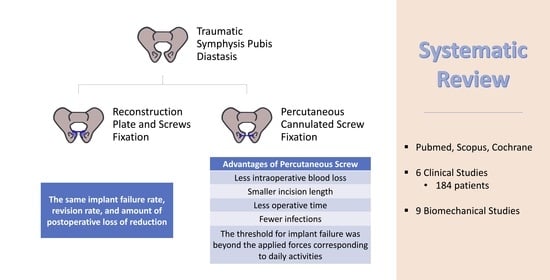
Percutaneous Fixation for Traumatic Symphysis Pubis Disruption—Are the Results Superior Compared to Open Techniques? A Systematic Review and Meta-Analysis of Clinical and Biomechanical Outcomes
Abstract
:1. Introduction
2. Material and Methods
2.1. Search Strategy and Eligibility Criteria
- The study reported clinical outcomes after the application of PCSF either alone or in comparison with RPSF for traumatic SPD in patients 16 years of age or older.
- The study reported biomechanical or anatomical properties of PCSF in cadaveric or software simulation studies.
- The report was a conference abstract.
- The study did not present clinical or biomechanical data, such as reviews and letters to the editor.
- The study evaluated nontraumatic SPD.
- The study was not written in the English language.
2.2. Data Extraction
2.3. Quality Assessment
2.4. Statistical Analysis
3. Results
3.1. Characteristics of Clinical Studies
3.2. Percutaneous Fixation Technique
3.3. Characteristics of Biomechanical and Anatomical Studies
3.4. Quality Assessment
3.5. Primary Outcomes
3.6. Secondary Outcomes
3.7. Biomechanical Outcomes
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Pohlemann, T.; Bosch, U.; Gänsslen, A.; Tscherne, H. The Hannover Experience in Management of Pelvic Fractures. Clin. Orthop. Relat. Res. 1994, 305, 69–80. [Google Scholar] [CrossRef]
- Yu, K.-H.; Hong, J.-J.; Guo, X.-S.; Zhou, D.-S. Comparison of Reconstruction Plate Screw Fixation and Percutaneous Cannulated Screw Fixation in Treatment of Tile B1 Type Pubic Symphysis Diastasis: A Finite Element Analysis and 10-Year Clinical Experience. J. Orthop. Surg. Res. 2015, 10, 151. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mu, W.; Wang, H.; Zhou, D.; Yu, L.; Jia, T.; Li, L. Computer Navigated Percutaneous Screw Fixation for Traumatic Pubic Symphysis Diastasis of Unstable Pelvic Ring Injuries. Chin. Med. J. 2009, 122, 1699–1703. [Google Scholar] [PubMed]
- Phieffer, L.S.; Lundberg, W.P.; Templeman, D.C. Instability of the Posterior Pelvic Ring Associated with Disruption of the Pubic Symphysis. Orthop. Clin. N. Am. 2004, 35, 445–449. [Google Scholar] [CrossRef] [PubMed]
- Putnis, S.E.; Pearce, R.; Wali, U.J.; Bircher, M.D.; Rickman, M.S. Open Reduction and Internal Fixation of a Traumatic Diastasis of the Pubic Symphysis: One-Year Radiological and Functional Outcomes. J. Bone Joint Surg. Br. 2011, 93, 78–84. [Google Scholar] [CrossRef]
- Cole, J.D.; Bolhofner, B.R. Acetabular Fracture Fixation via a Modified Stoppa Limited Intrapelvic Approach. Description of Operative Technique and Preliminary Treatment Results. Clin. Orthop. Relat. Res. 1994, 305, 112–123. [Google Scholar] [CrossRef]
- Feng, Y.; Hong, J.; Guo, X.; Lin, C.; Ling, W.; Zhang, L.; Wang, G. Percutaneous Fixation of Traumatic Pubic Symphysis Diastasis Using a TightRope and External Fixator versus Using a Cannulated Screw. J. Orthop. Surg. Res. 2016, 11, 62. [Google Scholar] [CrossRef] [Green Version]
- Grewal, I.S.; Starr, A.J. What’s New in Percutaneous Pelvis Fracture Surgery? Orthop. Clin. N. Am. 2020, 51, 317–324. [Google Scholar] [CrossRef]
- Purcell, K.F.; Bergin, P.F.; Spitler, C.A.; Graves, M.L.; Russell, G.V. Management of Pelvic and Acetabular Fractures in the Obese Patient. Orthop. Clin. N. Am. 2018, 49, 317–324. [Google Scholar] [CrossRef]
