Delirium and Its Association with Short- and Long-Term Health Outcomes in Medically Admitted Patients: A Prospective Study
Abstract
:1. Introduction
2. Materials and Methods
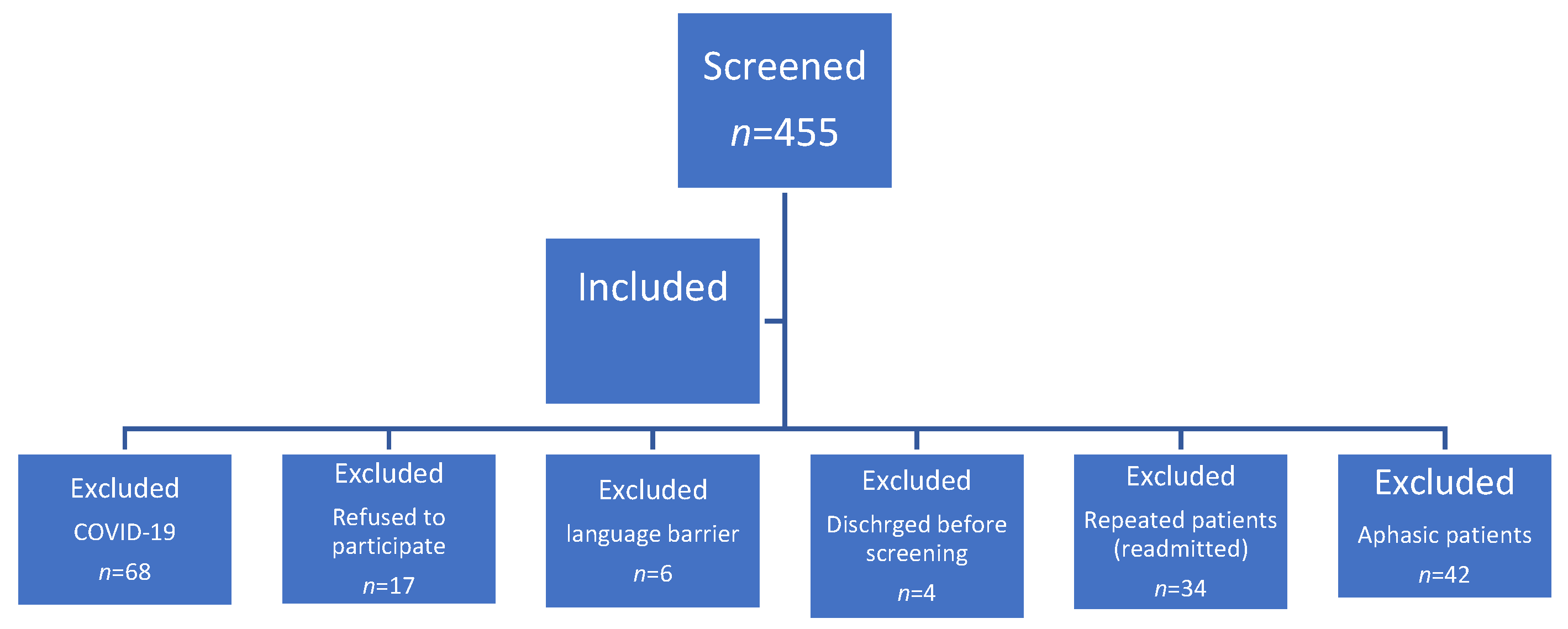
2.1. Study Population and Design
2.2. Assessment Tools and Data Collection
2.3. Definitions
- Multiple comorbidities were defined as ≥3 comorbid conditions.
- Polypharmacy was defined as ≥five chronic home medications.
- Pre-existing cognitive dysfunction was defined as patients with a short IQCODE score > 3 [20].
- Hyperactive delirium was defined as patients with agitation or disruptive behavior, hypoactive delirium described patients who appeared apathetic, withdrawn from the environment, or who had depressed levels of arousal, and mixed delirium was defined as patients who demonstrated hyperactive and hypoactive behaviors [22].
- Transient recovery from delirium was defined as delirium that recovered within 24 h, while recovered delirium was defined as delirium recovered via discharge and persistent delirium was defined as delirium present at the time of discharge.
