Contact Mechanics of Elliptical and Spherical Head Implants during Axial Rotation in Anatomic Total Shoulder Arthroplasty: A Biomechanical Comparison
Abstract
:1. Introduction
2. Materials and Methods
2.1. Specimen Preparation
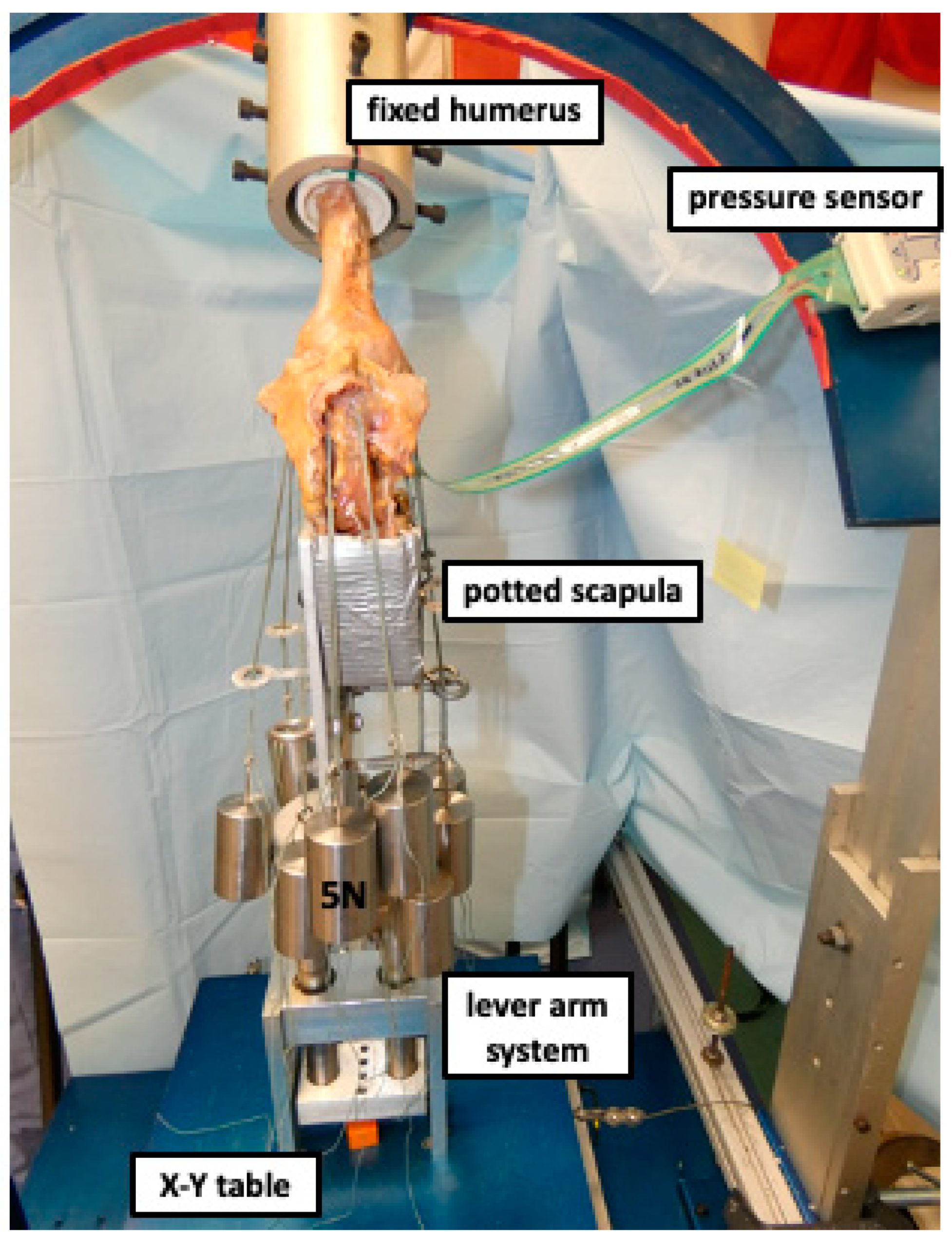
2.2. Testing Setup
2.3. Surgical Technique
2.4. Humeral Head Prosthetic Design
2.5. Biomechanical Testing
2.6. Statistical Analysis
3. Results
3.1. Contact Pressure
3.2. Peak Contact Pressure
3.3. Contact Area
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Bryant, D.; Litchfield, R.; Sandow, M.; Gartsman, G.M.; Guyatt, G.; Kirkley, A. A comparison of pain, strength, range of motion, and functional outcomes after hemiarthroplasty and total shoulder arthroplasty in patients with osteoarthritis of the shoulder. A systematic review and meta-analysis. J. Bone Jt. Surg. Am. 2005, 87, 1947–1956. [Google Scholar] [CrossRef] [Green Version]
- Lo, I.K.; Litchfield, R.; Griffin, S.; Faber, K.; Patterson, S.D.; Kirkley, A. Quality-of-life outcome following hemiarthroplasty or total shoulder arthroplasty in patients with osteoarthritis. A prospective, randomized trial. J. Bone Jt. Surg. Am. 2005, 87, 2178–2185. [Google Scholar]
- Hawi, N.; Magosch, P.; Tauber, M.; Lichtenberg, S.; Habermeyer, P. Nine-year outcome after anatomic stemless shoulder prosthesis: Clinical and radiologic results. J. Shoulder Elb. Surg. 2017, 26, 1609–1615. [Google Scholar] [CrossRef] [PubMed]
- Bigliani, L.U.; Kelkar, R.; Flatow, E.L.; Pollock, R.G.; Mow, V.C. Glenohumeral stability. Biomechanical properties of passive and active stabilizers. Clin. Orthop. Relat. Res. 1996, 330, 13–30. [Google Scholar] [CrossRef]
- Karduna, A.R.; Williams, G.R.; Williams, J.L.; Iannotti, J.P. Kinematics of the glenohumeral joint: Influences of muscle forces, ligamentous constraints, and articular geometry. J. Orthop. Res. 1996, 14, 986–993. [Google Scholar] [CrossRef] [Green Version]
- Kelkar, R.; Wang, V.M.; Flatow, E.L.; Newton, P.M.; Ateshian, G.; Bigliani, L.U.; Pawluk, R.J.; Mow, V.C. Glenohumeral mechanics: A study of articular geometry, contact, and kinematics. J. Shoulder Elb. Surg. 2001, 10, 73–84. [Google Scholar] [CrossRef]
- Soslowsky, L.J.; Flatow, E.L.; Bigliani, L.U.; Mow, V.C. Articular geometry of the glenohumeral joint. Clin. Orthop. Relat. Res. 1992, 285, 181–190. [Google Scholar] [CrossRef]