- Liu, Z.; Wang, K.; Zhang, K.; Zhou, J.; Zhang, Y. Minimally Invasive Surgery (MIS) of Anterior Ring Fracture Combined with Pubic Symphysis Separation. Med. Sci. Monit. 2014, 20, 1913–1917. [Google Scholar] [CrossRef]
- Kabir, K.; Lingohr, P.; Jaenisch, M.; Hackenberg, R.K.; Sommer, N.; Ossendorff, R.; Welle, K.; Gathen, M. Total Endoscopic Anterior Pelvic Approach (TAPA)-A New Approach to the Internal Fixation of the Symphysis. Injury 2022, 53, 802–808. [Google Scholar] [CrossRef]
- Hartel, M.J.; Althoff, G.; Wolter, S.; Ondruschka, B.; Dietz, E.; Frosch, K.-H.K.; Thiesen, D.M. Full Endoscopic Anterior Intrapelvic Plate Osteosynthesis: A Cadaveric Feasibility Study. Arch. Orthop. Trauma Surg. 2022, 143, 365–371. [Google Scholar] [CrossRef]
- Pierce, T.P.; Issa, K.; Callaghan, J.J.; Wright, C. Traumatic Diastasis of the Pubic Symphysis-A Review of Fixation Method Outcomes. Surg. Technol. Int. 2016, 29, 265–269. [Google Scholar]
- Cavalcanti Kußmaul, A.; Schwaabe, F.; Kistler, M.; Gennen, C.; Andreß, S.; Becker, C.A.; Böcker, W.; Greiner, A. Novel Minimally Invasive Tape Suture Osteosynthesis for Instabilities of the Pubic Symphysis: A Biomechanical Study. Arch. Orthop. Trauma Surg. 2021, 142, 2235–2243. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. BMJ 2009, 339, b2535. [Google Scholar] [CrossRef] [Green Version]
- Moga, C.; Guo, B.; Schopflocher, D.; Harstall, C. Development of a Quality Appraisal Tool for Case Series Studies Using a Modified Delphi Technique; Institute of Health Economics: Edmonton, AB, Canada, 2012. [Google Scholar]
- Coleman, B.D.; Khan, K.M.; Maffulli, N.; Cook, J.L.; Wark, J.D. Studies of Surgical Outcome after Patellar Tendinopathy: Clinical Significance of Methodological Deficiencies and Guidelines for Future Studies. Scand. J. Med. Sci. Sports 2000, 10, 2–11. [Google Scholar] [CrossRef]
- Dewan, V.; Webb, M.S.L.; Prakash, D.; Malik, A.; Gella, S.; Kipps, C. When Does the Patella Dislocate? A Systematic Review of Biomechanical & Kinematic Studies. J. Orthop. 2020, 20, 70–77. [Google Scholar] [CrossRef]
- Critical Appraisal Skills Programme CASP Cohort Study Checklist. Available online: http://docs.wixstatic.com/ugd/dded87_5ad0ece77a3f4fc9bcd3665a7d1fa91f.pdf (accessed on 14 April 2021).
- Wilke, J.; Krause, F.; Niederer, D.; Engeroff, T.; Nürnberger, F.; Vogt, L.; Banzer, W. Appraising the Methodological Quality of Cadaveric Studies: Validation of the QUACS Scale. J. Anat. 2015, 226, 440–446. [Google Scholar] [CrossRef]
- Higgins, J.P.T.; Thompson, S.G.; Deeks, J.J.; Altman, D.G. Measuring Inconsistency in Meta-Analyses. BMJ 2003, 327, 557–560. [Google Scholar] [CrossRef] [Green Version]
- Chen, L.; Zhang, G.; Song, D.; Guo, X.; Yuan, W. A Comparison of Percutaneous Reduction and Screw Fixation versus Open Reduction and Plate Fixation of Traumatic Symphysis Pubis Diastasis. Arch. Orthop. Trauma Surg. 2012, 132, 265–270. [Google Scholar] [CrossRef]
- Eakin, J.L.; Grewal, I.S.; Fene, E.S.; Sathy, A.K.; Starr, A.J. Percutaneous Screw Fixation of Pubic Symphysis Disruption: A Preliminary Report. J. Clin. Orthop. Trauma 2022, 26, 101806. [Google Scholar] [CrossRef] [PubMed]
- Chan, A.C.K.; Chui, K.H.; Lee, K.B.; Li, W. Three-Dimensional Navigation-Guided Percutaneous Trans-Symphyseal Screw for Mechanically Unstable Pubic Symphysis Diastasis. J. Orthop. Trauma Rehabil. 2022, 30, 1–11. [Google Scholar] [CrossRef]
