Trauma Patient Volume and the Quality of Care: A Scoping Review
Abstract
1. Introduction
1.1. Healthcare Challenges
1.2. Trauma Patient Volume and Quality of Healthcare
- Effective—providing evidence-based healthcare services to those who need them;
- Safe—avoiding harm to people for whom the care is intended; and
- People-centered—providing care that responds to individual preferences, needs and values.
- Timely—reducing waiting times and sometimes harmful delays;
- Equitable—providing care that does not vary in quality on account of gender, ethnicity, geographic location, and socio-economic status;
- Integrated—providing care that makes available the full range of health services throughout the life course;
- Efficient—maximizing the benefit of available resources and avoiding waste.”
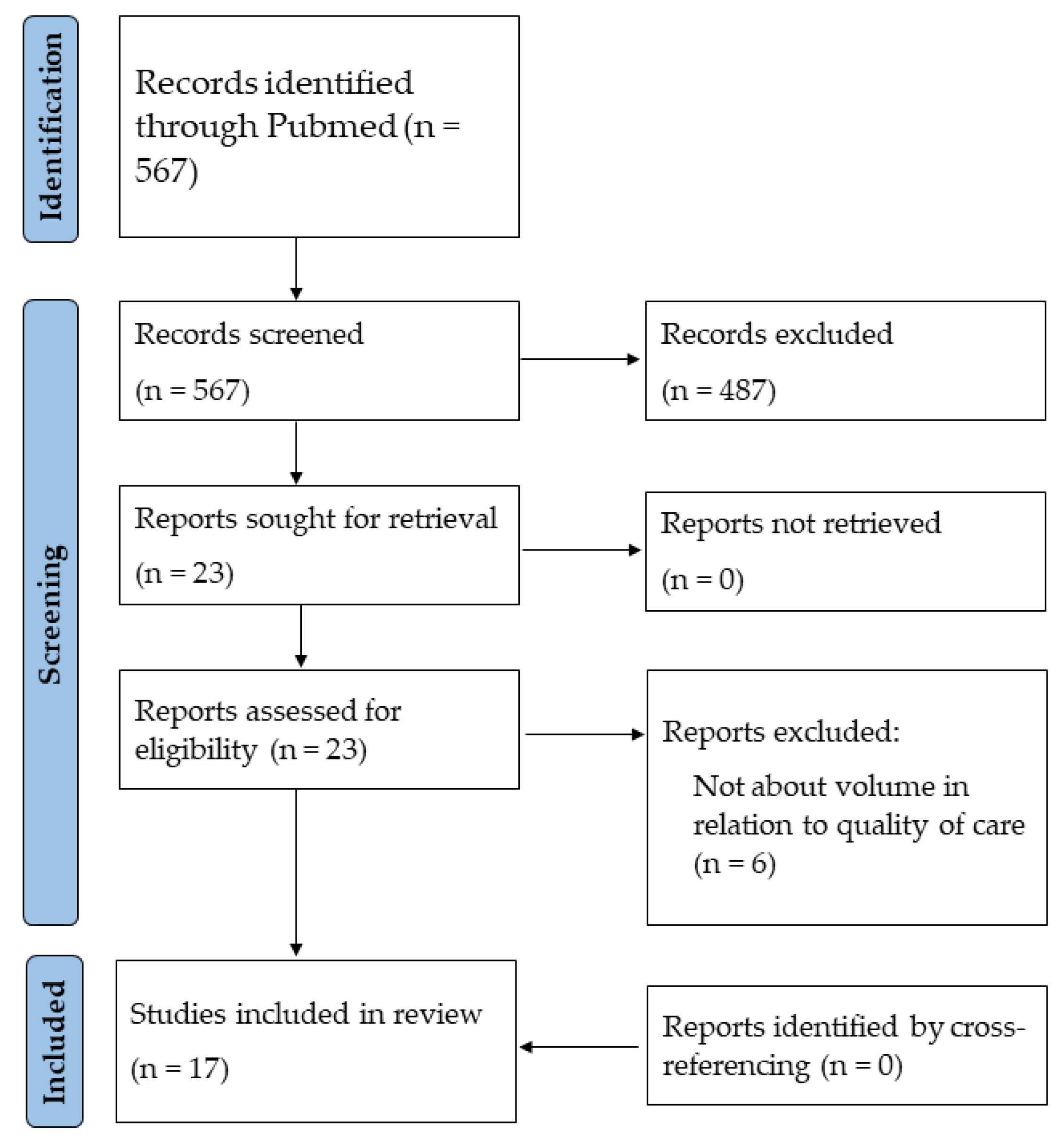
2. Materials and Methods
2.1. Literature Search
