The Association between Emergency Department Length of Stay and In-Hospital Mortality in Older Patients Using Machine Learning: An Observational Cohort Study
Abstract
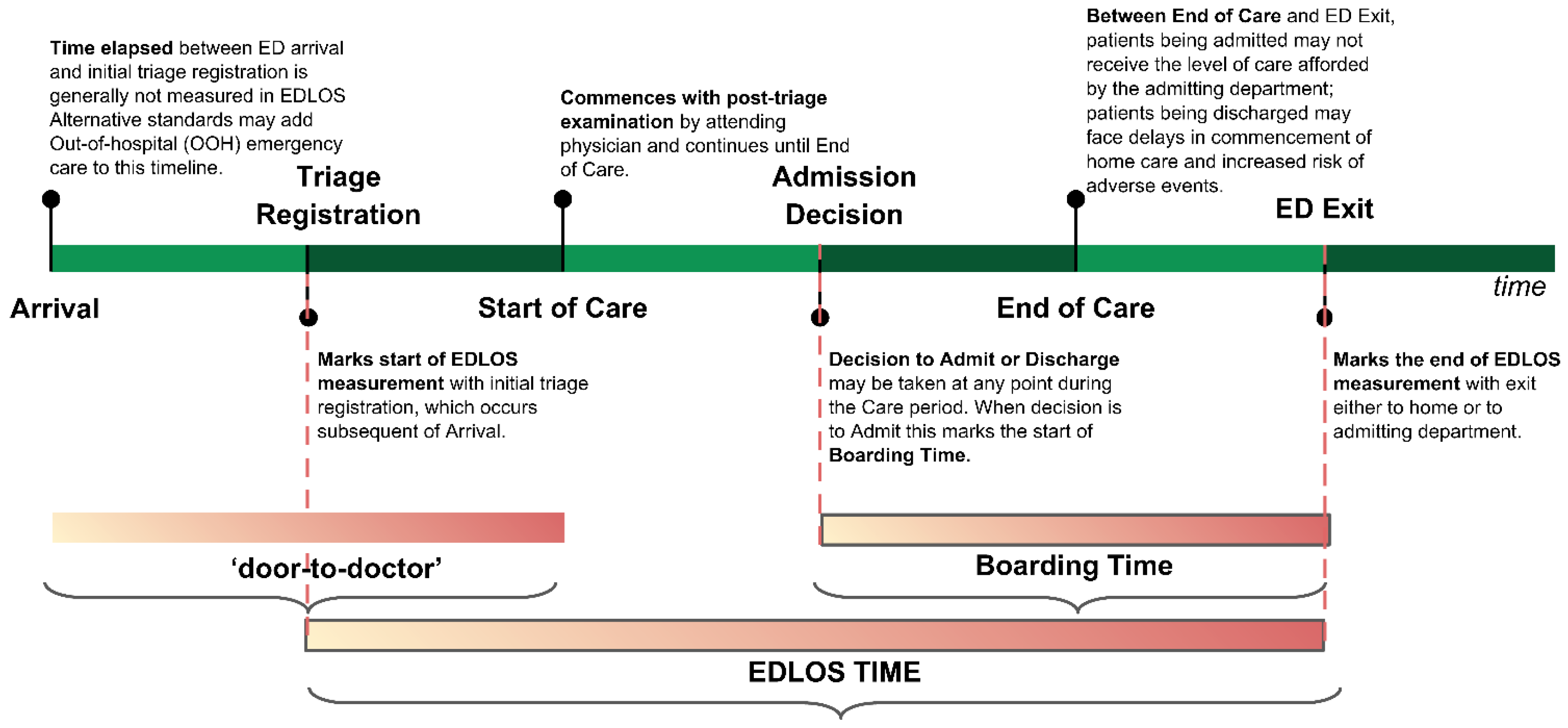
:1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Data Collection and Data Processing
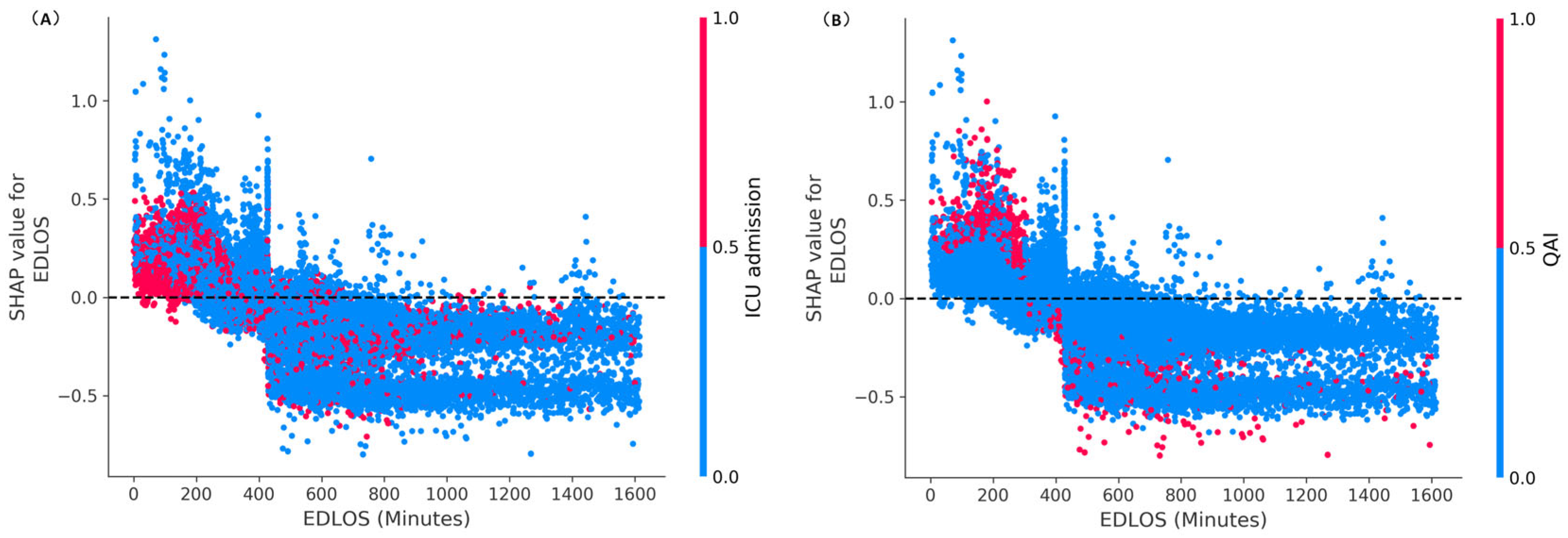
2.3. Experimental Methodology
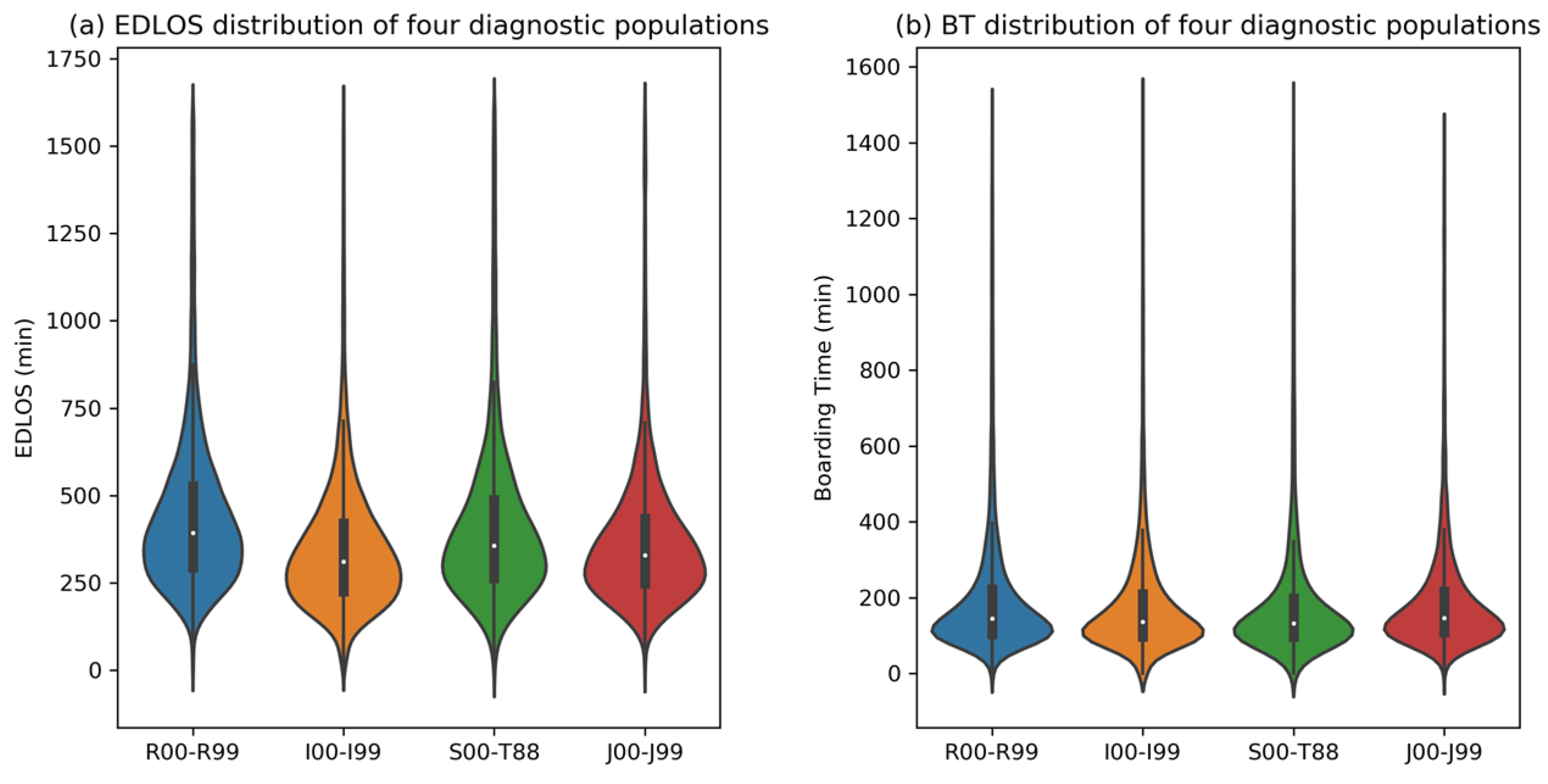
2.4. Diagnosis Subgroup Analysis
2.5. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Savioli, G.; Ceresa, I.F.; Gri, N.; Bavestrello Piccini, G.; Longhitano, Y.; Zanza, C.; Piccioni, A.; Esposito, C.; Ricevuti, G.; Bressan, M.A. Emergency department overcrowding: Understanding the factors to find corresponding solutions. J. Pers. Med. 2022, 12, 279. [Google Scholar] [CrossRef]
- Bouillon-Minois, J.-B.; Raconnat, J.; Clinchamps, M.; Schmidt, J.; Dutheil, F. Emergency department and overcrowding during COVID-19 outbreak; a letter to editor. Arch. Acad. Emerg. Med. 2021, 9, e28. [Google Scholar]
- Mohr, N.M.; Wessman, B.T.; Bassin, B.; Elie-Turenne, M.-C.; Ellender, T.; Emlet, L.L.; Ginsberg, Z.; Gunnerson, K.; Jones, K.M.; Kram, B.; et al. Boarding of critically ill patients in the emergency department. J. Am. Coll. Emerg. Physicians Open 2020, 1, 423–431. [Google Scholar] [CrossRef]
- Horwitz, L.I.; Green, J.; Bradley, E.H. US emergency department performance on wait time and length of visit. Ann. Emerg. Med. 2010, 55, 133–141. [Google Scholar] [CrossRef] [Green Version]
- Forero, R.; Man, N.; Ngo, H.; Mountain, D.; Mohsin, M.; Fatovich, D.; Toloo, G.; Celenza, A.; FitzGerald, G.; McCarthy, S.; et al. Impact of the four-hour National Emergency Access Target on 30 day mortality, access block and chronic emergency department overcrowding in Australian emergency departments. Emerg. Med. Australas. 2019, 31, 58–66. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Boudi, Z.; Lauque, D.; Alsabri, M.; Östlundh, L.; Oneyji, C.; Khalemsky, A.; Lojo Rial, C.; Liu, S.W.; Camargo, C.A., Jr.; Aburawi, E.; et al. Association between boarding in the emergency department and in-hospital mortality: A systematic review. PLoS ONE 2020, 15, e0231253. