkler, A.E.; Parikh, N.S.; Mir, S.; Gupta, A.; Kamel, H.; Lin, E.; Lantos, J.; Schenck, E.J.; Goyal, P.; Bruce, S.S.; et al. Risk of ischemic stroke in patients with coronavirus disease 2019 (COVID-19) vs. patients with influenza. JAMA Neurol. 2020, 77, 1366–1372. [Google Scholar]
- Oxley, T.J.; Mocco, J.; Majidi, S.; Kellner, C.P.; Shoirah, H.; Singh, I.P.; De Leacy, R.A.; Shigematsu, T.; Ladner, T.R.; Yaeger, K.A.; et al. Large-vessel stroke as a presenting feature of COVID-19 in the young. New Engl. J. Med. 2020, 382, e60. [Google Scholar] [PubMed]

| 2015–2019 (N = 259,588) | 2020 Lockdown (N = 6586) | 2020 Post-Lockdown (N = 34,716) | p-Value | |
|---|---|---|---|---|
| Gender (females), n (%) | 128,630 (49.6) | 3214 (48.8) | 16710 (48.1) | <0.001 |
| Age (years), mean ± SD | 75.9 ± 12.3 | 75.7 ± 12.2 | 75.5 ± 12.4 | <0.001 |
| Malignant neoplasms, n (%) | 20,917 (8.1) | 525 (8.0) | 2781 (8.0) | 0.93 |
| Diabetes mellitus, n (%) | 27,114 (10.4) | 545 (8.3) | 3034 (8.7) | <0.001 |
| Dyslipidemias, n (%) | 9797 (3.8) | 221 (3.4) | 1134 (3.3) | <0.001 |
| Obesity, n (%) | 3892 (1.5) | 87 (1.3) | 500 (1.4) | 0.36 |
| Obesity (ind. adm.), n (%) | 2648 (1.0) | 91 (1.4) | 521 (1.5) | <0.001 |
| Anemia, n (%) | 12,402 (4.8) | 280 (4.3) | 1467 (4.2) | <0.001 |
| Anemia (ind. adm.), n (%) | 6217 (2.4) | 157 (2.4) | 864 (2.5) | 0.56 |
| Blood clotting defects, n (%) | 534 (0.2) | 14 (0.2) | 55 (0.2) | 0.18 |
| Blood clotting defects (ind. adm.), n (%) | 288 (0.1) | 7 (0.1) | 41 (0.1) | 0.92 |
| Other hematological diseases, n (%) | 1510 (0.6) | 34 (0.5) | 207 (0.6) | 0.73 |
| Other hematological diseases (ind. adm.), n (%) | 1197 (0.5) | 32 (0.5) | 195 (0.6) | 0.04 |
| Hypertension, n (%) | 50,247 (19.4) | 1085 (16.5) | 5345 (15.4) | <0.001 |
| Previous myocardial infarction, n (%) | 12,684 (4.9) | 250 (3.8) | 1477 (4.3) | <0.001 |
| Heart failure, n (%) | 21,903 (8.4) | 469 (7.1) | 2489 (7.2) | <0.001 |
| Chronic coronary syndromes, n (%) | 23,516 (9.1) | 510 (7.7) | 2599 (7.5) | <0.001 |
| Rheumatic heart disease, n (%) | 3266 (1.3) | 63 (1.0) | 343 (1.0) | <0.001 |
| Rheumatic heart disease (ind. adm.), n (%) | 1921 (0.7) | 58 (0.9) | 363 (1.0) | <0.001 |
| Cardiomyopathy, n (%) | 3769 (1.5) | 83 (1.3) | 427 (1.2) | 0.002 |
| Cardiomyopathy (ind. adm.), n (%) | 1247 (0.5) | 32 (0.5) | 163 (0.5) | 0.99 |
| Endocarditis and acute myocarditis, n (%) | 352 (0.1) | 9 (0.1) | 43 (0.1) | 0.85 |
| Arrhythmias, n (%) | 32,296 (12.4) | 704 (10.7) | 3567 (10.3) | <0.001 |