- The educated patient was defined as a patient with a high school education. On the other hand, the uneducated patient was an illiterate person or a patient with an education lower than high school.
2.4. Sample Size
2.5. Statistical Analysis
2.6. Ethical Approval
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ely, E.W.; Shintani, A.; Truman, B.; Speroff, T.; Gordon, S.M.; Harrell, F.E., Jr.; Inouye, S.K.; Bernard, G.R.; Dittus, R.S. Delirium as a predictor of mortality in mechanically ventilated patients in the intensive care unit. JAMA 2004, 291, 1753–1762. [Google Scholar] [CrossRef]
- Wass, S.; Webster, P.J.; Nair, B.R. Delirium in the elderly: A review. Oman Med. J. 2008, 23, 150–157. [Google Scholar]
- Australian and New Zealand Society for Geriatric Medicine Position Statement Abstract: Delirium in older people. Australas. J. Ageing 2016, 35, 292. [CrossRef] [PubMed]
- Al Farsi, R.S.; Al Alawi, A.M.; Al Huraizi, A.R.; Al-Saadi, T.; Al-Hamadani, N.; Al Zeedy, K.; Al-Maqbali, J.S. Delirium in Medically Hospitalized Patients: Prevalence, Recognition and Risk Factors: A Prospective Cohort Study. J. Clin. Med. 2023, 12, 3897. [Google Scholar] [CrossRef] [PubMed]
- Meagher, D.; Adamis, D.; Leonard, M.; Trzepacz, P.; Grover, S.; Jabbar, F.; Meehan, K.; O’Connor, M.; Cronin, C.; Reynolds, P.; et al. Development of an abbreviated version of the delirium motor subtyping scale (DMSS-4). Int. Psychogeriatr. 2014, 26, 693–702. [Google Scholar] [CrossRef] [PubMed]
- Fiest, K.M.; Soo, A.; Hee Lee, C.; Niven, D.J.; Ely, E.W.; Doig, C.J.; Stelfox, H.T. Long-Term Outcomes in ICU Patients with Delirium: A Population-based Cohort Study. Am. J. Respir. Crit. Care Med. 2021, 204, 412–420. [Google Scholar] [CrossRef]
- Witlox, J.; Eurelings, L.S.; de Jonghe, J.F.; Kalisvaart, K.J.; Eikelenboom, P.; van Gool, W.A. Delirium in elderly patients and the risk of post-discharge mortality, institutionalization, and dementia: A meta-analysis. JAMA 2010, 304, 443–451. [Google Scholar] [CrossRef] [PubMed]
- Aung Thein, M.Z.; Pereira, J.V.; Nitchingham, A.; Caplan, G.A. A call to action for delirium research: Meta-analysis and regression of delirium associated mortality. BMC Geriatr. 2020, 20, 325. [Google Scholar] [CrossRef]
- Siddiqi, N.; House, A.O.; Holmes, J.D. Occurrence and outcome of delirium in medical inpatients: A systematic literature review. Age Ageing 2006, 35, 350–364. [Google Scholar] [CrossRef]
- Andrew, M.K.; Freter, S.H.; Rockwood, K. Incomplete functional recovery after delirium in elderly people: A prospective cohort study. BMC Geriatr. 2005, 5, 5. [Google Scholar] [CrossRef]