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gabayan, G.Z.; Derose, S.F.; Chiu, V.Y.; Yiu, S.C.; Sarkisian, C.A.; Jones, J.P.; Sun, B.C. Emergency department crowding and outcomes after emergency department discharge. Ann. Emerg. Med. 2015, 66, 483–492. [Google Scholar] [CrossRef] [Green Version]
- Lauque, D.; Khalemsky, A.; Boudi, Z.; Östlundh, L.; Xu, C.; Alsabri, M.; Onyeji, C.; Cellini, J.; Intas, G.; Soni, K.D.; et al. Length-of-Stay in the Emergency Department and In-Hospital Mortality: A Systematic Review and Meta-Analysis. J. Clin. Med. 2023, 12, 32. [Google Scholar] [CrossRef] [PubMed]
- Alsabri, M.; Boudi, Z.; Zoubeidi, T.; Alfaki, I.A.; Levy, P.; Oneyji, C.; Shan, L.; Camargo, C.A., Jr.; Michel, P.; Tazarourte, K.; et al. Analysis of risk factors for patient safety events occurring in the emergency department. J. Patient Saf. 2022, 18, e124–e135. [Google Scholar] [CrossRef]
- Vinutha, H.P.; Poornima, B.; Sagar, B.M. Detection of outliers using interquartile range technique from intrusion dataset. In Information and Decision Sciences; Springer: Berlin/Heidelberg, Germany, 2018; pp. 511–518. [Google Scholar]
- Breiman, L. Random forests. Mach. Learn. 2001, 45, 5–32. [Google Scholar] [CrossRef] [Green Version]
- Chen, T.; Guestrin, C. XGBoost: A scalable tree boosting system. In Proceedings of the 22nd Acm Sigkdd International Conference on Knowledge Discovery and Data Mining, San Francisco, CA, USA, 13–17 August 2016; pp. 785–794. [Google Scholar]
- Ke, G.; Meng, Q.; Finley, T.; Wang, T.; Chen, W.; Ma, W.; Ye, Q.; Liu, T.-Y. Lightgbm: A highly efficient gradient boosting decision tree. Adv. Neural Inf. Process. Syst. 2017, 30, 3146–3154. [Google Scholar]
- Lundberg, S.M.; Lee, S.-I. A unified approach to interpreting model predictions. Adv. Neural Inf. Process. Syst. 2017, 30, 4765–4774. [Google Scholar]
- Sun, X.; Xu, W. Fast implementation of DeLong’s algorithm for comparing the areas under correlated receiver operating characteristic curves. IEEE Signal Process. Lett. 2014, 21, 1389–1393. [Google Scholar] [CrossRef]