- Humphrey, C.S.; Sears, B.W.; Curtin, M.J. An anthropometric analysis to derive formulae for calculating the dimensions of anatomically shaped humeral heads. J. Shoulder Elb. Surg. 2016, 25, 1532–1541. [Google Scholar] [CrossRef]
- Humphrey, C.S.; Gale, A.L. Spherical versus elliptical prosthetic humeral heads: A comparison of anatomic fit. J. Shoulder Elbow Surg. 2018, 27, S50–S57. [Google Scholar] [CrossRef]
- Habermeyer, P.; Magosch, P.; Weiss, C.; Hawi, N.; Lichtenberg, S.; Tauber, M.; Ipach, B. Classification of humeral head pathomorphology in primary osteoarthritis: A radiographic and in vivo photographic analysis. J. Shoulder Elb. Surg. 2017, 26, 2193–2199. [Google Scholar] [CrossRef]
- Iannotti, J.P.; Gabriel, J.P.; Schneck, S.L.; Evans, B.G.; Misra, S. The normal glenohumeral relationships. An anatomical study of one hundred and forty shoulders. J. Bone Jt. Surg. Am. 1992, 74, 491–500. [Google Scholar] [CrossRef]
- Harrold, F.; Wigderowitz, C. Humeral head arthroplasty and its ability to restore original humeral head geometry. J. Shoulder Elb. Surg. 2013, 22, 115–121. [Google Scholar] [CrossRef]
- Jun, B.J.; Iannotti, J.P.; McGarry, M.H.; Yoo, J.C.; Quigley, R.J.; Lee, T.Q. The effects of prosthetic humeral head shape on glenohumeral joint kinematics: A comparison of non-spherical and spherical prosthetic heads to the native humeral head. J. Shoulder Elb. Surg. 2013, 22, 1423–1432. [Google Scholar] [CrossRef]
- Jun, B.J.; Lee, T.Q.; McGarry, M.H.; Quigley, R.J.; Shin, S.J.; Iannotti, J.P. The effects of prosthetic humeral head shape on glenohumeral joint kinematics during humeral axial rotation in total shoulder arthroplasty. J. Shoulder Elb. Surg. 2016, 25, 1084–1093. [Google Scholar] [CrossRef]
- Muench, L.N.; Otto, A.; Kia, C.; Obopilwe, E.; Cote, M.P.; Imhoff, A.B.; Beitzel, K.; Mazzocca, A.D.; Mehl, J. Rotational range of motion of elliptical and spherical heads in shoulder arthroplasty: A dynamic biomechanical evaluation. Arch. Orthop. Trauma Surg. 2020, 142, 67–76. [Google Scholar] [CrossRef]
- Spangenberg, G.W.; Faber, K.J.; Langohr, G.D.G.; Reeves, J.M. The sizing and suitability of nonspherical ellipsoid humeral heads for total shoulder arthroplasty. J. Shoulder Elb. Surg. 2023, 32, 232–239. [Google Scholar] [CrossRef]