- Rockwood, K.; Cosway, S.; Carver, D.; Jarrett, P.; Stadnyk, K.; Fisk, J. The risk of dementia and death after delirium. Age Ageing 1999, 28, 551–556. [Google Scholar] [CrossRef] [PubMed]
- Sahle, B.W.; Pilcher, D.; Litton, E.; Ofori-Asenso, R.; Peter, K.; McFadyen, J.; Bucknall, T. Association between frailty, delirium, and mortality in older critically ill patients: A binational registry study. Ann. Intensive Care 2022, 12, 108. [Google Scholar] [CrossRef] [PubMed]
- Pompei, P.; Foreman, M.; Rudberg, M.A.; Inouye, S.K.; Braund, V.; Cassel, C.K. Delirium in hospitalized older persons: Outcomes and predictors. J. Am. Geriatr. Soc. 1994, 42, 809–815. [Google Scholar] [CrossRef] [PubMed]
- Pereira, F.B.; Lopes, M.A. Delirium in elderly inpatients admitted to clinical wards prevalence and investigation of clinical conditions in a Brazilian sample. Dement. Neuropsychol. 2018, 12, 152–156. [Google Scholar] [CrossRef] [PubMed]
- Díez-Manglano, J.; Palazón-Fraile, C.; Diez-Massó, F.; Martínez-Álvarez, R.; Del Corral-Beamonte, E.; Carreño-Borrego, P.; Pueyo-Tejedor, P.; Gomes-Martín, J. Factors Associated with Onset of Delirium among Internal Medicine Inpatients in Spain. Nurs. Res. 2013, 62, 445–449. [Google Scholar] [CrossRef] [PubMed]
- Al-Yarabi, A.; Al Balushi, H.; Al Hatmi, K.; Al Yahyaie, R.; Al Alawi, A.M.; Al Zeedy, K.; Al Farhan, H. Inappropriate Hospital Stay of Patients Admitted Under Care of General Medicine Units: A retrospective study. Sultan Qaboos Univ. Med. J. 2022, 23. [Google Scholar] [CrossRef] [PubMed]
- Wei, L.A.; Fearing, M.A.; Sternberg, E.J.; Inouye, S.K. The Confusion Assessment Method: A systematic review of current usage. J. Am. Geriatr. Soc. 2008, 56, 823–830. [Google Scholar] [CrossRef]
- Marcantonio, E.R.; Ngo, L.H.; O’Connor, M.; Jones, R.N.; Crane, P.K.; Metzger, E.D.; Inouye, S.K. 3D-CAM: Derivation and validation of a 3-minute diagnostic interview for CAM-defined delirium: A cross-sectional diagnostic test study. Ann. Intern. Med. 2014, 161, 554–561. [Google Scholar] [CrossRef]
- Alamri, S.H.; Ashanqity, O.A.; Alshomrani, A.B.; Elmasri, A.H.; Saeed, M.B.; Yahya, S.A.; Almasoud, A.I.; Adam, Y.; Alamoudi, H.M.; Mukhtar, A.M. Delirium and correlates of delirium among newly admitted elderly patients: A cross-sectional study in a Saudi general hospital. Ann. Saudi Med. 2018, 38, 15–21. [Google Scholar] [CrossRef]
