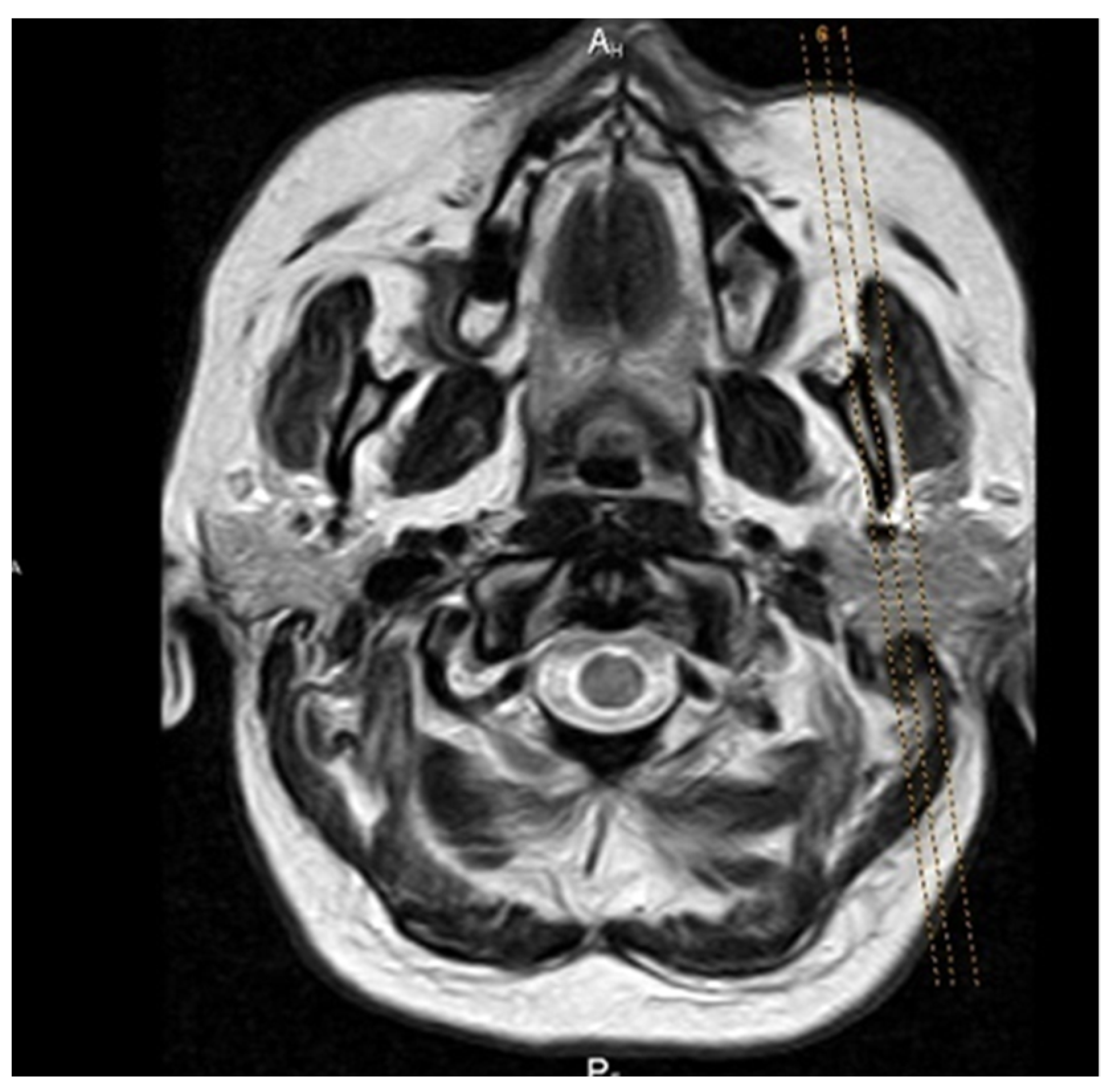
A New Mechanical Mouth Opener for Dynamic Magnetic Resonance Imaging of the Temporomandibular Joint
Abstract
:1. Introduction
2. Materials and Methods
2.1. Testing Protocol for Artifacts
- Signal-to-noise-ratio (SNR), which is further divided into three basic groups of artifacts (patient-dependent, hardware-dependent): edge artifacts, flow artifacts, and aliasing artifacts.