2.2. Study Selection
2.3. Data Extraction and Data Analysis
3. Results
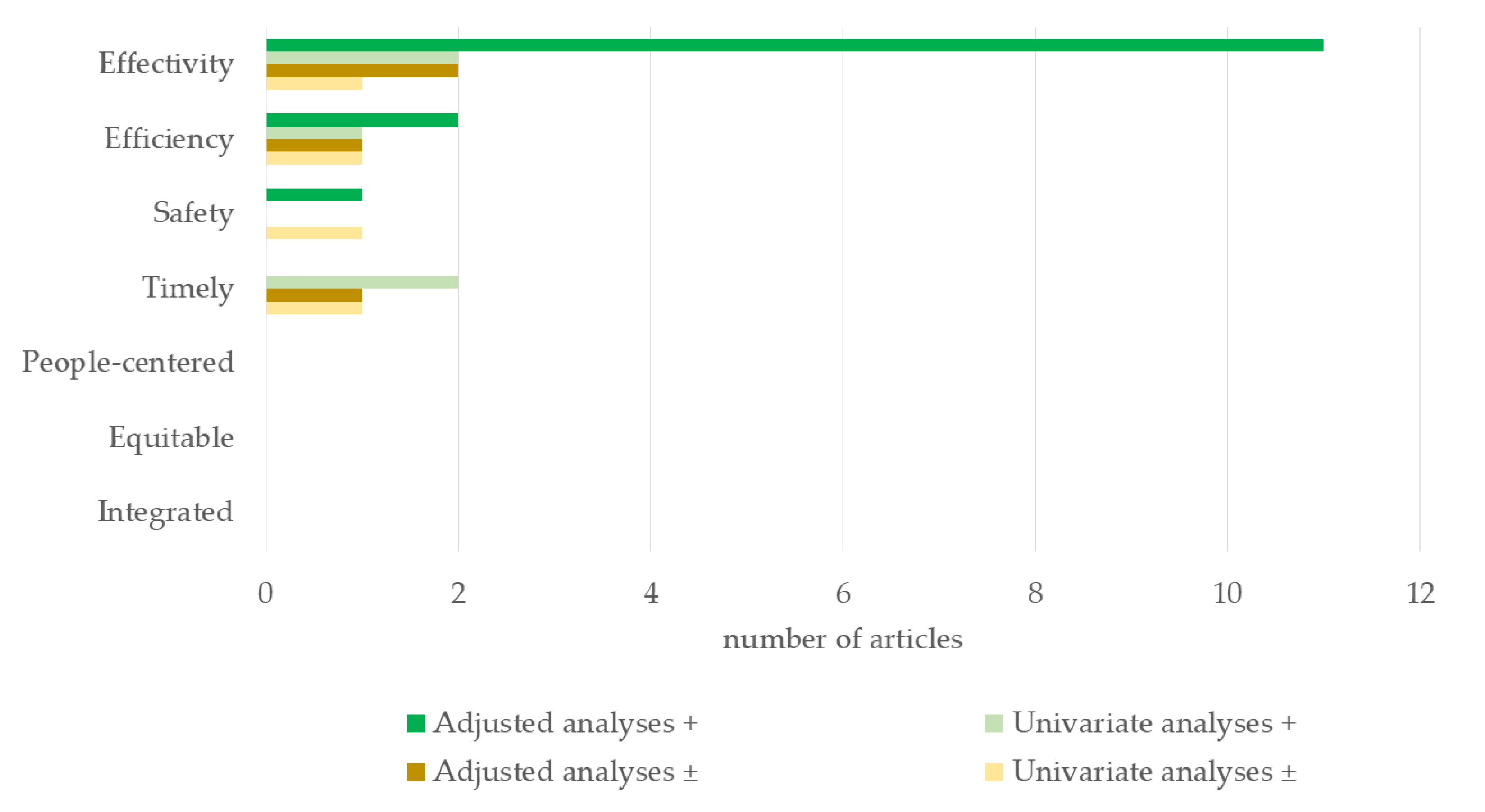
3.1. Effectivity
3.2. Efficiency
3.3. Safety
3.4. Timeliness
3.5. People-Centred, Equitable, and Integrated Qualities
4. Discussion
4.1. Summary of Evidence
4.2. Strengths and Limitations
4.3. Implications and Next Steps for Trauma Care in the Netherlands
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Hietbrink, F.; Houwert, R.M.; van Wessem, K.J.P.; Simmermacher, R.K.J.; Govaert, G.A.M.; de Jong, M.B.; de Bruin, I.G.J.; de Graaf, J.; Leenen, L.P.H. The Evolution of Trauma Care in the Netherlands over 20 Years. Eur. J. Trauma Emerg. Surg. 2020, 46, 329–335. [Google Scholar] [CrossRef]
- Landelijk Netwerk Acute Zorg. Landelijke Traumaregistratie 2016–2020. Available online: https://www.lnaz.nl/trauma/landelijke-traumaregistratie (accessed on 26 September 2022).