- Harrison, J.K.; Fearon, P.; Noel-Storr, A.H.; McShane, R.; Stott, D.J.; Quinn, T.J. Informant Questionnaire on Cognitive Decline in the Elderly (IQCODE) for the diagnosis of dementia within a secondary care setting. Cochrane Database Syst. Rev. 2015, Cd010772. [Google Scholar] [CrossRef]
- Shelkey, M.; Wallace, M. Katz Index of Independence in Activities of Daily Living (ADL). Director 2000, 8, 72–73. [Google Scholar] [PubMed]
- Smith, H.A.B.; Besunder, J.B.; Betters, K.A.; Johnson, P.N.; Srinivasan, V.; Stormorken, A.; Farrington, E.; Golianu, B.; Godshall, A.J.; Acinelli, L.; et al. 2022 Society of Critical Care Medicine Clinical Practice Guidelines on Prevention and Management of Pain, Agitation, Neuromuscular Blockade, and Delirium in Critically Ill Pediatric Patients with Consideration of the ICU Environment and Early Mobility. Pediatr. Crit. Care Med. 2022, 23, e74–e110. [Google Scholar] [CrossRef] [PubMed]
- McAvay, G.J.; Van Ness, P.H.; Bogardus, S.T., Jr.; Zhang, Y.; Leslie, D.L.; Leo-Summers, L.S.; Inouye, S.K. Older adults discharged from the hospital with delirium: 1-year outcomes. J. Am. Geriatr. Soc. 2006, 54, 1245–1250. [Google Scholar] [CrossRef] [PubMed]
- Al-Hoodar, R.K.; Lazarus, E.R.; Al Omari, O.; Al Zaabi, O. Incidence, Associated Factors, and Outcome of Delirium among Patients Admitted to ICUs in Oman. Crit. Care Res. Pract. 2022, 2022, 4692483. [Google Scholar] [CrossRef]
- Khalighi, E.; Tarjoman, A.; Abdi, A.; Borji, M. The prevalence of delirium in patients in Iran: A systematic review and meta-analysis. Future Neurol. 2019, 14, FNL34. [Google Scholar] [CrossRef]
- Grey, T.; Fleming, R.; Goodenough, B.J.; Xidous, D.; Möhler, R.; O’Neill, D. Hospital design for older people with cognitive impairment including dementia and delirium: Supporting inpatients and accompanying persons. Cochrane Database Syst. Rev. 2019, 20, CD013482. [Google Scholar] [CrossRef]
- Thomas, R.I.; Cameron, D.J.; Fahs, M.C. A prospective study of delirium and prolonged hospital stay. Exploratory study. Arch. Gen. Psychiatry 1988, 45, 937–940. [Google Scholar] [CrossRef]
- Dziegielewski, C.; Skead, C.; Canturk, T.; Webber, C.; Fernando, S.M.; Thompson, L.H.; Foster, M.; Ristovic, V.; Lawlor, P.G.; Chaudhuri, D.; et al. Delirium and Associated Length of Stay and Costs in Critically Ill Patients. Crit. Care Res. Pract. 2021, 2021, 6612187. [Google Scholar] [CrossRef]
- Welch, C.; McCluskey, L.; Wilson, D.; Chapman, G.E.; Jackson, T.A.; Treml, J.; Davis, D.; Cunningham, E.; Copeland, C.; Quinn, T.; et al. Delirium is prevalent in older hospital inpatients and associated with adverse outcomes: Results of a prospective multi-center study on World Delirium Awareness Day. BMC Med. 2019, 17, 229. [Google Scholar] [CrossRef]
