Management of Coronary Artery Disease in Older Adults: Recent Advances and Gaps in Evidence
Abstract
1. Introduction
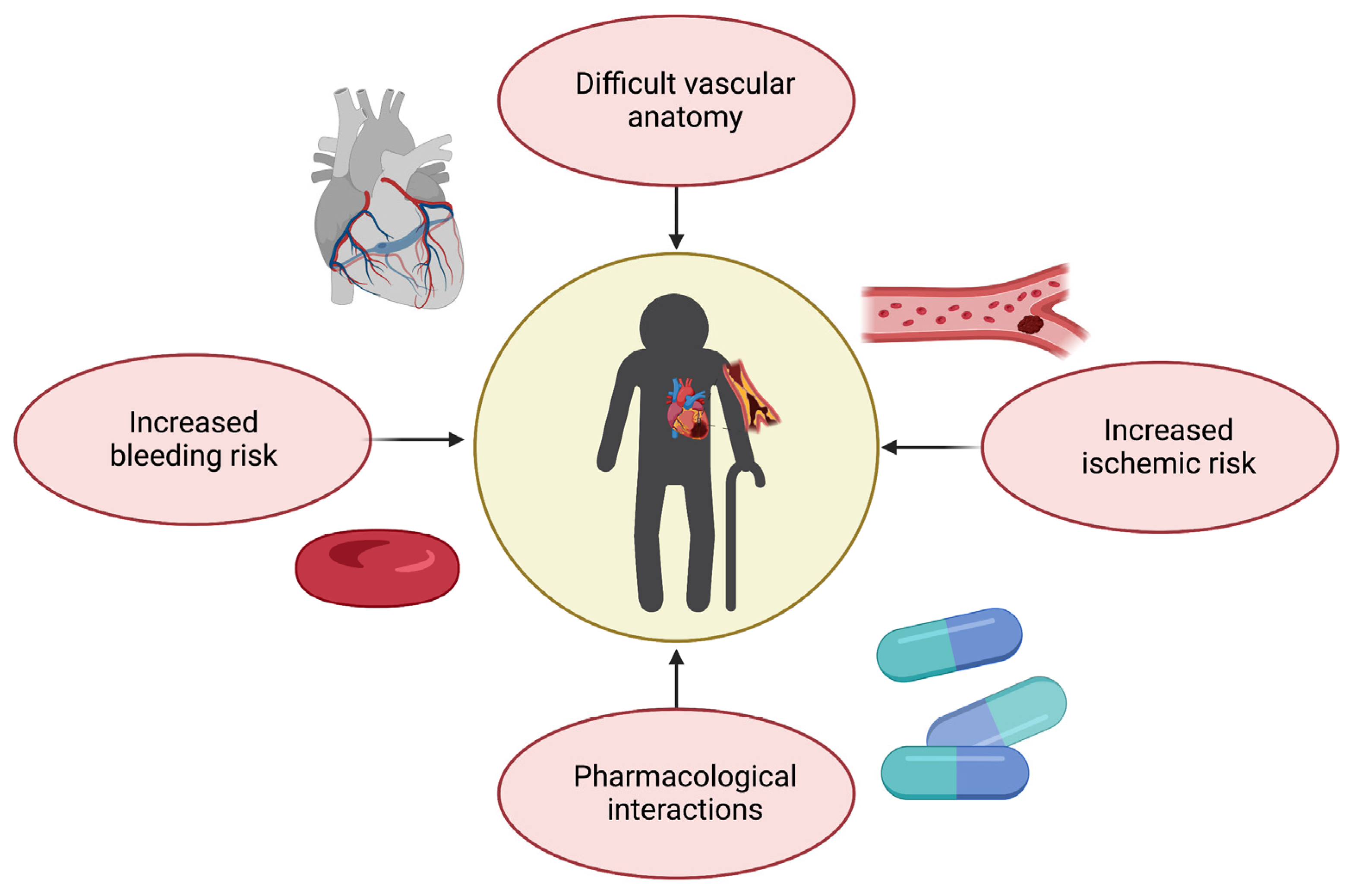
2. Assessment of Frailty
3. Optimal Strategy during the Acute Phase of Coronary Syndromes: Percutaneous Coronary Intervention, Coronary Artery Bypass Graft Surgery, or Medical Treatment?
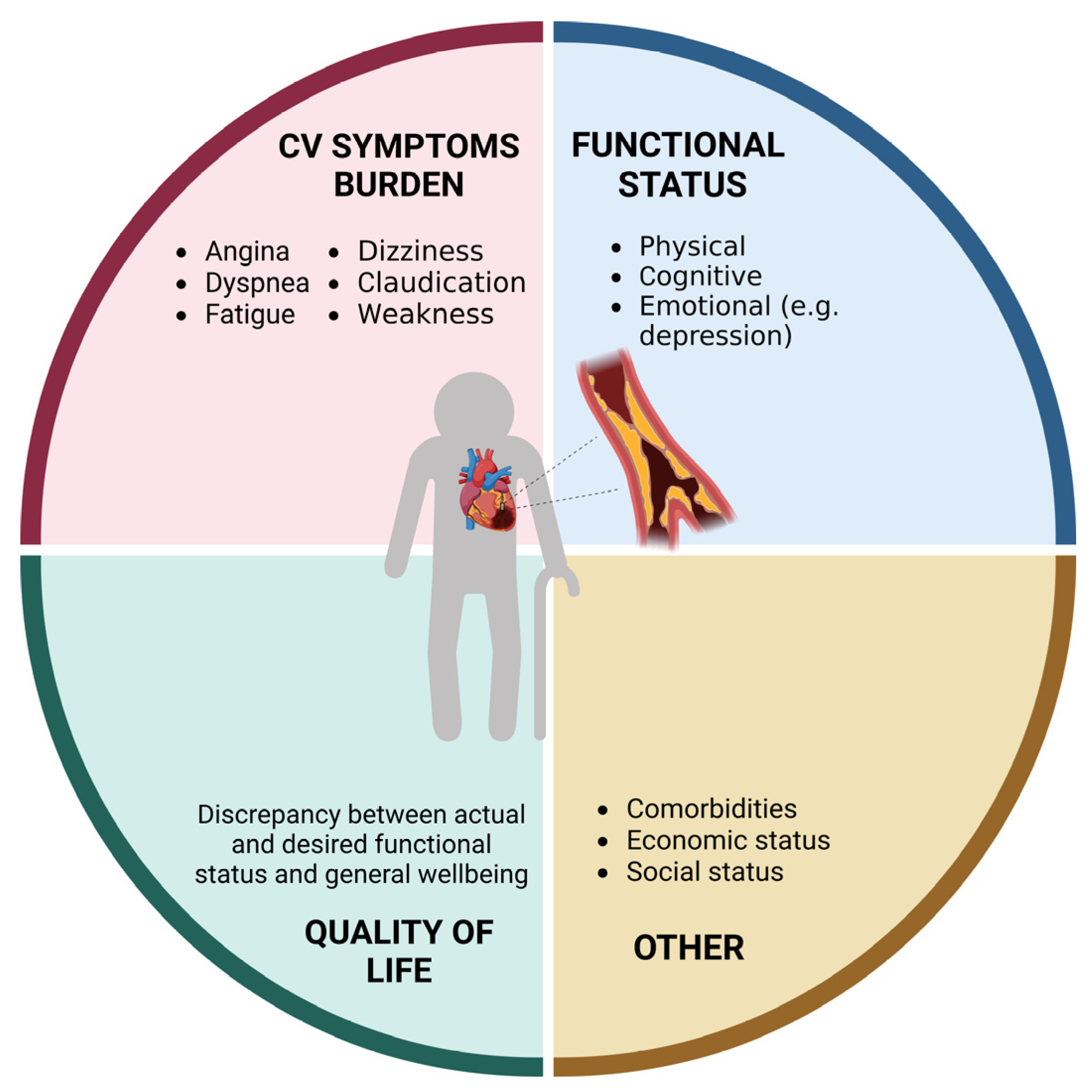
4. Medical Treatment
5. Follow-Up of Older Patients and Collaborative Approach
6. Gaps in Evidence
7. Future Perspectives and Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Camici, G.G.; Liberale, L. Aging: The next cardiovascular disease? Eur. Heart J. 2017, 38, 1621–1623. [Google Scholar] [CrossRef] [PubMed]
- Cacciatore, S.; Martone, A.M.; Landi, F.; Tosato, M. Acute Coronary Syndrome in Older Adults: An Update from the 2022 Scientific Statement by the American Heart Association. Heart Vessel. Transplant. 2023, 7, 7–10. [Google Scholar] [CrossRef]
- Nanna, M.G.; Chen, S.T.; Nelson, A.J.; Navar, A.M.; Peterson, E.D. Representation of Older Adults in Cardiovascular Disease Trials Since the Inclusion Across the Lifespan Policy. JAMA Intern. Med. 2020, 180, 1531–1533. [Google Scholar] [CrossRef] [PubMed]
- Hofman, C.S.; Makai, P.; Boter, H.; Buurman, B.M.; de Craen, A.J.; Olde Rikkert, M.G.; Donders, R.A.; Melis, R.J. Establishing a composite endpoint for measuring the effectiveness of geriatric interventions based on older persons’ and informal caregivers’ preference weights: A vignette study. BMC Geriatr. 2014, 14, 51. [Google Scholar] [CrossRef]
- Uchikado, Y.; Ikeda, Y.; Ohishi, M. Current Understanding of the Role of Frailty in Cardiovascular Disease. Circ. J. 2020, 84, 1903–1908. [Google Scholar] [CrossRef] [PubMed]
- Morley, J.E.; Vellas, B.; van Kan, G.A.; Anker, S.D.; Bauer, J.M.; Bernabei, R.; Cesari, M.; Chumlea, W.C.; Doehner, W.; Evans, J.; et al. Frailty consensus: A call to action. J. Am. Med. Dir. Assoc. 2013, 14, 392–397. [Google Scholar] [CrossRef] [PubMed]
- Ekerstad, N.; Swahn, E.; Janzon, M.; Alfredsson, J.; Löfmark, R.; Lindenberger, M.; Carlsson, P. Frailty is independently associated with short-term outcomes for elderly patients with non-ST-segment elevation myocardial infarction. Circulation 2011, 124, 2397–2404. [Google Scholar] [CrossRef] [PubMed]
- Collet, J.P.; Thiele, H.; Barbato, E.; Barthelemy, O.; Bauersachs, J.; Bhatt, D.L.; Dendale, P.; Dorobantu, M.; Edvardsen, T.; Folliguet, T.; et al. 2020 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation. Eur. Heart J. 2021, 42, 1289–1367. [Google Scholar] [CrossRef]
- Liperoti, R.; Vetrano, D.L.; Palmer, K.; Targowski, T.; Cipriani, M.C.; Lo Monaco, M.R.; Giovannini, S.; Acampora, N.; Villani, E.R.; Bernabei, R.; et al. Association between frailty and ischemic heart disease: A systematic review and meta-analysis. BMC Geriatr. 2021, 21, 357. [Google Scholar] [CrossRef]
- Fried, L.P.; Tangen, C.M.; Walston, J.; Newman, A.B.; Hirsch, C.; Gottdiener, J.; Seeman, T.; Tracy, R.; Kop, W.J.; Burke, G.; et al. Frailty in older adults: Evidence for a phenotype. J. Gerontol. A Biol. Sci. Med. Sci. 2001, 56, M146–M156. [Google Scholar] [CrossRef]
- Mitnitski, A.B.; Mogilner, A.J.; Rockwood, K. Accumulation of deficits as a proxy measure of aging. Sci. World J. 2001, 1, 323–336. [Google Scholar] [CrossRef]
- Reichart, D.; Rosato, S.; Nammas, W.; Onorati, F.; Dalen, M.; Castro, L.; Gherli, R.; Gatti, G.; Franzese, I.; Faggian, G.; et al. Clinical frailty scale and outcome after coronary artery bypass grafting. Eur. J. Cardiothorac. Surg. 2018, 54, 1102–1109. [Google Scholar] [CrossRef] [PubMed]
- Afilalo, J.; Lauck, S.; Kim, D.H.; Lefevre, T.; Piazza, N.; Lachapelle, K.; Martucci, G.; Lamy, A.; Labinaz, M.; Peterson, M.D.; et al. Frailty in Older Adults Undergoing Aortic Valve Replacement: The FRAILTY-AVR Study. J. Am. Coll. Cardiol. 2017, 70, 689–700. [Google Scholar] [CrossRef]
- Rolfson, D.B.; Majumdar, S.R.; Tsuyuki, R.T.; Tahir, A.; Rockwood, K. Validity and reliability of the Edmonton Frail Scale. Age Ageing 2006, 35, 526–529. [Google Scholar] [CrossRef]
- Miller, M.D.; Paradis, C.F.; Houck, P.R.; Mazumdar, S.; Stack, J.A.; Rifai, A.H.; Mulsant, B.; Reynolds, C.F., 3rd. Rating chronic medical illness burden in geropsychiatric practice and research: Application of the Cumulative Illness Rating Scale. Psychiatry Res. 1992, 41, 237–248. [Google Scholar] [CrossRef]
- Roehrig, B.; Hoeffken, K.; Pientka, L.; Wedding, U. How many and which items of activities of daily living (ADL) and instrumental activities of daily living (IADL) are necessary for screening. Crit. Rev. Oncol. Hematol. 2007, 62, 164–171. [Google Scholar] [CrossRef] [PubMed]
- Sainsbury, A.; Seebass, G.; Bansal, A.; Young, J.B. Reliability of the Barthel Index when used with older people. Age Ageing 2005, 34, 228–232. [Google Scholar] [CrossRef] [PubMed]
- Tombaugh, T.N.; McIntyre, N.J. The mini-mental state examination: A comprehensive review. J. Am. Geriatr. Soc. 1992, 40, 922–935. [Google Scholar] [CrossRef]
- Nasreddine, Z.S.; Phillips, N.A.; Bedirian, V.; Charbonneau, S.; Whitehead, V.; Collin, I.; Cummings, J.L.; Chertkow, H. The Montreal Cognitive Assessment, MoCA: A brief screening tool for mild cognitive impairment. J. Am. Geriatr. Soc. 2005, 53, 695–699. [Google Scholar] [CrossRef]
- Pfeiffer, E. A short portable mental status questionnaire for the assessment of organic brain deficit in elderly patients. J. Am. Geriatr. Soc. 1975, 23, 433–441. [Google Scholar] [CrossRef] [PubMed]