- Budge, M.D.; Orvets, N. Stemless total shoulder arthroplasty using a novel multiplanar osteotomy and elliptical humeral head results in both improved early range of motion and radiographic center of rotation compared with standard total shoulder arthroplasty. J. Shoulder Elb. Surg. 2023, 32, 318–325. [Google Scholar] [CrossRef] [PubMed]
- Cavinatto, L.; Khatib, O.; Martusiewicz, A.; Koueiter, D.M.; Wiater, B.P.; Wiater, J.M. Radiographic evaluation of humeral head reconstruction with stemmed and stemless spherical implants compared with stemless elliptical head implants. JSES Int. 2021, 5, 889–893. [Google Scholar] [CrossRef] [PubMed]
- Shapiro, T.A.; McGarry, M.H.; Gupta, R.; Lee, Y.S.; Lee, T.Q. Biomechanical effects of glenoid retroversion in total shoulder arthroplasty. J. Shoulder Elb. Surg. 2007, 16, S90–S95. [Google Scholar] [CrossRef]
- Imhoff, F.B.; Camenzind, R.S.; Obopilwe, E.; Cote, M.P.; Mehl, J.; Beitzel, K.; Imhoff, A.B.; Mazzocca, A.D.; Arciero, R.A.; Dyrna, F.G.E. Glenoid retroversion is an important factor for humeral head centration and the biomechanics of posterior shoulder stability. Knee Surg. Sports Traumatol. Arthrosc. 2019, 27, 3952–3961. [Google Scholar] [CrossRef]
- Mehl, J.; Otto, A.; Imhoff, F.B.; Murphy, M.; Dyrna, F.; Obopilwe, E.; Cote, M.; Ladermann, A.; Collin, P.; Beitzel, K.; et al. Dynamic Anterior Shoulder Stabilization with the Long Head of the Biceps Tendon: A Biomechanical Study. Am. J. Sports Med. 2019, 47, 1441–1450. [Google Scholar] [CrossRef] [PubMed]
- Muench, L.N.; Murphey, M.; Oei, B.; Kia, C.; Obopilwe, E.; Cote, M.P.; Mazzocca, A.D.; Berthold, D.P. Elliptical and spherical heads show similar obligate glenohumeral translation during axial rotation in total shoulder arthroplasty. BMC Musculoskelet. Disord. 2023, 24, 171. [Google Scholar] [CrossRef] [PubMed]
- Arciero, R.A.; Parrino, A.; Bernhardson, A.S.; Diaz-Doran, V.; Obopilwe, E.; Cote, M.P.; Golijanin, P.; Mazzocca, A.D.; Provencher, M.T. The effect of a combined glenoid and Hill-Sachs defect on glenohumeral stability: A biomechanical cadaveric study using 3-dimensional modeling of 142 patients. Am. J. Sports Med. 2015, 43, 1422–1429. [Google Scholar] [CrossRef] [PubMed]
- Mihata, T.; Lee, Y.; McGarry, M.H.; Abe, M.; Lee, T.Q. Excessive humeral external rotation results in increased shoulder laxity. Am. J. Sports Med. 2004, 32, 1278–1285. [Google Scholar] [CrossRef] [PubMed]