- Wetenschappelijke Raad Voor Het Regeringsbeleid, Den Haag, Kiezen Voor Houdbare Zorg, Mensen, Middelen en Maat Schappelijk Draagvlak. Available online: https://www.wrr.nl/adviesprojecten/houdbare-zorg/documenten/rapporten/2021/09/15/kiezen-voor-houdbare-zorg (accessed on 28 April 2023).
- Ministerie van Volksgezondheid Welzijn en Sport. Integraal Zorg Akkoord–Samen Werken Aan Gezonde Zorg. 2022. Available online: https://www.rijksoverheid.nl/documenten/rapporten/2022/09/16/integraal-zorgakkoord-samen-werken-aan-gezonde-zorg (accessed on 26 September 2022).
- American College of Surgeons; Committee on Trauma. Resources for Optimal Care of the Injured Patient; American College of Surgeons, Committee on Trauma: San Antonio, TX, USA, 2014; ISBN 9780984669981. [Google Scholar]
- World Health Organization Quality of Care. Available online: https://www.who.int/health-topics/quality-of-care#tab=tab_1 (accessed on 12 April 2023).
- Sewalt, C.; Wiegers, E.; Venema, E.; Lecky, F.; Schuit, S.; Den Hartog, D.; Lingsma, H. The Volume-Outcome Relationship in Severely Injured Patients: A Systematic Review and Meta-Analysis. J. Trauma Acute Care Surg. 2018, 85, 810–819. [Google Scholar] [CrossRef] [PubMed]
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.J.; Horsley, T.; Weeks, L.; et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann. Intern. Med. 2018, 169, 467–473. [Google Scholar] [CrossRef] [PubMed]
- Sanderson, S.; Tatt, I.D.; Higgins, J.P.T. Tools for Assessing Quality and Susceptibility to Bias in Observational Studies in Epidemiology: A Systematic Review and Annotated Bibliography. Int. J. Epidemiol. 2007, 36, 666–676. [Google Scholar] [CrossRef]
- Clement, R.C.; Carr, B.G.; Kallan, M.J.; Wolff, C.; Reilly, P.M.; Malhotra, N.R. Volume-Outcome Relationship in Neurotrauma Care. J. Neurosurg. 2013, 118, 687–693. [Google Scholar] [CrossRef] [PubMed]
- Matsushima, K.; Schaefer, E.W.; Won, E.J.; Armen, S.B.; Indeck, M.C.; Soybel, D.I. Positive and Negative Volume-Outcome Relationships in the Geriatric Trauma Population. JAMA Surg. 2014, 149, 319–326. [Google Scholar] [CrossRef] [PubMed]
- Zacher, M.T.; Kanz, K.G.; Hanschen, M.; Häberle, S.; Van Griensven, M.; Lefering, R.; Bühren, V.; Biberthaler, P.; Huber-Wagner, S. Association between Volume of Severely Injured Patients and Mortality in German Trauma Hospitals. Br. J. Surg. 2015, 102, 1213–1219. [Google Scholar] [CrossRef]
- Olufajo, O.A.; Metcalfe, D.; Rios-Diaz, A.; Lilley, E.; Havens, J.M.; Kelly, E.; Weissman, J.S.; Haider, A.H.; Salim, A.; Cooper, Z. Does Hospital Experience Rather than Volume Improve Outcomes in Geriatric Trauma Patients? J. Am. Coll. Surg. 2016, 223, 32–40.e1. [Google Scholar] [CrossRef]
- Brown, J.B.; Rosengart, M.R.; Kahn, J.M.; Mohan, D.; Zuckerbraun, B.S.; Billiar, T.R.; Peitzman, A.B.; Angus, D.C.; Sperry, J.L. Impact of Volume Change over Time on Trauma Mortality in the United States. Ann. Surg. 2017, 266, 173–178. [Google Scholar] [CrossRef]
- Endo, A.; Shiraishi, A.; Fushimi, K.; Murata, K.; Otomo, Y. Increased Severe Trauma Patient Volume Is Associated with Survival Benefit and Reduced Total Health Care Costs: A Retrospective Observational Study Using a Japanese Nationwide Administrative Database. Ann. Surg. 2017, 268, 1091–1096. [Google Scholar] [CrossRef]
- Miyata, S.; Cho, J.; Park, H.; Matsushima, K.; Bliss, D.W. Comparison of Outcomes in Severe Pediatric Trauma at Adult Trauma Centers with Different Trauma Case Volumes. J. Pediatr. Surg. 2017, 52, 1831–1835. [Google Scholar] [CrossRef] [PubMed]