- Artifacts related to the property of matter to be magnetized in a magnetic field (primarily refers to ferromagnetic and paramagnetic materials that cause defects in the voxel grid of sections).
- The intensity of the signal depends on the device itself.
- Homogeneity of the signal, which depends on the homogeneity of the MR device field.
2.2. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Talmaceanu, D.; Lenghel, L.M.; Bolog, N.; Hedesiu, M.; Buduru, S.; Rotar, H.; Baciut, M.; Baciut, G. Imaging modalities for temporomandibular joint disorders: An update. Clujul Med. 2018, 91, 280–287. [Google Scholar] [CrossRef] [PubMed]
- Schimmel, M.; Aarab, G.; Baad-Hansen, L.; Lobbezoo, F.; Svensson, P. A conceptual model of oro-facial health with an emphasis on function. J. Oral Rehabil. 2021, 48, 1283–1294. [Google Scholar] [CrossRef] [PubMed]
- Iturriaga, V.; Bornhardt, T.; Velasquez, N. Temporomandibular Joint: Review of Anatomy and Clinical Implications. Dent. Clin. N. Am. 2023, 67, 199–209. [Google Scholar] [CrossRef] [PubMed]
- Wilkie, G.; Al-Ani, Z. Temporomandibular joint anatomy, function and clinical relevance. Br. Dent. J. 2022, 233, 539–546. [Google Scholar] [CrossRef] [PubMed]
- Okeson, J.P. Management of Temporomandibular Disorders and Occlusion, 8th ed.; Elsevier: St. Louis, MO, USA; Mosby: New York, NY, USA, 2019; pp. 2–74. [Google Scholar]
- Bordoni, B.; Varacallo, M. Anatomy, Head and Neck, Temporomandibular Joint. In StatPearls Interntet; StatPearls Publishing: Treasure Island, FL, USA, 2023. [Google Scholar]
- Hoppenfeld, S. Physical Examination of the Cervical Spine and Temporomandibular Joint, Physical Examination of the Spine and Extremities, 2nd ed.; Appleton and Lange: Norwalk, CT, USA, 1976; pp. 105–132. [Google Scholar]
- Bitiniene, D.; Zamaliauskiene, R.; Kubilius, R.; Leketas, M.; Gailius, T.; Smirnovaite, K. Quality of life in patients with temporomandibular disorders. A systematic review. Stomatologija 2018, 20, 3–9. [Google Scholar]
- Pigozzi, L.B.; Progiante, P.S.; Pattussi, M.P.; Pellizzer, E.P.; Grossi, P.K.; Grossi, M.L. General health quality of life in patients with temporomandibular disorders in an adult population-based cross-sectional study in Southern-Brazil. Int. J. Prosthodont. 2019, 32, 237–240. [Google Scholar] [CrossRef]
- Ahuja, V.; Ranjan, V.; Passi, D.; Jaiswal, R. Study of stress-induced temporomandibular disorders among dental students: An institutional study. Natl. J. Maxillofac. Surg. 2018, 9, 147–154. [Google Scholar]
- Minervini, G.; Franco, R.; Marrapodi, M.M.; Mehta, V.; Fiorillo, L.; Badnjević, A.; Cervino, G.; Cicciù, M. The Association between COVID-19 Related Anxiety, Stress, Depression, Temporomandibular Disorders, and Headaches from Childhood to Adulthood: A Systematic Review. Brain Sci. 2023, 13, 481. [Google Scholar] [CrossRef]
- Ginszt, M.; Zieliński, G.; Szkutnik, J.; Wójcicki, M.; Baszczowski, M.; Litko-Rola, M.; Zielińska, D.; Różyło-Kalinowska, I. The Difference in Electromyographic Activity While Wearing a Medical Mask in Women with and without Temporomandibular Disorders. Int. J. Environ. Res. Public Health 2022, 19, 15559. [Google Scholar] [CrossRef]
- Jo, J.-H.; Chung, J.-W. Gender Differences in Clinical Characteristics of Korean Temporomandibular Disorder Patients. Appl. Sci. 2021, 11, 3583. [Google Scholar] [CrossRef]
