The Potential Role of Hypothalamic Phospholipid Liposomes in the Supportive Therapy of Some Manifestations of Post-COVID-19 Condition: Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS) and Brain Fog
Abstract
:1. Introduction
2. Definition and Epidemiology of Post-COVID-19 Condition
3. Clinical Symptoms and Syndromes
- -
- Persistent symptoms and conditions that begin at the time of acute COVID-19 illness;
- -
- Signs, symptoms, or conditions of new onset following asymptomatic illness or a period of improvement or remission of acute symptoms;
- -
- Evolution of symptoms and conditions, which include some persistent symptoms (e.g., shortness of breath) with the addition of new symptoms (e.g., cognitive difficulties);
- -
- Worsening of pre-existing symptoms or conditions.
| Post-COVID Syndrome | Clinical Manifestations | Comment |
|---|---|---|
| Post-COVID fatigue syndrome | Profound fatigue, post-exertion malaise, and/or poor resistance | Rule out causes like anemia, electrolyte imbalance, hypothyroidism. |
| Post-COVID cardio-respiratory syndrome | Cough, dyspnea or increased fatigue, low-grade fever, chest pain, orthostatic hypotension, palpitations, and tachycardia | Sudden worsening of dyspnea: consider tension pneumothorax, pulmonary embolism, coronary artery disease, or heart failure. |
| Post-COVID neuro-psychiatric syndrome | Headaches, anosmia or dysgeusia, cognitive impairment or “brain fog”, depression and other mood changes, paresthesia, insomnia and other sleep difficulties, dizziness | If acute onset neurological symptoms present, also consider vasculitis, thrombosis, or demyelination. Properly evaluate post-COVID psychological problems. |
| Post-COVID gastro-intestinal syndrome | Abdominal discomfort, diarrhea, constipation, vomiting | GI symptoms can be a sequalae of the disease or therapy-related side effects. |
| Post-COVID hepato-biliary syndrome | Nausea, jaundice, liver function test alterations | Drugs used in the treatment of COVID-19 can cause hepatic impairment. |
| Post-COVID musculo-skeletal syndrome | Arthralgia, myalgia, muscle weakness | Causes include COVID-19 disease, prolonged ICU care, neurological problems, myopathy, or electrolyte imbalance. Usually subside during follow up. Inflammatory arthralgia must be differentiated from other causes like Systemic Lupus Erythematosus, Rheumatoid Arthritis. |
| Post-COVID thromboembolic syndrome | Depending upon the vascular territory of involvement, dyspnea in Pulmonary Embolism, chest pain in Coronary Artery Disease, and limb weakness and neurological deficit in stroke | Early diagnosis and treatment are lifesaving. Follow the standard treatment protocol. |
| Post-COVID multisystem inflammatory syndrome/post-COVID autoimmune syndrome | Fever, gastrointestinal symptoms, rash, chest pain, palpitations | Elevated levels of markers of inflammation. |
| Post-COVID genito-urinary symptoms | Proteinuria, hematuria, development of kidney injury, menstrual cycle irregularities, erectile dysfunction | COVID-19 may predispose surviving patients to chronic kidney disease, independently of clinically apparent acute kidney injury (AKI). Therefore, post-acute COVID-19 care should include close attention to kidney function. |