- Pauzenberger, L.; Dyrna, F.; Obopilwe, E.; Heuberer, P.R.; Arciero, R.A.; Anderl, W.; Mazzocca, A.D. Biomechanical Evaluation of Glenoid Reconstruction with an Implant-Free J-Bone Graft for Anterior Glenoid Bone Loss. Am. J. Sports Med. 2017, 45, 2849–2857. [Google Scholar] [CrossRef] [PubMed]
- Schneider, D.J.; Tibone, J.E.; McGarry, M.H.; Grossman, M.G.; Veneziani, S.; Lee, T.Q. Biomechanical evaluation after five and ten millimeter anterior glenohumeral capsulorrhaphy using a novel shoulder model of increased laxity. J. Shoulder Elb. Surg. 2005, 14, 318–323. [Google Scholar] [CrossRef]
- Selecky, M.T.; Tibone, J.E.; Yang, B.Y.; McMahon, P.J.; Lee, T.Q. Glenohumeral joint translation after arthroscopic thermal capsuloplasty of the posterior capsule. J. Shoulder Elb. Surg. 2003, 12, 242–246. [Google Scholar] [CrossRef]
- Veeger, H.E.; Van der Helm, F.C.; Van der Woude, L.H.; Pronk, G.M.; Rozendal, R.H. Inertia and muscle contraction parameters for musculoskeletal modelling of the shoulder mechanism. J. Biomech. 1991, 24, 615–629. [Google Scholar] [CrossRef]
- Barrett Payne, W.; Kleiner, M.T.; McGarry, M.H.; Tibone, J.E.; Lee, T.Q. Biomechanical comparison of the Latarjet procedure with and without a coracoid bone block. Knee Surg. Sports Traumatol. Arthrosc. 2016, 24, 513–520. [Google Scholar] [CrossRef]
- Habermeyer, P.; Lichtenberg, S.; Tauber, M.; Magosch, P. Midterm results of stemless shoulder arthroplasty: A prospective study. J. Shoulder Elb. Surg. 2015, 24, 1463–1472. [Google Scholar] [CrossRef]
- Lin, T.; Javidan, P.; McGarry, M.H.; Gonzalez-Lomas, G.; Limpisvasti, O.; Lee, T.Q. Glenohumeral contact pressure in a simulated active compression test using cadaveric shoulders. J. Shoulder Elb. Surg. 2013, 22, 365–374. [Google Scholar] [CrossRef]
- Muench, L.N.; Berthold, D.P.; Otto, A.; Dyrna, F.; Bell, R.; Obopilwe, E.; Cote, M.P.; Imhoff, A.B.; Mazzocca, A.D.; Beitzel, K. Increased Glenohumeral Joint Loads Due to a Supraspinatus Tear Can Be Reversed with Rotator Cuff Repair: A Biomechanical Investigation. Arthroscopy 2021, 38, 1422–1432. [Google Scholar] [CrossRef] [PubMed]