- Lundberg, S.; Erion, G.G.; Chen, H.; Degrave, A.J.; Prutkin, J.M.; Nair, B.G.; Katz, R.; Himmelfarb, J.; Bansal, N.; Lee, S. From local explanations to global understanding with explainable AI for trees. Nat. Mach. Intell. 2020, 2, 56–67. [Google Scholar] [CrossRef] [PubMed]
- Lundberg, S.M.; Erion, G.; Chen, H.; DeGrave, A.; Prutkin, J.M.; Nair, B.; Katz, R.; Himmelfarb, J.; Bansal, N.; Lee, S.-I. Explainable AI for Trees: From Local Explanations to Global Understanding. arXiv 2019, arXiv:1905.04610. [Google Scholar] [CrossRef]
- Lundberg, S.M.; Erion, G.G.; Lee, S.-I. Consistent individualized feature attribution for tree ensembles. arXiv 2018, arXiv:1802.03888. [Google Scholar]
- Cardoso, L.T.Q.; Grion, C.; Matsuo, T.; Anami, E.H.T.; Kauss, I.A.M.; Seko, L.; Bonametti, A.M. Impact of delayed admission to intensive care units on mortality of critically ill patients: A cohort study. Crit. Care 2011, 15, R28. [Google Scholar] [CrossRef] [Green Version]
- Cheng, T.; Peng, Q.; Jin, Y.; Yu, H.; Zhong, P.; Gu, W.; Wang, X.; Lu, Y.; Luo, L. Access block and prolonged length of stay in the emergency department are associated with a higher patient mortality rate. World J. Emerg. Med. 2022, 13, 59. [Google Scholar] [CrossRef]
- Asheim, A.; Nilsen, S.M.; Carlsen, F.; Næss-Pleym, L.E.; Uleberg, O.; Dale, J.; Bjørnsen, L.P.B.-W.; Bjørngaard, J.H. The effect of emergency department delays on 30-day mortality in Central Norway. Eur. J. Emerg. Med. 2019, 26, 446–452. [Google Scholar] [CrossRef] [Green Version]
- Groenland, C.N.L.; Termorshuizen, F.; Rietdijk, W.J.R.; van den Brule, J.; Dongelmans, D.A.; de Jonge, E.; de Lange, D.W.; de Smet, A.M.G.A.; de Keizer, N.F.; Weigel, J.D.; et al. Emergency department to ICU time is associated with hospital mortality: A registry analysis of 14,788 patients from six university hospitals in The Netherlands. Crit. Care Med. 2019, 47, 1564. [Google Scholar] [CrossRef]