| Post-COVID dermatological syndrome | Vesicular, maculopapular, urticarial, or chilblain-like lesions on the extremities (COVID toe) |
3.1. Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS)
- Substantial reduction or alteration of employment, educational, social, or personal capacities that persists for more than 6 months and is accompanied by asthenia, often profound, of new or recent onset (not pre-existing), that is not the result of continuous excessive effort and is not effectively alleviated by rest.
- Post-exertion malaise.
- Non-restorative sleep.
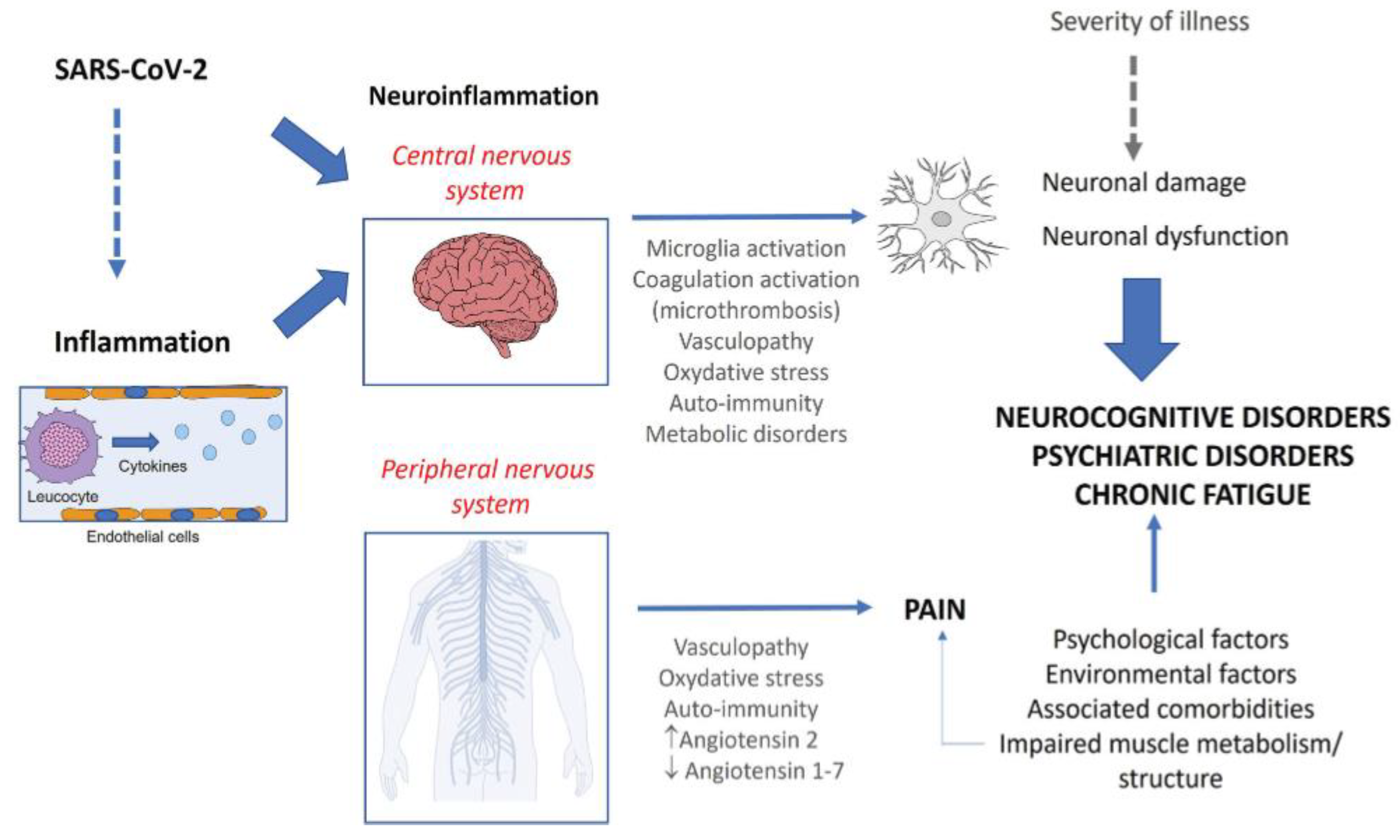
3.2. Cognitive Impairment
4. The Potential Role of Hypothalamic Phospholipid Liposomes in Post-COVID-19 Condition
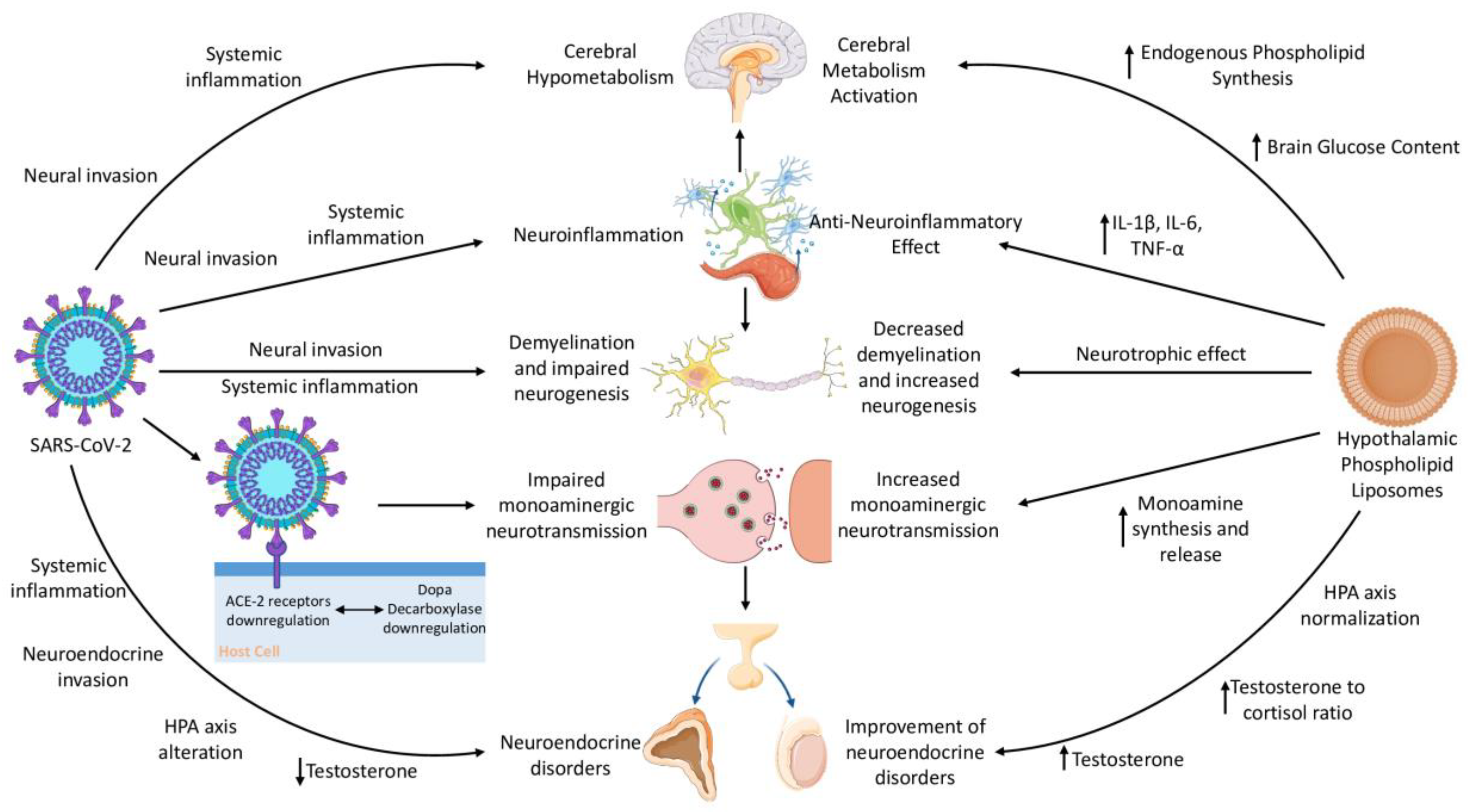
4.1. Pathophysiological Mechanisms in Post-COVID-19 Condition and the Pharmacology of Hypothalamic Phospholipid Liposomes
4.1.1. The Monoaminergic Hypothesis
4.1.2. Neuroinflammation, Demyelination, and Impaired Neurogenesis
4.1.3. Cerebral Hypometabolism
4.1.4. Male Fertility Alterations
4.2. Clinical Evidence on Hypothalamic Phospholipid Liposomes and Its Implications for Post-COVID-19 Condition
| Post-COVID-19 Condition | Hypothalamic Phospholipid Liposomes |
|---|---|
| Pathophysiology | Mechanism of Action |
| Hypometabolic activity in certain brain areas [72] | Activation of cerebral metabolism (i.e., increased brain glucose content and phospholipid synthesis) [47] |
| ACE2–Dopa Decarboxylase co-expression, which leads to impaired monoaminergic neurotransmission [49] | Increased catecholamine turnover and release, stimulation of tyrosine hydroxylase and dopamine-dependent adenylyl cyclase, modification of monoaminergic receptor adaptation [47,48] |
| Neuroinflammation from CSF cytokine elevation (e.g., IL-1β, IL-6) and microglial reactivity [23,62,64] | Antagonizing effect on proinflammatory cytokines (IL-1β, IL-6, TNF-α) in different brain areas [47] |
| Demyelination and impaired neurogenesis [27,64] | Neurotrophic effect, increase in neurogenesis and dendritogenesis, as well as antagonizing effect of PE, PC, and PS on demyelination [48,66,67] |
| Low testosterone [74,77] | PS increases plasma levels of testosterone compared to placebo and the testosterone to cortisol ratio in an exercise-related context [78,79] |
| Clinical Manifestations | Clinical Evidence |
| Fatigue | Improvement of asthenia [83,84] |
| Brain fog | PS: |
| Anxiety and depression | Improvement in the symptomatology of anxiety and depression as monotherapy or add-on to antidepressants [47,48] |
| Orthostatic intolerance | Antagonizing effect on hypotension and reflex tachycardia caused by trazodone [83] |
| Male sexual health problem | Phospholipids (PC in particular) improve erectile dysfunction and loss of libido [80] |
5. Conclusions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ministero della Salute. COVID-19—Situazione in Italia. Available online: https://www.salute.gov.it/portale/nuovocoronavirus/dettaglioContenutiNuovoCoronavirus.jsp?area=nuovoCoronavirus&id=5351&lingua=italiano&menu=vuoto (accessed on 24 July 2023).