- Nakahara, S.; Sakamoto, T.; Fujita, T.; Uchida, Y.; Katayama, Y.; Tanabe, S.; Yamamoto, Y. Evaluating Quality Indicators of Tertiary Care Hospitals for Trauma Care in Japan. Int. J. Qual. Health Care 2017, 29, 1006–1013. [Google Scholar] [CrossRef] [PubMed]
- Wada, T.; Yasunaga, H.; Doi, K.; Matsui, H.; Fushimi, K.; Kitsuta, Y.; Nakajima, S. Impact of Hospital Volume on Mortality in Patients with Severe Torso Injury. J. Surg. Res. 2018, 222, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Fu, C.Y.; Bajani, F.; Tatebe, L.; Butler, C.; Starr, F.; Dennis, A.; Kaminsky, M.; Messer, T.; Schlanser, V.; Kramer, K.; et al. Right Hospital, Right Patients: Penetrating Injury Patients Treated at High-Volume Penetrating Trauma Centers Have Lower Mortality. J. Trauma Acute Care Surg. 2019, 86, 961–966. [Google Scholar] [CrossRef] [PubMed]
- Sewalt, C.A.; Wiegers, E.J.A.; Lecky, F.E.; Den Hartog, D.; Schuit, S.C.E.; Venema, E.; Lingsma, H.F. The Volume-Outcome Relationship among Severely Injured Patients Admitted to English Major Trauma Centres: A Registry Study. Scand. J. Trauma Resusc. Emerg. Med. 2020, 28, 18. [Google Scholar] [CrossRef]
- Aoki, M.; Abe, T.; Saitoh, D.; Hagiwara, S.; Oshima, K. Severe Trauma Patient Volume Was Associated with Decreased Mortality. Eur. J. Trauma Emerg. Surg. 2021, 47, 1957–1964. [Google Scholar] [CrossRef]
- Sewalt, C.A.; Venema, E.; van Zwet, E.; van Ditshuizen, J.C.; Schuit, S.C.E.; Polinder, S.; Lingsma, H.F.; Den Hartog, D. The Relationship between Hospital Volume and In-Hospital Mortality of Severely Injured Patients in Dutch Level-1 Trauma Centers. J. Clin. Med. 2021, 10, 1700. [Google Scholar] [CrossRef]
- Tang, A.; Chehab, M.; Ditillo, M.; Asmar, S.; Khurrum, M.; Douglas, M.; Bible, L.; Kulvatunyou, N.; Joseph, B. Regionalization of Trauma Care by Operative Experience: Does the Volume of Emergent Laparotomy Matter? J. Trauma Acute Care Surg. 2021, 90, 11–20. [Google Scholar] [CrossRef]
- Toida, C.; Muguruma, T.; Gakumazawa, M.; Shinohara, M.; Abe, T.; Takeuchi, I.; Morimura, N. Correlation between Hospital Volume of Severely Injured Patients and In-Hospital Mortality of Severely Injured Pediatric Patients in Japan: A Nationwide 5-Year Retrospective Study. J. Clin. Med. 2021, 10, 1422. [Google Scholar] [CrossRef]
- Floan, G.M.; Calvo, R.Y.; Prieto, J.M.; Krzyzaniak, A.; Patwardhan, U.; Checchi, K.D.; Beth Sise, C.; Sise, M.J.; Bansal, V.; Ignacio, R.C.; et al. Pediatric Penetrating Thoracic Trauma: Examining the Impact of Trauma Center Designation and Penetrating Trauma Volume on Outcomes. J. Pediatr. Surg. 2022, 58, 330–336. [Google Scholar] [CrossRef]
- Lefering, R.; Waydhas, C. Process Times of Severely Injured Patients in the Emergency Room Are Associated with Patient Volume: A Registry-Based Analysis. Eur. J. Trauma Emerg. Surg. 2022, 48, 4615–4622. [Google Scholar] [CrossRef] [PubMed]
- Caputo, L.M.; Salottolo, K.M.; Slone, D.S.; Mains, C.W.; Bar-Or, D. The Relationship between Patient Volume and Mortality in American Trauma Centres: A Systematic Review of the Evidence. Injury 2014, 45, 478–486. [Google Scholar] [CrossRef] [PubMed]
- Van Kempen, J. Traumacentrum VUmc Officieel over Naar Locatie AMC. Available online: https://www.parool.nl/amsterdam/traumacentrum-vumc-officieel-over-naar-locatie-amc~b5fd7b47/?referrer=https%3A%2F%2Fwww.google.com%2F (accessed on 17 April 2023).
- Baltesen, F. Level 1-Traumazorg HagaZiekenhuis Gaat Naar HMC. Available online: https://www.skipr.nl/nieuws/hagaziekenhuis-stopt-met-traumacentrum-level1-zorg-naar-hmc/ (accessed on 17 April 2023).