- Walczyńska-Dragon, K.; Baron, S.; Nitecka-Buchta, A.; Tkacz, E. Correlation between TMD and cervical spine pain and mobility: Is the whole-body balance TMJ related? Biomed. Res. Int. 2014, 2014, 582414. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Raya, C.R.; Plaza-Manzano, G.; Pecos-Martín, D.; Ferragut-Garcías, A.; Martín-Casas, P.; Gallego-Izquierdo, T.; Romero-Franco, N. Role of upper cervical spine in temporomandibular disorders. J. Back Musculoskelet Rehabil. 2017, 30, 1245–1250. [Google Scholar] [CrossRef]
- Zieliński, G.; Matysik-Woźniak, A.; Rapa, M.; Baszczowski, M.; Ginszt, M.; Zawadka, M.; Szkutnik, J.; Rejdak, R.; Gawda, P. The Influence of Visual Input on Electromyographic Patterns of Masticatory and Cervical Spine Muscles in Subjects with Myopia. J. Clin. Med. 2021, 10, 5376. [Google Scholar] [CrossRef] [PubMed]
- National Institute of Dental and Craniofacial Research (NIDCR). Facial Pain; National Institutes of Health: Betseda, MD, USA, 2014. Available online: www.nidcr.nih.gov/DataStatistics/FindDataByTopic/FacialPain (accessed on 14 October 2017).
- Sharma, S.; Ohrbach, R. Definition, aetiology, and epidemiology of temporomandibular disorders. In Temporomandibular Disorders: Manual Therapy, Exercise and Needling Therapies, 7th ed.; Fernández-de-las-Peñas, C., Mesa, J., Leon, C., Eds.; Handspring Publishing: Edinburgh, Scotland, 2018; pp. 243–255. [Google Scholar]
- Valesan, L.F.; Da-Cas, C.D.; Reus, J.C.; Denardin, A.C.S.; Garanhani, R.R.; Bonotto, D.; Januzzi, E.; de Souza, B.D.M. Prevalence of temporomandibular joint disorders: A systematic review and meta-analysis. Clin. Oral. Investig. 2021, 25, 441–453. [Google Scholar] [CrossRef]
- Gharavi, S.M.; Qiao, Y.; Faghihimehr, A.; Vossen, J. Imaging of the Temporomandibular Joint. Diagnostics 2022, 12, 1006. [Google Scholar] [CrossRef]
- Jeremic-Knezevic, M. Determing the Validity of Clinical Findings of Temporomandibular Disorders with Magnetic Resonance Imaging. Ph.D. Thesis, University of Novi Sad, Novi Sad, Serbia, 2015. [Google Scholar]
- Bag, A.K.; Gaddikeri, S.; Singhal, A.; Hardin, S.; Tran, B.D.; Medina, J.A.; Curé, J.K. Imaging of the temporomandibular joint: An update. World J. Radiol. 2014, 6, 567–582. [Google Scholar] [CrossRef] [PubMed]
- Poluha, R.L.; Canales, G.T.; Costa, Y.M.; Grossmann, E.; Bonjardim, L.R.; Conti, P.C.R. Temporomandibular joint disc displacement with reduction: A review of mechanisms and clinical presentation. J. Appl. Oral. Sci. 2019, 27, e20180433. [Google Scholar] [CrossRef]
- Vogl, T.J.; Lauer, H.C.; Lehnert, T.; Naguib, N.N.; Ottl, P.; Filmann, N. The value of MRI in patients with temporomandibular joint dysfunction: Correlation of MRI and clinical findings. Eur. J. Radiol. 2016, 85, 714–719. [Google Scholar] [CrossRef]
- Costen, J. Syndrome of ear and sinus symptoms dependent upon disturbed function of the temporomandibular joint. Ann. Otol. Rhinol. Laryngolo. 1934, 43, 1–15. [Google Scholar] [CrossRef]
- Vogl, T.J.; Eberhard, D.; Bergman, C.; Lissner, J. Incremental hydraulic jaw opener for MR imaging of the temporomandibular joint. J. Magn. Reson. Imaging 1992, 2, 479–482. [Google Scholar] [CrossRef]
- GE Healthcare. Medrad TMJ-200 Bi-Directional Device. 2020. Available online: https://services.gehealthcare.com/gehcstorefront/c/ACC_CTG_L2_MR_26 (accessed on 25 October 2020).