- Siletz, A.; Jin, K.; Cohen, M.; Lewis, C.; Tillou, A.; Cryer, H.M.; Cheaito, A. Emergency department length of stay in critical nonoperative trauma. J. Surg. Res. 2017, 214, 102–108. [Google Scholar] [CrossRef] [PubMed]
- Mowery, N.T.; Dougherty, S.D.; Hildreth, A.N.; Holmes IV, J.H.; Chang, M.C.; Martin, R.S.; Hoth, J.J.; Meredith, J.W.; Miller, P.R. Emergency department length of stay is an independent predictor of hospital mortality in trauma activation patients. J. Trauma Acute Care Surg. 2011, 70, 1317–1325. [Google Scholar] [CrossRef] [PubMed]
- Aitavaara-Anttila, M.; Liisanantti, J.H.; Raatiniemi, L.; Ohtonen, P.; Ala-Kokko, T. Factors related to delayed intensive care unit admission from emergency department—A retrospective cohort study. Acta Anaesthesiol. Scand. 2019, 63, 939–946. [Google Scholar] [CrossRef] [Green Version]
- Paton, A.; Mitra, B.; Considine, J. Longer time to transfer from the emergency department after bed request is associated with worse outcomes. Emerg. Med. Australas. 2019, 31, 211–215. [Google Scholar] [CrossRef] [PubMed]
- Ashkenazi, I.; Gefen, L.; Hochman, O.; Tannous, E. The 4-hour target in the emergency department, in-hospital mortality, and length of hospitalization: A single center-retrospective study. Am. J. Emerg. Med. 2021, 47, 95–100. [Google Scholar] [CrossRef]
- Aletreby, W.T.; Brindley, P.G.; Balshi, A.N.; Huwait, B.M.; Alharthy, A.M.; Madi, A.F.; Ramadan, O.E.; Noor, A.S.N.; Alzayer, W.S.; Alodat, M.A.; et al. Delayed intensive care unit admission from the emergency department: Impact on patient outcomes. A retrospective study. Rev. Bras. Ter. Intensiva 2021, 33, 125–137. [Google Scholar] [PubMed]
- Jones, E.M.; Boehme, A.K.; Aysenne, A.; Chang, T.; Albright, K.C.; Burns, C.; Beasley, T.M.; Martin-Schild, S. Prolonged emergency department length of stay as a predictor of adverse outcomes in patients with intracranial hemorrhage. J. Crit. Care Med. 2015, 2015, 526319. [Google Scholar] [CrossRef] [Green Version]
- Stey, A.M.; Kanzaria, H.K.; Dudley, R.A.; Bilimoria, K.Y.; Knudson, M.M.; Callcut, R.A. Emergency department length of stay and mortality in critically injured patients. J. Intensive Care Med. 2022, 37, 278–287. [Google Scholar] [CrossRef]