- Sturms, L.M.; Driessen, M.L.S.; Van Klaveren, D.; Jan, H.; Kommer, G.J.; Bloemers, F.W.; Den Hartog, D.; Edwards, M.J.; Leenhouts, P.A.; Van Zutphen, S.; et al. Dutch Trauma System Performance: Are Injured Patients Treated at the Right Place? Injury 2021, 52, 1688–1696. [Google Scholar] [CrossRef]
- Van Rein, E.A.J.; Van Der Sluijs, R.; Voskens, F.J.; Lansink, K.W.W.; Houwert, R.M.; Lichtveld, R.A.; De Jongh, M.A.; Dijkgraaf, M.G.W.; Champion, H.R.; Beeres, F.J.P.; et al. Development and Validation of a Prediction Model for Prehospital Triage of Trauma Patients. JAMA Surg. 2019, 154, 421–429. [Google Scholar] [CrossRef] [PubMed]
- Van der Sluijs, R.; Fiddelers, A.A.A.; Waalwijk, J.F.; Reitsma, J.B.; Dirx, M.J.; den Hartog, D.; Evers, S.M.A.A.; Goslings, J.C.; Hoogeveen, W.M.; Lansink, K.W.; et al. The Impact of the Trauma Triage App on Pre-Hospital Trauma Triage: Design and Protocol of the Stepped-Wedge, Cluster-Randomized TESLA Trial. Diagn. Progn. Res. 2020, 4, 10. [Google Scholar] [CrossRef]
- Lokerman, R.D.; van Rein, E.A.J.; Waalwijk, J.F.; van der Sluijs, R.; Houwert, R.M.; Lansink, K.W.W.; Edwards, M.J.R.; van Vliet, R.; Verhagen, T.F.; Diets-Veenendaal, N.; et al. Accuracy of Prehospital Triage of Adult Patients With Traumatic Injuries Following Implementation of a Trauma Triage Intervention. JAMA Netw. Open 2023, 6, e236805. [Google Scholar] [CrossRef]
| PubMed | |
|---|---|
| 1. | (Advanced Trauma Life Support Care[MeSH Terms] OR Multiple Trauma[MeSH Terms] OR polytrauma[Title/Abstract] OR multitrauma[Title/Abstract] OR trauma care[Title/Abstract] OR trauma patient[Title/Abstract] OR trauma victim[Title/Abstract] OR severely injured[Title/Abstract]) |
| 2. | (Centralized hospital service[MeSH Terms] OR centralized[Title/Abstract] OR decentralized[Title/Abstract] OR centralization[Title/Abstract] OR volume[Title/Abstract]) |
| 3. | (y_10[Filter]) |
| 4. | 1 AND 2 AND 3 |
| Study | Design | Country | Sample Size (N) | Population | Age (Years) | Volume Definition |
|---|---|---|---|---|---|---|
| Clement et al., 2013 [10] | Retrospective, multicenter (Nationwide Inpatient Sample 2006) | United States | 12,493 | Patients with neurological trauma (ICD-9 codes for subarachnoid, subdural, and extradural hematoma) | Range: 15–85+ | Categories: <6 [reference], 6–11, 12–23, 24–59, and 60+ annual patients with neurological trauma |
| Matsushima et al., 2014 [11] | Retrospective, multicenter (Statewide trauma registry 2001–2010) | United States | 39,431 | Geriatric trauma patients, median ISS = 13; 43% with ISS > 15 | Median 80 (range: 66–114) | Analyses for 100-patient increase in annual volume |
| Zacher et al., 2015 [12] | Retrospective, multicenter (TraumaRegister DGU 2009–2013) | Germany | 39,289 | Severe trauma patients with ISS > 15, mean ISS = 27 (sd ± 12) | Mean: 50 (sd ± 22) | Continuous |
| Olufajo et al., 2016 [13] | Retrospective, multicenter (California State Inpatient Database 2007–2011) | United States | 61,915 | Geriatric trauma patients >65 years | 65–84: 67% >85: 33% | Analyses for 100-patient increase in annual volume |
| Brown et al., 2017 [14] | Retrospective, multicenter (National trauma data bank 2000–2012) | United States | 839,809 | Severe trauma patients with ISS > 15 | Median: 41 (IQR 23–60) | Categories based on median: ≤247, >247 annual severe trauma patients |
| Endo et al., 2017 [15] | Retrospective, multicenter (National trauma data bank 2010–2015) | Japan | 116,329 | Severe trauma patients ≥16 years (ICD-10 based trauma severity scoring system) | Median: 67–75 | Categories: 1–50 [reference], 51–100, 101–150, 151–200, and >200 annual severe trauma patients ≥16 years |
| Miyata et al., 2017 [16] | Retrospective, multicenter (National trauma data bank 2007–2014) | United States | 3747 | Severely injured pediatric patients with ISS > 15 treated at adult trauma centers | 10–15: 64% | Quartiles: 8–93 [reference], 94–179, 180–265, and 266–352 annual severe pediatric trauma patients |
| Nakahara et al., 2017 [17] | Retrospective, multicenter (National trauma data bank 2012–2013) | Japan | 12,378 | Blunt trauma patients ≥15 years and ISS ≥ 9 (49.9% ISS > 15) | Categories: 15–24: 10% 25–44: 16% 45–64: 24% ≥65: 50% | Quartiles: ≤124 [reference], 125–178, 179–312, and ≥313 annual blunt trauma patients ≥15 years and ISS ≥ 9 |