- Wilharm, A.; Hurschler, C.; Dermitas, T.; Bohnsack, M. Use of Tekscan K-scan sensors for retropatellar pressure measurement avoiding errors during implantation and the effects of shear forces on the measurement precision. Biomed. Res. Int. 2013, 2013, 829171. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.M.; Chacon, A.C.; Andrews, S.H.; Roush, E.P.; Cho, E.; Conaway, W.K.; Kunselman, A.R.; Lewis, G.S. Biomechanical benefits of anterior offsetting of humeral head component in posteriorly unstable total shoulder arthroplasty: A cadaveric study. J. Orthop. Res. 2016, 34, 666–674. [Google Scholar] [CrossRef] [PubMed]
- Hertel, R.; Knothe, U.; Ballmer, F.T. Geometry of the proximal humerus and implications for prosthetic design. J. Shoulder Elb. Surg. 2002, 11, 331–338. [Google Scholar] [CrossRef]
- Harryman, D.T.; Sidles, J.A.; Harris, S.L.; Lippitt, S.B.; Matsen, F.A. The effect of articular conformity and the size of the humeral head component on laxity and motion after glenohumeral arthroplasty. A study in cadavera. J. Bone Jt. Surg. Am. 1995, 77, 555–563. [Google Scholar] [CrossRef] [PubMed]
- Muench, L.N.; Kia, C.; Murphey, M.; Obopilwe, E.; Cote, M.P.; Imhoff, A.B.; Mazzocca, A.D.; Berthold, D.P. Elliptical heads result in increased glenohumeral translation along with micro-motion of the glenoid component during axial rotation in total shoulder arthroplasty. Arch. Orthop. Trauma Surg. 2021, 143, 177–187. [Google Scholar] [CrossRef] [PubMed]

| Neutral Rotation | External Rotation | Internal Rotation | |||
|---|---|---|---|---|---|
| 0° | Native | mean ± SD | 132.0 ± 18.2 | 271.3 ± 321.7 | 133.1 ± 66.4 |
| median | 128.0 | 150.0 | 115.0 | ||
| IQR | 6.0 | 177.0 | 80.0 | ||
| Elliptical | mean ± SD | 187.8 ± 57.1 | 227.2 ± 160.8 | 211.2 ± 67.5 | |
| median | 192.0 | 182.5 | 189.5 | ||
| IQR | 93.0 | 75.0 | 26.0 | ||
| Sphere | mean ± SD | 220.3 ± 128.3 | 339.2 ± 228.0 | 218.3 ± 78.2 | |
| median | 193.5 | 297.5 | 205.5 | ||
| IQR | 192.0 | 192.0 | 61.0 | ||
| 15° | Native | mean ± SD | 123.7 ± 33.0 | 236.0 ± 182.0 | 118.0 ± 66.3 |
| median | 129.5 | 172.5 | 101.5 | ||
| IQR | 22.0 | 299.0 | 44.0 | ||
| Elliptical | mean ± SD | 174.3 ± 166.8 | 194.0 ± 114.1 | 206.0 ± 56.0 | |
| median | 183.0 | 159.0 | 193.0 | ||
| IQR | 51.0 | 63.0 | 88.0 | ||
| Sphere | mean ± SD | 178.4 ± 56.8 | 289.7 ± 185.7 | 153.3 ± 51.9 | |
| median | 184.0 | 196.0 | 156.0 | ||
| IQR | 49.0 | 390.0 | 119.0 | ||
| 30° | Native | mean ± SD | 179.6 ± 115.5 | 225.3 ± 114.3 | 162.4 ± 94.3 |