- O’Keeffe, S.; Lavan, J. The Prognostic Significance of Delirium in Older Hospital Patients. J. Am. Geriatr. Soc. 1997, 45, 174–178. [Google Scholar] [CrossRef]
- Krewulak, K.D.; Stelfox, H.T.; Leigh, J.P.; Ely, E.W.; Fiest, K.M. Incidence and Prevalence of Delirium Subtypes in an Adult ICU: A Systematic Review and Meta-Analysis. Crit. Care Med. 2018, 46, 2029–2035. [Google Scholar] [CrossRef] [PubMed]
- Serafim, R.B.; Bozza, F.A.; Soares, M.; do Brasil, P.E.; Tura, B.R.; Ely, E.W.; Salluh, J.I. Pharmacologic prevention and treatment of delirium in intensive care patients: A systematic review. J. Crit. Care 2015, 30, 799–807. [Google Scholar] [CrossRef] [PubMed]
- Cortés-Beringola, A.; Vicent, L.; Martín-Asenjo, R.; Puerto, E.; Domínguez-Pérez, L.; Maruri, R.; Moreno, G.; Vidán, M.T.; Fernando, A.; Bueno, H. Diagnosis, prevention, and management of delirium in the intensive cardiac care unit. Am. Heart J. 2021, 232, 164–176. [Google Scholar] [CrossRef]
- Al Sibani, M.; Al-Maqbali, J.S.; Yusuf, Z.; Al Alawi, A.M. Incidence and Risk Factors for 28 Days Hospital Readmission: A Retrospective Study from Oman. Oman Med. J. 2022, 37, e423. [Google Scholar] [CrossRef]
- McCusker, J.; Cole, M.; Abrahamowicz, M.; Primeau, F.; Belzile, E. Delirium predicts 12-month mortality. Arch. Intern. Med. 2002, 162, 457–463. [Google Scholar] [CrossRef]
- Hapca, S.; Guthrie, B.; Cvoro, V.; Bu, F.; Rutherford, A.C.; Reynish, E.; Donnan, P.T. Mortality in people with dementia, delirium, and unspecified cognitive impairment in the general hospital: A prospective cohort study of 6724 patients with 2 years follow-up. Clin. Epidemiol. 2018, 10, 1743–1753. [Google Scholar] [CrossRef] [PubMed]
- Cole, M.G.; Ciampi, A.; Belzile, E.; Zhong, L. Persistent delirium in older hospital patients: A systematic review of frequency and prognosis. Age Ageing 2009, 38, 19–26. [Google Scholar] [CrossRef] [PubMed]
- Jackson, T.A.; Wilson, D.; Richardson, S.; Lord, J.M. Predicting outcome in older hospital patients with delirium: A systematic literature review. Int. J. Geriatr. Psychiatry 2016, 31, 392–399. [Google Scholar] [CrossRef]
- Marcantonio, E.; Ta, T.; Duthie, E.; Resnick, N.M. Delirium severity and psychomotor types: Their relationship with outcomes after hip fracture repair. J. Am. Geriatr. Soc. 2002, 50, 850–857. [Google Scholar] [CrossRef]
- Tropea, J.; Slee, J.A.; Brand, C.A.; Gray, L.; Snell, T. Clinical practice guidelines for the management of delirium in older people in Australia. Australas. J. Ageing 2008, 27, 150–156. [Google Scholar] [CrossRef]