| Wada et al., 2018 [18] | Retrospective, multicenter (National trauma data bank 2010–2014) | Japan | 7725 | Severe torso injury patients with emergency surgery or interventional radiology treatment | Median 58–61 | Quartiles: ≤8 [reference], 8- ≤ 13, 13- ≤ 20, and >20 annual trauma patients with ISS > 15 |
| Fu et al., 2019 [19] | Retrospective, multicenter (National trauma data bank 2011–2015) | United States | 55,696 | Penetrating injury patients; 18% with ISS > 15 | Mean 33–35 | Quartiles: ≤37 (bottom 25%) [reference] vs. ≥167 (top 25%) annual penetrating injury patients |
| Sewalt et al., 2020 [20] | Retrospective, multicenter (National trauma data bank 2013–2016) | England and Wales | 47,159 | All trauma patients with ISS > 15 in major trauma center | Median 53 (IQR 32–74) | Tertiles: ≤163, 164–191, and >191 annual trauma patients with an ISS > 15 |
| Aoki et al., 2021 [21] | Retrospective, multicenter (National trauma data bank 2004–2015) | Japan | 74,957 | Severe trauma patients with ISS > 15 | Median: 60 (IQR 38–74) | Categories: LV 1–49, MV 50–99, and HV ≥ 100 annual trauma patients with ISS > 15 |
| Sewalt et al., 2021 [22] | Retrospective, multicenter (Dutch Trauma registry 2015–2018) | The Netherlands | 11,917 | Severe adult trauma patients with ISS > 15 admitted to a MTC | LV: median 58 (IQR 35–74) HV: median 53 (IQR 30–69) | Analyses for 50-patient increase in annual volume |
| Tang et al., 2021 [23] | Retrospective, multicenter (Trauma Quality Improvement Program database 2017) | United States | 8588 | Blunt and penetrating trauma patients with emergent laparotomies < 24 h for hemorrhage control | Blunt, penetrating: 18–44: 52%, 79% 45–64: 32%, 18% ≥65: 16%, 3% | Categories: LV ≤ 12, MV 13–24, and HV ≥ 25 annual emergent laparotomies for hemorrhage control |
| Toida et al., 2021 [24] | Retrospective, multicenter (National trauma data bank 2014–2018) | Japan | 53,088 | Severe trauma patients with ISS >15 | Range 0–65+ | Categories: LV < 150 annual trauma patients with ISS > 15, and HV ≥ 150 |
| Floan et al., 2022 [25] | Retrospective, multicenter (National trauma data bank 2013–2016) | United States | 4134 | Pediatric penetrating thoracic trauma | Mean 15 (sd ± 3.5) | Continuous |
| Lefering et al., 2022 [26] | Retrospective, multicenter (Trauma-Register DGU 2013–2017) | Germany | 129,193 | Trauma patients, mean ISS 18 (sd ± 12), 50% with ISS > 15 | Mean 51 (sd ± 22) | Categories: 1–9, 10–19, 20–39, 40–99, 100+ annual trauma patients |
| Study | Nationwide (Sample) | Type of Hospitals Reported | Time Period Reported | Eligibility Criteria Reported | Volume Definitions Reported | N Severely Injured Patients Reported | Reported Quality Aspect of Healthcare | Volume-Outcome: Odds Ratio or Absolute Values | 95%CI or p-Value Reported | Analyses Adjusted for Patient Demographics | Analyses Adjusted for Injury Severity | Analyses Adjusted for Trauma-Center Level | Funding Sources Reported or No Conflicts of Interest |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Clement et al., 2013 [10] | + | + | + | + | + | − | Effectivity Efficiency | + + | + + | + + | + + | − − | + |
| Matsushima et al., 2014 [11] | − | + | + | + | + | + | Effectivity Safety | + + | + + | + + | + + | − − | + |
| Zacher et al., 2015 [12] | + | + | + | + | + | + | Effectivity | + | + | + * | + * | + | + |
| Olufajo et al., 2016 [13] | − | + | + | + | + | + | Effectivity Efficiency | + + | + + | + + | + + | + + | + |
| Brown et al., 2017 [14] | + | − | + | + | + | + | Effectivity | + | + | ~ 1 | ~ 1 | − | + |
| Endo et al., 2017 [15] | + | + | + | + | + | + | Effectivity Efficiency | + + | + + | − − | + + | − − | + |
| Miyata et al., 2017 [16] | + | + | + | + | + | + | Effectivity | + | + | + | + | + | − |
| Nakahara et al., 2017 [17] | + | + | + | + | + | + | Effectivity | + | + | + | + | − | + |
| Wada et al., 2018 [18] | + | + | + | + | + | + | Effectivity | + | + | + | + | − | + |
| Fu et al., 2019 [19] | + | + | + | + | + | + | Effectivity | + | + | + | + | − | + |
| Sewalt et al., 2020 [20] | + | + | + | + | + | + | Effectivity Efficiency Timely | + + + | + + + | + + + | + + + | NA NA NA | + |