| median | 136.0 | 202.0 | 140.0 | ||
| IQR | 178.0 | 240.0 | 179.0 | ||
| Elliptical | mean ± SD | 259.4 ± 217.5 | 148.4 ± 44.6 | 209.9 ± 72.6 | |
| median | 176.0 | 159.0 | 242.0 | ||
| IQR | 20.0 | 71.0 | 148.0 | ||
| Sphere | mean ± SD | 253.3 ± 215.0 | 259.9 ± 207.5 | 262.9 ± 150.4 | |
| median | 177.0 | 279.0 | 199.0 | ||
| IQR | 127.0 | 267.0 | 170.0 | ||
| 45° | Native | mean ± SD | 145.1 ± 46.3 | 189.0 ± 115.4 | 124.0 ± 37.6 |
| median | 126.0 | 156.0 | 123.0 | ||
| IQR | 101.0 | 185.0 | 54.0 | ||
| Elliptical | mean ± SD | 292.3 ± 139.5 | 191.9 ± 94.5 | 240.9 ± 128.1 | |
| median | 250.0 | 204.0 | 241.0 | ||
| IQR | 76.0 | 159.0 | 266.0 | ||
| Sphere | mean ± SD | 242.1 ± 158.3 | 297.7 ± 281.8 | 218.3 ± 157.5 | |
| median | 186.0 | 161.0 | 142.0 | ||
| IQR | 280.0 | 304.0 | 136.0 | ||
| 60° | Native | mean ± SD | 112.3 ± 15.8 | 177.6 ± 88.9 | 149.0 ± 50.6 |
| median | 113.0 | 176.0 | 131.0 | ||
| IQR | 18.0 | 71.0 | 104.0 | ||
| Elliptical | mean ± SD | 224.0 ± 124.5 | 254.9 ± 140.7 | 174.9 ± 81.8 | |
| median | 224.0 | 266.0 | 155.0 | ||
| IQR | 161.0 | 253.0 | 160.0 | ||
| Sphere | mean ± SD | 253.9 ± 231.8 | 244.3 ± 124.5 | 262.4 ± 177.4 | |
| median | 155.0 | 285.0 | 199.0 | ||
| IQR | 242.0 | 206.0 | 275.0 |
| Neutral Rotation | External Rotation | Internal Rotation | |||
|---|---|---|---|---|---|
| 0° | Native | mean ± SD | 383.2 ± 60.5 | 1043.0 ± 1258.9 | 520.1 ± 235.0 |
| median | 360.0 | 537.0 | 559.0 | ||
| IQR | 108.0 | 962.0 | 478.0 | ||
| Elliptical | mean ± SD | 1136.5 ± 1146.7 | 682.3 ± 343.7 | 1177.8 ± 663.0 | |
| median | 831.5 | 606.0 | 1003.5 | ||
| IQR | 729.0 | 214.0 | 974.0 | ||
| Sphere | mean ± SD | 1335.3 ± 1360.9 | 1394.3 ± 728.1 | 983.2 ± 554.8 | |
| median | 837.0 | 1225.5 | 778.5 | ||
| IQR | 1805.0 | 776.0 | 737.0 | ||
| 15° | Native | mean ± SD | 386.3 ± 139.0 | 937.7 ± 1148.9 | 416.7 ± 200.9 |
| median | 367.0 | 515.0 | 372.5 | ||
| IQR | 68.0 | 891.0 | 197.0 | ||
| Elliptical | mean ± SD | 1179.1 ± 480.4 | 586.9 ± 181.8 | 1207.7 ± 690.4 | |
| median | 1108.0 | 559.0 | 1123.0 | ||
| IQR | 947.0 | 329.0 | 1162.0 | ||
| Sphere | mean ± SD | 1126.9 ± 739.3 | 1481.7 ± 1253.2 | 857.0 ± 626.5 | |
| median | 1149.0 | 1050.0 | 748.0 | ||
| IQR | 892.0 | 2429.0 | 1053.0 | ||
| 30° | Native | mean ± SD | 602.6 ± 385.7 | 794.9 ± 657.3 | 581.4 ± 415.1 |