- Huang, D.D.; Fischer, P.E. Management of Delirium in the Intensive Care Unit. Surg. Clin. N. Am. 2022, 102, 139–148. [Google Scholar] [CrossRef]
- Cerveira, C.C.T.; Pupo, C.C.; Dos Santos, S.S.; Santos, J.E.M. Delirium in the elderly: A systematic review of pharmacological and non-pharmacological treatments. Dement. Neuropsychol. 2017, 11, 270–275. [Google Scholar] [CrossRef] [PubMed]
- Grover, S.; Avasthi, A. Clinical Practice Guidelines for Management of Delirium in Elderly. Indian J. Psychiatry 2018, 60, S329–S340. [Google Scholar] [CrossRef] [PubMed]

| Total 284 (100%) | No Delirium 131 (46.13%) | Delirium 153 (53.87%) | p-Value | |
|---|---|---|---|---|
| Age (IQR), years | 71 (66–78) | 68 (64–74) | 75 (68–80) | <0.01 |
| Female | 148 (52.11%) | 59 (45.04%) | 89 (58.17%) | 0.027 |
| Not educated | 219 (77.11%) | 88 (67.18%) | 131 (85.62%) | <0.01 |
| Functional impairment (BADL < 6) | 191 (67.25%) | 57 (43.51%) | 134 (87.58%) | <0.01 |
| Pre-existing cognitive dysfunction | 63 (22.18%) | 10 (7.63%) | 53 (34.64%) | <0.01 |
| Multiple comorbidities (≥3) | 239 (84.15%) | 100 (76.34%) | 139 (90.85%) | <0.01 |
| Polypharmacy (≥5) | 260 (91.55%) | 112 (85.50%) | 149 (96.73%) | <0.01 |
| Inpatient clinical outcomes | ||||
| LOS (IQR), days | 6 (3–9) | 5 (3–8) | 7 (4–13) | <0.01 |
| ICU admission | 17 (5.99%) | 2 (1.53%) | 15 (9.80%) | <0.01 |
| HD admission | 35 (12.32%) | 4 (3.05%) | 31 (20.26%) | <0.01 |
| Nosocomial complication | 53 (18.79%) | 11 (8.53%) | 42 (27.45%) | <0.01 |
| Pressure injury | 15 (5.35%) | 1 (0.78%) | 14 (9.15%) | <0.01 |
| Hospital-acquired infection | 38 (13.48%) | 11 (8.53%) | 27 (17.65%) | 0.03 |
| Stress upper GI ulcers | 13 (4.61%) | 0 | 13 (8.50%) | <0.01 |
| Venous thromboembolism | 4 (1.42%) | 1 (0.78%) | 3 (1.96%) | 0.628 |
| All-cause mortality | ||||
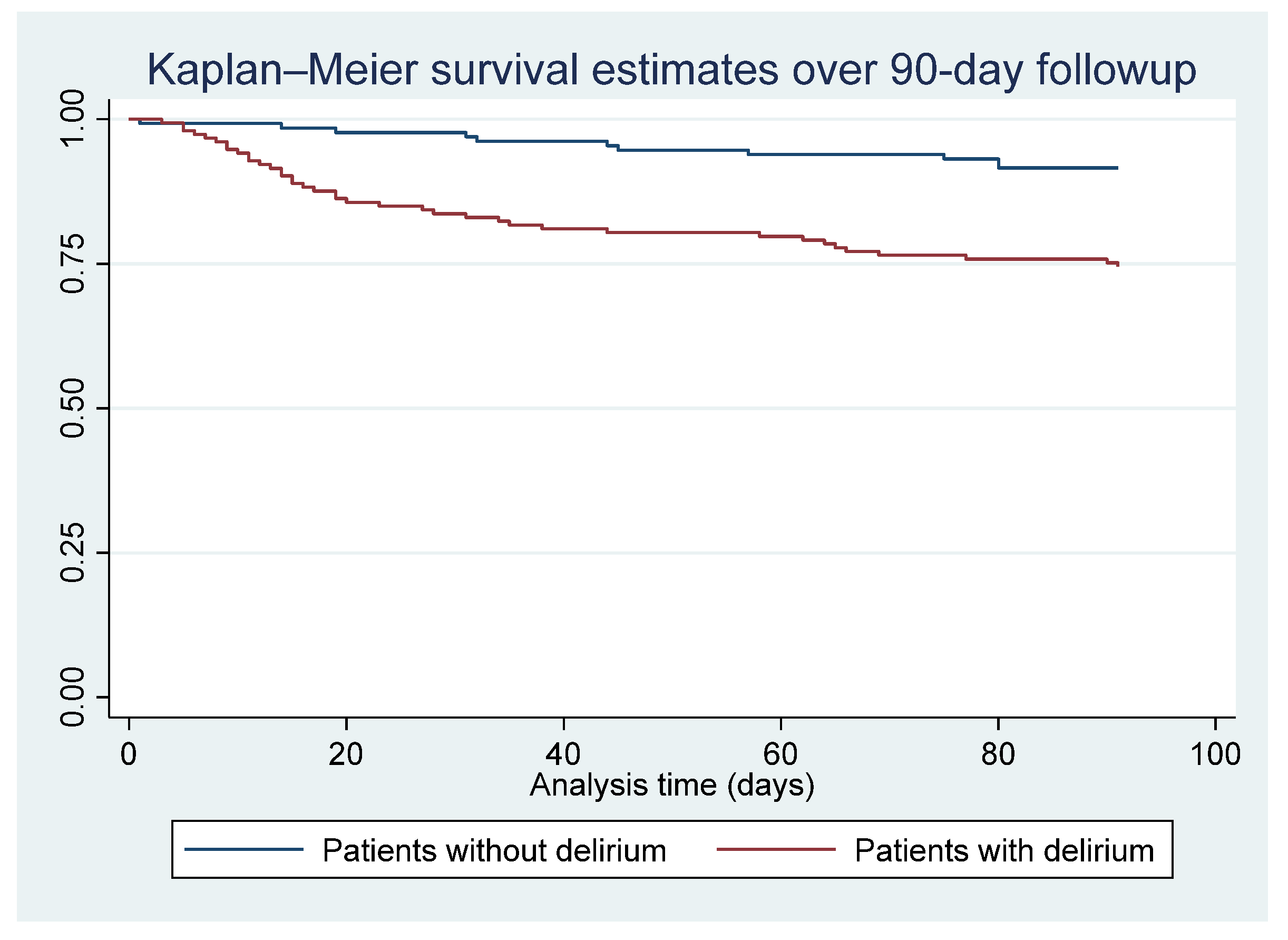
| Inpatient all-cause mortality | 27 (9.51%) | 2 (1.53%) | 25 (16.34%) | <0.01 |
| 90-day all-cause mortality | 50 (17.61%) | 11 (8.40%) | 39 (25.49%) | <0.01 |
| 1-year all-cause mortality | 76 (26.76%) | 21 (16.03%) | 55 (35.95%) | <0.01 |
| Clinical Outcomes n (%) unless Specified Otherwise | Total 153 (100%) | Hypoactive Delirium 102 (66.67%) | Hyperactive Delirium 11 (7.19%) | Mixed Delirium 40 (26.14%) | p-Value |
|---|---|---|---|---|---|
| LOS (IQR), days | 7 (4–13) | 7 (4–12) | 6 (4–6) | 9 (6–16) | 0.05 |
| Inpatient all-cause mortality | 25 (16.34%) | 19 (18.63%) | 1 (9.09%) | 5 (12.50%) | 0.62 |
| 90-day all-cause mortality | 39 (25.49%) | 28 (27.45%) | 1 (9.09%) | 10 (25.00%) | 0.47 |