- Nurek, M.; Rayner, C.; Freyer, A.; Taylor, S.; Järte, L.; MacDermott, N.; Delaney, B.C. Recommendations for the Recognition, Diagnosis, and Management of Long COVID: A Delphi Study. Br. J. Gen. Pract. 2021, 71, e815–e825. [Google Scholar] [CrossRef]
- Soriano, J.B.; Murthy, S.; Marshall, J.C.; Relan, P.; Diaz, J.V. A Clinical Case Definition of Post-COVID-19 Condition by a Delphi Consensus. Lancet Infect. Dis. 2022, 22, e102–e107. [Google Scholar] [CrossRef]
- Montani, D.; Savale, L.; Noel, N.; Meyrignac, O.; Colle, R.; Gasnier, M.; Corruble, E.; Beurnier, A.; Jutant, E.-M.; Pham, T.; et al. Post-Acute COVID-19 Syndrome. Eur. Respir. Rev. 2022, 31, 210185. [Google Scholar] [CrossRef]
- Yelin, D.; Moschopoulos, C.D.; Margalit, I.; Gkrania-Klotsas, E.; Landi, F.; Stahl, J.-P.; Yahav, D. ESCMID Rapid Guidelines for Assessment and Management of Long COVID. Clin. Microbiol. Infect. 2022, 28, 955–972. [Google Scholar] [CrossRef]
- Department of Health and Human Services, Office of the Assistant Secretary for Health. National Research Action Plan on Long COVID; Department of Health and Human Services, Office of the Assistant Secretary for Health: Washington, DC, USA, 2022.
- Centers for Disease Control and Prevention. Post-COVID Conditions: Information for Healthcare Providers. Available online: https://www.cdc.gov/coronavirus/2019-ncov/hcp/clinical-care/post-covid-conditions.html (accessed on 10 July 2023).
- Giuliano, M.; Tiple, D.; Agostoni, P.; Armocida, B.; Biardi, L.; Bonfigli, A.R.; Campana, A.; Ciardi, M.; Di Marco, F.; Floridia, M.; et al. Italian Good Practice Recommendations on Management of Persons with Long-COVID. Front. Public Health 2023, 11, 1122141. [Google Scholar] [CrossRef]
- Woodrow, M.; Carey, C.; Ziauddeen, N.; Thomas, R.; Akrami, A.; Lutje, V.; Greenwood, D.C.; Alwan, N.A. Systematic Review of the Prevalence of Long COVID. Open Forum Infect. Dis. 2023, 10, ofad233. [Google Scholar] [CrossRef]
- Subramanian, A.; Nirantharakumar, K.; Hughes, S.; Myles, P.; Williams, T.; Gokhale, K.M.; Taverner, T.; Chandan, J.S.; Brown, K.; Simms-Williams, N.; et al. Symptoms and Risk Factors for Long COVID in Non-Hospitalized Adults. Nat. Med. 2022, 28, 1706–1714. [Google Scholar] [CrossRef]
- Lam, I.C.H.; Wong, C.K.H.; Zhang, R.; Chui, C.S.L.; Lai, F.T.T.; Li, X.; Chan, E.W.Y.; Luo, H.; Zhang, Q.; Man, K.K.C.; et al. Long-Term Post-Acute Sequelae of COVID-19 Infection: A Retrospective, Multi-Database Cohort Study in Hong Kong and the UK. eClinicalMedicine 2023, 60, 102000. [Google Scholar] [CrossRef]
- Mizrahi, B.; Sudry, T.; Flaks-Manov, N.; Yehezkelli, Y.; Kalkstein, N.; Akiva, P.; Ekka-Zohar, A.; Ben David, S.S.; Lerner, U.; Bivas-Benita, M.; et al. Long COVID Outcomes at One Year after Mild SARS-CoV-2 Infection: Nationwide Cohort Study. BMJ 2023, 380, e072529. [Google Scholar] [CrossRef]
- Ballouz, T.; Menges, D.; Anagnostopoulos, A.; Domenghino, A.; Aschmann, H.E.; Frei, A.; Fehr, J.S.; Puhan, M.A. Recovery and Symptom Trajectories up to Two Years after SARS-CoV-2 Infection: Population Based, Longitudinal Cohort Study. BMJ 2023, 381, e074425. [Google Scholar] [CrossRef]
- National Center for Health Statistics. U.S. Census Bureau, Household Pulse Survey, 2022–2023. Long COVID. Generated Interactively. Available online: https://www.cdc.gov/nchs/COVID19/pulse/long-COVID.htm (accessed on 12 July 2023).