- Cacciatore, S.; Marzetti, E. Sarcopenia and physical function: Proxies of overall health and predictors of mortality in older adults. Arch. Gerontol. Geriatr. 2023, 112, 105037. [Google Scholar] [CrossRef]
- Kang, S.H.; Song, H.N.; Moon, J.Y.; Kim, S.H.; Sung, J.H.; Kim, I.J.; Lim, S.W.; Cha, D.H.; Kim, W.J. Prevalence and prognostic significance of malnutrition in patients with acute coronary syndrome treated with percutaneous coronary intervention. Medicine 2022, 101, e30100. [Google Scholar] [CrossRef]
- Cruz-Jentoft, A.J.; Bahat, G.; Bauer, J.; Boirie, Y.; Bruyere, O.; Cederholm, T.; Cooper, C.; Landi, F.; Rolland, Y.; Sayer, A.A.; et al. Sarcopenia: Revised European consensus on definition and diagnosis. Age Ageing 2019, 48, 16–31. [Google Scholar] [CrossRef]
- Damluji, A.A.; Alfaraidhy, M.; AlHajri, N.; Rohant, N.N.; Kumar, M.; Al Malouf, C.; Bahrainy, S.; Ji Kwak, M.; Batchelor, W.B.; Forman, D.E.; et al. Sarcopenia and Cardiovascular Diseases. Circulation 2023, 147, 1534–1553. [Google Scholar] [CrossRef] [PubMed]
- Tobe, A.; Tanaka, A.; Shirai, Y.; Kubota, Y.; Kunieda, T.; Sato, S.; Furusawa, K.; Ishii, H.; Murohara, T. Impact of Handgrip Strength on Clinical Outcomes after Percutaneous Coronary Intervention. J. Atheroscler. Thromb. 2022, 63854. [Google Scholar] [CrossRef]
- Larcher, B.; Zanolin-Purin, D.; Vonbank, A.; Heinzle, C.F.; Mader, A.; Sternbauer, S.; Drexel, H.; Saely, C.H. Usefulness of Handgrip Strength to Predict Mortality in Patients With Coronary Artery Disease. Am. J. Cardiol. 2020, 129, 5–9. [Google Scholar] [CrossRef] [PubMed]
- Fountotos, R.; Munir, H.; Goldfarb, M.; Lauck, S.; Kim, D.; Perrault, L.; Arora, R.; Moss, E.; Rudski, L.G.; Bendayan, M.; et al. Prognostic Value of Handgrip Strength in Older Adults Undergoing Cardiac Surgery. Can. J. Cardiol. 2021, 37, 1760–1766. [Google Scholar] [CrossRef] [PubMed]
- Han, P.; Yu, H.; Zhang, Y.; Xie, F.; Shao, B.; Liu, X.; Yuan, B.; Liu, Z.; Liu, X.; Guo, Q. Preoperative Short Physical Performance Battery as a predictor of prolonged hospitalization after coronary artery bypass grafting in older patients. J. Int. Med. Res. 2021, 49, 3000605211044043. [Google Scholar] [CrossRef]
- Komici, K.; Vitale, D.F.; Mancini, A.; Bencivenga, L.; Conte, M.; Provenzano, S.; Grieco, F.V.; Visaggi, L.; Ronga, I.; Cittadini, A.; et al. Impact of Malnutrition on Long-Term Mortality in Elderly Patients with Acute Myocardial Infarction. Nutrients 2019, 11, 224. [Google Scholar] [CrossRef]
- Komici, K.; Vitale, D.F.; Leosco, D.; Mancini, A.; Corbi, G.; Bencivenga, L.; Mezzani, A.; Trimarco, B.; Morisco, C.; Ferrara, N.; et al. Pressure injuries in elderly with acute myocardial infarction. Clin. Interv. Aging 2017, 12, 1495–1501. [Google Scholar] [CrossRef] [PubMed]
- Cederholm, T.; Jensen, G.L.; Correia, M.; Gonzalez, M.C.; Fukushima, R.; Higashiguchi, T.; Baptista, G.; Barazzoni, R.; Blaauw, R.; Coats, A.; et al. GLIM criteria for the diagnosis of malnutrition—A consensus report from the global clinical nutrition community. Clin. Nutr. 2019, 38, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Tonet, E.; Campana, R.; Caglioni, S.; Gibiino, F.; Fiorio, A.; Chiaranda, G.; Zagnoni, S.; Casella, G.; Campo, G. Tools for the Assessment of the Malnutrition Status and Possible Interventions in Elderly with Cardiovascular Diseases. J. Clin. Med. 2021, 10, 1508. [Google Scholar] [CrossRef] [PubMed]
- Kananen, L.; Eriksdotter, M.; Bostrom, A.M.; Kivipelto, M.; Annetorp, M.; Metzner, C.; Back Jerlardtz, V.; Engstrom, M.; Johnson, P.; Lundberg, L.G.; et al. Body mass index and Mini Nutritional Assessment-Short Form as predictors of in-geriatric hospital mortality in older adults with COVID-19. Clin. Nutr. 2022, 41, 2973–2979. [Google Scholar] [CrossRef]
- Keller, U. Nutritional Laboratory Markers in Malnutrition. J. Clin. Med. 2019, 8, 775. [Google Scholar] [CrossRef] [PubMed]
- Nicholson, A.; Kuper, H.; Hemingway, H. Depression as an aetiologic and prognostic factor in coronary heart disease: A meta-analysis of 6362 events among 146,538 participants in 54 observational studies. Eur. Heart J. 2006, 27, 2763–2774. [Google Scholar] [CrossRef]
- Yesavage, J.A.; Brink, T.L.; Rose, T.L.; Lum, O.; Huang, V.; Adey, M.; Leirer, V.O. Development and validation of a geriatric depression screening scale: A preliminary report. J. Psychiatr. Res. 1982, 17, 37–49. [Google Scholar] [CrossRef] [PubMed]
- Boreskie, K.F.; Hay, J.L.; Boreskie, P.E.; Arora, R.C.; Duhamel, T.A. Frailty-aware care: Giving value to frailty assessment across different healthcare settings. BMC Geriatr. 2022, 22, 13. [Google Scholar] [CrossRef]
- Galli, M.; Angiolillo, D.J. De-escalation of antiplatelet therapy in acute coronary syndromes: Why, how and when? Front. Cardiovasc. Med. 2022, 9, 975969. [Google Scholar] [CrossRef]
- Wang, T.Y.; Gutierrez, A.; Peterson, E.D. Percutaneous coronary intervention in the elderly. Nat. Rev. Cardiol. 2011, 8, 79–90. [Google Scholar] [CrossRef]
- Rathore, S.S.; Weinfurt, K.P.; Foody, J.M.; Krumholz, H.M. Performance of the Thrombolysis in Myocardial Infarction (TIMI) ST-elevation myocardial infarction risk score in a national cohort of elderly patients. Am. Heart J. 2005, 150, 402–410. [Google Scholar] [CrossRef]
- van der Sangen, N.M.R.; Azzahhafi, J.; Chan Pin Yin, D.; Peper, J.; Rayhi, S.; Walhout, R.J.; Tjon Joe Gin, M.; Nicastia, D.M.; Langerveld, J.; Vlachojannis, G.J.; et al. External validation of the GRACE risk score and the risk-treatment paradox in patients with acute coronary syndrome. Open Heart 2022, 9, e001984. [Google Scholar] [CrossRef]