| median | 515.0 | 577.0 | 411.0 | ||
| IQR | 683.0 | 995.0 | 538.0 | ||
| Elliptical | mean ± SD | 1170.7 ± 282.5 | 593.7 ± 308.1 | 1140.4 ± 716.4 | |
| median | 1066.0 | 598.0 | 892.0 | ||
| IQR | 311.0 | 471.0 | 1349.0 | ||
| Sphere | mean ± SD | 1175.9 ± 676.3 | 1491.4 ± 1159.1 | 1275.4 ± 854.7 | |
| median | 995.0 | 1493.0 | 974.0 | ||
| IQR | 1388.0 | 2139.0 | 657.0 | ||
| 45° | Native | mean ± SD | 481.4 ± 177.2 | 682.0 ± 556.3 | 425.3 ± 143.8 |
| median | 400.0 | 499.0 | 427.0 | ||
| IQR | 364.0 | 1016.0 | 273.0 | ||
| Elliptical | mean ± SD | 1318.9 ± 428.6 | 803.3 ± 733.9 | 1072.7 ± 886.1 | |
| median | 1224.0 | 739.0 | 984.0 | ||
| IQR | 604.0 | 578.0 | 1350.0 | ||
| Sphere | mean ± SD | 1366.4 ± 894.5 | 1600.1 ± 1297.7 | 1153.1 ± 906.1 | |
| median | 1078.0 | 1042.0 | 644.0 | ||
| IQR | 1047.0 | 2135.0 | 1800.0 | ||
| 60° | Native | mean ± SD | 356.3 ± 115.4 | 582.3 ± 299.7 | 572.7 ± 188.9 |
| median | 308.0 | 439.0 | 640.0 | ||
| IQR | 214.0 | 571.0 | 317.0 | ||
| Elliptical | mean ± SD | 1119.1 ± 896.5 | 1322.0 ± 1071.3 | 801.1 ± 549.2 | |
| median | 688.0 | 888.0 | 743.0 | ||
| IQR | 1136.0 | 2202.0 | 1259.0 | ||
| Sphere | mean ± SD | 1104.6 ± 1049.2 | 1088.1 ± 745.9 | 1213.4 ± 784.1 | |
| median | 733.0 | 1082.0 | 1375.0 | ||
| IQR | 2027.0 | 1129.0 | 1519.0 |
| Neutral Rotation | External Rotation | Internal Rotation | |||
|---|---|---|---|---|---|
| 0° | Native | mean ± SD | 328.6 ± 119.8 | 203.0 ± 67.3 | 270.7 ± 97.5 |
| median | 312.0 | 203.0 | 312.0 | ||
| IQR | 207.0 | 73.0 | 181.0 | ||
| Elliptical | mean ± SD | 203.2 ± 52.9 | 110.7 ± 63.6 | 158.0 ± 83.7 | |
| median | 198.0 | 88.5 | 143.5 | ||
| IQR | 62.0 | 55.0 | 123.0 | ||
| Sphere | mean ± SD | 177.2 ± 50.2 | 102.2 ± 40.9 | 143.2 ± 79.0 | |
| median | 183.5 | 94.0 | 128.5 | ||
| IQR | 73.0 | 66.0 | 123.0 | ||
| 15° | Native | mean ± SD | 312.0 ± 78.3 | 196.5 ± 97.1 | 242.8 ± 76.3 |
| median | 301.0 | 197.5 | 249.5 | ||
| IQR | 95.0 | 116.0 | 83.0 | ||
| Elliptical | mean ± SD | 155.0 ± 56.7 | 93.6 ± 46.1 | 117.1 ± 64.5 | |
| median | 149.0 | 87.0 | 98.0 | ||
| IQR | 65.0 | 69.0 | 118.0 | ||
| Sphere | mean ± SD | 202.7 ± 56.4 | 107.3 ± 53.4 | 122.3 ± 39.8 | |
| median | 200.0 | 116.0 | 98.0 | ||
| IQR | 62.0 | 109.0 | 83.0 | ||
| 30° | Native | mean ± SD | 257.3 ± 98.2 | 182.9 ± 114.4 | 226.6 ± 77.3 |