- Walker, S.; Goodfellow, H.; Pookarnjanamorakot, P.; Murray, E.; Bindman, J.; Blandford, A.; Bradbury, K.; Cooper, B.; Hamilton, F.L.; Hurst, J.R.; et al. Impact of Fatigue as the Primary Determinant of Functional Limitations among Patients with Post-COVID-19 Syndrome: A Cross-Sectional Observational Study. BMJ Open 2023, 13, e069217. [Google Scholar] [CrossRef]
- Davis, H.E.; McCorkell, L.; Vogel, J.M.; Topol, E.J. Long COVID: Major Findings, Mechanisms and Recommendations. Nat. Rev. Microbiol. 2023, 21, 133–146. [Google Scholar] [CrossRef]
- Raveendran, A.V.; Jayadevan, R.; Sashidharan, S. Long COVID: An Overview. Diabetes Metab. Syndr. Clin. Res. Rev. 2021, 15, 869–875. [Google Scholar] [CrossRef]
- Schiffl, H.; Lang, S.M. Long-Term Interplay between COVID-19 and Chronic Kidney Disease. Int. Urol. Nephrol. 2023, 55, 1977–1984. [Google Scholar] [CrossRef]
- Bateman, L.; Bested, A.C.; Bonilla, H.F.; Chheda, B.V.; Chu, L.; Curtin, J.M.; Dempsey, T.T.; Dimmock, M.E.; Dowell, T.G.; Felsenstein, D.; et al. Myalgic Encephalomyelitis/Chronic Fatigue Syndrome: Essentials of Diagnosis and Management. Mayo Clin. Proc. 2021, 96, 2861–2878. [Google Scholar] [CrossRef]
- Campos, M.C.; Nery, T.; Starke, A.C.; De Bem Alves, A.C.; Speck, A.E.; S Aguiar, A. Post-Viral Fatigue in COVID-19: A Review of Symptom Assessment Methods, Mental, Cognitive, and Physical Impairment. Neurosci. Biobehav. Rev. 2022, 142, 104902. [Google Scholar] [CrossRef]
- Sukocheva, O.A.; Maksoud, R.; Beeraka, N.M.; Madhunapantula, S.V.; Sinelnikov, M.; Nikolenko, V.N.; Neganova, M.E.; Klochkov, S.G.; Amjad Kamal, M.; Staines, D.R.; et al. Analysis of Post COVID-19 Condition and Its Overlap with Myalgic Encephalomyelitis/Chronic Fatigue Syndrome. J. Adv. Res. 2022, 40, 179–196. [Google Scholar] [CrossRef]
- Retornaz, F.; Rebaudet, S.; Stavris, C.; Jammes, Y. Long-Term Neuromuscular Consequences of SARS-CoV-2 and Their Similarities with Myalgic Encephalomyelitis/Chronic Fatigue Syndrome: Results of the Retrospective CoLGEM Study. J. Transl. Med. 2022, 20, 429. [Google Scholar] [CrossRef]
- Castanares-Zapatero, D.; Chalon, P.; Kohn, L.; Dauvrin, M.; Detollenaere, J.; Maertens De Noordhout, C.; Primus-de Jong, C.; Cleemput, I.; Van Den Heede, K. Pathophysiology and Mechanism of Long COVID: A Comprehensive Review. Ann. Med. 2022, 54, 1473–1487. [Google Scholar] [CrossRef]
- Quan, M.; Wang, X.; Gong, M.; Wang, Q.; Li, Y.; Jia, J. Post-COVID Cognitive Dysfunction: Current Status and Research Recommendations for High Risk Population. Lancet Reg. Health-West. Pac. 2023, 38, 100836. [Google Scholar] [CrossRef]
- Merad, M.; Blish, C.A.; Sallusto, F.; Iwasaki, A. The Immunology and Immunopathology of COVID-19. Science 2022, 375, 1122–1127. [Google Scholar] [CrossRef] [PubMed]
- Nicolai, L.; Kaiser, R.; Stark, K. Thromboinflammation in Long COVID—The Elusive Key to Postinfection Sequelae? J. Thromb. Haemost. 2023, 21, 2020–2031. [Google Scholar] [CrossRef] [PubMed]
- Khodanovich, M.Y.; Kamaeva, D.A.; Naumova, A.V. Role of Demyelination in the Persistence of Neurological and Mental Impairments after COVID-19. Int. J. Mol. Sci. 2022, 23, 11291. [Google Scholar] [CrossRef] [PubMed]
- Kell, D.B.; Laubscher, G.J.; Pretorius, E. A Central Role for Amyloid Fibrin Microclots in Long COVID/PASC: Origins and Therapeutic Implications. Biochem. J. 2022, 479, 537–559. [Google Scholar] [CrossRef] [PubMed]
- Davies, M. Long COVID Patients Travel Abroad for Expensive and Experimental “Blood Washing”. BMJ 2022, 378, o1671. [Google Scholar] [CrossRef]
- Auwaerter, P.G. The Race to Understand Post–COVID-19 Conditions. Ann. Intern. Med. 2021, 174, 1458–1459. [Google Scholar] [CrossRef]
- Wang, C.; Yu, C.; Jing, H.; Wu, X.; Novakovic, V.A.; Xie, R.; Shi, J. Long COVID: The Nature of Thrombotic Sequelae Determines the Necessity of Early Anticoagulation. Front. Cell. Infect. Microbiol. 2022, 12, 861703. [Google Scholar] [CrossRef]
- Barrea, L.; Verde, L.; Grant, W.B.; Frias-Toral, E.; Sarno, G.; Vetrani, C.; Ceriani, F.; Garcia-Velasquez, E.; Contreras-Briceño, J.; Savastano, S.; et al. Vitamin D: A Role Also in Long COVID-19? Nutrients 2022, 14, 1625. [Google Scholar] [CrossRef]