- Anand, A.; Cudmore, S.; Robertson, S.; Stephen, J.; Haga, K.; Weir, C.J.; Murray, S.A.; Boyd, K.; Gunn, J.; Iqbal, J.; et al. Frailty assessment and risk prediction by GRACE score in older patients with acute myocardial infarction. BMC Geriatr. 2020, 20, 102. [Google Scholar] [CrossRef]
- Fox, K.A.; Fitzgerald, G.; Puymirat, E.; Huang, W.; Carruthers, K.; Simon, T.; Coste, P.; Monsegu, J.; Gabriel Steg, P.; Danchin, N.; et al. Should patients with acute coronary disease be stratified for management according to their risk? Derivation, external validation and outcomes using the updated GRACE risk score. BMJ Open 2014, 4, e004425. [Google Scholar] [CrossRef] [PubMed]
- Urban, P.; Mehran, R.; Colleran, R.; Angiolillo, D.J.; Byrne, R.A.; Capodanno, D.; Cuisset, T.; Cutlip, D.; Eerdmans, P.; Eikelboom, J.; et al. Defining High Bleeding Risk in Patients Undergoing Percutaneous Coronary Intervention. Circulation 2019, 140, 240–261. [Google Scholar] [CrossRef]
- Skolnick, A.H.; Alexander, K.P.; Chen, A.Y.; Roe, M.T.; Pollack, C.V., Jr.; Ohman, E.M.; Rumsfeld, J.S.; Gibler, W.B.; Peterson, E.D.; Cohen, D.J. Characteristics, management, and outcomes of 5,557 patients age > or =90 years with acute coronary syndromes: Results from the CRUSADE Initiative. J. Am. Coll. Cardiol. 2007, 49, 1790–1797. [Google Scholar] [CrossRef]
- De Luca, L.; Marini, M.; Gonzini, L.; Boccanelli, A.; Casella, G.; Chiarella, F.; De Servi, S.; Di Chiara, A.; Di Pasquale, G.; Olivari, Z.; et al. Contemporary Trends and Age-Specific Sex Differences in Management and Outcome for Patients With ST-Segment Elevation Myocardial Infarction. J. Am. Heart Assoc. 2016, 5, e004202. [Google Scholar] [CrossRef] [PubMed]
- De Luca, L.; Olivari, Z.; Bolognese, L.; Lucci, D.; Gonzini, L.; Di Chiara, A.; Casella, G.; Chiarella, F.; Boccanelli, A.; Di Pasquale, G.; et al. A decade of changes in clinical characteristics and management of elderly patients with non-ST elevation myocardial infarction admitted in Italian cardiac care units. Open Heart 2014, 1, e000148. [Google Scholar] [CrossRef]
- Spadafora, L.; Bernardi, M.; Biondi-Zoccai, G.; Frati, G. Coronary artery bypass grafting added to surgical aortic valve replacement in octogenarians. Interact. Cardiovasc. Thorac. Surg. 2022, 35, ivac191. [Google Scholar] [CrossRef] [PubMed]
- Gallingani, A.; D’Alessandro, S.; Singh, G.; Hernandez-Vaquero, D.; Celik, M.; Ceccato, E.; Nicolini, F.; Formica, F. The impact of coronary artery bypass grafting added to aortic valve replacement on long-term outcomes in octogenarian patients: A reconstructed time-to-event meta-analysis. Interact. Cardiovasc. Thorac. Surg. 2022, 35, ivac164. [Google Scholar] [CrossRef]
- Adelborg, K.; Horvath-Puho, E.; Schmidt, M.; Munch, T.; Pedersen, L.; Nielsen, P.H.; Botker, H.E.; Toft Sorensen, H. Thirty-Year Mortality After Coronary Artery Bypass Graft Surgery: A Danish Nationwide Population-Based Cohort Study. Circ. Cardiovasc. Qual. Outcomes 2017, 10, e002708. [Google Scholar] [CrossRef]
- Lemaire, A.; Soto, C.; Salgueiro, L.; Ikegami, H.; Russo, M.J.; Lee, L.Y. The impact of age on outcomes of coronary artery bypass grafting. J. Cardiothorac. Surg. 2020, 15, 158. [Google Scholar] [CrossRef]
- Park, D.Y.; Jamil, Y.; Hu, J.R.; Lowenstern, A.; Frampton, J.; Abdullah, A.; Damluji, A.A.; Ahmad, Y.; Soufer, R.; Nanna, M.G. Delirium in older adults after percutaneous coronary intervention: Prevalence, risks, and clinical phenotypes. Cardiovasc. Revasc. Med. 2023; in press. [Google Scholar] [CrossRef]
- Nanna, M.G.; Sutton, N.R.; Kochar, A.; Rymer, J.A.; Lowenstern, A.M.; Gackenbach, G.; Hummel, S.L.; Goyal, P.; Rich, M.W.; Kirkpatrick, J.N.; et al. A Geriatric Approach to Percutaneous Coronary Interventions in Older Adults, Part II. JACC Adv. 2023, 2, 100421. [Google Scholar] [CrossRef]
- Damluji, A.A.; Forman, D.E.; van Diepen, S.; Alexander, K.P.; Page, R.L.; Hummel, S.L.; Menon, V.; Katz, J.N.; Albert, N.M.; Afilalo, J.; et al. Older Adults in the Cardiac Intensive Care Unit: Factoring Geriatric Syndromes in the Management, Prognosis, and Process of Care: A Scientific Statement From the American Heart Association. Circulation 2020, 141, e6–e32. [Google Scholar] [CrossRef] [PubMed]
- De Caterina, R.; Agewall, S.; Andreotti, F.; Angiolillo, D.J.; Bhatt, D.L.; Byrne, R.A.; Collet, J.P.; Eikelboom, J.; Fanaroff, A.C.; Gibson, C.M.; et al. Great Debate: Triple antithrombotic therapy in patients with atrial fibrillation undergoing coronary stenting should be limited to 1 week. Eur. Heart J. 2022, 43, 3512–3527. [Google Scholar] [CrossRef] [PubMed]
- Smith, W.; Whitlock, E.L. Cardiac surgery, ICU sedation, and delirium: Is dexmedetomidine the silver bullet? Curr. Opin. Anaesthesiol. 2023, 36, 50–56. [Google Scholar] [CrossRef] [PubMed]
- Lozano-Vicario, L.; Garcia-Hermoso, A.; Cedeno-Veloz, B.A.; Fernandez-Irigoyen, J.; Santamaria, E.; Romero-Ortuno, R.; Zambom-Ferraresi, F.; Saez de Asteasu, M.L.; Munoz-Vazquez, A.J.; Izquierdo, M.; et al. Biomarkers of delirium risk in older adults: A systematic review and meta-analysis. Front. Aging Neurosci. 2023, 15, 1174644. [Google Scholar] [CrossRef] [PubMed]
- Watne, L.O.; Pollmann, C.T.; Neerland, B.E.; Quist-Paulsen, E.; Halaas, N.B.; Idland, A.V.; Hassel, B.; Henjum, K.; Knapskog, A.B.; Frihagen, F.; et al. Cerebrospinal fluid quinolinic acid is strongly associated with delirium and mortality in hip-fracture patients. J. Clin. Investig. 2023, 133, e163472. [Google Scholar] [CrossRef] [PubMed]