- Cano-Luis, P.; Giráldez-Sanchez, M.A.; Martínez-Reina, J.; Serrano-Escalante, F.J.; Galleguillos-Rioboo, C.; Lázaro-Gonzálvez, A.; García-Rodríguez, J.; Navarro, A. Biomechanical Analysis of a New Minimally Invasive System for Osteosynthesis of Pubis Symphysis Disruption. Injury 2012, 43, 20–27. [Google Scholar] [CrossRef] [PubMed]
- Gonzálvez, Á.L.; Reina, J.M.; Luis, P.C.; Baquero, J.J.; Fernández, J.S.; Sánchez, M.Á.G.; Lázaro Gonzálvez, Á.; Martínez Reina, J.; Cano Luis, P.; Jiménez Baquero, J.; et al. Is Cannulated-Screw Fixation an Alternative to Plate Osteosynthesis in Open Book Fractures? A Biomechanical Analysis. Injury 2016, 47, S72–S77. [Google Scholar] [CrossRef] [PubMed]
- Sun, G.; Yin, C.; Liu, Z.; Wang, L.; Mu, W. Three-Dimensionally-Navigated Cross-Cannulated Screw Fixation for Traumatic Pubic Symphysis Diastasis: An Anatomical Study. Acta Orthop. Traumatol. Turc. 2016, 50, 214–221. [Google Scholar] [CrossRef]
- Xu, P.; Wang, H.; Liu, Z.; Mu, W.; Xu, S.; Wang, L.; Chen, C.; Cavanaugh, J.M. An Evaluation of Three-Dimensional Image-Guided Technologies in Percutaneous Pelvic and Acetabular Lag Screw Placement. J. Surg. Res. 2013, 185, 338–346. [Google Scholar] [CrossRef]
- Yao, F.; He, Y.; Qian, H.; Zhou, D.; Li, Q. Comparison of Biomechanical Characteristics and Pelvic Ring Stability Using Different Fixation Methods to Treat Pubic Symphysis Diastasis a Finite Element Study. Medicine 2015, 94, e2207. [Google Scholar] [CrossRef]
- Yu, K.; Hong, J.; Sun, Y.; Shi, C.; Guo, X.; Zhou, D. Anatomical Measurement and Finite Element Study on Screw Channel Parameter in Percutaneous Fixation of Canulated Screw for Symphyseolysis. Cell Biochem. Biophys. 2015, 71, 1243–1248. [Google Scholar] [CrossRef]
- Liu, L.; Fan, S.; Zeng, D.; Song, H.; Zeng, L.; Wen, X.; Jin, D. Identification of Safe Channels for Screws in the Anterior Pelvic Ring Fixation System. J. Orthop. Surg. Res. 2022, 17, 312. [Google Scholar] [CrossRef]
- O’Neill, D.E.; Bradley, H.R.; Hull, B.; Pierce, W.; Grewal, I.S.; Starr, A.J.; Sathy, A.; Neill, D.E.O.; Bradley, H.R.; Hull, B.; et al. Percutaneous Screw Fixation of the Pubic Symphysis versus Plate Osteosynthesis: A Biomechanical Study. OTA Int. 2022, 5, e215. [Google Scholar] [CrossRef]
- Majeed, S.A. Grading the Outcome of Pelvic Fractures. J. Bone Joint Surg. Br. 1989, 71, 304–306. [Google Scholar] [CrossRef] [Green Version]
- Becker, I.; Woodley, S.J.; Stringer, M.D. The Adult Human Pubic Symphysis: A Systematic Review. J. Anat. 2010, 217, 475–487. [Google Scholar] [CrossRef]
- Sagi, H.C.; Papp, S. Comparative Radiographic and Clinical Outcome of Two-Hole and Multi-Hole Symphyseal Plating. J. Orthop. Trauma 2008, 22, 373–378. [Google Scholar] [CrossRef]
- Virkus, W.V.; Goldberg, S.H.; Lorenz, E.P. A Comparison of Compressive Force Generation by Plating and Intramedullary Nailing Techniques in a Transverse Diaphyseal Humerus Fracture Model. J. Trauma 2008, 65, 103–108. [Google Scholar] [CrossRef]


| Study | Technique | N | Mean Age (yr) | Males/Females | Mean Follow-Up (mo) |
|---|---|---|---|---|---|
| Chan et al. [24], 2022 | Single or dual 6.5 mm PCSF | 13 | 57.9 (24–95) | 8/7 | At least 6 |
| Chen et al. [22], 2012 |
| 41 | 32 ± 9 | 29/12 | 21 (18–26) |
| 43 | 26 ± 11 | 33/9 | ||
| Eakin et al. [23], 2022 | Single or dual 5.5, 6.5, or 7.3 mm PCSF | 12 | 44 (16–76) | 10/2 | 15 (10.7–27.7) |
| Feng et al. [7], 2016 |
| 16 | 33.2 ± 5.8 | 11/5 | 15 (12–20) |
| 10 | 32.5 ± 6.2 | 7/3 | ||
| Mu et al. [3], 2016 | Single or dual crossed 7.3 mm PCSF, computer navigation | 8 | 40.9 ± 17.9 | 6/2 | 16.1 ± 2.5 |
| Yu et al. [2], 2015 |