| 1-year all-cause mortality | 55 (35.95%) | 40 (39.22%) | 2 (18.18%) | 13 (32.50%) | 0.38 |
| Clinical Outcomes n (%) unless Specified Otherwise | Total 153 (100%) | Persistent Delirium 82 (53.59%) | Transit Delirium 29 (18.95%) | Recovered Delirium 42 (27.45%) | p-Value |
|---|---|---|---|---|---|
| LOS (IQR), days | 7 (4–13) | 9 (5–16) | 5 (2–6) | 7 (4–9) | <0.01 |
| Inpatient all-cause mortality | 25 (16.34%) | 24 (29.27%) | 1 (3.45%) | 0 | <0.01 |
| 90-day all-cause mortality | 39 (25.49%) | 33 (40.24%) | 2 (6.90%) | 4 (9.52%) | <0.01 |
| 1-year all-cause mortality | 55 (35.95%) | 44 (53.66%) | 4 (13.79%) | 7 (16.67%) | <0.01 |
| Clinical Outcomes n (%) unless Specified Otherwise | Total 153 (100%) | Not-Administered Delirium Medications 111 (72.55%) | Administered Delirium Medications 42 (27.45%) | p-Value |
|---|---|---|---|---|
| LOS (IQR), days | 7 (4–13) | 7 (4–13) | 8 (5–13) | 0.57 |
| Inpatient all-cause mortality | 25 (16.34%) | 17 (15.35%) | 8 (19.05%) | 0.58 |
| 90-day all-cause mortality | 39 (25.49%) | 30 (27.03%) | 9 (21.43%) | 0.48 |
| 1-year all-cause mortality | 55 (35.95%) | 41 (36.94%) | 14 (33.33%) | 0.68 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Al Huraizi, A.R.; Al-Maqbali, J.S.; Al Farsi, R.S.; Al Zeedy, K.; Al-Saadi, T.; Al-Hamadani, N.; Al Alawi, A.M. Delirium and Its Association with Short- and Long-Term Health Outcomes in Medically Admitted Patients: A Prospective Study. J. Clin. Med. 2023, 12, 5346. https://doi.org/10.3390/jcm12165346
Al Huraizi AR, Al-Maqbali JS, Al Farsi RS, Al Zeedy K, Al-Saadi T, Al-Hamadani N, Al Alawi AM. Delirium and Its Association with Short- and Long-Term Health Outcomes in Medically Admitted Patients: A Prospective Study. Journal of Clinical Medicine. 2023; 12(16):5346. https://doi.org/10.3390/jcm12165346
Chicago/Turabian StyleAl Huraizi, Aisha Ramadhan, Juhaina Salim Al-Maqbali, Rajaa Saleh Al Farsi, Khalfan Al Zeedy, Taif Al-Saadi, Noof Al-Hamadani, and Abdullah M. Al Alawi. 2023. "Delirium and Its Association with Short- and Long-Term Health Outcomes in Medically Admitted Patients: A Prospective Study" Journal of Clinical Medicine 12, no. 16: 5346. https://doi.org/10.3390/jcm12165346
APA StyleAl Huraizi, A. R., Al-Maqbali, J. S., Al Farsi, R. S., Al Zeedy, K., Al-Saadi, T., Al-Hamadani, N., & Al Alawi, A. M. (2023). Delirium and Its Association with Short- and Long-Term Health Outcomes in Medically Admitted Patients: A Prospective Study. Journal of Clinical Medicine, 12(16), 5346. https://doi.org/10.3390/jcm12165346