- Spadafora, L.; Bernardi, M.; Galli, M.; Biondi-Zoccai, G.; Sabouret, P. Which future for aspirin in acute coronary syndromes treated with percutaneous coronary intervention? An overview on aspirin-free strategies. Arch. Med. Sci. 2022, 18, 1689–1692. [Google Scholar] [CrossRef]
- Sabouret, P.; Spadafora, L.; Fischman, D.; Ullah, W.; Zeitouni, M.; Gulati, M.; De Rosa, S.; Savage, M.P.; Costabel, J.P.; Banach, M.; et al. De-escalation of antiplatelet therapy in patients with coronary artery disease: Time to change our strategy? Eur. J. Intern. Med. 2023, 110, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Calsolaro, V.; Okoye, C.; Rogani, S.; Calabrese, A.M.; Dell’Agnello, U.; Antognoli, R.; Guarino, D.; Monzani, F. Different glomerular filtration rate estimating formula for prescribing DOACs in oldest patients: Appropriate dosage and bleeding risk. Post hoc analysis of a prospective cohort. Aging Clin. Exp. Res. 2022, 34, 591–598. [Google Scholar] [CrossRef]
- Galli, M.; Andreotti, F.; D’Amario, D.; Vergallo, R.; Montone, R.A.; Porto, I.; Crea, F. Aspirin in primary prevention of cardiovascular disease in the elderly. Eur. Heart J. Cardiovasc. Pharmacother. 2020, 6, 326–327. [Google Scholar] [CrossRef] [PubMed]
- Arnett, D.K.; Blumenthal, R.S.; Albert, M.A.; Buroker, A.B.; Goldberger, Z.D.; Hahn, E.J.; Himmelfarb, C.D.; Khera, A.; Lloyd-Jones, D.; McEvoy, J.W.; et al. 2019 ACC/AHA Guideline on the Primary Prevention of Cardiovascular Disease: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation 2019, 140, e596–e646. [Google Scholar] [CrossRef] [PubMed]
- Costa, F.; van Klaveren, D.; James, S.; Heg, D.; Räber, L.; Feres, F.; Pilgrim, T.; Hong, M.K.; Kim, H.S.; Colombo, A.; et al. Derivation and validation of the predicting bleeding complications in patients undergoing stent implantation and subsequent dual antiplatelet therapy (PRECISE-DAPT) score: A pooled analysis of individual-patient datasets from clinical trials. Lancet 2017, 389, 1025–1034. [Google Scholar] [CrossRef] [PubMed]
- Yeh, R.W.; Secemsky, E.A.; Kereiakes, D.J.; Normand, S.L.; Gershlick, A.H.; Cohen, D.J.; Spertus, J.A.; Steg, P.G.; Cutlip, D.E.; Rinaldi, M.J.; et al. Development and Validation of a Prediction Rule for Benefit and Harm of Dual Antiplatelet Therapy Beyond 1 Year After Percutaneous Coronary Intervention. JAMA 2016, 315, 1735–1749. [Google Scholar] [CrossRef] [PubMed]
- Wiviott, S.D.; Braunwald, E.; McCabe, C.H.; Montalescot, G.; Ruzyllo, W.; Gottlieb, S.; Neumann, F.J.; Ardissino, D.; De Servi, S.; Murphy, S.A.; et al. Prasugrel versus clopidogrel in patients with acute coronary syndromes. N. Engl. J. Med. 2007, 357, 2001–2015. [Google Scholar] [CrossRef] [PubMed]
- Husted, S.; James, S.; Becker, R.C.; Horrow, J.; Katus, H.; Storey, R.F.; Cannon, C.P.; Heras, M.; Lopes, R.D.; Morais, J.; et al. Ticagrelor versus clopidogrel in elderly patients with acute coronary syndromes: A substudy from the prospective randomized PLATelet inhibition and patient Outcomes (PLATO) trial. Circ. Cardiovasc. Qual. Outcomes 2012, 5, 680–688. [Google Scholar] [CrossRef] [PubMed]
- Bonaca, M.P.; Bhatt, D.L.; Cohen, M.; Steg, P.G.; Storey, R.F.; Jensen, E.C.; Magnani, G.; Bansilal, S.; Fish, M.P.; Im, K.; et al. Long-term use of ticagrelor in patients with prior myocardial infarction. N. Engl. J. Med. 2015, 372, 1791–1800. [Google Scholar] [CrossRef] [PubMed]
- Gimbel, M.; Qaderdan, K.; Willemsen, L.; Hermanides, R.; Bergmeijer, T.; de Vrey, E.; Heestermans, T.; Tjon Joe Gin, M.; Waalewijn, R.; Hofma, S.; et al. Clopidogrel versus ticagrelor or prasugrel in patients aged 70 years or older with non-ST-elevation acute coronary syndrome (POPular AGE): The randomised, open-label, non-inferiority trial. Lancet 2020, 395, 1374–1381. [Google Scholar] [CrossRef]
- Kralev, S.; Schneider, K.; Lang, S.; Süselbeck, T.; Borggrefe, M. Incidence and severity of coronary artery disease in patients with atrial fibrillation undergoing first-time coronary angiography. PLoS ONE 2011, 6, e24964. [Google Scholar] [CrossRef] [PubMed]
- Hansen, M.L.; Sørensen, R.; Clausen, M.T.; Fog-Petersen, M.L.; Raunsø, J.; Gadsbøll, N.; Gislason, G.H.; Folke, F.; Andersen, S.S.; Schramm, T.K.; et al. Risk of bleeding with single, dual, or triple therapy with warfarin, aspirin, and clopidogrel in patients with atrial fibrillation. Arch. Intern. Med. 2010, 170, 1433–1441. [Google Scholar] [CrossRef] [PubMed]
- Potpara, T.S.; Mujovic, N.; Proietti, M.; Dagres, N.; Hindricks, G.; Collet, J.P.; Valgimigli, M.; Heidbuchel, H.; Lip, G.Y.H. Revisiting the effects of omitting aspirin in combined antithrombotic therapies for atrial fibrillation and acute coronary syndromes or percutaneous coronary interventions: Meta-analysis of pooled data from the PIONEER AF-PCI, RE-DUAL PCI, and AUGUSTUS trials. Europace 2020, 22, 33–46. [Google Scholar] [CrossRef] [PubMed]
- Bencivenga, L.; Komici, K.; Corbi, G.; Cittadini, A.; Ferrara, N.; Rengo, G. The Management of Combined Antithrombotic Therapy in Patients With Atrial Fibrillation Undergoing Percutaneous Coronary Intervention: A Particularly Complex Challenge, Especially in the Elderly. Front. Physiol. 2018, 9, 876. [Google Scholar] [CrossRef] [PubMed]
- Galli, M.; Andreotti, F.; Porto, I.; Crea, F. Intracranial haemorrhages vs. stent thromboses with direct oral anticoagulant plus single antiplatelet agent or triple antithrombotic therapy: A meta-analysis of randomized trials in atrial fibrillation and percutaneous coronary intervention/acute coronary syndrome patients. Europace 2020, 22, 538–546. [Google Scholar] [CrossRef] [PubMed]