| Other chronic heart conditions, n (%) | 6355 (2.4) | 163 (2.5) | 814 (2.3) | 0.49 |
| Other chronic heart conditions (ind.adm.), n (%) | 6591 (2.5) | 189 (2.9) | 1068 (3.1) | <0.001 |
| Vascular disease, n (%) | 12,706 (4.9) | 288 (4.4) | 1404 (4.0) | <0.001 |
| Vascular disease (ind. adm.), n (%) | 8747 (3.4) | 245 (3.7) | 1390 (4.0) | <0.001 |
| Chronic obstructive pulmonary disease, n (%) | 14,382 (5.5) | 283 (4.3) | 1410 (4.1) | <0.001 |
| Chronic kidney disease, n (%) | 14,042 (5.4) | 341 (5.2) | 1556 (4.5) | <0.001 |
| Chronic kidney diseases (ind. adm.), n (%) | 11,582 (4.5) | 286 (4.3) | 1420 (4.1) | 0.006 |
| Other chronic disease (liver, pancreas, intestine), n (%) | 4401 (1.7) | 70 (1.1) | 459 (1.3) | <0.001 |
| Other chronic disease (liver, pancreas, intestine) (ind. adm.), n (%) | 2152 (0.8) | 31 (0.5) | 221 (0.6) | <0.001 |
| Previous coronary revascularization, n (%) | 12,399 (4.8) | 314 (4.8) | 1581 (4.6) | 0.19 |
| Previous coronary revascularization (ind. Adm.), n (%) | 5699 (2.2) | 151 (2.3) | 676 (1.9) | 0.009 |
| Previous vascular surgery, n (%) | 11,106 (4.3) | 291 (4.4) | 1398 (4.0) | 0.07 |
| Thrombolysis < 48 h, n (%) | 25,872 (10.0) | 791 (12.0) | 4228 (12.2) | <0.001 |
| Stroke unit, n (%) | 160,928 (62.0) | 4643 (70.5) | 24105 (69.4) | <0.001 |
| LOS (mean ± SD) | 10.3 ± 9.4 | 9.4 ± 8.7 | 9.6 ± 7.7 | <0.001 |
| COVID-19 diagnosis | 0 | 274 (4.2) | 828 (2.4) | <0.001 |
| HR | 95% CI | p-Value | ||
|---|---|---|---|---|
| Gender, females | 1.07 | 1.06 | 1.09 | <0.0001 |
| Age, years | 1.09 | 1.08 | 1.09 | <0.0001 |
| Pre-COVID-19 | Ref | |||
| Lockdown—No COVID-19 | 1.29 | 1.23 | 1.35 | <0.0001 |
| Lockdown—COVID-19 | 2.11 | 1.76 | 2.52 | <0.0001 |
| Post-Lockdown—No COVID-19 | 1.14 | 1.11 | 1.16 | <0.0001 |
| Post-Lockdown—COVID-19 | 1.75 | 1.56 | 1.96 | <0.0001 |
| Malignant neoplasms | 1.26 | 1.23 | 1.29 | <0.0001 |
| Diabetes mellitus | 1.23 | 1.20 | 1.26 | <0.0001 |
| Dyslipidemia | 0.81 | 0.78 | 0.85 | <0.0001 |
| Obesity | 1.11 | 1.05 | 1.17 | 0.0002 |
| Anemia | 1.18 | 1.15 | 1.21 | <0.0001 |
| Anemia (ind. adm.) | 1.12 | 1.08 | 1.17 | <0.0001 |
| Blood clotting defects | 1.18 | 1.04 | 1.33 | 0.008 |
| Blood clotting defects (ind. adm.) | 1.62 | 1.29 | 2.05 | <0.0001 |
| Other hematological diseases | 1.29 | 1.20 | 1.39 | <0.0001 |
| Hypertension | 0.97 | 0.95 | 0.99 | 0.003 |
| Previous myocardial infarction | 1.10 | 1.06 | 1.14 | <0.0001 |
| Heart failure | 1.37 | 1.34 | 1.40 | <0.0001 |
| Rheumatic heart disease | 1.08 | 1.02 | 1.13 | 0.004 |