- Chen, H.-C.; Lee, W.-C.; Chen, Y.-L.; Fang, H.-Y.; Chen, C.-J.; Yang, C.-H.; Hang, C.-L.; Fang, C.-Y.; Yip, H.-K.; Wu, C.-J. The impacts of prolonged emergency department length of stay on clinical outcomes of patients with ST-segment elevation myocardial infarction after reperfusion. Intern. Emerg. Med. 2016, 11, 107–114. [Google Scholar] [CrossRef]
- Mitra, B.; Cameron, P.A.; Archer, P.; Bailey, M.; Pielage, P.; Mele, G.; Smit, D.V.; Newnham, H. The association between time to disposition plan in the emergency department and in-hospital mortality of general medical patients. Intern. Med. J. 2012, 42, 444–450. [Google Scholar] [CrossRef]
- Choi, W.; Woo, S.H.; Kim, D.H.; Lee, J.Y.; Lee, W.J.; Jeong, S.; Cha, K.; Youn, C.S.; Park, S. Prolonged length of stay in the emergency department and mortality in critically ill elderly patients with infections: A retrospective multicenter study. Emerg. Med. Int. 2021, 2021, 9952324. [Google Scholar] [CrossRef] [PubMed]
- Verma, A.; Shishodia, S.; Jaiswal, S.; Sheikh, W.R.; Haldar, M.; Vishen, A.; Ahuja, R.; Khatai, A.A.; Khanna, P. Increased Length of Stay of Critically Ill Patients in the Emergency Department Associated with Higher In-hospital Mortality. Indian J. Crit. Care Med. Peer-Rev. Off. Publ. Indian Soc. Crit. Care Med. 2021, 25, 1221. [Google Scholar] [CrossRef] [PubMed]
- Singer, A.J.; Thode, H.C., Jr.; Viccellio, P.; Pines, J.M. The association between length of emergency department boarding and mortality. Acad. Emerg. Med. 2011, 18, 1324–1329. [Google Scholar] [CrossRef] [PubMed]





| Characteristics | (n = 78,847) | Early Elderly, Age 60–74 (n = 38,817) | Late Elderly, Age 75–89 (n = 32,261) | Longevous Elderly, 90 (n = 7769) | p Value |
|---|---|---|---|---|---|
| Age, years, median (Q1, Q3) | 75 (67, 84) | 67 (63, 70) | 82 (78, 85) | 92 (91, 95) | <0.001 |
| Male, n (%) | 37,211 (47.2) | 20,052 (51.7) | 14,535 (45.1) | 2624 (33.8) | <0.001 |
| Race, n (%) | <0.001 | ||||
| Unknown | 1428 (1.8) | 654 (1.7) | 624 (1.9) | 150 (1.9) | |