- Knuuti, J.; Wijns, W.; Saraste, A.; Capodanno, D.; Barbato, E.; Funck-Brentano, C.; Prescott, E.; Storey, R.F.; Deaton, C.; Cuisset, T.; et al. 2019 ESC Guidelines for the diagnosis and management of chronic coronary syndromes. Eur. Heart J. 2020, 41, 407–477. [Google Scholar] [CrossRef] [PubMed]
- Kanenawa, K.; Yamaji, K.; Tashiro, H.; Morimoto, T.; Hiromasa, T.; Hayashi, M.; Hiramori, S.; Tomoi, Y.; Kuramitsu, S.; Domei, T.; et al. Frailty and Bleeding After Percutaneous Coronary Intervention. Am. J. Cardiol. 2021, 148, 22–29. [Google Scholar] [CrossRef] [PubMed]
- Galli, M.; Franchi, F.; Rollini, F.; Angiolillo, D.J. Role of platelet function and genetic testing in patients undergoing percutaneous coronary intervention. Trends Cardiovasc. Med. 2023, 33, 133–138. [Google Scholar] [CrossRef] [PubMed]
- Galli, M.; Benenati, S.; Capodanno, D.; Franchi, F.; Rollini, F.; D’Amario, D.; Porto, I.; Angiolillo, D.J. Guided versus standard antiplatelet therapy in patients undergoing percutaneous coronary intervention: A systematic review and meta-analysis. Lancet 2021, 397, 1470–1483. [Google Scholar] [CrossRef] [PubMed]
- Galli, M.; Benenati, S.; Franchi, F.; Rollini, F.; Capodanno, D.; Biondi-Zoccai, G.; Vescovo, G.M.; Cavallari, L.H.; Bikdeli, B.; Ten Berg, J.; et al. Comparative effects of guided vs. potent P2Y12 inhibitor therapy in acute coronary syndrome: A network meta-analysis of 61 898 patients from 15 randomized trials. Eur. Heart J. 2022, 43, 959–967. [Google Scholar] [CrossRef] [PubMed]
- Andrade, C.; Sandarsh, S.; Chethan, K.B.; Nagesh, K.S. Serotonin reuptake inhibitor antidepressants and abnormal bleeding: A review for clinicians and a reconsideration of mechanisms. J. Clin. Psychiatry 2010, 71, 1565–1575. [Google Scholar] [CrossRef]
- de Alencar Neto, J.N. Morphine, Oxygen, Nitrates, and Mortality Reducing Pharmacological Treatment for Acute Coronary Syndrome: An Evidence-based Review. Cureus 2018, 10, e2114. [Google Scholar] [CrossRef] [PubMed]
- Tarkin, J.M.; Kaski, J.C. Vasodilator Therapy: Nitrates and Nicorandil. Cardiovasc. Drugs Ther. 2016, 30, 367–378. [Google Scholar] [CrossRef] [PubMed]
- Testa, G.; Ceccofiglio, A.; Mussi, C.; Bellelli, G.; Nicosia, F.; Bo, M.; Riccio, D.; Curcio, F.; Martone, A.M.; Noro, G.; et al. Hypotensive Drugs and Syncope Due to Orthostatic Hypotension in Older Adults with Dementia (Syncope and Dementia Study). J. Am. Geriatr. Soc. 2018, 66, 1532–1537. [Google Scholar] [CrossRef] [PubMed]
- Alpert, J.S. Nitrate therapy in the elderly. Am. J. Cardiol. 1990, 65, J23–J27. [Google Scholar] [CrossRef] [PubMed]
- Andreasen, C.; Andersson, C. Current use of beta-blockers in patients with coronary artery disease. Trends Cardiovasc. Med. 2018, 28, 382–389. [Google Scholar] [CrossRef] [PubMed]
- Joseph, P.; Swedberg, K.; Leong, D.P.; Yusuf, S. The Evolution of beta-Blockers in Coronary Artery Disease and Heart Failure (Part 1/5). J. Am. Coll. Cardiol. 2019, 74, 672–682. [Google Scholar] [CrossRef] [PubMed]
- Motivala, A.A.; Parikh, V.; Roe, M.; Dai, D.; Abbott, J.D.; Prasad, A.; Mukherjee, D. Predictors, Trends, and Outcomes (Among Older Patients >/=65 Years of Age) Associated With Beta-Blocker Use in Patients With Stable Angina Undergoing Elective Percutaneous Coronary Intervention: Insights From the NCDR Registry. JACC Cardiovasc. Interv. 2016, 9, 1639–1648. [Google Scholar] [CrossRef]
- Huang, B.T.; Huang, F.Y.; Zuo, Z.L.; Liao, Y.B.; Heng, Y.; Wang, P.J.; Gui, Y.Y.; Xia, T.L.; Xin, Z.M.; Liu, W.; et al. Meta-Analysis of Relation Between Oral beta-Blocker Therapy and Outcomes in Patients With Acute Myocardial Infarction Who Underwent Percutaneous Coronary Intervention. Am. J. Cardiol. 2015, 115, 1529–1538. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.-D.; Li, F.-F.; Wen, Z.-P.; Liao, X.-X.; Du, Z.-M. Renin-angiotensin system inhibitors in patients with coronary artery disease who have undergone percutaneous coronary intervention. Ther. Adv. Cardiovasc. Dis. 2016, 10, 172–177. [Google Scholar] [CrossRef]
- Hoang, V.; Alam, M.; Addison, D.; Macedo, F.; Virani, S.; Birnbaum, Y. Efficacy of Angiotensin-Converting Enzyme Inhibitors and Angiotensin-Receptor Blockers in Coronary Artery Disease without Heart Failure in the Modern Statin Era: A Meta-Analysis of Randomized-Controlled Trials. Cardiovasc. Drugs Ther. 2016, 30, 189–198. [Google Scholar] [CrossRef] [PubMed]
- Turgutalp, K.; Bardak, S.; Helvaci, I.; Isguzar, G.; Payas, E.; Demir, S.; Kiykim, A. Community-acquired hyperkalemia in elderly patients: Risk factors and clinical outcomes. Ren. Fail. 2016, 38, 1405–1412. [Google Scholar] [CrossRef]
- Mukoyama, M.; Kuwabara, T. Role of renin-angiotensin system blockade in advanced CKD: To use or not to use? Hypertens. Res. 2022, 45, 1072–1075. [Google Scholar] [CrossRef] [PubMed]
- Ziaeian, B.; Fonarow, G.C. Statins and the Prevention of Heart Disease. JAMA Cardiol. 2017, 2, 464. [Google Scholar] [CrossRef] [PubMed]
- Aeschbacher-Germann, M.; Kaiser, N.; Speierer, A.; Blum, M.R.; Bauer, D.C.; Del Giovane, C.; Aujesky, D.; Gencer, B.; Rodondi, N.; Moutzouri, E. Lipid-Lowering Trials Are Not Representative of Patients Managed in Clinical Practice: A Systematic Review and Meta-Analysis of Exclusion Criteria. J. Am. Heart Assoc. 2023, 12, e026551. [Google Scholar] [CrossRef]
- Ward, N.C.; Watts, G.F.; Eckel, R.H. Statin Toxicity. Circ. Res. 2019, 124, 328–350. [Google Scholar] [CrossRef] [PubMed]