| Aoki et al., 2021 [21] | + | − | + | + | + | + | Effectivity Timely | + + | + + | + − | + − | − − | + |
| Sewalt et al., 2021 [22] | + | + | + | + | + | + | Effectivity | + | + | + | + | NA | + |
| Tang et al., 2021 [23] | + | + | + | + | + | + | Effectivity Efficiency Safety Timely | + + + + | + + + + | + − − − | + − − − | + − − − | + |
| Toida et al., 2021 [24] | + | + | + | + | + | + | Effectivity | + | + | − | − | − | + |
| Floan et al., 2022 [25] | + | + | + | + | + | − | Effectivity | − | + | − | ~ 2 | − | + |
| Lefering et al., 2022 [26] | + | − | + | + | + | + | Timely | + | − | − | − | − | + |
| Study | Outcome (Adjusted) | |
|---|---|---|
| United States | ||
| Clement et al., 2013 [10] | Hospitals with 6+ cases/year with subarachnoid, subdural, and extradural hematomas had significant lower mortality rates compared to hospitals with <6 annual cases (adjusted ORs range 0.45–0.63). Adjusted for, e.g., age, sex, geographical region, hospital characteristics, comorbidities, other severe head trauma, neurosurgical procedures performed, significant non-neurological injury, and severity of intracranial hemorrhage | + |
| Matsushima et al., 2014 [11] | Larger institutional volume of geriatric trauma cases was significantly associated with lower in-hospital mortality (adjusted OR 0.75 for a 100-patient increase; CI 0.61–0.92). Adjusted for patient characteristics, injury severity, and preexisting conditions | + |
| Olufajo et al., 2016 [13] | Significant decrease in hospital mortality per 100 increase in geriatric trauma patients with ISS > 15 (adjusted OR 0.89; CI 0.82–0.97). Adjusted for patient demographic, injury, admission, and hospital characteristics | + |
| Miyata et al., 2017 [16] | Highest volume group was associated with lower mortality compared to the lowest quartile volume center (adjusted OR 0.47; CI 0.30–0.75; p < 0.01). For level 1 trauma centers specifically, the highest volume group was associated with lower mortality compared to the lowest quartile volume center (adjusted OR 0.50; CI 0.31–0.79; p < 0.01). Adjusted for trauma center characteristics and patient characteristics (e.g., age, injury severity) | + |
| Fu et al., 2019 [19] | Significant increase in survival per 10 increase in penetrating injury patients (adjusted OR 1.01, p = 0.03). Adjusted for age, pulse, systolic blood pressure, ventilation, ISS and total number of trauma patients | + |
| Tang et al., 2021 [23] | Lower odds of in-hospital mortality in HV centers for blunt injury patients (adjusted OR 0.74; CI 0.59–0.93; p = 0.011) and penetrating injury patients (adjusted 0.86; CI 0.77–0.96; p = 0.023) with emergent laparotomies < 24 h for hemorrhage control. Adjusted for age, sex, comorbidities, systolic blood pressure, GCS, prehospital cardiac arrest, ISS, trauma center level, and injury-specific center laparotomy volume | + |
| Japan | ||
| Endo et al., 2017 [15] | Severe trauma patient volume was significantly associated with higher in-hospital survival for each 50-patient increase (adjusted OR 1.16; CI 1.12–1.21). Adjusted for trauma severity and hospital characteristics | + |
| Nakahara et al., 2017 [17] | Higher patient volume was significantly associated with lower 30-day mortality risk (HR for the highest vs. lowest quartile (adjusted OR 0.74; CI 0.56–0.98). Adjusted for age, gender, GCS, blood pressure, respiratory rate, and ISS | + |
| Wada et al., 2018 [18] | Hospitals with >20 patients with severe torso injuries had a significant lower 1-d mortality (adjusted OR 0.64; CI 0.43–0.96) and 28-d mortality (adjusted OR 0.59; CI 0.44–0.79) compared to hospitals with <8 patients with severe torso injuries. Adjusted for age, gender, rural hospital, Japan Coma Score, trauma severity, mechanical ventilation on admission, transfusion on admission, and neurosurgery on admission | + |
| Aoki et al., 2020 [21] | Severe trauma patient (ISS > 15) volume was associated with reduced in-hospital mortality compared to low volume (adjusted OR = 0.76; CI = 0.63–0.92). Adjusted for age, gender, cause of injury, vital signs, ISS, and hospital | + |
| Europe | ||