- Szopinski, K.; Regulski, P.A. A simple graded bite block for dynamic magnetic resonance imaging of the temporomandibular joint. Dentomaxillofac. Radiol. 2022, 51, 20210119. [Google Scholar] [CrossRef]
- Kamel, Z.S.A.S.A.; El-Shafey, M.H.R.; Hassanien, O.A.; Nagy, H.A. Can dynamic magnetic resonance imaging replace static magnetic resonance sequences in evaluation of temporomandibular joint dysfunction? Egypt. J. Radiol. Nucl. Med. 2021, 52, 19. [Google Scholar] [CrossRef]
- Faul, F.; Erdfelder, E.; Buchner, A.; Lang, A.-G. Statistical power analyses using G*Power 3.1: Tests for correlation and regression analyses. Behav. Res. Methods 2009, 41, 1149–1160. [Google Scholar] [CrossRef] [Green Version]
- Shrout, P.E.; Fleiss, J.L. Intraclass correlations: Uses in assessingrater reliability. Psychol. Bull. 1979, 86, 420–428. [Google Scholar] [CrossRef]
- Pihut, M.; Kulesa-Mrowiecka, M. The Emergencies in the Group of Patients with Temporomandibular Disorders. J. Clin. Med. 2023, 12, 298. [Google Scholar] [CrossRef]
- Xiong, X.; Ye, Z.; Tang, H.; Wei, Y.; Nie, L.; Wei, X.; Liu, Y.; Song, B. MRI of Temporomandibular Joint Disorders: Recent Advances and Future Directions. J. Magn. Reson. Imaging 2021, 54, 1039–1052. [Google Scholar] [CrossRef]
- Zieliński, G.; Matysik-Woźniak, A.; Pankowska, A.; Pietura, R.; Rejdak, R.; Jonak, K. High Myopia and Thickness of Extraocular and Masticatory Muscles—7T MRI, Preliminary Study. J. Clin. Med. 2023, 12, 4166. [Google Scholar] [CrossRef]
- Raszewski, Z.; Nowakowska-Toporowska, A.; Nowakowska, D.; Więckiewicz, W. Update on Acrylic Resins Used in Dentistry. Mini. Rev. Med. Chem. 2021, 21, 2130–2137. [Google Scholar] [CrossRef]
- Zafar, M.S. Prosthodontic Applications of Polymethyl Methacrylate (PMMA): An Update. Polymers 2020, 12, 2299. [Google Scholar] [CrossRef]
- Tegnander, T.; Chladek, G.; Hovland, A.; Żmudzki, J.; Wojtek, P. Relationship between Clinical Symptoms and Magnetic Resonance Imaging in Temporomandibular Disorder (TMD) Patients Utilizing the Piper MRI Diagnostic System. J. Clin. Med. 2021, 10, 4698. [Google Scholar] [CrossRef]
- Vogl, T.J.; Günther, D.; Weigl, P.; Scholtz, J.E. Diagnostic value of dynamic magnetic resonance imaging of temporomandibular joint dysfunction. Eur. J. Radiol. Open 2021, 8, 100390. [Google Scholar] [CrossRef]
- Jeremic-Knezevic, M.; Knezevic, A.; Boban, N.; Koprivica, D.D.; Boban, J. Correlation of somatization, depression, and chronic pain with clinical findings of the temporomandibular disorders in asymptomatic women. CRANIO® 2021, 39, 17–23. [Google Scholar] [CrossRef]
- Knezevic, M.J.; Knezevic, A.; Boban, J.; Maletin, A.; Milekic, B.; Koprivica, D.D.; Puskar, T.; Semnic, R. High-Field Magnetic Resonance Imaging of the Temporomandibular Joint Low Agreement with Clinical Diagnosis in Asymptomatic Females. Diagnostics 2023, 13, 1986. [Google Scholar] [CrossRef]