- Damiani, I.; Corsini, A.; Bellosta, S. Potential statin drug interactions in elderly patients: A review. Expert Opin. Drug Metab. Toxicol. 2020, 16, 1133–1145. [Google Scholar] [CrossRef] [PubMed]
- Wiggins, B.S.; Saseen, J.J.; Page, R.L., 2nd; Reed, B.N.; Sneed, K.; Kostis, J.B.; Lanfear, D.; Virani, S.; Morris, P.B.; American Heart Association Clinical Pharmacology Committee of the Council on Clinical Cardiology; et al. Recommendations for Management of Clinically Significant Drug-Drug Interactions With Statins and Select Agents Used in Patients With Cardiovascular Disease: A Scientific Statement From the American Heart Association. Circulation 2016, 134, e468–e495. [Google Scholar] [CrossRef] [PubMed]
- Ho, C.K.; Walker, S.W. Statins and their interactions with other lipid-modifying medications: Safety issues in the elderly. Ther. Adv. Drug Saf. 2012, 3, 35–46. [Google Scholar] [CrossRef] [PubMed]
- Thai, M.; Reeve, E.; Hilmer, S.N.; Qi, K.; Pearson, S.A.; Gnjidic, D. Prevalence of statin-drug interactions in older people: A systematic review. Eur. J. Clin. Pharmacol. 2016, 72, 513–521. [Google Scholar] [CrossRef] [PubMed]
- Tonelli, M.; Lloyd, A.M.; Bello, A.K.; James, M.T.; Klarenbach, S.W.; McAlister, F.A.; Manns, B.J.; Tsuyuki, R.T.; Hemmelgarn, B.R.; Alberta Kidney Disease Network. Statin use and the risk of acute kidney injury in older adults. BMC Nephrol. 2019, 20, 103. [Google Scholar] [CrossRef] [PubMed]
- Cholesterol Treatment Trialists Collaboration. Efficacy and safety of statin therapy in older people: A meta-analysis of individual participant data from 28 randomised controlled trials. Lancet 2019, 393, 407–415. [Google Scholar] [CrossRef] [PubMed]
- Zhou, Z.; Ofori-Asenso, R.; Curtis, A.J.; Breslin, M.; Wolfe, R.; McNeil, J.J.; Murray, A.M.; Ernst, M.E.; Reid, C.M.; Lockery, J.E.; et al. Association of Statin Use With Disability-Free Survival and Cardiovascular Disease Among Healthy Older Adults. J. Am. Coll. Cardiol. 2020, 76, 17–27. [Google Scholar] [CrossRef] [PubMed]
- Thalmann, I.; Preiss, D.; Schlackow, I.; Gray, A.; Mihaylova, B. Population-wide cohort study of statin use for the secondary cardiovascular disease prevention in Scotland in 2009–2017. Heart 2023, 109, 388–395. [Google Scholar] [CrossRef] [PubMed]
- Nanna, M.G.; Navar, A.M.; Wang, T.Y.; Mi, X.; Virani, S.S.; Louie, M.J.; Lee, L.V.; Goldberg, A.C.; Roger, V.L.; Robinson, J.; et al. Statin Use and Adverse Effects Among Adults >75 Years of Age: Insights From the Patient and Provider Assessment of Lipid Management (PALM) Registry. J. Am. Heart Assoc. 2018, 7, e008546. [Google Scholar] [CrossRef] [PubMed]
- Stone, N.J. Statins in Secondary Prevention: Intensity Matters. J. Am. Coll. Cardiol. 2017, 69, 2707–2709. [Google Scholar] [CrossRef] [PubMed]
- Awad, K.; Mohammed, M.; Zaki, M.M.; Abushouk, A.I.; Lip, G.Y.H.; Blaha, M.J.; Lavie, C.J.; Toth, P.P.; Jukema, J.W.; Sattar, N.; et al. Association of statin use in older people primary prevention group with risk of cardiovascular events and mortality: A systematic review and meta-analysis of observational studies. BMC Med. 2021, 19, 139. [Google Scholar] [CrossRef] [PubMed]
- Lavan, A.H.; Gallagher, P.; Parsons, C.; O’Mahony, D. STOPPFrail (Screening Tool of Older Persons Prescriptions in Frail adults with limited life expectancy): Consensus validation. Age Ageing 2017, 46, 600–607. [Google Scholar] [CrossRef]
- Laufs, U.; Banach, M.; Mancini, G.B.J.; Gaudet, D.; Bloedon, L.T.; Sterling, L.R.; Kelly, S.; Stroes, E.S.G. Efficacy and Safety of Bempedoic Acid in Patients With Hypercholesterolemia and Statin Intolerance. J. Am. Heart Assoc. 2019, 8, e011662. [Google Scholar] [CrossRef] [PubMed]
- Bytyci, I.; Penson, P.E.; Mikhailidis, D.P.; Wong, N.D.; Hernandez, A.V.; Sahebkar, A.; Thompson, P.D.; Mazidi, M.; Rysz, J.; Pella, D.; et al. Prevalence of statin intolerance: A meta-analysis. Eur. Heart J. 2022, 43, 3213–3223. [Google Scholar] [CrossRef] [PubMed]
- Banach, M.; Penson, P.E.; Farnier, M.; Fras, Z.; Latkovskis, G.; Laufs, U.; Paneni, F.; Parini, P.; Pirro, M.; Reiner, Z.; et al. Bempedoic acid in the management of lipid disorders and cardiovascular risk. 2023 position paper of the International Lipid Expert Panel (ILEP). Prog. Cardiovasc. Dis. 2023. [Google Scholar] [CrossRef] [PubMed]
- Zazzara, M.B.; Palmer, K.; Vetrano, D.L.; Carfi, A.; Onder, G. Adverse drug reactions in older adults: A narrative review of the literature. Eur. Geriatr. Med. 2021, 12, 463–473. [Google Scholar] [CrossRef] [PubMed]
- Damluji, A.A.; Forman, D.E.; Wang, T.Y.; Chikwe, J.; Kunadian, V.; Rich, M.W.; Young, B.A.; Page, R.L., 2nd; DeVon, H.A.; Alexander, K.P.; et al. Management of Acute Coronary Syndrome in the Older Adult Population: A Scientific Statement From the American Heart Association. Circulation 2023, 147, e32–e62. [Google Scholar] [CrossRef]
- Bueno, H. Managing end of life in intensive cardiac care units. Eur. Heart J. Acute Cardiovasc. Care 2022, 11, 198–200. [Google Scholar] [CrossRef]
- Krumholz, H.M. Post-hospital syndrome--an acquired, transient condition of generalized risk. N. Engl. J. Med. 2013, 368, 100–102. [Google Scholar] [CrossRef] [PubMed]
- Lettieri, C.; Colombo, P.; Rosiello, R.; Morici, N.; Parogni, P.; Musumeci, G.; Tabaglio, E.; Zadra, A.; Cattaneo, M.G.; Soriano, F.; et al. A novel standard protocol of long-term follow-up shared with general practitioners after percutaneous coronary intervention: Appropriateness and economic impact. G. Ital. Cardiol. 2015, 16, 565–573. [Google Scholar] [CrossRef]