| Rheumatic heart disease (ind. adm.) | 0.76 | 0.70 | 0.83 | <0.0001 |
| Cardiomyopathy | 1.23 | 1.17 | 1.29 | <0.0001 |
| Endocarditis and acute myocarditis | 1.26 | 1.07 | 1.48 | 0.006 |
| Other chronic heart conditions | 1.09 | 1.05 | 1.14 | <0.0001 |
| Other chronic heart conditions (ind.adm.) | 0.81 | 0.76 | 0.86 | <0.0001 |
| Arrhythmias | 1.22 | 1.20 | 1.25 | <0.0001 |
| Vascular disease | 1.13 | 1.09 | 1.17 | <0.0001 |
| Vascular disease (ind. adm.) | 0.77 | 0.74 | 0.81 | <0.0001 |
| Chronic obstructive pulmonary disease | 1.20 | 1.17 | 1.23 | <0.0001 |
| Chronic kidney disease | 1.21 | 1.18 | 1.24 | <0.0001 |
| Chronic kidney diseases (ind. adm.) | 1.08 | 1.05 | 1.11 | <0.0001 |
| Other chronic disease (liver, pancreas, intestine) | 1.20 | 1.14 | 1.26 | <0.0001 |
| Other chronic disease (liver, pancreas, intestine) (ind. adm.) | 1.22 | 1.12 | 1.32 | <0.0001 |
| Previous coronary revascularization | 0.86 | 0.83 | 0.90 | <0.0001 |
| Previous vascular surgery | 1.31 | 1.27 | 1.36 | <0.0001 |
| Thrombolysis < 48 h | 0.93 | 0.91 | 0.96 | <0.0001 |
| Stroke unit admission | 0.76 | 0.75 | 0.78 | <0.0001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
De Luca, L.; D’Errigo, P.; Rosato, S.; Badoni, G.; Giordani, B.; Mureddu, G.F.; Tavilla, A.; Seccareccia, F.; Baglio, G. Impact of COVID-19 Diagnosis on Mortality in Patients with Ischemic Stroke Admitted during the 2020 Pandemic in Italy. J. Clin. Med. 2023, 12, 4560. https://doi.org/10.3390/jcm12144560
De Luca L, D’Errigo P, Rosato S, Badoni G, Giordani B, Mureddu GF, Tavilla A, Seccareccia F, Baglio G. Impact of COVID-19 Diagnosis on Mortality in Patients with Ischemic Stroke Admitted during the 2020 Pandemic in Italy. Journal of Clinical Medicine. 2023; 12(14):4560. https://doi.org/10.3390/jcm12144560
Chicago/Turabian StyleDe Luca, Leonardo, Paola D’Errigo, Stefano Rosato, Gabriella Badoni, Barbara Giordani, Gian Francesco Mureddu, Andrea Tavilla, Fulvia Seccareccia, and Giovanni Baglio. 2023. "Impact of COVID-19 Diagnosis on Mortality in Patients with Ischemic Stroke Admitted during the 2020 Pandemic in Italy" Journal of Clinical Medicine 12, no. 14: 4560. https://doi.org/10.3390/jcm12144560
APA StyleDe Luca, L., D’Errigo, P., Rosato, S., Badoni, G., Giordani, B., Mureddu, G. F., Tavilla, A., Seccareccia, F., & Baglio, G. (2023). Impact of COVID-19 Diagnosis on Mortality in Patients with Ischemic Stroke Admitted during the 2020 Pandemic in Italy. Journal of Clinical Medicine, 12(14), 4560. https://doi.org/10.3390/jcm12144560