| White | 57,429 (72.8) | 26,966 (69.5) | 24,167 (74.9) | 6296 (81) | |
| Black | 11,675 (14.8) | 6658 (17.2) | 4205 (13) | 812 (10.5) | |
| Hispanic | 3032 (3.8) | 1847 (4.8) | 1079 (3.3) | 106 (1.4) | |
| Asian | 2497 (3.2) | 1240 (3.2) | 1077 (3.3) | 180 (2.3) | |
| Other | 2786 (3.5) | 1452 (3.7) | 1109 (3.4) | 225 (2.9) | |
| Language-English, n (%) | 68,213 (86.5) | 34,919 (90) | 26,809 (83.1) | 6485 (83.5) | <0.001 |
| Insurance, n (%) | <0.001 | ||||
| Unknown | 3,970 (5) | 2147 (5.5) | 1494 (4.6) | 329 (4.2) | |
| Medicare | 54,441 (69) | 20,920 (53.9) | 26,750 (82.9) | 6771 (87.2) | |
| Medicaid | 106 (0.1) | 72 (0.2) | 25 (0.1) | 9 (0.1) | |
| Other | 20,330 (25.8) | 15,678 (40.4) | 3992 (12.4) | 660 (8.5) | |
| Triage and acuity score, n (%) | <0.001 | ||||
| Resuscitation | 12,565 (15.9) | 5870 (15.1) | 5323 (16.5) | 1372 (17.7) | |
| Emergent | 37,963 (48.1) | 18,430 (47.5) | 15,837 (49.1) | 3696 (47.6) | |
| Urgent | 28,095 (35.6) | 14,396 (37.1) | 11,013 (34.1) | 2686 (34.6) | |
| Less urgent | 217 (0.3) | 117 (0.3) | 86 (0.3) | 14 (0.2) | |
| Nonurgent | 7 (0) | 4 (0) | 2 (0) | 1 (0) | |
| Mode of transport, n (%) | <0.001 | ||||
| Unknown | 2312 (2.9) | 1127 (2.9) | 962 (3) | 223 (2.9) | |
| Walk-in | 32,888 (41.7) | 18,863 (48.6) | 11,953 (37.1) | 2072 (26.7) | |
| Ambulance | 43,215 (54.8) | 18,592 (47.9) | 19,178 (59.4) | 5445 (70.1) | |
| Helicopter | 340 (0.4) | 178 (0.5) | 143 (0.4) | 19 (0.2) | |
| Other | 92 (0.1) | 57 (0.1) | 25 (0.1) | 10 (0.1) | |
| ED waiting time, min, median (Q1, Q3) | 10 (6, 29) | 11 (6, 33) | 10 (5, 27) | 9 (5, 23) | <0.001 |
| Length of stay in ED, min, median (Q1, Q3) | 366 (271, 495) | 370 (272, 503) | 360 (269, 488) | 363 (272, 487) | <0.001 |
| Boarding time, min, median (Q1, Q3) | 143 (104, 219) | 145 (104, 223) | 141 (103, 214) | 144 (105, 218) | <0.001 |
| Charlson score, n (%) | <0.001 | ||||
| 0 | 54,001 (68.5) | 26,713 (68.8) | 21,691 (67.2) | 5597 (72) | |
| 1 | 16,995 (21.6) | 7613 (19.6) | 7632 (23.7) | 1750 (22.5) | |
| 2 | 4271 (5.4) | 2192 (5.6) | 1757 (5.4) | 322 (4.1) | |
| >2 | 3580 (4.5) | 2299 (6) | 1181 (3.7) | 100 (1.4) | |