- Sabouret, P.; Lemesle, G.; Bellemain-Appaix, A.; Aubry, P.; Bocchino, P.P.; Rafflenbeul, E.; Belle, L.; Nolan, J.; Bernardi, M.; Biondi-Zoccai, G.; et al. Post-discharge and long-term follow-up after an acute coronary syndrome: International Collaborative Group of CNCF position paper. Arch. Med. Sci. 2022, 18, 839–854. [Google Scholar] [CrossRef]
- Bencivenga, L.; Femminella, G.D.; Ambrosino, P.; Bosco, Q.; De Lucia, C.; Perrotta, G.; Formisano, R.; Komici, K.; Vitale, D.F.; Ferrara, N.; et al. Role of frailty on cardiac rehabilitation in hospitalized older patients. Aging Clin. Exp. Res. 2022, 34, 2675–2682. [Google Scholar] [CrossRef] [PubMed]
- Ibrahim, K.; Cox, N.J.; Stevenson, J.M.; Lim, S.; Fraser, S.D.S.; Roberts, H.C. A systematic review of the evidence for deprescribing interventions among older people living with frailty. BMC Geriatr. 2021, 21, 258. [Google Scholar] [CrossRef] [PubMed]
- Wang, H.; Zhao, T.; Wei, X.; Lu, H.; Lin, X. The prevalence of 30-day readmission after acute myocardial infarction: A systematic review and meta-analysis. Clin. Cardiol. 2019, 42, 889–898. [Google Scholar] [CrossRef] [PubMed]
- Ibanez, B.; James, S.; Agewall, S.; Antunes, M.J.; Bucciarelli-Ducci, C.; Bueno, H.; Caforio, A.L.P.; Crea, F.; Goudevenos, J.A.; Halvorsen, S.; et al. 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: The Task Force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC). Eur. Heart J. 2018, 39, 119–177. [Google Scholar] [CrossRef] [PubMed]
- Baldasseroni, S.; Silverii, M.V.; Pratesi, A.; Burgisser, C.; Orso, F.; Lucarelli, G.; Turrin, G.; Ungar, A.; Marchionni, N.; Fattirolli, F. Cardiac Rehabilitation in Advanced aGE after PCI for acute coronary syndromes: Predictors of exercise capacity improvement in the CR-AGE ACS study. Aging Clin. Exp. Res. 2022, 34, 2195–2203. [Google Scholar] [CrossRef] [PubMed]
- Salzwedel, A.; Jensen, K.; Rauch, B.; Doherty, P.; Metzendorf, M.I.; Hackbusch, M.; Voller, H.; Schmid, J.P.; Davos, C.H. Effectiveness of comprehensive cardiac rehabilitation in coronary artery disease patients treated according to contemporary evidence based medicine: Update of the Cardiac Rehabilitation Outcome Study (CROS-II). Eur. J. Prev. Cardiol. 2020, 27, 1756–1774. [Google Scholar] [CrossRef] [PubMed]
- Rauch, B.; Davos, C.H.; Doherty, P.; Saure, D.; Metzendorf, M.I.; Salzwedel, A.; Voller, H.; Jensen, K.; Schmid, J.P.; Cardiac Rehabilitation Section; et al. The prognostic effect of cardiac rehabilitation in the era of acute revascularisation and statin therapy: A systematic review and meta-analysis of randomized and non-randomized studies—The Cardiac Rehabilitation Outcome Study (CROS). Eur. J. Prev. Cardiol. 2016, 23, 1914–1939. [Google Scholar] [CrossRef] [PubMed]
- Khan, Z.; Musa, K.; Abumedian, M.; Ibekwe, M. Prevalence of Depression in Patients With Post-Acute Coronary Syndrome and the Role of Cardiac Rehabilitation in Reducing the Risk of Depression: A Systematic Review. Cureus 2021, 13, e20851. [Google Scholar] [CrossRef] [PubMed]
- Silverii, M.V.; Pratesi, A.; Lucarelli, G.; Fattirolli, F. Cardiac rehabilitation protocols in the elderly. Monaldi Arch. Chest Dis. 2020, 90, 1253. [Google Scholar] [CrossRef] [PubMed]
- Zhao, E.; Lowres, N.; Woolaston, A.; Naismith, S.L.; Gallagher, R. Prevalence and patterns of cognitive impairment in acute coronary syndrome patients: A systematic review. Eur. J. Prev. Cardiol. 2020, 27, 284–293. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Babazono, A.; Jamal, A.; Liu, N.; Yamao, R. Population-Based Multilevel Models to Estimate the Management Strategies for Acute Myocardial Infarction in Older Adults with Dementia. Clin. Epidemiol. 2021, 13, 883–892. [Google Scholar] [CrossRef] [PubMed]
- Lovell, J.; Pham, T.; Noaman, S.Q.; Davis, M.C.; Johnson, M.; Ibrahim, J.E. Self-management of heart failure in dementia and cognitive impairment: A systematic review. BMC Cardiovasc. Disord. 2019, 19, 99. [Google Scholar] [CrossRef] [PubMed]
- Tegn, N.; Abdelnoor, M.; Aaberge, L.; Endresen, K.; Smith, P.; Aakhus, S.; Gjertsen, E.; Dahl-Hofseth, O.; Ranhoff, A.H.; Gullestad, L.; et al. Invasive versus conservative strategy in patients aged 80 years or older with non-ST-elevation myocardial infarction or unstable angina pectoris (After Eighty study): An open-label randomised controlled trial. Lancet 2016, 387, 1057–1065. [Google Scholar] [CrossRef] [PubMed]
- Kaura, A.; Sterne, J.A.C.; Trickey, A.; Abbott, S.; Mulla, A.; Glampson, B.; Panoulas, V.; Davies, J.; Woods, K.; Omigie, J.; et al. Invasive versus non-invasive management of older patients with non-ST elevation myocardial infarction (SENIOR-NSTEMI): A cohort study based on routine clinical data. Lancet 2020, 396, 623–634. [Google Scholar] [CrossRef] [PubMed]
- Savonitto, S.; Cavallini, C.; Petronio, A.S.; Murena, E.; Antonicelli, R.; Sacco, A.; Steffenino, G.; Bonechi, F.; Mossuti, E.; Manari, A.; et al. Early aggressive versus initially conservative treatment in elderly patients with non-ST-segment elevation acute coronary syndrome: A randomized controlled trial. JACC Cardiovasc. Interv. 2012, 5, 906–916. [Google Scholar] [CrossRef] [PubMed]
- Sanchis, J.; Nunez, E.; Barrabes, J.A.; Marin, F.; Consuegra-Sanchez, L.; Ventura, S.; Valero, E.; Roque, M.; Bayes-Genis, A.; Del Blanco, B.G.; et al. Randomized comparison between the invasive and conservative strategies in comorbid elderly patients with non-ST elevation myocardial infarction. Eur. J. Intern. Med. 2016, 35, 89–94. [Google Scholar] [CrossRef] [PubMed]