- Schiffman, E.; Ohrbach, R.; Truelove, E.; Look, J.; Anderson, G.; Goulet, J.P.; List, T.; Svensson, P.; Gonzalez, Y.; Lobbezoo, F.; et al. International RDC/TMD Consortium Network, International association for Dental Research; Orofacial Pain Special Interest Group, International Association for the Study of Pain. Diagnostic Criteria for Temporomandibular Disorders (DC/TMD) for Clinical and Research Applications: Recommendations of the International RDC/TMD Consortium Network and Orofacial Pain Special Interest Group. J. Oral. Facial. Pain Headache 2014, 28, 6–27. [Google Scholar]
- Jeremić-Knežević, M.; Boban, J.; Đurović-Koprivica, D.; Krstić, V.; Marković, V.; Knežević, A. Imaging of the temporomandibular joint: Contemporary clinical and radiological implications. Srpski arhiv za celokupno lekarstvo 2020, 148, 242–250. [Google Scholar] [CrossRef] [Green Version]




| Types of Artifacts | Artifacts Presented | Artifacts Missing |
|---|---|---|
| Signal-to-noise-ratio (SNR) | 1–3 | 0 |
| Susceptibility | 1–3 | 0 |
| Signal intensity | 1–3 | 0 |
| Homogeneity of the field | 1–3 | 0 |
| Diagnosis According to MRI | N | % |
|---|---|---|
| Normal TMJ | 198 | 49.5 |
| Anterior dislocation with reduction | 46 | 11.5 |
| Anterior disclocation without reduction | 18 | 4.5 |
| Posterior dislocation | 4 | 1 |
| Ostheoarthritis | 100 | 25 |
| Disc dislocation with reduction + Ostheoarthritis | 20 | 5 |
| Disc dislocation without reduction + Ostheoarthritis | 6 | 1.5 |
| Posterior + Ostheoarthritis | 8 | 2 |
| Total | 400 | 100 |
| ICC | 95% CI | |
|---|---|---|
| SNR | 0.836 | 0.800–0.865 |
| Susceptibility | 0.818 | 0.779–0.850 |
| Signal intensity | 0.835 | 0.799–0.865 |
| Homogeneity of the field | 0.850 | 0.818–0.877 |
| ICC | 95% CI | |
|---|---|---|
| SNR | 0.910 | 0.891–0.926 |
| Susceptibility | 0.937 | 0.923–0.948 |
| Signal intensity | 0.912 | 0.893–0.928 |
| Homogeneity of the field | 0.907 | 0.887–0.924 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Knezevic, M.J.; Knezevic, A.; Boban, J.; Maletin, A.; Milekic, B.; Koprivica, D.D.; Mijatov, I.; Puskar, T. A New Mechanical Mouth Opener for Dynamic Magnetic Resonance Imaging of the Temporomandibular Joint. J. Clin. Med. 2023, 12, 5035. https://doi.org/10.3390/jcm12155035
Knezevic MJ, Knezevic A, Boban J, Maletin A, Milekic B, Koprivica DD, Mijatov I, Puskar T. A New Mechanical Mouth Opener for Dynamic Magnetic Resonance Imaging of the Temporomandibular Joint. Journal of Clinical Medicine. 2023; 12(15):5035. https://doi.org/10.3390/jcm12155035
Chicago/Turabian StyleKnezevic, Milica Jeremic, Aleksandar Knezevic, Jasmina Boban, Aleksandra Maletin, Bojana Milekic, Daniela Djurovic Koprivica, Ivana Mijatov, and Tatjana Puskar. 2023. "A New Mechanical Mouth Opener for Dynamic Magnetic Resonance Imaging of the Temporomandibular Joint" Journal of Clinical Medicine 12, no. 15: 5035. https://doi.org/10.3390/jcm12155035
APA StyleKnezevic, M. J., Knezevic, A., Boban, J., Maletin, A., Milekic, B., Koprivica, D. D., Mijatov, I., & Puskar, T. (2023). A New Mechanical Mouth Opener for Dynamic Magnetic Resonance Imaging of the Temporomandibular Joint. Journal of Clinical Medicine, 12(15), 5035. https://doi.org/10.3390/jcm12155035