- Corrao, S.; Mallaci Bocchio, R.; Lo Monaco, M.; Natoli, G.; Cavezzi, A.; Troiani, E.; Argano, C. Does Evidence Exist to Blunt Inflammatory Response by Nutraceutical Supplementation during COVID-19 Pandemic? An Overview of Systematic Reviews of Vitamin D, Vitamin C, Melatonin, and Zinc. Nutrients 2021, 13, 1261. [Google Scholar] [CrossRef]
- Wei, J.; Liu, X.; Xiao, W.; Lu, J.; Guan, L.; Fang, Z.; Chen, J.; Sun, B.; Cai, Z.; Sun, X.; et al. Phospholipid Remodeling and Its Derivatives Are Associated with COVID-19 Severity. J. Allergy Clin. Immunol. 2023, 151, 1259–1268. [Google Scholar] [CrossRef]
- Žarković, N.; Łuczaj, W.; Jarocka-Karpowicz, I.; Orehovec, B.; Baršić, B.; Tarle, M.; Kmet, M.; Lukšić, I.; Biernacki, M.; Skrzydlewska, E. Diversified Effects of COVID-19 as a Consequence of the Differential Metabolism of Phospholipids and Lipid Peroxidation Evaluated in the Plasma of Survivors and Deceased Patients upon Admission to the Hospital. Int. J. Mol. Sci. 2022, 23, 11810. [Google Scholar] [CrossRef] [PubMed]
- Žarković, N.; Orehovec, B.; Baršić, B.; Tarle, M.; Kmet, M.; Lukšić, I.; Tatzber, F.; Wonisch, W.; Skrzydlewska, E.; Łuczaj, W. Lipidomics Revealed Plasma Phospholipid Profile Differences between Deceased and Recovered COVID-19 Patients. Biomolecules 2022, 12, 1488. [Google Scholar] [CrossRef] [PubMed]
- Kurano, M.; Okamoto, K.; Jubishi, D.; Hashimoto, H.; Sakai, E.; Saigusa, D.; Kano, K.; Aoki, J.; Harada, S.; Okugawa, S.; et al. Dynamic Modulations of Sphingolipids and Glycerophospholipids in COVID-19. Clin. Transl. Med. 2022, 12, e1069. [Google Scholar] [CrossRef]
- Kaur, G.; Ji, X.; Rahman, I. SARS-CoV-2 Infection Alters Tryptophan Catabolism and Phospholipid Metabolism. Metabolites 2021, 11, 659. [Google Scholar] [CrossRef] [PubMed]
- Clough, E.; Inigo, J.; Chandra, D.; Chaves, L.; Reynolds, J.L.; Aalinkeel, R.; Schwartz, S.A.; Khmaladze, A.; Mahajan, S.D. Mitochondrial Dynamics in SARS-CoV-2 Spike Protein Treated Human Microglia: Implications for Neuro-COVID. J. Neuroimmune Pharmacol. 2021, 16, 770–784. [Google Scholar] [CrossRef] [PubMed]
- Hornick, M.G.; Olson, M.E.; Jadhav, A.L. SARS-CoV-2 Psychiatric Sequelae: A Review of Neuroendocrine Mechanisms and Therapeutic Strategies. Int. J. Neuropsychopharmacol. 2022, 25, 1–12. [Google Scholar] [CrossRef]
- Elkazzaz, M.; Ahmed, A.; Abo-Amer, Y.E.-E.; Hydara, T.; Haikal, A.; Razek, D.N.A.E.; Eltayb, W.A.; Wang, X.; Karpi´nski, T.M.; Hamza, D.; et al. In Silico Discovery of GPCRs and GnRHRs as Novel Binding Receptors of SARS-CoV-2 Spike Protein Could Explain Neuroendocrine Disorders in COVID-19. Vaccines 2022, 10, 1500. [Google Scholar] [CrossRef]
- Hammad, R.; Elshafei, A.; Khidr, E.G.; El-Husseiny, A.A.; Gomaa, M.H.; Kotb, H.G.; Eltrawy, H.H.; Farhoud, H. Copeptin: A Neuroendocrine Biomarker of COVID-19 Severity. Biomark. Med. 2022, 16, 589–597. [Google Scholar] [CrossRef]
- Raony, Í.; De Figueiredo, C.S.; Pandolfo, P.; Giestal-de-Araujo, E.; Oliveira-Silva Bomfim, P.; Savino, W. Psycho-Neuroendocrine-Immune Interactions in COVID-19: Potential Impacts on Mental Health. Front. Immunol. 2020, 11, 1170. [Google Scholar] [CrossRef]
- Jensterle, M.; Herman, R.; Janež, A.; Mahmeed, W.A.; Al-Rasadi, K.; Al-Alawi, K.; Banach, M.; Banerjee, Y.; Ceriello, A.; Cesur, M.; et al. The Relationship between COVID-19 and Hypothalamic–Pituitary–Adrenal Axis: A Large Spectrum from Glucocorticoid Insufficiency to Excess—The CAPISCO International Expert Panel. Int. J. Mol. Sci. 2022, 23, 7326. [Google Scholar] [CrossRef]
- Murga, I.; Aranburu, L.; Gargiulo, P.A.; Gómez Esteban, J.C.; Lafuente, J.-V. Clinical Heterogeneity in ME/CFS. A Way to Understand Long-COVID19 Fatigue. Front. Psychiatry 2021, 12, 735784. [Google Scholar] [CrossRef] [PubMed]
- Noor, N.; Urits, I.; Degueure, A.; Rando, L.; Kata, V.; Cornett, E.M.; Kaye, A.D.; Imani, F.; Narimani-Zamanabadi, M.; Varrassi, G.; et al. A Comprehensive Update of the Current Understanding of Chronic Fatigue Syndrome. Anesth. Pain. Med. 2021, 11, e113629. [Google Scholar] [CrossRef] [PubMed]