| Zacher et al., 2015[12] | Severe trauma patient volume was significantly associated with survival in Germany (OR 1.001 per patient per year (for each patient increase); p = 0.01). Adjusted for Revised Injury Severity Classification (RISC) II score, number of patients per year, and hospital level of care | + |
| Sewalt et al., 2020 [20] | No association between hospital volume and in-hospital mortality of severe trauma patients in England with ISS > 15 (adjusted OR 1.02; CI 0.68–1.54; p = 0.92). Adjusted for age, gender, ISS, Revised Trauma Score, comorbidities, penetrating injury, Abbreviated Injury Score, head injury, and referral | ± |
| Sewalt et al., 2021 [22] | No association between hospital volume and in-hospital mortality in the Netherlands (OR 0.97 per 50 extra patients; CI 0.90–1.04, p = 0.44). Adjusted for age, sex, ISS, systolic blood pressure, respiratory rate, GCS, prehospital intubation, ASA, penetrating injury, and Abbreviated Injury Score for head injury | ± |
| Outcome (Unadjusted) | ||
| Brown et al., 2017 [14] | Each 1% increase in volume was associated with 73% increased odds of improving standardized mortality ratios over time in the United States (OR 1.73; CI 1.03–2.91; p = 0.03). Standardized mortality rates included age, several clinical parameters at admission, GCS, ISS, and mechanism of injury | + |
| Toida et al., 2021 [24] | No significant differences in in-hospital mortality for severe trauma patients (ISS > 15) in Japan between high-volume and low-volume hospitals (median 2.13% vs. 0%), p = 0.25) | ± |
| Floan et al., 2022 [25] | Higher annual case volume was associated with improved hospital performance (lower observed mortality compared to expected mortality) for firearm-related thoracic trauma in pediatric patients in the United States, but not for cut/pierce trauma | + |
| Study | Outcome (Adjusted) | |
|---|---|---|
| Clement et al., 2013 [10] | No significant difference in the average cost per case with subarachnoid, subdural, and extradural hematoma between the hospital cohort <6 cases/year as compared with hospitals with more cases annually. Adjusted for, e.g., age, sex, geographical region, hospital characteristics, comorbidities, other severe head trauma, neurosurgical procedures performed, significant non-neurological injury, and severity of intracranial hemorrhage | ± |
| Endo et al., 2017 [15] | Increased severe trauma patient volume was significantly associated with lower total costs per admission for each 50-patient increase (adjusted difference −$488.0 (CI −$818.0 to −$158.0)). Adjusted for trauma severity and hospital characteristics | + |
| Sewalt et al., 2020 [20] | Significant association between hospital volume and critical care length of stay for each 10-patient with (ISS > 15) increase (adjusted OR 0.47; CI 0.02–0.94). Adjusted for age, gender, ISS, Revised Trauma Score, comorbidities, penetrating injury, Abbreviated Injury Score, head injury and referral | + |
| Outcome (Unadjusted) | ||
| Tang et al., 2021 [23] | No difference between high-, medium-, and low-volume hospitals in hospital length of stay for blunt and penetrating trauma patients with emergent laparotomies <24 h for hemorrhage control | ± |
| Floan et al., 2022 [25] | A higher annual case volume of pediatric penetrating thoracic trauma was associated with significant shorter hospital and intensive care length of stay | + |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Foppen, W.; Claassen, Y.; Falck, D.; van der Meer, N.J.M. Trauma Patient Volume and the Quality of Care: A Scoping Review. J. Clin. Med. 2023, 12, 5317. https://doi.org/10.3390/jcm12165317
Foppen W, Claassen Y, Falck D, van der Meer NJM. Trauma Patient Volume and the Quality of Care: A Scoping Review. Journal of Clinical Medicine. 2023; 12(16):5317. https://doi.org/10.3390/jcm12165317
Chicago/Turabian StyleFoppen, Wouter, Yvette Claassen, Debby Falck, and Nardo J. M. van der Meer. 2023. "Trauma Patient Volume and the Quality of Care: A Scoping Review" Journal of Clinical Medicine 12, no. 16: 5317. https://doi.org/10.3390/jcm12165317
APA StyleFoppen, W., Claassen, Y., Falck, D., & van der Meer, N. J. M. (2023). Trauma Patient Volume and the Quality of Care: A Scoping Review. Journal of Clinical Medicine, 12(16), 5317. https://doi.org/10.3390/jcm12165317