| 24 | 33.4 ± 9.1 | 15/9 | 29.4 ± 8.8 |
| 27 | 34.8 ± 11.7 | 19/8 |
| Study | Fracture Simulation | Implants | Testing Method | Outcomes | Specimens | Results/Conclusions |
|---|---|---|---|---|---|---|
| Cano-Luis et al. [25], 2012 | Tile B1 | Dual 6.5 mm PCSF | Axial load 300N (dual-leg standing) | Displacement of pubic symphysis | 10 cadavers | PCSF biomechanically sufficient |
| Gonzálvez et al. [26], 2016 | Tile B1 |
| Axial load 300N (dual-leg standing) | Displacement of pubic symphysis | 9 cadavers | PCSF more stable than RPSF |
| Liu et al. [31], 2022 | Intact pelvis | Single 7.5 mm PCSF | Determination of the optimal insertion point and safe channels of screws | Screws diameter and length, distance between screw and anterior inferior iliac spine, coronal, sagittal, and horizontal plane angles |
| Screw length 47.0 ± 2.0 mm (M) and 39.8 ± 3.9 mm (F), diameter 7.1 ± 0.4 mm (M) and 6.1 ± 0.4 mm (F), distance between screw and AIIS 5.5 ± 0.5 mm (M) and 5.6 ± 0.7 mm (F), angle of coronal plane 55.9° ± 1.3° (M) and 50.7° ± 1.5° (F), angle of sagittal plane 26.7° ± 0.5° (M) and 24.1° ± 0.9° (F), and angle of horizontal plane 64.8° ± 0.6° (M) and 58.8° ± 0.8° (F). Safe screw insertion 5 mm above AIIS, and 10 mm outside the midline of the symphysis pubis. |
| O’Neill et al. [32], 2022 | Tile C1 |
| 7 mm vertical compressive displacement through the sacrum at a rate of 2 mm/s (single-leg standing) | Displacement and rotation in 3 dimensions at the sacroiliac joint and pubic symphysis, stiffness at maximum stroke distance |
| There was no significant difference in net displacement at both sacroiliac joint and pubic symphysis. There was significantly less rotation but more dis-placement in the screw group in the Z-axis. The screw group showed increased stiffness compared with the plate group. |
| Sun et al. [27], 2016 | Intact pelvis | Dual crossed 6.5 mm PCSF | Optimization of the secure trajectory of crossed screws using computer navigation | Trajectory, mean screw length, distance from surrounding major structures | 15 cadavers | Mean screw length 7.0 ± 4.2 and 7.1 ± 3.8 cm. Minimum distance between entry point and spermatic cord (fallopian arch in the female) was 9 mm. All screw corridors were intact. Computer navigation is reliable for PCSF. The trajectories of crossed screws are reliable and safe. |
| Xu et al. [28], 2016 | Intact pelvis |
| Determination of the accuracy of screw position, instrumentation time, and fluoroscopic time | Malposition rate, mean instrumentation time, mean fluoroscopic time | 6 cadavers | 3D fluoroscopic navigation showed a higher accuracy rate in positioning and a shorter instrumentation time. The fluoroscopic time was the shortest in 2D fluoroscopic navigation. |
| Yao et al. [29], 2015 | Tile B1 |
|
| Construct stiffness, incremental micromotion of anterior and posterior pelvic ring, incremental rotational angle of anterior pelvic ring | 3D finite element model analysis | Dual crossed PCSF and dual RPSF more stable methods |
| Yu et al. [2], 2015 | Tile B1 |
| Axial load 600 N (single-leg standing) | Whole stress, displacement of the bilateral pelvis, stress analysis of implants | 3D finite element model analysis | Both PCSF and RPSF biomechanically adequate |
| Yu et al. [30], 2015 | Intact pelvis | Single 6.5 mm PCSF | Optimization of the secure trajectory of screws | Distance from surrounding major structures, screw trajectory parameters |