- Biggio, G.; Mostallino, M.C.; Giusti, P.; Zusso, M.; Toffano, G. Overview of the Pharmacological Properties and Therapeutic Efficacy of Phospholipid Liposomes (Liposom Forte®) in Patients with Depressive Disorders. Minerva Psychiatry 2018, 59, 45–53. [Google Scholar] [CrossRef]
- Biggio, G.; Mostallino, M.C.; Biggio, F.; Minervino, A.; Giannetti, F. Therapeutic Efficacy and Tolerability of Phospholipid Liposomes (Liposom Forte®) for the Management of Depressive Disorders in Elderly Patients. Evid. Based Psychiatr. Care 2020, 6, 76–91. [Google Scholar] [CrossRef]
- Nataf, S. An Alteration of the Dopamine Synthetic Pathway Is Possibly Involved in the Pathophysiology of COVID-19. J. Med. Virol. 2020, 92, 1743–1744. [Google Scholar] [CrossRef]
- Antonini, A.; Leta, V.; Teo, J.; Chaudhuri, K.R. Outcome of Parkinson’s Disease Patients Affected by COVID-19. Mov. Disord. 2020, 35, 905–908. [Google Scholar] [CrossRef]
- Pawlak, R.; Napiorkowska-Pawlak, D.; Takada, Y.; Urano, T.; Nagai, N.; Ihara, H.; Takada, A. The Differential Effect of Angiotensin II and Angiotensin 1-7 on Norepinephrine, Epinephrine, and Dopamine Concentrations in Rat Hypothalamus: The Involvement of Angiotensin Receptors. Brain Res. Bull. 2001, 54, 689–694. [Google Scholar] [CrossRef]
- Klempin, F.; Mosienko, V.; Matthes, S.; Villela, D.C.; Todiras, M.; Penninger, J.M.; Bader, M.; Santos, R.A.S.; Alenina, N. Depletion of Angiotensin-Converting Enzyme 2 Reduces Brain Serotonin and Impairs the Running-Induced Neurogenic Response. Cell. Mol. Life Sci. 2018, 75, 3625–3634. [Google Scholar] [CrossRef]
- Bauer, L.; Laksono, B.M.; De Vrij, F.M.S.; Kushner, S.A.; Harschnitz, O.; Van Riel, D. The Neuroinvasiveness, Neurotropism, and Neurovirulence of SARS-CoV-2. Trends Neurosci. 2022, 45, 358–368. [Google Scholar] [CrossRef]
- Lu, Y.; Zhu, Q.; Fox, D.M.; Gao, C.; Stanley, S.A.; Luo, K. SARS-CoV-2 down-Regulates ACE2 through Lysosomal Degradation. MBoC 2022, 33, ar147. [Google Scholar] [CrossRef]
- Attademo, L.; Bernardini, F. Are Dopamine and Serotonin Involved in COVID-19 Pathophysiology? Eur. J. Psychiatry 2021, 35, 62–63. [Google Scholar] [CrossRef]
- Cordeiro, L.M.S.; Rabelo, P.C.R.; Moraes, M.M.; Teixeira-Coelho, F.; Coimbra, C.C.; Wanner, S.P.; Soares, D.D. Physical Exercise-Induced Fatigue: The Role of Serotonergic and Dopaminergic Systems. Braz. J. Med. Biol. Res. 2017, 50, e6432. [Google Scholar] [CrossRef] [PubMed]
- Tornero-Aguilera, J.F.; Jimenez-Morcillo, J.; Rubio-Zarapuz, A.; Clemente-Suárez, V.J. Central and Peripheral Fatigue in Physical Exercise Explained: A Narrative Review. Int. J. Environ. Res. Public Health 2022, 19, 3909. [Google Scholar] [CrossRef] [PubMed]
- Nizzo, M.C.; Tegos, S.; Gallaminia, A.; Toffano, G.; Polleri, A.; Massarottib, M. Brain Cortex Phospholipids Liposomes Effects on CSF HVA, 5-HIAA and on Prolactin and Somatotropin Secretion in Man. J. Neural Transm. 1978, 43, 93–102. [Google Scholar] [CrossRef] [PubMed]
- Toffano, G.; Bruni, A. Pharmacological Properties of Phospholipid Liposomes. Pharmacol. Res. Commun. 1980, 12, 829–845. [Google Scholar] [CrossRef]
- Canonico, P.L.; Annunziato, L.; Toffano, G.; Bernardini, R.; Stanzani, S.; Foti, M.; Clementi, G.; Drago, F.; Scapagnini, U. In Vivo and in Vitro Interference of Phosphatidylserine Liposomes on Prolactin Secretion in the Rat. Neuroendocrinology 1981, 33, 358–362. [Google Scholar] [CrossRef]
- Inukai, S.; Hara, S.; Ichinose, H. Tyrosine Hydroxylase Activity Is Regulated through the Modification of the 176th Cysteine Residue. Biochem. Biophys. Res. Commun. 2022, 589, 209–214. [Google Scholar] [CrossRef]
- Soung, A.L.; Vanderheiden, A.; Nordvig, A.S.; Sissoko, C.A.; Canoll, P.; Mariani, M.B.; Jiang, X.; Bricker, T.; Rosoklija, G.B.; Arango, V.; et al. COVID-19 Induces CNS Cytokine Expression and Loss of Hippocampal Neurogenesis. Brain 2022, 145, 4193–4201. [Google Scholar] [CrossRef]
- Leng, A.; Shah, M.; Ahmad, S.A.; Premraj, L.; Wildi, K.; Li Bassi, G.; Pardo, C.A.; Choi, A.; Cho, S.-M. Pathogenesis Underlying Neurological Manifestations of Long COVID Syndrome and Potential Therapeutics. Cells 2023, 12, 816. [Google Scholar] [CrossRef]