| median | 258.0 | 196.0 | 261.0 | ||
| IQR | 84.0 | 221.0 | 156.0 | ||
| Elliptical | mean ± SD | 153.9 ± 64.3 | 114.9 ± 65.7 | 117.9 ± 39.2 | |
| median | 178.0 | 92.0 | 124.0 | ||
| IQR | 101.0 | 134.0 | 47.0 | ||
| Sphere | mean ± SD | 166.0 ± 65.7 | 105.7 ± 63.3 | 115.4 ± 57.1 | |
| median | 178.0 | 94.0 | 116.0 | ||
| IQR | 83.0 | 109.0 | 84.0 | ||
| 45° | Native | mean ± SD | 361.9 ± 164.4 | 260.3 ± 140.4 | 293.4 ± 106.9 |
| median | 305.0 | 265.0 | 261.0 | ||
| IQR | 316.0 | 291.0 | 123.0 | ||
| Elliptical | mean ± SD | 131.4 ± 61.2 | 96.9 ± 51.8 | 109.0 ± 52.5 | |
| median | 120.0 | 80.0 | 112.0 | ||
| IQR | 62.0 | 76.0 | 43.0 | ||
| Sphere | mean ± SD | 146.6 ± 49.5 | 105.3 ± 70.4 | 125.1 ± 64.8 | |
| median | 149.0 | 105.0 | 112.0 | ||
| IQR | 29.0 | 69.0 | 105.0 | ||
| 60° | Native | mean ± SD | 397.4 ± 108.4 | 290.6 ± 111.7 | 357.1 ± 128.4 |
| median | 363.0 | 299.0 | 368.0 | ||
| IQR | 58.0 | 254.0 | 156.0 | ||
| Elliptical | mean ± SD | 123.3 ± 56.7 | 118.0 ± 61.9 | 114.7 ± 61.1 | |
| median | 112.0 | 120.0 | 102.0 | ||
| IQR | 44.0 | 77.0 | 36.0 | ||
| Sphere | mean ± SD | 144.6 ± 80.7 | 98.4 ± 75.9 | 103.6 ± 63.5 | |
| median | 152.0 | 58.0 | 102.0 | ||
| IQR | 171.0 | 123.0 | 80.0 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Muench, L.N.; Slater, M.; Archambault, S.; Berthold, D.P.; Rupp, M.-C.; Obopilwe, E.; Cote, M.P.; Mazzocca, A.D. Contact Mechanics of Elliptical and Spherical Head Implants during Axial Rotation in Anatomic Total Shoulder Arthroplasty: A Biomechanical Comparison. J. Clin. Med. 2023, 12, 4918. https://doi.org/10.3390/jcm12154918
Muench LN, Slater M, Archambault S, Berthold DP, Rupp M-C, Obopilwe E, Cote MP, Mazzocca AD. Contact Mechanics of Elliptical and Spherical Head Implants during Axial Rotation in Anatomic Total Shoulder Arthroplasty: A Biomechanical Comparison. Journal of Clinical Medicine. 2023; 12(15):4918. https://doi.org/10.3390/jcm12154918
Chicago/Turabian StyleMuench, Lukas N., Maria Slater, Simon Archambault, Daniel P. Berthold, Marco-Christopher Rupp, Elifho Obopilwe, Mark P. Cote, and Augustus D. Mazzocca. 2023. "Contact Mechanics of Elliptical and Spherical Head Implants during Axial Rotation in Anatomic Total Shoulder Arthroplasty: A Biomechanical Comparison" Journal of Clinical Medicine 12, no. 15: 4918. https://doi.org/10.3390/jcm12154918