| Distance between round ligament of the uterus and pubic tubercle was 4.408 ± 0.304 mm, and between spermatic cord and pubic tubercle was 5.196 ± 0.251 mm. Study on parameters of screw channel in PCSF can improve the accuracy of the screw placement. |
| Study | Objective Stated | Appropriate Study Design | Basic Information about Specimens | Conditions of Specimens | Study Protocol Clearly Stated | Exposure Accurately Measured | Outcome Accurately Measured | Results Presented Thoroughly | Stats Appropriate | Limitations Discussed | Clinical Implica-tions Discussed | Conclusions in Keeping with Results | Results Fit with Other Studies |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Cano-Luis et al. [25], 2012 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
| Gonzálvez et al. [26], 2016 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
| Liu et al. [31], 2022 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
| O’Neill et al. [32], 2022 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
| Sun et al. [27], 2016 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
| Xu et al. [28], 2016 | ✓ | ✓ | ✗ | ✗ | ✓ | ✓ | ✓ | ✓ | ✓ | ✗ | ✓ | ✓ | ✓ |
| Yao et al. [29], 2015 | ✓ | ✓ | N/A | N/A | ✓ | ✓ | ✓ | ✓ | ✗ | ✓ | ✓ | ✓ | ✓ |
| Yu et al. [2], 2015 (1) | ✓ | ✓ | N/A | N/A | ✓ | ✓ | ✓ | ✓ | ✗ * | ✓ | ✓ | ✓ | ✓ |
| Yu et al. [30], 2015 (2) | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✗ | ✓ | ✓ | ✓ | ✓ |
| Study | Technique | N | Implant Failure | Revision Surgery | Wound Infection |
|---|---|---|---|---|---|
| Chan et al. [24], 2022 | PCSF | 13 | - | - | - |
| Chen et al. [22], 2012 |
| 41 | 5 | 2 | 2 |
| 43 | 8 | 6 | 8 | |
| Eakin et al. [23], 2022 | PCSF | 12 | - | - | - |
| Feng et al. [7], 2016 |
| 16 | 3 | 1 | - |
| 10 | 1 | - | 1 | |
| Mu et al. [3], 2016 | PCSF | 8 | - | - | - |
| Yu et al. [2], 2015 |
| 24 | 2 | 1 | 1 |
| 27 | 2 | 1 | 2 |
| Study | Technique | N | Excellent (>85) | Good (70–84) | Fair (55–69) | Poor (<55) | p |
|---|---|---|---|---|---|---|---|
| Chan et al. [24], 2022 | PCSF | 12 | 2 | 2 | 4 | 4 | - |
| Chen et al. [22], 2012 | PCSF | 41 | 23 | 12 | 5 | 1 | 0.01 |
| RPSF | 43 | 10 | 24 | 5 | 3 | ||
| Feng et al. [7], 2016 | PCSF | 16 | 11 | 4 | 1 | - | n.s. |
| Tightrope and ex-fix | 10 | 7 | 3 | - | - | ||
| Yu et al. [2], 2015 | PCSF | 24 | 18 | 5 | 1 | - | n.s. |
| RPSF | 27 | 18 | 7 | 2 | - |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kitridis, D.; Tsikopoulos, K.; Givissis, P.; Chalidis, B. Percutaneous Fixation for Traumatic Symphysis Pubis Disruption—Are the Results Superior Compared to Open Techniques? A Systematic Review and Meta-Analysis of Clinical and Biomechanical Outcomes. J. Clin. Med. 2023, 12, 4988. https://doi.org/10.3390/jcm12154988
Kitridis D, Tsikopoulos K, Givissis P, Chalidis B. Percutaneous Fixation for Traumatic Symphysis Pubis Disruption—Are the Results Superior Compared to Open Techniques? A Systematic Review and Meta-Analysis of Clinical and Biomechanical Outcomes. Journal of Clinical Medicine. 2023; 12(15):4988. https://doi.org/10.3390/jcm12154988
Chicago/Turabian StyleKitridis, Dimitrios, Konstantinos Tsikopoulos, Panagiotis Givissis, and Byron Chalidis. 2023. "Percutaneous Fixation for Traumatic Symphysis Pubis Disruption—Are the Results Superior Compared to Open Techniques? A Systematic Review and Meta-Analysis of Clinical and Biomechanical Outcomes" Journal of Clinical Medicine 12, no. 15: 4988. https://doi.org/10.3390/jcm12154988