- Fernández-Castañeda, A.; Lu, P.; Geraghty, A.C.; Song, E.; Lee, M.-H.; Wood, J.; O’Dea, M.R.; Dutton, S.; Shamardani, K.; Nwangwu, K.; et al. Mild Respiratory COVID Can Cause Multi-Lineage Neural Cell and Myelin Dysregulation. Cell 2022, 185, 2452–2468. [Google Scholar] [CrossRef]
- Barnes-Vélez, J.A.; Aksoy Yasar, F.B.; Hu, J. Myelin Lipid Metabolism and Its Role in Myelination and Myelin Maintenance. The Innovation 2023, 4, 100360. [Google Scholar] [CrossRef] [PubMed]
- Fledrich, R.; Abdelaal, T.; Rasch, L.; Bansal, V.; Schütza, V.; Brügger, B.; Lüchtenborg, C.; Prukop, T.; Stenzel, J.; Rahman, R.U.; et al. Targeting Myelin Lipid Metabolism as a Potential Therapeutic Strategy in a Model of CMT1A Neuropathy. Nat. Commun. 2018, 9, 3025. [Google Scholar] [CrossRef] [PubMed]
- Monastra, G.; Cross, A.H.; Bruni, A.; Raine, C.S. Phosphatidylserine, a Putative Inhibitor of Tumor Necrosis Factor, Prevents Autoimmune Demyelination. Neurology 1993, 43 Pt 1, 153. [Google Scholar] [CrossRef]
- Karimi-Galougahi, M.; Yousefi-Koma, A.; Bakhshayeshkaram, M.; Raad, N.; Haseli, S. 18FDG PET/CT Scan Reveals Hypoactive Orbitofrontal Cortex in Anosmia of COVID-19. Acad. Radiol. 2020, 27, 1042–1043. [Google Scholar] [CrossRef] [PubMed]
- Sollini, M.; Morbelli, S.; Ciccarelli, M.; Cecconi, M.; Aghemo, A.; Morelli, P.; Chiola, S.; Gelardi, F.; Chiti, A. Long COVID Hallmarks on [18F]FDG-PET/CT: A Case-Control Study. Eur. J. Nucl. Med. Mol. Imaging 2021, 48, 3187–3197. [Google Scholar] [CrossRef]
- Guedj, E.; Campion, J.Y.; Dudouet, P.; Kaphan, E.; Bregeon, F.; Tissot-Dupont, H.; Guis, S.; Barthelemy, F.; Habert, P.; Ceccaldi, M.; et al. 18F-FDG Brain PET Hypometabolism in Patients with Long COVID. Eur. J. Nucl. Med. Mol. Imaging 2021, 48, 2823–2833. [Google Scholar] [CrossRef]
- Donegani, M.I.; Miceli, A.; Pardini, M.; Bauckneht, M.; Chiola, S.; Pennone, M.; Marini, C.; Massa, F.; Raffa, S.; Ferrarazzo, G.; et al. Brain Metabolic Correlates of Persistent Olfactory Dysfunction after SARS-CoV-2 Infection. Biomedicines 2021, 9, 287. [Google Scholar] [CrossRef]
- Rudroff, T.; Workman, C.D.; Ponto, L.L.B. 18F-FDG-PET Imaging for Post-COVID-19 Brain and Skeletal Muscle Alterations. Viruses 2021, 13, 2283. [Google Scholar] [CrossRef]
- Ferrucci, R.; Cuffaro, L.; Capozza, A.; Rosci, C.; Maiorana, N.; Groppo, E.; Reitano, M.R.; Poletti, B.; Ticozzi, N.; Tagliabue, L.; et al. Brain Positron Emission Tomography (PET) and Cognitive Abnormalities One Year after COVID-19. J. Neurol. 2023, 270, 1823–1834. [Google Scholar] [CrossRef]
- Salonia, A.; Pontillo, M.; Capogrosso, P.; Pozzi, E.; Ferrara, A.M.; Cotelessa, A.; Belladelli, F.; Corsini, C.; Gregori, S.; Rowe, I.; et al. Testosterone in Males with COVID-19: A 12-month Cohort Study. Andrology 2023, 11, 17–23. [Google Scholar] [CrossRef]
- Uckert, S.; Fuhlenriede, M.H.; Becker, A.J.; Stief, C.G.; Scheller, F.; Knapp, W.H.; Jonas, U. Is There an Inhibitory Role of Cortisol in the Mechanism of Male Sexual Arousal and Penile Erection? Urol. Res. 2003, 31, 402–406. [Google Scholar] [CrossRef] [PubMed]
- Salvio, G.; Martino, M.; Giancola, G.; Arnaldi, G.; Balercia, G. Hypothalamic–Pituitary Diseases and Erectile Dysfunction. J. Clin. Med. 2021, 10, 2551. [Google Scholar] [CrossRef] [PubMed]
- Adeyemi, D.H.; Odetayo, A.F.; Hamed, M.A.; Akhigbe, R.E. Impact of COVID 19 on Erectile Function. Aging Male 2022, 25, 202–216. [Google Scholar] [CrossRef] [PubMed]
- Leema Rose, A.; Manickam, A.; Agrawal, M. A Mathematical Model for The Special Effects of Phosphatidylserine on Endocrine Reaction to Reasonable Concentration Exercise in Healthy Male Subjects. Turk. J. Comput. Math. Educ. 2021, 12, 3555–3559. [Google Scholar] [CrossRef]
- Starks, M.A.; Starks, S.L.; Kingsley, M.; Purpura, M.; Jäger, R. The Effects of Phosphatidylserine on Endocrine Response to Moderate Intensity Exercise. J. Int. Soc. Sports Nutr. 2008, 5, 11. [Google Scholar] [CrossRef] [PubMed]