| Quality Assurance Issue (QAI), n (%) | 1960 (2.5) | 882 (2.3) | 859 (2.7) | 219 (2.8) | 0.001 |
| Patient Safety Events (PSE), n (%) | 129 (0.2) | 53 (0.1) | 60 (0.2) | 16 (0.2) | 0.167 |
| ICU admission, n (%) | 16,668 (21.1) | 7996 (20.6) | 7039 (21.8) | 1633 (21) | <0.001 |
| Death in hospital, n (%) | 2975 (3.8) | 1046 (2.7) | 1440 (4.5) | 489 (6.3) | <0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wu, L.; Chen, X.; Khalemsky, A.; Li, D.; Zoubeidi, T.; Lauque, D.; Alsabri, M.; Boudi, Z.; Kumar, V.A.; Paxton, J.; et al. The Association between Emergency Department Length of Stay and In-Hospital Mortality in Older Patients Using Machine Learning: An Observational Cohort Study. J. Clin. Med. 2023, 12, 4750. https://doi.org/10.3390/jcm12144750
Wu L, Chen X, Khalemsky A, Li D, Zoubeidi T, Lauque D, Alsabri M, Boudi Z, Kumar VA, Paxton J, et al. The Association between Emergency Department Length of Stay and In-Hospital Mortality in Older Patients Using Machine Learning: An Observational Cohort Study. Journal of Clinical Medicine. 2023; 12(14):4750. https://doi.org/10.3390/jcm12144750
Chicago/Turabian StyleWu, Lijuan, Xuanhui Chen, Anna Khalemsky, Deyang Li, Taoufik Zoubeidi, Dominique Lauque, Mohammed Alsabri, Zoubir Boudi, Vijaya Arun Kumar, James Paxton, and et al. 2023. "The Association between Emergency Department Length of Stay and In-Hospital Mortality in Older Patients Using Machine Learning: An Observational Cohort Study" Journal of Clinical Medicine 12, no. 14: 4750. https://doi.org/10.3390/jcm12144750
APA StyleWu, L., Chen, X., Khalemsky, A., Li, D., Zoubeidi, T., Lauque, D., Alsabri, M., Boudi, Z., Kumar, V. A., Paxton, J., Tsilimingras, D., Kurland, L., Schwartz, D., Hachimi-Idrissi, S., Camargo, C. A., Jr., Liu, S. W., Savioli, G., Intas, G., Soni, K. D., ... Bellou, A. (2023). The Association between Emergency Department Length of Stay and In-Hospital Mortality in Older Patients Using Machine Learning: An Observational Cohort Study. Journal of Clinical Medicine, 12(14), 4750. https://doi.org/10.3390/jcm12144750