- Hirlekar, G.; Libungan, B.; Karlsson, T.; Back, M.; Herlitz, J.; Albertsson, P. Percutaneous coronary intervention in the very elderly with NSTE-ACS: The randomized 80+ study. Scand. Cardiovasc. J 2020, 54, 315–321. [Google Scholar] [CrossRef] [PubMed]
- de Belder, A.; Myat, A.; Blaxill, J.; Haworth, P.; O’Kane, P.D.; Hatrick, R.; Aggarwal, R.K.; Davie, A.; Smith, W.; Gerber, R.; et al. Revascularisation or medical therapy in elderly patients with acute anginal syndromes: The RINCAL randomised trial. EuroIntervention 2021, 17, 67–74. [Google Scholar] [CrossRef] [PubMed]
- Sanchis, J.; Ariza-Sole, A.; Abu-Assi, E.; Alegre, O.; Alfonso, F.; Barrabes, J.A.; Baz, J.A.; Carol, A.; Diez Villanueva, P.; Garcia Del Blanco, B.; et al. Invasive Versus Conservative Strategy in Frail Patients With NSTEMI: The MOSCA-FRAIL Clinical Trial Study Design. Rev. Esp. Cardiol. (Engl. Ed.) 2019, 72, 154–159. [Google Scholar] [CrossRef]
- Khoong, E.C.; Olazo, K.; Rivadeneira, N.A.; Thatipelli, S.; Barr-Walker, J.; Fontil, V.; Lyles, C.R.; Sarkar, U. Mobile health strategies for blood pressure self-management in urban populations with digital barriers: Systematic review and meta-analyses. NPJ Digit. Med. 2021, 4, 114. [Google Scholar] [CrossRef]
- Molinari, G.; Molinari, M.; Di Biase, M.; Brunetti, N.D. Telecardiology and its settings of application: An update. J. Telemed. Telecare 2018, 24, 373–381. [Google Scholar] [CrossRef] [PubMed]
- Brunetti, N.D.; De Gennaro, L.; Amodio, G.; Dellegrottaglie, G.; Pellegrino, P.L.; Di Biase, M.; Antonelli, G. Telecardiology improves quality of diagnosis and reduces delay to treatment in elderly patients with acute myocardial infarction and atypical presentation. Eur. J. Cardiovasc. Prev. Rehabil. 2010, 17, 615–620. [Google Scholar] [CrossRef] [PubMed]
- Kirakalaprathapan, A.; Oremus, M. Efficacy of telehealth in integrated chronic disease management for older, multimorbid adults with heart failure: A systematic review. Int. J. Med. Inform. 2022, 162, 104756. [Google Scholar] [CrossRef] [PubMed]
- Doraiswamy, S.; Abraham, A.; Mamtani, R.; Cheema, S. Use of Telehealth During the COVID-19 Pandemic: Scoping Review. J. Med. Internet Res. 2020, 22, e24087. [Google Scholar] [CrossRef]
- Goldberg, E.M.; Lin, M.P.; Burke, L.G.; Jimenez, F.N.; Davoodi, N.M.; Merchant, R.C. Perspectives on Telehealth for older adults during the COVID-19 pandemic using the quadruple aim: Interviews with 48 physicians. BMC Geriatr. 2022, 22, 188. [Google Scholar] [CrossRef] [PubMed]
- Inzitari, M.; Arnal, C.; Ribera, A.; Hendry, A.; Cesari, M.; Roca, S.; Perez, L.M. Comprehensive Geriatric Hospital at Home: Adaptation to Referral and Case-Mix Changes During the COVID-19 Pandemic. J. Am. Med. Dir. Assoc. 2023, 24, 3–9.e1. [Google Scholar] [CrossRef] [PubMed]
- Arsenault-Lapierre, G.; Henein, M.; Gaid, D.; Le Berre, M.; Gore, G.; Vedel, I. Hospital-at-Home Interventions vs In-Hospital Stay for Patients With Chronic Disease Who Present to the Emergency Department: A Systematic Review and Meta-analysis. JAMA Netw. Open 2021, 4, e2111568. [Google Scholar] [CrossRef] [PubMed]
- Calsolaro, V.; Antognoli, R.; Pasqualetti, G.; Okoye, C.; Aquilini, F.; Cristofano, M.; Briani, S.; Monzani, F. 30-Day Potentially Preventable Hospital Readmissions In Older Patients: Clinical Phenotype And Health Care Related Risk Factors. Clin. Interv. Aging 2019, 14, 1851–1858. [Google Scholar] [CrossRef] [PubMed]
- Pirhonen, L.; Bolin, K.; Olofsson, E.H.; Fors, A.; Ekman, I.; Swedberg, K.; Gyllensten, H. Person-Centred Care in Patients with Acute Coronary Syndrome: Cost-Effectiveness Analysis Alongside a Randomised Controlled Trial. PharmacoEconomics-open 2019, 3, 495–504. [Google Scholar] [CrossRef] [PubMed]
- Pardo, Y.; Garin, O.; Oriol, C.; Zamora, V.; Ribera, A.; Ferrer, M. Patient-centered care in Coronary Heart Disease: What do you want to measure? A systematic review of reviews on patient-reported outcome measures. Qual. Life Res. 2023, 32, 1405–1425. [Google Scholar] [CrossRef] [PubMed]

Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cacciatore, S.; Spadafora, L.; Bernardi, M.; Galli, M.; Betti, M.; Perone, F.; Nicolaio, G.; Marzetti, E.; Martone, A.M.; Landi, F.; et al. Management of Coronary Artery Disease in Older Adults: Recent Advances and Gaps in Evidence. J. Clin. Med. 2023, 12, 5233. https://doi.org/10.3390/jcm12165233
Cacciatore S, Spadafora L, Bernardi M, Galli M, Betti M, Perone F, Nicolaio G, Marzetti E, Martone AM, Landi F, et al. Management of Coronary Artery Disease in Older Adults: Recent Advances and Gaps in Evidence. Journal of Clinical Medicine. 2023; 12(16):5233. https://doi.org/10.3390/jcm12165233
Chicago/Turabian StyleCacciatore, Stefano, Luigi Spadafora, Marco Bernardi, Mattia Galli, Matteo Betti, Francesco Perone, Giulia Nicolaio, Emanuele Marzetti, Anna Maria Martone, Francesco Landi, and et al. 2023. "Management of Coronary Artery Disease in Older Adults: Recent Advances and Gaps in Evidence" Journal of Clinical Medicine 12, no. 16: 5233. https://doi.org/10.3390/jcm12165233
APA StyleCacciatore, S., Spadafora, L., Bernardi, M., Galli, M., Betti, M., Perone, F., Nicolaio, G., Marzetti, E., Martone, A. M., Landi, F., Asher, E., Banach, M., Hanon, O., Biondi-Zoccai, G., & Sabouret, P. (2023). Management of Coronary Artery Disease in Older Adults: Recent Advances and Gaps in Evidence. Journal of Clinical Medicine, 12(16), 5233. https://doi.org/10.3390/jcm12165233