- Kiriakova, N.; Kiriakov, A.; Schneider, E.; Bonev, A. Therapeutic Effect of Essential Phospholipids on Functional Sexual Disorders in Males. J. Eur. Acad. Dermatol. Venerol. 1998, 11, 191–193. [Google Scholar] [CrossRef] [PubMed]
- Casacchia, M.; Marola, W.; Meco, G.; Pirro, R.; Di Cesare, E.; Allegro, A.; Cusimano, G. Phospholipid Liposomes in Depression: A Double-Blind Study versus Placebo. Int. Pharmacopsychiatry 1982, 17, 274–279. [Google Scholar] [CrossRef]
- Aguglia, E.; Calandra, C.; Rapisarda, V.; Maugeri, D. The Effect of Hypothalamic Phospholipid Liposomes in Patients Treated with Sulpiride or Haloperidol. Acta Ther. 1984, 10, 133–144. [Google Scholar]
- Giannelli, A.; Rabboni, M.; Zarattini, F.; Malgeri, C.; Magnolfi, G. A Combination of Hypothalamic Phospholipid Liposomes with Trazodone for Treatment of Depression.: An Open Controlled Study. Acta Psychiatr. Scand. 1989, 79, 52–58. [Google Scholar] [CrossRef]
- Rachev, E.; Nalbansky, B.; Kolarov, G.; Agrosì, M. Efficacy and Safety of Phospholipid Liposomes in the Treatment of Neuropsychological Disorders Associated with the Menopause: A Double-Blind, Randomised, Placebo-Controlled Study. Curr. Med. Res. Opin. 2001, 17, 105–110. [Google Scholar] [CrossRef]
- Bruni, A.; Toffano, G.; Leon, A.; Boarato, E. Pharmacological Effects of Phosphatidylserine Liposomes. Nature 1976, 260, 331–333. [Google Scholar] [CrossRef] [PubMed]
- Kang, E.Y.; Cui, F.; Kim, H.K.; Nawaz, H.; Kang, S.; Kim, H.; Jang, J.; Go, G. Effect of Phosphatidylserine on Cognitive Function in the Elderly: A Systematic Review and Meta-Analysis. Korean J. Food Sci. Technol. 2022, 54, 52–58. [Google Scholar] [CrossRef]
- US Food and Drug Administration. Letter Updating the Phosphatidylserine and Cognitive Function and Dementia Qualified Health Claim, 2004. Available online: http://wayback.archive-it.org/7993/20171114183737/https://www.fda.gov/Food/IngredientsPackagingLabeling/LabelingNutrition/ucm072999.htm (accessed on 6 June 2023).
- Zhang, Y.Y.; Yang, L.Q.; Guo, L.M. Effect of Phosphatidylserine on Memory in Patients and Rats with Alzheimer’s Disease. Genet. Mol. Res. 2015, 14, 9325–9333. [Google Scholar] [CrossRef]
- Castro-Marrero, J.; Sáez-Francàs, N.; Santillo, D.; Alegre, J. Treatment and Management of Chronic Fatigue Syndrome/Myalgic Encephalomyelitis: All Roads Lead to Rome: Therapy and Management in CFS/ME. Br. J. Pharmacol. 2017, 174, 345–369. [Google Scholar] [CrossRef]
- Licata, G. Hypothalamic phospholipid liposomes. A drug for the treatment of anxiety-depressive syndromes in internal medicine. Recent. Prog. Med. 1984, 75, 1076–1080. [Google Scholar]
- Wolff Sagy, Y.; Feldhamer, I.; Brammli-Greenberg, S.; Lavie, G. Estimating the Economic Burden of Long-COVID: The Additive Cost of Healthcare Utilisation among COVID-19 Recoverees in Israel. BMJ Glob. Health 2023, 8, e012588. [Google Scholar] [CrossRef] [PubMed]

Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Menichetti, F. The Potential Role of Hypothalamic Phospholipid Liposomes in the Supportive Therapy of Some Manifestations of Post-COVID-19 Condition: Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS) and Brain Fog. J. Clin. Med. 2023, 12, 5478. https://doi.org/10.3390/jcm12175478
Menichetti F. The Potential Role of Hypothalamic Phospholipid Liposomes in the Supportive Therapy of Some Manifestations of Post-COVID-19 Condition: Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS) and Brain Fog. Journal of Clinical Medicine. 2023; 12(17):5478. https://doi.org/10.3390/jcm12175478
Chicago/Turabian StyleMenichetti, Francesco. 2023. "The Potential Role of Hypothalamic Phospholipid Liposomes in the Supportive Therapy of Some Manifestations of Post-COVID-19 Condition: Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS) and Brain Fog" Journal of Clinical Medicine 12, no. 17: 5478. https://doi.org/10.3390/jcm12175478
APA StyleMenichetti, F. (2023). The Potential Role of Hypothalamic Phospholipid Liposomes in the Supportive Therapy of Some Manifestations of Post-COVID-19 Condition: Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS) and Brain Fog. Journal of Clinical Medicine, 12(17), 5478. https://doi.org/10.3390/jcm12175478




